Abstract
Background
Body image can be affected by bodily experiences extending beyond physical appearance. This study evaluated associations among speech, eating, and body image concerns for surgically treated patients with oral cavity, midface, and cutaneous cancers of the head and neck.
Methods
Using a cross-sectional design, 280 participants completed the Body Image Scale, a survey evaluating disease-specific body image issues, and the Functional Assessment of Cancer Therapy Scale – General.
Results
Participants with speech and eating concerns reported the highest levels of body image/appearance dissatisfaction compared to those without such concerns. This group also reported greater cognitive and behavioral difficulties associated with body image concerns and significantly higher levels of interest in psychosocial interventions to address appearance-related difficulties compared to all other participants.
Conclusions
Findings point to the need for more comprehensive psychosocial care for head and neck patients with speech and eating difficulties, which extends beyond functional rehabilitation.
Keywords: body image, quality of life, speech, eating, swallowing
Background
Surgical resection remains a primary treatment for patients with head and neck cancer especially those with oral cavity, midfacial and cutaneous malignancies.1,2 These patients often experience psychological and physiological difficulties as the illness and its treatment can significantly alter appearance and affect functionally critical structures. Although there can be wide variation in clinical presentation and treatment-specific issues based on disease characteristics, an important commonality shared by patients surgically treated for head and neck cancer is that they experience some degree of physical changes to a highly visible and socially significant part of their body (i.e., their face) due to cancer. Common concerns reported by individuals with head and neck cancers involve bodily changes they will undergo related tospeech, swallowing, eating, dry mouth, and appearance changes.3 All of these changes have the potential to influence body image and ultimately affect a patient’s quality of life (QOL).
Speaking abilities have been shown to be the single most important contributor to health-related quality of life after treatment for head and neck cancer.4 Swallowing function also substantially affects patients’ well-being, and ranked second in importance among contributors to QOL after treatment in a multi-center study.4 Moreover, speech and swallowing concerns appear to be highly prevalent for surgically treated patients with head and neck cancer. A recent systematic review suggests that deviant speech characteristics (e.g., abnormal articulation) and impaired swallowing efficiency were reported for a majority of surgically treated patients with advanced stage oral cancer.5 Surgical resection of midfacial or cutaneous cancers can also have adverse effects on the articulation of labial sounds and speech resonance, but these cases are not often reported in the literature.6 Patients with oral cavity malignancies are more likely than others to experience eating-related impairments such as pain, taste loss, and inability to open the mouth, along with problems associated with mastication and oral transit.7 However, patients with midfacial or cutaneous cancers can also experience difficulties related to labial incompetence, facial paresis, and oronasal separation6,8 which can affect the ability to keep food in the mouth during mastication and impede food transit to the pharynx.
The purpose of this study was to evaluate associations among speech, eating, and body image concerns for patients undergoing surgical treatment for head and neck cancer. Our sample was comprised of patients with oral cavity, midface, and cutaneous cancers of the head and neck. As far as we are aware, there has been no investigation into the connection between these functional concerns and body image outcomes among patients with these types of head and neck cancers. This relationship is of interest when one considers body image as a multifaceted concept involving perceptions, thoughts, and feelings about the entire body and its functioning.9 Body image is recognized to extend beyond one’s view of his or her physical appearance and can be affected by bodily sensations and other aspects of physical functioning.10 Another fundamental component of body image is its inherently subjective nature.10 A patient’s body image does not necessarily reflect the objective reality of the body.
Cash11 and White12 have developed models of body image development and distress that have been previously applied and discussed within the oncology setting.13 These models highlight the importance of examining the manner in which one evaluates his/her body image (satisfaction/dissatisfaction) and discuss related cognitions, behaviors, and emotions. This study considers a wide range of body-related concerns that patients with head and neck cancer experience before, during, and after treatment. The bodily alterations these patients encounter can be numerous and a significant source of psychological distress. We were interested in examining the manner in which specific types of body-related concerns (i.e., those tied to speech and swallowing) were associated with body image outcomes.
