Abstract
The fractalkine/CX3CR1 axis plays an important role in regulating glucose and lipid metabolism. However, the role of fractalkine in metabolic disorders remains to be fully elucidated. We selected 887 Chinese (40–65 years old) at baseline, with a subgroup of 459 participants examined again 2 years later. The relationship of serum fractalkine levels with the metabolic syndrome (MetS) and its components was investigated. At baseline, participants with MetS had higher fractalkine concentrations than their counterparts without MetS (P < 0.001). At the 2-year follow-up, participants in the highest quartile of baseline fractalkine exhibited higher values for body mass index, waist circumference, waist-to-hip ratio, body fat percentage, glucose, insulin, total cholesterol, triglycerides (TG), and homeostasis model assessment of insulin resistance (HOMA-IR) and lower value for high density lipoprotein-cholesterol (HDL-c) (all P < 0.05). Among 390 participants without MetS at baseline, 45 developed it at year 2. Even after multiple adjustments for visceral adipose tissue area, HOMA-IR, C-reactive protein (CRP), or TG and HDL-c, baseline fractalkine predicted the development of MetS (OR = 7.18, 95%CI: 2.28–18.59). In conclusion, circulating fractalkine predicts the development of the MetS independently of central obesity, CRP, insulin resistance, and dyslipidemia.
1. Introduction
Metabolic syndrome (MetS) comprises a group of conditions, including central obesity, dyslipidemia elevated blood pressure (BP), and abnormal glucose metabolism. It is associated with increased risk of type 2 diabetes (T2DM) and cardiovascular disease (CVD). The prevalence of MetS has been increasing dramatically in China during the past decade, accompanied by the rapid economic growth and adoption of a sedentary lifestyle [1–3]. Pathophysiologically, MetS is characterized by chronic low-grade inflammatory responses which are associated with abnormal levels of cytokines and other inflammatory signaling markers [4–6].
Fractalkine (CX3CL1), the only known member of the CX3C class of chemokines, is known to convey its signals through a single G-protein-coupled receptor, CX3CR1, thereby promoting leukocyte activation and survival [7]. Fractalkine expression has been detected in activated or stressed endothelial, smooth muscle cells, skeletal muscle, macrophages, neurons, hepatocytes [8–12], and adipocytes [13]. It is characterized as a structurally unique chemokine, with both membrane-bound and soluble forms that act, respectively, to promote cell-to-cell adhesion of circulating leukocyte or as a classical chemoattractant of monocytes and lymphocytes [9, 14–16]. The soluble fractalkine is generated by cleavage of the membrane-bound form by two peptidases, ADAM10 and ADAM17 [17, 18].
Patients with unstable angina pectoris and plaque rupture [19] or CVD [8] show strongly enhanced activation of the fractalkine/CX3CR1 axis, and this signal has been implicated in the development of these pathogenic processes. A recent study reported that inflammation upregulates fractalkine, particularly in the adipose tissue of obese individuals and T2DM patients [13]. A putative explanation for the association between fractalkine and MetS was published recently [20], but the evidence of such a relationship remains scarce. Therefore, this study was designed to investigate the relationship between baseline serum fractalkine and the development of MetS using a group of middle-aged Chinese adults. In addition, the fractalkine-MetS association was evaluated to determine any potential dependence upon well-established risk factors of MetS, such as central obesity, C-reactive protein (CRP), insulin resistance, and dyslipidemia.
2. Methods and Procedures
2.1. Study Design
This population-based cross-sectional survey was conducted from March to May 2010 in the Caihe community of Hangzhou, Zhejiang province, China. A total of 887 eligible Han Chinese participants, aged 40–65 years, were recruited in the baseline study. None of the participants had a previous diagnosis of diabetes, moderate to severe hypertension (resting BP > 170/100 mmHg), other CVD, chronic renal disease, acute infectious disease or chronic inflammatory disease, endocrine disease, cancer, or treatment with lipid-lowering drugs. During the 2-year follow-up period, 428 participants dropped out because of death (n = 8), loss of contact (n = 143), or withdrawal from the study (n = 277). At the end of the study, 459 participants were followed up. The study protocol was approved by the Ethics Committee of Sir Run Run Shaw Hospital and conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from all participants. Face-to-face interviews were conducted by trained medical staff using a standardized questionnaire to collect participant demographic data and to obtain baseline lifestyle and health status information.
2.2. Laboratory Measurements
Participants visited local community health care centers between 7 and 8 am following an overnight fast. Venous blood samples were collected at 0 and 2 hours following a 75-g oral glucose tolerance test (OGTT). Blood samples obtained for laboratory testing were immediately centrifuged, and the serum was stored at −80°C. Serum glucose concentrations, triglyceride (TG), total cholesterol (TC), low density lipoprotein-cholesterol (LDL-c), high density lipoprotein-cholesterol (HDL-c), and CRP were assayed with an autoanalyzer (Aeroset, Chicago, IL, USA). Glycosylated hemoglobin A1c (HbA1c) was measured by ion-exchange high-performance liquid chromatography (Hemoglobin Testing System; Bio-Rad, Hercules, CA, USA). Serum insulin levels were measured by a radioimmunoassay using an insulin detection kit (Beijing North Institute of Biological Technology, China). Homeostatic model assessment of insulin resistance (HOMA-IR) was calculated using the following formula: [fasting serum insulin (FINS; mU/L) × fasting serum glucose (FPG; mmol/L)/22.5] [21]. Fractalkine concentration was determined with a commercially available enzyme-linked immunosorbent assay (R&D Systems, Minneapolis, MN, USA). All assay procedures followed the manufacturer's instructions. Intra- and interassay coefficient of variation were 1.7% to 4.3% and 3.5% to 7.9%, respectively.
2.3. Anthropometric Measurement
Body mass index (BMI) was calculated by dividing body weight by height squared (kg/m2). Waist circumference (WC) was measured at the midpoint between the lower border of the rib cage and the iliac crest. Hip circumference was measured at the widest point of the hips, and the waist-to-hip ratio (WHR) was calculated and recorded for each patient. Both measurements were taken while the patient was standing. Body fat percentage (Fat%) was measured by bioelectrical impedance analysis (TBF-300, Tanita Co., Tokyo, Japan). Systolic blood pressure (SBP) and diastolic blood pressure (DBP) were measured in triplicate using a mercury sphygmomanometer, and the average of the three measurements was recorded.
Abdominal adipose tissue was measured using a whole-body imaging system (SMT-100, Shimadzu Co., Kyoto, Japan) with TR-500 and TE-200 of SE. Magnetic resonance imaging (MRI) was performed at the umbilical level with the participant in a supine position; abdominal visceral adipose tissue area (VFA) and abdominal subcutaneous adipose tissue area (SFA) were calculated with the accompanying software.