Methods
This study involves secondary analysis of a larger project designed to evaluate body image, QOL, and satisfaction with care for a broad range of surgically treated patients with head and neck cancer who are at risk for experiencing facial disfigurement.14 We were interested in examining whether functional concerns tied to speech and eating were associated with body image outcomes. This included evaluating speech and eating concerns in isolation versus combined speech and eating concerns. We divided our sample into three groups: a) those who reported a wide range of body-related concerns that included speech and eating, b) those who denied speech and eating concerns but reported other body-related concerns largely tied to physical appearance, and c) those who denied any body-related concern. Our primary outcomes of interest included body image/appearance dissatisfaction scores, endorsement of cognitive/behavioral difficulties related to body image, and interest in psychosocial intervention. We were also interested in evaluating the associations between different types of body-related concerns and QOL.
Sample
Our sample included 280 patients who have either had or were about to undergo surgical treatment for head and neck cancer at the University of Texas MD Anderson Cancer Center. We used a cross-sectional design to obtain data from a broad array of surgically treated patients with head and neck cancer at different time points relative to the initiation of treatment. Due to the goals of our larger project, participants were considered for inclusion based on their primary cancer site. This study included patients receiving surgical treatment for oral cavity cancer, cutaneous cancer of the head and neck, or other cancer of the midface. Patients with cancers occurring in the oropharynx or larynx, which are more typically treated with radiation and/or chemotherapy as a primary treatment modality, were not considered for inclusion. Patients were also excluded if they were less than 18 years of age, did not speak English, had a significant preexisting facial disfigurement from a previous trauma or congenital defect, a diagnosis of a serious mental illness involving formal thought disorder, or cognitive impairment.
Procedure
The study protocol was approved by the Institutional Review Board. After providing informed consent, participants completed a questionnaire packet that included the Body Image Scale (BIS), a survey designed for the study, and the Functional Assessment of Cancer Therapy Scale –General Version (FACT-G). Additional medical and demographic information were obtained from a review of the patient’s medical chart.
Measures
The BIS is a 10-item scale assessing body image/appearance dissatisfaction designed to be applicable for patients with any cancer site and form of therapy.15 This instrument inquires, for example, about the degree to which patients feel self-conscious about their appearance, whether they feel less physically attractive as a result of their disease or treatment, or whether they are dissatisfied with the appearance of their scar. The BIS has only been previously validated with breast cancer patients, but was used in another study with oral cancer patients where it demonstrated adequate internal consistency and correlated highly with other measures of body image.16 Cronbach’s alpha for our sample on the BIS was 0.91
The survey designed for the study initially inquired about 15 types of body-related changes relevant to head and neck cancer and asked whether participants were concerned or embarrassed by these difficulties either currently or at any point following diagnosis/treatment (see Table 1). Response options involved endorsing presence or absence of a concern. Additional information was gathered on cognitive/behavioral difficulties associated with body-related concerns and interest in psychosocial intervention to help patients cope with body image difficulties. Outcomes on these variables were dichotomized (presence/absence of difficulty, interest/no interest in intervention). Table 1 presents specific items from the survey that was used as part of this secondary data analysis. Additional data from this survey and further details about its content are presented elsewhere.14
Table 1.
Survey Questions
Presence of Body-Related Concerns
|
Cognitive/Behavioral Difficulties Associated with Body-Related Concerns
|
Interest in Psychosocial Care/Intervention
|
Note.
Participants endorsing either of these two items were placed in speech/eating concerns group (SE group). Those endorsing any other concern item were placed in the group that denied speech and eating issues, but reported other types of concerns largely tied to appearance (AC group).