2.4. Definition of MetS
MetS was defined according to criteria established by the Joint Committee for Developing Chinese Guidelines on Prevention and Treatment of Dyslipidemia in Adults (JCDCG) [22]. Individuals with three or more of the following abnormalities were considered as having MetS: central obesity (WC > 90 cm for men and >85 cm for women); hypertriglyceridemia (≥1.70 mmol/L); low HDL-C (<1.04 mmol/L); elevated BP (≥130/85 mmHg or current treatment for hypertension); and hyperglycemia (FPG ≥ 6.1 mmol/L or 2 h postprandial glucose (2 h PG) ≥7.8 mmol/L).
2.5. Statistical Analyses
Normally distributed variables were expressed as mean ± standard deviation (SD); variables with a skewed distribution, including fractalkine, insulin, glucose, HOMA-IR, TC, TG, CRP, SFA, and VFA, underwent a lg(x) transformation to achieve a normal distribution and were reported as median value (interquartile range) [M(IQR)]. Categorical variables were expressed as frequency and percentage. Fractalkine levels of the 459 participants with 2-year follow-up data were grouped into quartiles to simplify the interpretation of the results of subsequent analyses. The chi-squared test was used to compare categorical variables between groups. For continuous variables, t-test was used to compare between 2 groups, and ANOVA test was used for comparison of multiple groups. Bivariate correlation analyses between fractalkine and the metabolic parameters were performed using Pearson's correlation analysis. The adjusted odds ratios (ORs) for the development of MetS at year 2 according to the baseline fractalkine quartiles were calculated in multivariate logistic regression models. Potential confounders, including age, sex, and lifestyle factors, were carefully controlled. Potential interactions between VFA, CRP, HOMA-IR, TG, HDL-c, and fractalkine were also examined. All statistical analyses were performed with SPSS 20.0 (IBM, Armonk, NY, USA) and considered statistically significant when the 2-sided P value was <0.05.
3. Results
The baseline characteristics for all participants are shown in Table 1. The mean (±SD) age was 56.90 (±7.28) years, and 39.5% of the participants were male. Among the participants, 14.2% had MetS. The median (range) for serum fractalkine was 0.44 (0.28–0.65) ng/mL for males and 0.40 (0.25–0.62) ng/mL for females (P = 0.379). As expected, participants with MetS at baseline had a greater number of adverse risk factors than participants without MetS, including higher BMI, WHR, Fat%, insulin, HOMA-IR, HbA1c, TC, CRP, SFA, VFA, and MetS defining parameters (Table 1, P < 0.05 for all parameters). In addition, the fractalkine concentration was significantly higher in participants with the MetS (Table 1, P < 0.001).
Table 1.
Baseline characteristics of participants according to the presence or absence of the MetS (n = 887).
| Variables | Total | Metabolic syndrome absent | Metabolic syndrome | P for trend |
|---|---|---|---|---|
| n (case/control) | 887 | 761 | 126 | |
| Fractalkine (ng/mL) | 0.41 (0.25–0.64) | 0.40 (0.23–0.59) | 0.65 (0.48–0.74) | <0.001 |
| Age (years) | 56.90 ± 7.28 | 56.72 ± 7.34 | 57.96 ± 6.81 | 0.077 |
| Male, n (%) | 350 (39.5) | 271 (35.6) | 79 (62.7) | <0.001 |
| Education level, n (%) | 0.668 | |||
| Less than high school | 80 (9.0) | 68 (8.9) | 12 (9.5) | |
| High school | 674 (76.0) | 582 (76.5) | 92 (73.0) | |
| More than high school | 133 (15.0) | 111 (14.6) | 22 (17.5) | |
| Current smoker, n (%) | 218 (24.6) | 162 (21.3) | 56 (44.4) | <0.001 |
| Alcohol drinker, n (%) | 187 (21.1) | 146 (19.2) | 41 (32.5) | 0.001 |
| BMI (kg/m2) | 23.46 ± 2.93 | 23.02 ± 2.68 | 26.13 ± 2.96 | <0.001 |
| WC (cm) | 78.44 ± 9.06 | 76.76 ± 8.18 | 88.62 ± 7.34 | <0.001 |
| WHR | 0.87 ± 0.07 | 0.86 ± 0.07 | 0.94 ± 0.06 | <0.001 |
| Fat% (%) | 29.14 ± 7.05 | 28.57 ± 6.77 | 32.55 ± 7.75 | <0.001 |
| SBP (mm Hg) | 124.04 ± 16.57 | 122.15 ± 16.02 | 135.41 ± 15.32 | <0.001 |
| DBP (mm Hg) | 81.02 ± 9.92 | 79.90 ± 9.60 | 87.71 ± 9.20 | <0.001 |
| FPG (mmol/L) | 4.83 (4.50–5.22) | 4.78 (4.44–5.17) | 5.17 (4.78–6.11) | <0.001 |
| 2 h PG (mmol/L) | 5.33 (4.50–6.50) | 4.72 (4.11–5.61) | 7.33 (5.22–9.44) | <0.001 |
| FINS (μU/mL) | 10.64 (8.19–13.86) | 10.09 (8.02–12.92) | 14.95 (11.40–18.66) | <0.001 |
| 2 h INS (μU/mL) | 56.45 (37.17–86.06) | 53.08 (35.61–80.24) | 86.44 (52.88–155.52) | <0.001 |
| HOMA-IR | 2.27 (1.72–3.09) | 2.11 (1.65–2.83) | 3.60 (2.62–5.12) | <0.001 |
| HbA1c (%) | 5.64 ± 0.60 | 5.59 ± 0.54 | 5.98 ± 0.83 | <0.001 |
| TC (mmol/L) | 5.57 (4.90–6.24) | 5.54 (4.87–6.22) | 5.75 (5.21–6.42) | 0.017 |
| LDL-c (mmol/L) | 2.42 ± 0.59 | 2.42 ± 0.58 | 2.44 ± 0.65 | 0.664 |
| HDL-c (mmol/L) | 1.46 ± 0.37 | 1.52 ± 0.36 | 1.12 ± 0.24 | <0.001 |
| TG (mmol/L) | 1.29 (0.95–1.82) | 1.22 (0.89–1.59) | 2.38 (1.84–3.39) | <0.001 |
| CRP (mg/dL) | 0.63 (0.28–1.59) | 0.60 (0.27–1.41) | 1.77 (0.79–4.38) | 0.003 |
| SFA (cm2) | 154.6 (118.90–203.90) | 152.90 (115.65–201.50) | 176.40 (137.58–211.83) | <0.001 |
| VFA (cm2) | 69.41 (45.90–110.50) | 63.39 (41.77–97.76) | 127.35 (102.40–163.18) | <0.001 |
| Central obesity (%) | 122 (13.8) | 53 (7.0) | 69 (55.2) | <0.001 |
| Elevated BP (%) | 467 (52.6) | 353 (46.4) | 114 (90.5) | <0.001 |
| Hyperglycemia (%) | 134 (15.1) | 71 (9.3) | 63 (50.0) | <0.001 |
| Hypertriglyceridemia (%) | 266 (30.0) | 152 (20.0) | 114 (90.5) | <0.001 |
| Low HDL-c (%) | 83 (9.4) | 25 (3.3) | 58 (46.0) | <0.001 |
Variables with normal distributions are presented as mean ± SD; skewed variables are presented as the median value (interquartile range) [M (IQR)]. The chi-squared test was used for categorical values and t-test for continuous. P for trend depicts the significance in the difference of the mean values between participants with and without metabolic syndrome. MetS: metabolic syndrome; BMI: body mass index; WC: waist circumference; WHR: waist-hip ratio; Fat%: body fat percentage; SBP: systolic blood pressure; DBP: diastolic blood pressure; FPG: fasting serum glucose; 2 h PG: 2-hour postprandial glucose; FINS: fasting insulin; 2 h INS: 2-hour insulin; HOMA-IR: homeostatic model assessment of insulin resistance; HbA1c: glycosylated hemoglobin A1c; TC: total cholesterol; LDL-c: low density lipoprotein-cholesterol; HDL-c: high density lipoprotein-cholesterol; TG: triglyceride; CRP: C-reactive protein; SFA: subcutaneous adipose tissue area; and VFA: visceral adipose tissue area.