Participants also completed the Functional Assessment of Cancer Therapy-General (FACT-G), a validated and widely used measure of QOL designed to be used with patients with any form of cancer.17 The FACT-G has also been validated with individuals with other chronic illness conditions and in the general population. This 27-item questionnaire is comprised of the following 4 subscales: physical well-being, social/family well-being, emotional well-being, and functional well-being. Cronbach’s alpha for our sample on the FACT-G (using all individual items across the 4 subscales) was 0.91
Data Analysis
Our primary group of interest was participants who reported body-related concerns involving speech and eating. (“SE” group = speech/eating concerns group). Based on previous literature we further subdivided the SE group into those reporting a single functional concern (speech or eating) versus those reporting both functional concerns (speech and eating). The second group included participants who denied speech and eating concerns but reported other types of body-related concerns, which were largely tied to physical appearance (“AC” group = appearance-only concerns group). The third group included participants who denied the presence of any of the body-related concerns listed (“NC” group = no concerns group). We performed descriptive analyses on the entire sample as well as the three different groups of participants. ANCOVA models were used to conduct between-group comparisons for the BIS and FACT-G. These models controlled for the effects of age, gender, type of cancer, and time point in treatment. In these analyses, we grouped participants on the basis of concerns they endorsed at the time of the evaluation (i.e., “current” concerns). Prior to creating the ANCOVA models, a 2-sample t-test was performed for each outcome to determine if there were significant differences between our two SE concerns subgroups (single vs. combined). If there were no differences, these groups were collapsed into one larger group in the ANCOVA. We used contrasts to look for differences between concerns groups when an ANCOVA was statistically significant, and we adjusted for multiple comparisons using Bonferroni adjustments.
A logistic regression analysis was used to evaluate group differences on survey items related to cognitive/behavioral difficulties. The model used the NC group as the reference group, and controlled for age, gender, cancer type, and time point in treatment. A fisher’s exact test was performed to evaluate group differences on the survey item related to interest in psychosocial intervention18. If the Fisher’s exact test found a difference between any of the three groups, we then examined each possible pairwise comparison using a Fisher’s exact test to determine which group differed. The definition of a statistical significance for these pairwise comparisons was revised to p < 0.017 to account for three sets of pairwise comparisons for each item.
Results
Demographic and Other Key Participant Characteristics
The sample was comprised of 280 patients, the majority of whom were male (63.9%). Participants ranged in age from 18 to 91, with a mean age of 59.9 (SD = 15.11). Regarding race, 88% identified themselves as Caucasian, 4% as African American, 3% as Asian, and 5% as other. Approximately 8% of the sample identified themselves as being Hispanic. The majority of participants were married or in a committed relationship (79%), and were educated beyond high school (63%).
Participants with oral cavity cancer (33.5%) had tumors largely in the retromolar trigone, gingiva, hard palate, tongue, alveolar ridge, floor of mouth, buccal mucosa, and tongue. Participants classified with cutaneous cancer of the head and neck (41.4%) had tumors largely in the cheek, forehead, nose, ear, eyelid, and temple. Participants with other midface cancers (25%) mainly had tumors in the nasal cavity, maxilla, mandible, and eye. Our sample was comprised of patients along the cancer treatment trajectory. Time since diagnosis ranged from less than one month to greater than 5 years. Approximately 18% of our sample had not yet undergone surgical treatment, 41% had surgery within the last year, and 41% had surgery greater than a year ago. Tumor size and extent of illness were variable as well. Patients were included with all T-classifications. Approximately 22% of the participants had received chemotherapy, 46% had received radiation treatment, and 19% had undergone plastic/reconstructive surgery. Only 41% of the sample indicated they had completed treatment for their head and neck cancer. Additional information on the sample are reported elsewhere.14
Descriptive Data for Body-Related Concerns
Table 2 presents data on participant groupings based on current body-related concerns. Approximately one-third of participants (N = 86) reported concerns that involved speech and/or eating. Not surprisingly, the majority of patients in the speech/eating concerns group (SE) had cancer in the oral cavity (54%), 30% of the SE group was comprised of patients with cancers of the midface, and the remaining 16% were patients with cutaneous cancers. Patients across the cancer treatment continuum reported current concerns related to speech and eating. There were 46 participants who reported a single functional concern (speech or eating) and there were 40 participants who reported combined functional concerns (speech and eating). Nearly ¼ of participants (23.6%) reported body image concerns tied more exclusively to physical appearance. The top appearance-related concern involved scarring/disfigurement. The majority of participants in the AC group had cutaneous cancers of the head and neck; however, this group also included patients with oral cavity and other midface cancers. Relatively few patients in the AC group (12%) reported appearance-based concerns at the preoperative time point.
Table 2.
Participant Groupings Based on Current Body-Related Concerns
| Total Sample N (percent) | Cancer Type | Time Point In Treatment | |||||
|---|---|---|---|---|---|---|---|
| Oral Cavity | Cutaneous | Other Midface | Before | <1 year | > 1 year | ||
| Speech/Eating | 86 (30.7) | 46 (53.5) | 14 (16.3) | 26 (30.2) | 18 (20.9) | 34 (39.5) | 34 (39.5) |
| Appearance Only | 66 (23.6) | 14 (21.2) | 38 (57.6) | 14 (21.2) | 8 (12.1) | 29 (43.9) | 29 (43.9) |
| No Concerns | 120 (42.9) | 31 (25.8) | 62 (51.7) | 27 (22.5) | 20 (16.7) | 51 (42.5) | 49 (40.8) |
Note. All values are presented as frequency (percent). Percentages calculated based on number of participants responding to relevant survey data (N = 272).
Group Differences in BIS Scores
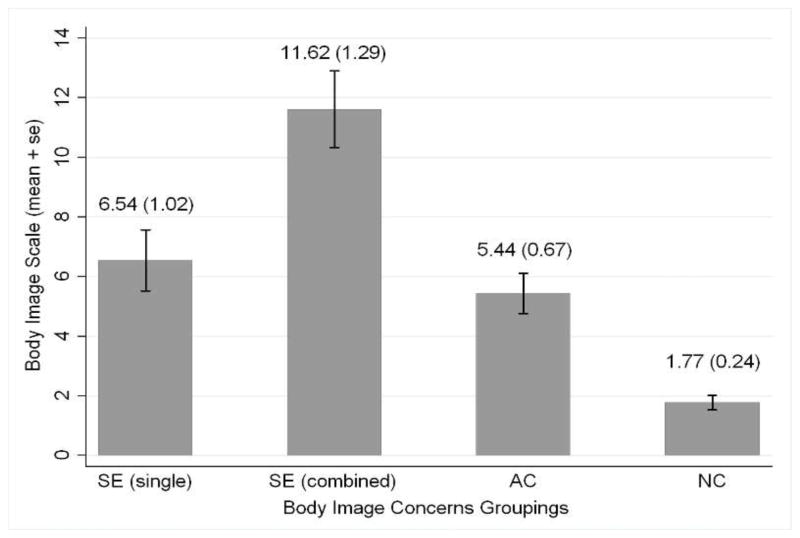
Scores on the BIS ranged from 0–30 with an overall mean of 4.93 (SD = 6.21). Figure 1 illustrates significant group differences on the Body Image Scale (BIS) based on the type of current body-related concerns reported. Note that higher scores on the BIS reflect higher levels of body image/appearance dissatisfaction. The overall ANCOVA model was significant (p < 0.0001) and involved a 4-way comparison (SE single, SE combined, AC, NC groups). This analysis controlled for the effects of age, gender, cancer type and time point in treatment. Pairwise t-tests revealed that the SE combined group (i.e. patients reporting both speech and eating concerns) had significantly higher levels of appearance dissatisfaction compared to all other groups (i.e., all p’s <0.0001). Comparable levels of appearance dissatisfaction were found between the SE single group and the AC group.
Figure 1. Body Image/Appearance Dissatisfaction Based on Current Body-Related Concerns.
Note: SE (single) = Speech/Eating Concerns Group with single functional concern (speech or eating); SE (combined) = Speech/Eating Concerns Group with combined functional concerns (speech and eating); AC = appearance-based only concerns group; NC = no bodily concerns group. All group comparison significant at p < 0.0001 except SE (single) versus AC (P = 0.089). This analysis controlled for the effects of age, gender, cancer type and time point in treatment.