Serum fractalkine concentration was positively correlated with BMI, WC, WHR, Fat%, BP, blood glucose, insulin, HOMA-IR, TC, TG, SFA, and VFA but negatively correlated with serum HDL-c after adjustment for age, sex, education, smoking, and drinking at baseline (Table 2). Of all the metabolic parameters, fractalkine showed the strongest correlation with VFA (r = 0.28, P < 0.001).
Table 2.
Correlations between serum fractalkine and metabolic parameters at baseline (n = 887).
| Unadjusted | Age-, sex-, education-, smoking-, and drinking-adjusted | |||
|---|---|---|---|---|
| r | P value | r | P value | |
| BMI | 0.24 | <0.001 | 0.16 | 0.001 |
| WC | 0.29 | <0.001 | 0.23 | <0.001 |
| WHR | 0.26 | <0.001 | 0.20 | <0.001 |
| Fat% | 0.23 | <0.001 | 0.23 | <0.001 |
| SBP | 0.23 | <0.001 | 0.12 | 0.019 |
| DBP | 0.19 | <0.001 | 0.12 | 0.013 |
| FPGa | 0.19 | <0.001 | 0.14 | 0.006 |
| 2 h PGa | 0.25 | <0.001 | 0.24 | <0.001 |
| FINSa | 0.21 | <0.001 | 0.17 | 0.001 |
| 2 h insulina | 0.24 | <0.001 | 0.24 | <0.001 |
| HOMA-IRa | 0.25 | <0.001 | 0.20 | <0.001 |
| HbA1c | 0.08 | 0.020 | 0.10 | 0.053 |
| TCa | 0.16 | <0.001 | 0.10 | 0.040 |
| LDL-c | 0.17 | <0.001 | 0.18 | 0.058 |
| HDL-c | −0.14 | <0.001 | −0.15 | <0.001 |
| TGa | 0.24 | <0.001 | 0.20 | <0.001 |
| CRPa | 0.10 | 0.030 | 0.09 | 0.062 |
| SFAa | 0.20 | <0.001 | 0.20 | <0.001 |
| VFAa | 0.32 | <0.001 | 0.28 | <0.001 |
Abbreviations as in Table 1.
Coefficients were performed using Pearson's correlation analysis.
alg(x) transformation was performed because of a skewed distribution.
After the 2-year follow-up, 459 participants were completely investigated. There was no significant difference in baseline characteristics between these subjects and the general participants (see Table 1 in Supplementary Material available online at http://dx.doi.org/10.1155/2014/715148). Among them, 399 participants did not have MetS at baseline. Participants in the higher fractalkine quartiles at baseline exhibited higher levels for BMI, WC, WHR, Fat%, blood glucose, insulin, HOMA-IR, TC, and TG (all P < 0.05) than participants in the lower quartile after 2 years. In addition, participants with higher fractalkine levels had lower HDL-c levels (P = 0.035). The prevalence of MetS and each component at year 2 increased along with the elevation of baseline fractalkine concentration (Table 3 and Figure 1). As presented in Table 4, the baseline age-, sex-, education-, smoking-, and drinking-adjusted fractalkine was found to have significant positive correlations with multiple adverse metabolic parameters at year 2, including high BMI, WC, WHR, Fat%, blood glucose, insulin, HOMA-IR, HbA1c, and TG. On the other hand, a significant negative correlation was found between baseline fractalkine and HDL-c level at year 2. In addition, the number of MetS components, indicated as ≤1, 2, 3, and ≥4, increased gradually across the baseline fractalkine concentration at the 2-year follow-up (Figure 2).
Table 3.
Association of baseline fractalkine concentrations with metabolic parameters at year 2 (n = 459).
| Variables | Q1 | Q2 | Q3 | Q4 | P for trend |
|---|---|---|---|---|---|
| ≤0.28 ng/mL | 0.28–0.43 ng/mL | 0.43–0.64 ng/mL | >0.64 ng/mL | ||
| n (case/control) | 115 | 114 | 115 | 115 | |
| Fractalkine (ng/mL) | 0.18 (0.10–0.23) | 0.35 (0.30–0.40) | 0.51 (0.48–0.57) | 0.71 (0.66–0.78) | <0.001 |
| Age (years) | 57.92 ± 6.58 | 57.75 ± 6.80 | 60.57 ± 6.01 | 60.73 ± 6.44 | <0.001 |
| Male, n (%) | 39 (35.4) | 42 (37.8) | 44 (38.9) | 45 (39.8) | 0.855 |
| Education | 0.992 | ||||
| Less than high school | 11 (9.7) | 11 (9.9) | 11 (9.7) | 13 (11.5) | |
| High school | 86 (76.1) | 83 (74.8) | 88 (77.9) | 83 (73.5) | |
| More than high school | 16 (14.2) | 17 (15.3) | 14 (12.4) | 17 (15.0) | |
| Current smoker, n (%) | 24 (21.2) | 24 (21.6) | 22 (19.5) | 29 (25.7) | 0.717 |
| Alcohol drinker, n (%) | 15 (13.3) | 24 (21.6) | 25 (22.1) | 29 (25.7) | 0.127 |
| MetS, n (%) | 6 (6.6) | 14 (12.6) | 31 (27.4) | 40 (35.4) | <0.001 |
| BMI (kg/m2) | 22.84 ± 2.50 | 24.04 ± 2.64 | 24.77 ± 2.84 | 24.83 ± 2.86 | 0.001 |
| WC (cm) | 75.71 ± 8.31 | 80.61 ± 7.67 | 83.69 ± 9.13 | 85.35 ± 9.25 | <0.001 |
| WHR | 0.84 ± 0.07 | 0.88 ± 0.06 | 0.89 ± 0.07 | 0.91 ± 0.08 | <0.001 |
| Fat% (%) | 27.92 ± 9.71 | 29.52 ± 6.82 | 30.75 ± 6.29 | 31.51 ± 8.75 | 0.006 |
| SBP (mm Hg) | 117.05 ± 14.34 | 117.32 ± 11.78 | 121.11 ± 13.97 | 120.71 ± 14.81 | 0.117 |
| DBP (mm Hg) | 70.24 ± 9.78 | 71.19 ± 8.39 | 73.85 ± 9.69 | 72.77 ± 9.54 | 0.069 |
| FPG (mmol/L) | 5.00 (4.70–5.20) | 5.10 (4.90–5.45) | 5.10 (4.80–5.50) | 5.30 (5.00–5.85) | <0.001 |
| 2 h PG (mmol/L) | 5.50 (4.30–6.50) | 5.60 (4.65–6.60) | 5.80 (5.00–7.00) | 5.90 (5.10–7.95) | <0.001 |
| FINS (μU/mL) | 5.83 (4.20–9.28) | 7.89 (5.90–9.91) | 8.44 (5.86–11.25) | 8.30 (5.94–11.48) | <0.001 |
| 2 h INS (μU/mL) | 27.62 (16.32–47.32) | 33.52 (20.67–49.04) | 39.60 (22.25–61.16) | 36.55 (23.53–65.52) | 0.002 |
| HOMA-IR | 1.27 (0.85–2.08) | 1.78 (1.36–2.30) | 1.93 (1.31–2.68) | 2.08 (1.39–2.73) | <0.001 |
| HbA1c (%) | 5.40 ± 0.31 | 5.53 ± 0.39 | 5.57 ± 0.46 | 5.64 ± 1.13 | 0.060 |
| TC (mmol/L) | 4.80 (4.20–5.60) | 5.05 (4.20–5.80) | 5.00 (4.70–5.60) | 5.30 (4.70–5.80) | 0.013 |
| LDL-c (mmol/L) | 3.01 ± 0.86 | 3.16 ± 0.88 | 3.22 ± 0.83 | 3.28 ± 0.94 | 0.137 |
| HDL-c (mmol/L) | 1.36 ± 0.32 | 1.28 ± 0.26 | 1.27 ± 0.31 | 1.25 ± 0.30 | 0.035 |
| TG (mmol/L) | 1.00 (0.80–1.40) | 1.15 (0.90–1.73) | 1.40 (1.00–1.85) | 1.60 (1.10–2.10) | <0.001 |
Variables with normal distributions are presented as mean ± SD; skewed variables are presented as the median value (interquartile range) [M (IQR)].
The chi-squared test was used for categorical values and ANOVA test for continuous values.
Abbreviations as in Table 1.
Figure 1.
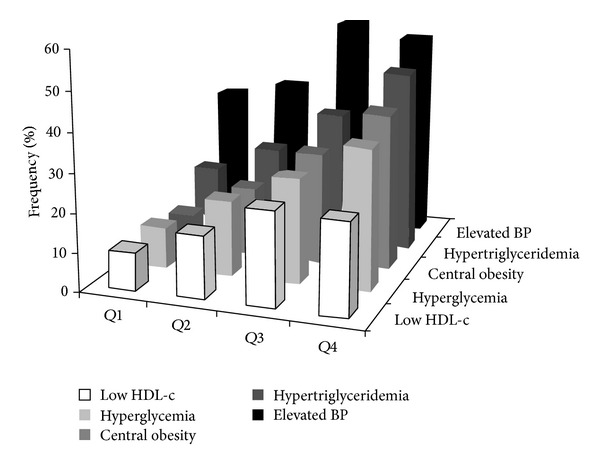
The frequency of each MetS component plotted according to baseline fractalkine quartiles at year 2.
Table 4.
Correlations between baseline fractalkine and metabolic parameters at year 2 (n = 459).
| Unadjusted | Age-, sex-, education-, smoking-, and drinking-adjusted | |||
|---|---|---|---|---|
| r | P value | r | P value | |
| BMI | 0.24 | <0.001 | 0.23 | <0.001 |
| WC | 0.28 | <0.001 | 0.27 | <0.001 |
| WHR | 0.24 | <0.001 | 0.24 | <0.001 |
| Fat% | 0.12 | 0.009 | 0.18 | <0.001 |
| SBP | 0.11 | 0.054 | 0.04 | 0.470 |
| DBP | 0.11 | 0.053 | 0.07 | 0.187 |
| FPGa | 0.20 | <0.001 | 0.16 | 0.001 |
| 2 h PGa | 0.22 | <0.001 | 0.20 | <0.001 |
| FINSa | 0.20 | <0.001 | 0.17 | 0.001 |
| 2 h insulina | 0.17 | <0.001 | 0.21 | <0.001 |
| HOMA-IRa | 0.23 | <0.001 | 0.21 | <0.001 |
| HbA1c | 0.10 | 0.037 | 0.11 | 0.024 |
| TCa | 0.14 | 0.011 | 0.10 | 0.058 |
| LDL-c | 0.11 | 0.033 | 0.08 | 0.130 |
| HDL-c | −0.16 | 0.001 | −0.18 | <0.001 |
| TGa | 0.24 | <0.001 | 0.23 | <0.001 |
Abbreviations as in Table 1.
Coefficients were performed using Pearson's correlation analysis.
alg(x) transformation was performed because of a skewed distribution
Figure 2.
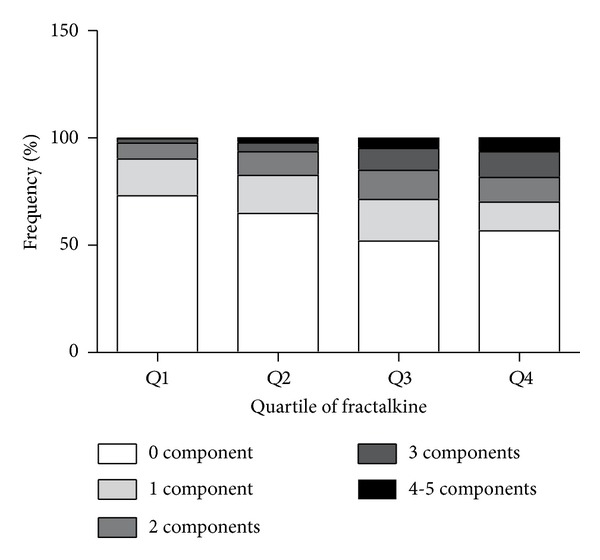
The number of MetS components plotted according to baseline fractalkine quartiles at year 2.