Group Differences in Survey Scores
Survey findings revealed a high prevalence of body-related concerns across the entire sample. Nearly 75% of participants reported they were concerned or embarrassed by bodily changes at some point following diagnosis with 56% reporting such difficulties currently. The average number of current body-related concerns in the speech/eating concerns group (SE group) was much higher compared to the appearance-only group (AC group) (M = 4.19 vs. 1.83), due to the fact that those in the SE group reported functional as well as appearance-based concerns. When considering individual body-related concerns, the SE group endorsed each concern at similar or higher levels compared to the AC group. No significant differences were found between the SE and AC groups regarding the presence of current body-related concerns involving swelling, skin discoloration, weight loss, hair loss, removal of nose, scarring/disfigurement, weight gain, removal of eye, or removal of ear. It is not surprising that those in the SE group had significantly higher rates of body-related concerns involving drooling (p < 0.0001) and lack of teeth (p < 0.0001) compared to the AC group.
The endorsement of cognitive and behavioral difficulties was significantly associated with the presence of body-related concerns reported following diagnosis (see Table 3). The SE and AC groups reported significantly higher rates of preoccupation with appearance and reassurance seeking compared to the NC group. The SE group reported the highest levels of social avoidance, whether due to appearance, speech or eating. The SE group also reported significantly increased time spent grooming compared to the NC group. There were no group differences with respect to avoidance of grooming, and this item was endorsed at relatively low levels compared to other items.
Table 3.
Cognitive/Behavioral Difficulties Based on Body-Related Concerns Following Diagnosis
| P-Values | |||||||
|---|---|---|---|---|---|---|---|
| SE group (N =86) | AC group (N = 66) | NC group (N = 120) | Comparison of SE, AC and NC Groups | SE v. AC | SE v. NC | AC v. NC | |
| Frequent thoughts about appearance changes | 63 (75.00%) | 42 (64.62%) | 37 (31.36%) | <0.0001 | 0.1305 | < 0.0001 | < 0.0001 |
| Avoidance of social activities due to appearance | 38 (45.24%) | 15 (27.69%) | 16 (13.56%) | <0.0001 | 0.0144 | < 0.0001 | 0.0237 |
| Avoidance of social activities due to speech | 41 (48.81%) | 4 (6.15%) | 13 (11.02%) | <0.0001 | < 0.0001 | < 0.0001 | 0.3322 |
| Avoidance of social activities due to eating | 39 (46.43%) | 11 (16.92%) | 17 (14.41%) | 0.0003 | 0.0085 | < 0.0001 | 0.5556 |
| Increase time engaged in grooming | 25 (29.76%) | 14 (21.54%) | 15 (12.71%) | 0.0203 | 0.3095 | 0.0057 | 0.1182 |
| Avoidance of grooming | 11 (13.10%) | 5 (7.69%) | 6 (5.08%) | 0.2318 | 0.4147 | 0.0878 | 0.4659 |
| Reassurance seeking | 27 (32.14%) | 20 (30.77%) | 15 (12.71%) | 0.0007 | 0.5697 | 0.0004 | 0.0032 |
Note. SE = speaking/eating concerns, AC = appearance-based only concerns, NC = no bodily concerns. Percentages were based on the total number of people responding to that item which did not always equal the total N for the group. Comparisons conducted with logistic regression model using NC as the reference group. A contrast was used to test for differences between SE and AC.
Regarding overall interest in psychosocial interventions to address appearance-related concerns, 34% of the entire sample indicated they would like this help now or would have liked this help previously. Most people reported a preference for obtaining written materials over other forms of intervention. Participants in the SE group were significantly more likely to report intervention interest compared to those in the AC (p = 0.0015) and NC groups (p < 0.0001). Of those interested in receiving resources to cope with appearance-related changes, 62.6% were in the SE group, 27.7% were in the AC group, and 9.6% were in the NC group. There were no group differences regarding the optimal time to offer an intervention.
Group Differences in QOL scores
Total FACT-G scores ranged from 36–108 with an overall mean of 85.76 (SD= 16.5). Table 4 demonstrates that the presence of current body-related concerns was significantly associated with FACT-G scores. In addition, there were significant group differences on the subscale of the FACT-G based on the type of body-related concerns reported. These analyses controlled for the effects of gender, age, cancer type, and time point in treatment. Note that lower scores on the FACT-G subscales are reflective of poorer QOL. The SE concerns subgroups (single vs. combined) significantly differed only for physical well-being, with scores reflecting worse outcomes for the SE combined group versus the SE single group (p = 0.0294). The SE single group demonstrated worse scores on physical well-being compared to the NC group (p = 0.0040) but did not differ from the AC group (p = 0.6471). The SE combined group demonstrated worse scores on physical well-being compared to the AC group (p = 0.0070) and the NC group (p < 0.0001). The SE concerns subgroups did not significantly differ from each other on any of the other main subscales (social well-being, emotional well-being, functional well-being), thus our ANCOVA models for these outcomes involved a 3-way comparison (SE, AC, NC groups). For the social well-being subscale, the SE group demonstrated significantly worse QOL compared to the AC and NC groups. For the emotional and functional-well being subscales, the SE and AC groups demonstrated comparable QOL scores, which were significantly worse compared to the NC group.
Table 4.
Quality of Life Scores (FACT-G) Based on Current Body-Related Concerns
| SE group | AC group | NC group | p value | |
|---|---|---|---|---|
| FACT-G physical | 20.21 (6.88) | 22.83 (5.58) | 25.02 (4.59) | <0.0001 |
| FACT-G social | 21.91 (5.44) | 23.22 (5.03) | 23.93 (4.99) | 0.0273 |
| FACT-G emotional | 16.88 (4.39) | 18.84 (5.29) | 20.15 (4.69) | 0.0003 |
| FACT-G functional | 18.09 (6.72) | 19.64 (6.33) | 23.25 (5.62) | <0.0001 |
Note. FACT-G = Functional Assessment of Cancer Therapy Scale- General Version. SE = speech/eating concerns group, AC = appearance-only concerns group, NC = no bodily concerns group. P values are
Discussion
This study offers new insight regarding associations between speech, eating, and body image concerns for patients with cancers affecting the head and neck. Our findings highlight that body image can be affected by a broad range of body-related experiences. In our sample, we found that patients reporting speech and eating concerns experience body image difficulties at least equivalent to or even more so that patients with body-related concerns tied more exclusively to physical appearance. Patients with speech and eating concerns demonstrated significantly higher levels of appearance dissatisfaction on the BIS compared to those with appearance-only based concerns. In addition, we found that those with speech and eating concerns were significantly more likely to be avoidant of social activities and to report interest in psychosocial interventions to address appearance-related difficulties. These findings suggest the importance of providing comprehensive psychosocial care to patients with speech and eating concerns that extend beyond functional rehabilitation.
Additional findings support previous research on the association between speech and eating concerns and QOL in this population. We found that participants with any type of body-related concern (whether tied to speech, eating or physical appearance) had worse QOL outcomes related to physical well-being, functional well-being, social well-being and emotional well-being. This is relevant because the QOL outcomes we incorporated were considered to be more broadly based and not specific to head and neck cancer. Thus, we are able to demonstrate links between head and neck-specific body-related concerns identified on our survey and more global aspects of functioning.
In this study we explored body image and psychosocial functioning in patients with oral cavity cancer, which has been the focus of much previous research, as well as among patients with other cancers involving cutaneous and midface regions where psychosocial issues have not been given much attention in the literature. We were surprised to find that such a large percentage of participants (46%) endorsing speech and eating concerns was comprised of patients with cutaneous and other midface cancers. In many of these cases, participants reported having cancer affecting their cheek, lip, ear, or inside their nasal cavity which, depending on the extent of their tumor and surgical treatment, could ultimately affect speech production, intelligibility or sound quality, as well as swallowing function. As reflected by our study speech and eating concerns are reported by a broad array of surgically treated head and neck cancer patients, and are clearly not limited to patients with cancer in the oral cavity.