Among 399 participants who did not have MetS at baseline, 45 had developed MetS at year 2. Nine of 399 participants were on statins at year 2 but did not have pretreatment lipid profiles for accurate classification of the MetS status and hence were excluded from year 2 analysis. The baseline fractalkine concentrations were significantly higher in participants who had progressed to MetS by year 2 than in participants without MetS [0.51 (0.36–0.68) versus 0.40 (0.24–0.58), P < 0.001]. In the multiple stepwise logistic regression analysis, participants in the higher quartiles for fractalkine had higher OR for the development of MetS and its components by year 2.Table 5 (model 2) showed that, compared with the lowest quartile of fractalkine concentration, the ORs in the highest quartile were 7.18 (95% CI: 2.28–18.59) for MetS, 4.83 (95% CI: 2.09–11.19) for central obesity, 1.03 (95% CI: 0.55–1.93) for elevated BP, 3.61 (95% CI: 1.63–8.02) for hyperglycemia, 2.63 (95% CI: 1.30–5.34) for hypertriglyceridemia, and 1.59 (95% CI: 0.60–4.24) for low HDL-c. Further adjustment for VFA (model 3), VFA and CRP (model 4), HOMA-IR (model 5), or TG and HDL-c (model 6) only slightly reduced the magnitude of the association of baseline fractalkine with the development of MetS (OR = 5.31, 95% CI: 1.65–14.09 for model 3, OR = 5.17, 95% CI: 1.60–13.74 for model 4, OR = 5.73, 95% CI: 1.79–14.34 for model 5, and OR = 5.94, 95% CI: 1.85–15.09 for model 6). These results suggest that the association between fractalkine and the development of MetS is independent of central obesity, CRP, insulin resistance, and dyslipidemia. In addition, circulating fractalkine concentration was significantly associated with the development of each MetS component (Table 5). The associations of fractalkine with hyperglycemia were particularly strong and independent of VFA; the association between fractalkine and the other MetS components was largely explained by central obesity.
Table 5.
Multiple logistic regression analysis of baseline fractalkine quartiles in the prediction of MetS and its components at year 2: ORs (n = 390).
| ORs (95% CI) | Q1 | Q2 | Q3 | Q4 | P for trend |
|---|---|---|---|---|---|
| ≤0.28 ng/mL | 0.28–0.43 ng/mL | 0.43–0.64 ng/mL | >0.64 ng/mL | ||
| MetS | |||||
| Model 1 | 1 | 1.61 (0.73–3.52) | 2.81 (1.17–6.74) | 7.05 (2.26–18.00) | <0.001 |
| Model 2 | 1 | 1.64 (0.75–3.63) | 2.89 (1.19–6.98) | 7.18 (2.28–18.59) | <0.001 |
| Model 3 | 1 | 1.80 (0.79–4.10) | 2.67 (1.08–6.59) | 5.31 (1.65–14.09) | 0.016 |
| Model 4 | 1 | 1.81 (0.79–4.16) | 2.65 (1.06–6.61) | 5.17 (1.60–13.74) | 0.019 |
| Model 5 | 1 | 1.67 (0.75–3.73) | 2.86 (1.17–6.99) | 5.73 (1.79–14.34) | 0.007 |
| Model 6 | 1 | 1.50 (0.66–3.40) | 2.64 (1.06–6.56) | 5.94 (1.85–15.09) | 0.006 |
| Central obesity | |||||
| Model 1 | 1 | 1.46 (0.75–2.84) | 2.44 (1.19–4.99) | 5.00 (2.17–11.50) | <0.001 |
| Model 2 | 1 | 1.43 (0.73–2.80) | 2.37 (1.15–4.87) | 4.83 (2.09–11.19) | <0.001 |
| Model 3 | 1 | 1.28 (0.62–2.65) | 1.60 (0.73–3.48) | 2.46 (0.99–6.03) | 0.146 |
| Model 4 | 1 | 1.46 (0.69–3.06) | 1.51 (0.72–2.99) | 2.18 (0.95–6.01) | 0.126 |
| Model 5 | 1 | 1.44 (0.73–2.84) | 2.34 (1.13–4.84) | 4.17 (1.78–9.79) | 0.004 |
| Model 6 | 1 | 1.41 (0.72–2.80) | 2.36 (1.14–4.91) | 4.58 (1.96–10.72) | 0.001 |
| Elevated BP | |||||
| Model 1 | 1 | 0.54 (0.29–1.11) | 1.10 (0.59–2.05) | 1.08 (0.59–2.01) | 0.069 |
| Model 2 | 1 | 0.53 (0.28–1.10) | 1.09 (0.58–2.07) | 1.03 (0.55–1.93) | 0.078 |
| Model 3 | 1 | 0.54 (0.28–1.12) | 1.03 (0.54–1.97) | 0.86 (0.45–1.64) | 0.150 |
| Model 4 | 1 | 0.49 (0.27–1.04) | 0.94 (0.49–1.80) | 0.77 (0.40–1.48) | 0.118 |
| Model 5 | 1 | 0.53 (0.28–1.11) | 1.08 (0.57–2.04) | 0.90 (0.47–1.72) | 0.105 |
| Model 6 | 1 | 0.52 (0.28–1.08) | 1.05 (0.55–1.99) | 0.95 (0.50–1.80) | 0.085 |
| Hyperglycemia | |||||
| Model 1 | 1 | 1.65 (0.82–3.32) | 1.87 (0.92–3.79) | 3.53 (1.60–7.81) | 0.014 |
| Model 2 | 1 | 1.66 (0.82–3.35) | 1.89 (0.93–3.83) | 3.61 (1.63–8.02) | 0.013 |
| Model 3 | 1 | 1.69 (0.83–3.43) | 1.83 (0.90–3.74) | 3.35 (1.49–7.55) | 0.029 |
| Model 4a | 1 | 1.71 (0.84–3.51) | 1.86 (0.90–3.84) | 3.40 (1.49–7.75) | 0.029 |
| Model 5 | 1 | 1.68 (0.83–3.41) | 1.84 (0.90–3.75) | 3.07 (1.24–7.14) | 0.071 |
| Model 6 | 1 | 1.69 (0.83–3.43) | 1.92 (0.94–3.92) | 3.57 (1.60–7.99) | 0.016 |
| Hypertriglyceridemiab | |||||
| Model 1 | 1 | 1.37 (0.71–2.64) | 1.82 (0.93–3.55) | 2.69 (1.33–5.44) | 0.038 |
| Model 2 | 1 | 1.36 (0.70–2.62) | 1.78 (0.91–3.50) | 2.63 (1.30–5.34) | 0.046 |
| Model 3 | 1 | 1.38 (0.71–2.68) | 1.72 (0.87–3.38) | 2.28 (1.01–4.69) | 0.141 |
| Model 4 | 1 | 1.09 (0.55–2.17) | 1.33 (0.65–2.69) | 1.75 (0.83–3.71) | 0.460 |
| Model 5 | 1 | 1.36 (0.70–2.63) | 1.77 (0.90–3.47) | 2.33 (1.03–4.79) | 0.113 |
| Model 6 | 1 | 1.33 (0.67–2.63) | 1.82 (0.91–3.64) | 2.46 (1.19–5.11) | 0.080 |
| Low HDL-cb | |||||
| Model 1 | 1 | 0.84 (0.34–2.10) | 0.93 (0.38–2.32) | 1.51 (0.58–3.98) | 0.595 |
| Model 2 | 1 | 0.86 (0.34–2.15) | 0.96 (0.38–2.38) | 1.59 (0.60–4.24) | 0.550 |
| Model 3 | 1 | 0.86 (0.34–2.16) | 0.95 (0.38–2.38) | 1.50 (0.56–4.05) | 0.665 |
| Model 4 | 1 | 0.92 (0.37–2.34) | 1.04 (0.41–2.64) | 1.69 (0.61–4.63) | 0.603 |
| Model 5 | 1 | 0.85 (0.34–2.14) | 0.96 (0.39–2.40) | 1.64 (0.61–4.42) | 0.532 |
| Model 6 | 1 | 0.92 (0.37–2.34) | 1.05 (0.42–2.64) | 1.78 (0.66–4.80) | 0.502 |
OR: odds ratio, CI: confidence interval.
Model 1: adjusted for age, sex.
Model 2: further adjusted for education attainment, smoking, alcohol, and drinking based on model 1.
Model 3: further adjusted for visceral fat based on model 2.