Since we included participants prior to, during, and after treatment, we were also able to examine the presence of body-related concerns and body image difficulties across the cancer-treatment trajectory. We found that these issues were not limited to the immediate postoperative phase or the first year following treatment, but were present preoperatively and extended well into the period of cancer survivorship. We note that body-related concerns were not evenly distributed across the continuum of cancer treatment. It is not surprising that these concerns were more prevalent following treatment. Preoperative body-related concerns may be associated with tumor-related changes but more likely reflect anxiety associated with impending treatment. Body-related concerns and body image difficulties that persist into survivorship likely reflect long lasting adjustment issues with bodily changes due to cancer and its treatment, which can be further exacerbated by late effects of concomitant therapies.
This study examined all psychosocial outcomes, including concerns related to speech and eating, from the perception of the patient using self-report instruments. The patient’s subjective experience of bodily concerns is an important component and one of the defining features of body image.9,13 This study further highlights and reinforces the notion that body image can be affected by a broad range of body-related experiences. In our sample, we found that patients reporting speech and eating concerns experience body image difficulties at least equivalent to or even more so than patients with body-related concerns tied more exclusively to physical appearance. It is particularly surprising that patients with speech and eating concerns demonstrated significantly worse scores on the BIS compared to those with appearance-based only concerns considering that the items on the BIS relate almost entirely to physical appearance. As we have mentioned, however, patients in the speech and eating concerns group did endorse appearance-related concerns alongside these functional concerns. We must consider here that the SE group as a whole experienced a greater number of total body image concerns compared to those in the AC group. This suggests that there may be an additive effect of combining functional concerns with appearance-related concerns that contributes to worse body image outcomes. Future research would benefit from evaluating the severity, frequency, and intensity of these concerns rather than only their presence or absence.
Findings from this study have a number of clinical implications. The majority of patients (75%) reported experiencing concerns or embarrassment about body-related changes at some point following diagnosis. Body image therapy delivered by a mental health specialist may be particularly relevant and useful for any patient experiencing difficulty coping with bodily changes resulting from head and neck cancer and its treatment. Patients with speech and eating concerns are often referred for functional rehabilitation; which is a critical part of their multidisciplinary treatment. This study suggests the importance of attending to body image difficulties that cannot be fully addressed with functional rehabilitation. For instance, body image specialists can assist patients with speech and swallowing impairment in reducing preoccupation about their functional difficulties and managing depression and anxiety tied to social situations. They can also promote adaptive coping strategies for dealing with body image concerns that may also include distress involving disfigurement and other appearance-related changes.
We acknowledge limitations of this study including the cross-sectional design, heterogeneity of the sample with respect to cancer type and time since diagnosis, limited racial and ethnic diversity of the sample, and exclusion of laryngeal cancer patients. Patients with laryngeal cancer were not included in the larger body image study because it focused on patients with tumors concentrated in the facial region that typically undergo surgery as a primary treatment modality. Clearly, these findings need to be explored with laryngeal patients as well as other groups of head and neck patients not included here. There are additional limitations with respect to some of the instruments used in this study. The survey we designed is not a validated instrument, but was created for a larger study to obtain descriptive information about disease-specific body-related concerns and associated body image difficulties.14 The BIS has not been widely used with head and neck patients, although it has a distinct advantage as one of the only body image tools available focusing on satisfaction with appearance changes resulting from disease and treatment. There are no clinical cut-offs established for the BIS to determine severity of body image concerns.
Information gleaned from this study is believed to provide a starting point for further investigation to understand the association between speech, eating and body image concerns of surgically treated patients with head and neck cancer. Longitudinal work is needed to evaluate and determine causative factors. Moreover, there are additional medical- and treatment-related variables that need to be considered in larger scale studies. We were unable to control for the effects of tumor stage in this study due to the heterogeneity of the sample and inclusion of patients with cutaneous cancers who can be staged differently from other head and neck patients depending on their cancer type. Additionally, we did not examine for the effects of comorbid conditions. Future research is needed to elucidate these effects and to determine how to better meet the psychosocial needs of this population.