Model 4: further adjusted for CRP based on model 3.
Model 5: further adjusted for HOMA-IR based on model 2; afor hyperglycemia: further adjusted for FINS based on model 2.
Model 6: further adjusted for TG and HDL-c based on model 2.
bNot adjusted for itself.
Abbreviations as in Table 1.
4. Discussion
Altered circulating cytokine levels can be used as early abnormal markers and may contribute to MetS development. This study addressed the relationship between fractalkine and the development of MetS in a 2-year prospective study. We found that elevated serum fractalkine concentrations were significantly correlated with the development of MetS. And the MetS severity at the 2-year follow-up defined as the number of MetS components increased along with the elevation of baseline fractalkine concentration. Central obesity, insulin resistance, inflammatory marker (CRP), and dyslipidemia are well-established risk factors of MetS [23–25]. However, in this study, adjustments for VFA, CRP, HOMA-IR, or TG and HDL-c and other potential confounders yielded only minor reductions in the risk of MetS development across fractalkine quartiles. Thus, the observed association between fractalkine concentrations and development of MetS cannot be attributed mainly to central obesity, CRP, insulin resistance, or dyslipidemia.
In this study, body composition was assessed not only by BMI, WC, WHR, and Fat%, but also by SFA and VFA. Body fat distribution, especially visceral fat accumulation, is more strongly correlated with obesity-related metabolic disorders than the overall amount of body fat [26, 27]. Compared with subcutaneous fat, visceral adipose tissue is known to have more extensive inflammatory leukocyte infiltration [28] and adipocytokines content [29]. Shah et al. [13] reported that fractalkine levels in subcutaneous adipose were significantly higher in obese individuals compared to their lean counterparts and that fractalkine concentrations were more strongly correlated with visceral than subcutaneous adiposity. However, they did not report an observation of increased serum fractalkine concentrations in the obese participants. Recent studies in 3306 middle-aged UK women and in a group of obese Mexican-American children both showed higher fractalkine levels in obese participants with MetS than in nonobese participants. However, the differences did not reach statistical significance [30, 31]. Our analysis showed a positive correlation between serum fractalkine levels and BMI, WC, WHR, Fat%, SFA, and VFA. The discrepancies between those studies and our results might be explained by differences in study design and in the methods of selecting the study participants.
There are also differences in the available study data describing the association between fractalkine levels and hyperglycemia. Shah et al. [13] reported that serum fractalkine concentrations were significantly higher in 281 patients with T2DM than in 274 nondiabetic participants. Another study using a cohort of middle-aged UK women showed that higher fractalkine levels were correlated with elevated insulin levels [30]. Our data from both cross-sectional and prospective studies also suggest that serum fractalkine is positively associated with glucose and insulin. However, in another study of CVD patients with and without T2DM or with and without MetS, no differences in circulating fractalkine concentration or expression of CX3CR1 were observed [32]. The lack of correlation between fractalkine levels and diabetes has also been reported by others [8, 33, 34]. Accumulating evidence, mainly from cell culture and animal studies, suggests that high glucose concentrations, similar to those seen in type 2 diabetes, promote the expression of fractalkine by smooth muscle cells and endothelial cells in vitro, which may then enhance monocyte adhesion and potentially promote atherogenesis [35, 36].
Relationships between circulating fractalkine concentrations and the lipoprotein-lipid profile have been observed in some studies. Franco et al. [30] reported that increased fractalkine levels correlated with elevated levels of Apo-B and LDL-c. Statin therapy can significantly reduce the expression of fractalkine and CX3CR1 [33]. In the present study, we found significant correlations between circulating fractalkine and TG and HDL-c at baseline and at the 2-year follow-up. And the fractalkine concentrations were associated with the development of hypertriglyceridemia, however, which was largely mediated by VFA or HOMA-IR. Therefore, it may also be possible that relationships reported in other cross-sectional studies between the lipid profile and fractalkine levels were not causal but largely explained by the concomitant variation in central obesity or insulin resistance.
Recent studies have shown that inflammatory cytokines, such as TNF-α, IFN-γ, and IL-1β, may upregulate membrane-bound fractalkine expression and the release of functional, soluble fractalkine from the bound form [9, 37, 38]. Notably, in our study, we did not observe a significant correlation between fractalkine and CRP. And the effect of CRP on the fractalkine-MetS association was rather minor. Together, this data suggested that fractalkine might provide incremental value in MetS prediction beyond current approaches. Further studies are required to determine whether an increase in circulating fractalkine is merely a reflection of obesity-related inflammation or the result of specific regulation by common mediators in adipocytes.
There are some limitations in the present study. First, because of the relatively short follow-up time of 2 years, only a small number of participants developed MetS. Whether serum fractalkine levels can be useful in predicting MetS has to be confirmed in studies involving larger populations with different genetic and environmental backgrounds. Secondly, although participants with a higher baseline serum fractalkine level present a higher risk of developing MetS, we did not have sufficient data on cardiovascular end points to investigate whether this would translate into a greater risk of cardiovascular mortality or morbidity. Thirdly, the dietary intake and work-related physical activity were not assessed in our study. Thus, the data are subject to potential under- or overestimation.
In conclusion, in this population-based middle-aged Chinese cohort, we have shown that serum fractalkine levels could predict the development of the MetS. Our findings suggest that fractalkine plays a potential role in the pathogenesis of MetS that is independent of its relationship with central obesity as reflected by VFA, insulin resistance as reflected by HOMA-IR, systemic inflammation as reflected by CRP, and dyslipidemia as reflected by TG and HDL-c. Further studies are required to investigate the efficacy of fractalkine as a biomarker or intervention target for MetS.
Supplementary Material
Supplementary table 1. Baseline Characteristics of Participants Completely Investigated According to the Presence or Absence of the Mets (n=459).
Acknowledgments
This study was supported by Grants from the Science and Technology Major Project of Zhejiang Province (no. 2009C03010-4), the National Key Technology R&D Program of China (no. 2012BAI02B03), and the National Key Technology R&D Program of China (no. 2009BAI80B00).
Conflict of Interests
The authors report no conflict of interests and declare no competing financial interests.
References
- 1.Gu D, Reynolds K, Wu X, et al. Prevalence of the metabolic syndrome and overweight among adults in China. The Lancet. 2005;365(9468):1398–1405. doi: 10.1016/S0140-6736(05)66375-1. [DOI] [PubMed] [Google Scholar]
- 2.Wang Y, Mi J, Shan X-Y, Wang QJ, Ge K-Y. Is China facing an obesity epidemic and the consequences? The trends in obesity and chronic disease in China. International Journal of Obesity. 2007;31(1):177–188. doi: 10.1038/sj.ijo.0803354. [DOI] [PubMed] [Google Scholar]
- 3.Yang W, Lu J, Weng J, et al. Prevalence of diabetes among men and women in China. The New England Journal of Medicine. 2010;362(12):1090–1101. doi: 10.1056/NEJMoa0908292. [DOI] [PubMed] [Google Scholar]
- 4.Hotamisligil GS. Inflammation and metabolic disorders. Nature. 2006;444(7121):860–867. doi: 10.1038/nature05485. [DOI] [PubMed] [Google Scholar]
- 5.Lumeng CN, Saltiel AR. Inflammatory links between obesity and metabolic disease. Journal of Clinical Investigation. 2011;121(6):2111–2117. doi: 10.1172/JCI57132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haffner SM. The metabolic syndrome: inflammation, diabetes mellitus, and cardiovascular disease. American Journal of Cardiology. 2006;97(2):3A–11A. doi: 10.1016/j.amjcard.2005.11.010. [DOI] [PubMed] [Google Scholar]
- 7.Lee S-J, Namkoong S, Kim Y-M, et al. Fractalkine stimulates angiogenesis by activating the Raf-1/MEK/ERK- and PI3K/Akt/eNOS-dependent signal pathways. American Journal of Physiology. 2006;291(6):H2836–H2846. doi: 10.1152/ajpheart.00113.2006. [DOI] [PubMed] [Google Scholar]
- 8.Maegdefessel L, Schlitt A, Pippig S, et al. Patients with insulin-dependent diabetes or coronary heart disease following rehabilitation express serum fractalkine levels similar to those in healthy control subjects. Vascular Health and Risk Management. 2009;5:849–857. doi: 10.2147/vhrm.s6829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.White GE, Tan TCC, John AE, Whatling C, McPheat WL, Greaves DR. Fractalkine has anti-apoptotic and proliferative effects on human vascular smooth muscle cells via epidermal growth factor receptor signalling. Cardiovascular Research. 2010;85(4):825–835. doi: 10.1093/cvr/cvp341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aoyama T, Inokuchi S, Brenner DA, Seki E. CX3CL1-CX3CR1 interaction prevents carbon tetrachloride-induced liver inflammation and fibrosis in mice. Hepatology. 2010;52(4):1390–1400. doi: 10.1002/hep.23795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cardona AE, Pioro EP, Sasse ME, et al. Control of microglial neurotoxicity by the fractalkine receptor. Nature Neuroscience. 2006;9(7):917–924. doi: 10.1038/nn1715. [DOI] [PubMed] [Google Scholar]
- 12.Catoire M, Mensink M, Kalkhoven E, Schrauwen P, Kersten S. Identification of human exercise-induced myokines using secretome analysis. Physiol Genomics. 2014 doi: 10.1152/physiolgenomics.00174.2013. [DOI] [PubMed] [Google Scholar]
- 13.Shah R, Hinkle CC, Ferguson JF, et al. Fractalkine is a novel human adipochemokine associated with type 2 diabetes. Diabetes. 2011;60(5):1512–1518. doi: 10.2337/db10-0956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bazan JF, Bacon KB, Hardiman G, et al. A new class of membrane-bound chemokine with a CX3C motif. Nature. 1997;385(6617):640–642. doi: 10.1038/385640a0. [DOI] [PubMed] [Google Scholar]
- 15.Imai T, Hieshima K, Haskell C, et al. Identification and molecular characterization of fractalkine receptor CX3CR1, which mediates both leukocyte migration and adhesion. Cell. 1997;91(4):521–530. doi: 10.1016/s0092-8674(00)80438-9. [DOI] [PubMed] [Google Scholar]
- 16.Lucas AD, Bursill C, Guzik TJ, Sadowski J, Channon KM, Greaves DR. Smooth muscle cells in human atherosclerotic plaques express the fractalkine receptor CX3CR1 and undergo chemotaxis to the CX 3C chemokine fractalkine (CX3CL1) Circulation. 2003;108(20):2498–2504. doi: 10.1161/01.CIR.0000097119.57756.EF. [DOI] [PubMed] [Google Scholar]
- 17.Garton KJ, Gough PJ, Blobel CP, et al. Tumor necrosis factor-α-converting enzyme (ADAM17) mediates the cleavage and shedding of fractalkine (CX3CL1) Journal of Biological Chemistry. 2001;276(41):37993–38001. doi: 10.1074/jbc.M106434200. [DOI] [PubMed] [Google Scholar]
- 18.Hundhausen C, Misztela D, Berkhout TA, et al. The disintegrin-like metalloproteinase ADAM10 is involved in constitutive cleavage of CX3CL1 (fractalkine) and regulates CX3CL1-mediated cell-cell adhesion. Blood. 2003;102(4):1186–1195. doi: 10.1182/blood-2002-12-3775. [DOI] [PubMed] [Google Scholar]
- 19.Ikejima H, Imanishi T, Tsujioka H, et al. Upregulation of fractalkine and its receptor, CX3CR1, is associated with coronary plaque rupture in patients with unstable angina pectoris. Circulation Journal. 2010;74(2):337–345. doi: 10.1253/circj.cj-09-0484. [DOI] [PubMed] [Google Scholar]
- 20.White GE, Greaves DR. Fractalkine: a survivor’s guide chemokines as antiapoptotic mediators. Arteriosclerosis, Thrombosis, and Vascular Biology. 2012;32(3):589–594. doi: 10.1161/ATVBAHA.111.237412. [DOI] [PubMed] [Google Scholar]
- 21.Matthews DR, Hosker JP, Rudenski AS. Homeostasis model assessment: insulin resistance and β-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28(7):412–419. doi: 10.1007/BF00280883. [DOI] [PubMed] [Google Scholar]
- 22.Chinese guidelines on prevention and treatment of dyslipidemia in adults. Zhonghua Xin Xue Guan Bing Za Zhi. 2007;35(5):390–419. [PubMed] [Google Scholar]
- 23.Després J-P, Lemieux I. Abdominal obesity and metabolic syndrome. Nature. 2006;444(7121):881–887. doi: 10.1038/nature05488. [DOI] [PubMed] [Google Scholar]
- 24.Mokdad AH, Bowman BA, Ford ES, Vinicor F, Marks JS, Koplan JP. The continuing epidemics of obesity and diabetes in the United States. Journal of the American Medical Association. 2001;286(10):1195–1200. doi: 10.1001/jama.286.10.1195. [DOI] [PubMed] [Google Scholar]
- 25.Mottillo S, Filion KB, Genest J, et al. The metabolic syndrome and cardiovascular risk: a systematic review and meta-analysis. Journal of the American College of Cardiology. 2010;56(14):1113–1132. doi: 10.1016/j.jacc.2010.05.034. [DOI] [PubMed] [Google Scholar]
- 26.Kishida K, Funahashi T, Matsuzawa Y, Shimomura I. Visceral adiposity as a target for the management of the metabolic syndrome. Annals of Medicine. 2012;44(3):233–241. doi: 10.3109/07853890.2011.564202. [DOI] [PubMed] [Google Scholar]
- 27.Matsuzawa Y, Funahashi T, Nakamura T. The concept of metabolic syndrome: contribution of visceral fat accumulation and its molecular mechanism. Journal of Atherosclerosis and Thrombosis. 2011;18(8):629–639. doi: 10.5551/jat.7922. [DOI] [PubMed] [Google Scholar]
- 28.Baranova A, Collantes R, Gowder SJ, et al. Obesity-related differential gene expression in the visceral adipose tissue. Obesity Surgery. 2005;15(6):758–765. doi: 10.1381/0960892054222876. [DOI] [PubMed] [Google Scholar]
- 29.Funahashi T, Matsuzawa Y. Metabolic syndrome: clinical concept and molecular basis. Annals of Medicine. 2007;39(7):482–494. doi: 10.1080/07853890701491026. [DOI] [PubMed] [Google Scholar]
- 30.Franco L, Williams FM, Trofimov S, Surdulescu G, Spector T, Livshits G. Elevated plasma fractalkine levels are associated with higher levels of IL-6, Apo-B, LDL-C and insulin, but not with body composition in a large female twin sample. Metabolism. 2013;62(8):1081–1087. doi: 10.1016/j.metabol.2013.02.001. [DOI] [PubMed] [Google Scholar]
- 31.Breslin WL, Johnston CA, Strohacker K, et al. Obese Mexican American children have elevated MCP-1, TNF-α, monocyte concentration, and dyslipidemia. Pediatrics. 2012;129(5):e1180–e1186. doi: 10.1542/peds.2011-2477. [DOI] [PubMed] [Google Scholar]
- 32.Njerve IU, Pettersen AA, Opstad TB, Arnesen H, Seljeflot I. Fractalkine and its receptor (CX3CR1) in patients with stable coronary artery disease and diabetes mellitus. Metabolic Syndrome and Related Disorders. 2012;10(6):400–406. doi: 10.1089/met.2012.0052. [DOI] [PubMed] [Google Scholar]
- 33.Damås JK, Boullier A, Wæhre T, et al. Expression of fractalkine (CX3CL1) and its receptor, CX3CR1, is elevated in coronary artery disease and is reduced during statin therapy. Arteriosclerosis, Thrombosis, and Vascular Biology. 2005;25(12):2567–2572. doi: 10.1161/01.ATV.0000190672.36490.7b. [DOI] [PubMed] [Google Scholar]
- 34.McDermott DH, Halcox JPJ, Schenke WH, et al. Association between polymorphism in the chemokine receptor CX3CR1 and coronary vascular endothelial dysfunction and atherosclerosis. Circulation Research. 2001;89(5):401–407. doi: 10.1161/hh1701.095642. [DOI] [PubMed] [Google Scholar]
- 35.Meng L, Park J, Cai Q, Lanting L, Reddy MA, Natarajan R. Diabetic conditions promote binding of monocytes to vascular smooth muscle cells and their subsequent differentiation. American Journal of Physiology. 2010;298(3):H736–H745. doi: 10.1152/ajpheart.00935.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Dragomir E, Manduteanu I, Calin M, et al. High glucose conditions induce upregulation of fractalkine and monocyte chemotactic protein-1 in human smooth muscle cells. Thrombosis and Haemostasis. 2008;100(6):1155–1165. [PubMed] [Google Scholar]
- 37.Garcia GE, Xia Y, Chen S, et al. NF-κB-dependent fractalkine induction in rat aortic endothelial cells stimulated by IL-1β, TNF-α, and LPS. Journal of Leukocyte Biology. 2000;67(4):577–584. doi: 10.1002/jlb.67.4.577. [DOI] [PubMed] [Google Scholar]
- 38.Ludwig A, Berkhout T, Moores K, Groot P, Chapman G. Fractalkine is expressed by smooth muscle cells in response to IFN-γ and TNF-α and is modulated by metalloproteinase activity. Journal of Immunology. 2002;168(2):604–612. doi: 10.4049/jimmunol.168.2.604. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary table 1. Baseline Characteristics of Participants Completely Investigated According to the Presence or Absence of the Mets (n=459).