References
- 1.Funk GF, Karnell LH, Robinson RA, Zhen WK, Trask DK, Hoffman HT. Presentation, treatment, and outcome of oral cavity cancer: a National Cancer Data Base report. Head Neck. 2002 Feb;24(2):165–180. doi: 10.1002/hed.10004. [DOI] [PubMed] [Google Scholar]
- 2.Cooper JS, Porter K, Mallin K, et al. National Cancer Database report on cancer of the head and neck: 10-year update. Head Neck. 2009 Jun;31(6):748–758. doi: 10.1002/hed.21022. [DOI] [PubMed] [Google Scholar]
- 3.Martino R, Ringash J. Evaluation of quality of life and organ function in head and neck squamous cell carcinoma. Hematol Oncol Clin North Am. 2008 Dec;22(6):1239–1256. x. doi: 10.1016/j.hoc.2008.08.011. [DOI] [PubMed] [Google Scholar]
- 4.Radford K, Woods H, Lowe D, Rogers SN. A UK multi-centre pilot study of speech and swallowing outcomes following head and neck cancer. Clin Otolaryngol Allied Sci. 2004 Aug;29(4):376–381. doi: 10.1111/j.1365-2273.2004.00823.x. [DOI] [PubMed] [Google Scholar]
- 5.Kreeft AM, van der Molen L, Hilgers FJ, Balm AJ. Speech and swallowing after surgical treatment of advanced oral and oropharyngeal carcinoma: a systematic review of the literature. Eur Arch Otorhinolaryngol. 2009 Nov;266(11):1687–1698. doi: 10.1007/s00405-009-1089-2. [DOI] [PubMed] [Google Scholar]
- 6.Denewer AD, Setit AE, Hussein OA, Aly OF. Functinal and aesthetic outcome of reconstruction of large oro-facial defects involving the lip after tumor resection. J Egypt Natl Canc Inst. 2006 Mar;18(1):61–66. [PubMed] [Google Scholar]
- 7.Aplak B, Malcok M, Gelecek N, Sen M. Quality of life of Turkish patients with head and neck cancer. Turkish Journal of Cancer. 2007;37(4):129–136. [Google Scholar]
- 8.Andrades P, Rosenthal EL, Carroll WR, Baranano CF, Peters GE. Zygomatic-maxillary buttress reconstruction of midface defects with the osteocutaneous radial forearm free flap. Head Neck. 2008 Oct;30(10):1295–1302. doi: 10.1002/hed.20874. [DOI] [PubMed] [Google Scholar]
- 9.Pruzinsky T. Social and psychological effects of facial disfigurement: Quality of life, body image and surgical reconstruction. In: Weber RW, Goepfert H, Miller MJ, editors. Basal and Squamous Cell Carcinomas Skin Cancers of the Head and Neck. Philadelphia, PA: Williams & Wilkins; 1996. pp. 357–362. [Google Scholar]
- 10.Pruzinsky T. Enhancing quality of life in medical populations: A vision for body image assessment and rehabilitation as standards of care. Body Image: An International Journal of Research. 2004;1(1):71–81. doi: 10.1016/S1740-1445(03)00010-X. [DOI] [PubMed] [Google Scholar]
- 11.Cash TF, Pruzinsky T. Body image: A handbook of theory, research, & clinical practice. New York: The Guilford Press; 2002. [Google Scholar]
- 12.White CA. Body image dimensions and cancer: a heuristic cognitive behavioural model. Psychooncology. 2000 May-Jun;9(3):183–192. doi: 10.1002/1099-1611(200005/06)9:3<183::aid-pon446>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 13.Fingeret MC. Body image and disfigurement. In: Duffy J, Valentine A, editors. M. D. Anderson Manual of Psychosocial Oncology. New York: McGraw Hill; 2010. pp. 271–288. [Google Scholar]
- 14.Fingeret MC, Yuan Y, Urbauer D, Weston J, Nipomnick S, Weber RS. The nature and extent of body image concerns among surgically treated patients with head and neck cancer. Psycho-Oncology. doi: 10.1002/pon.1990. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hopwood P, Fletcher I, Lee A, Al Ghazal S. A body image scale for use with cancer patients. Eur J Cancer. 2001 Jan;37(2):189–197. doi: 10.1016/s0959-8049(00)00353-1. [DOI] [PubMed] [Google Scholar]
- 16.Fingeret MC, Vidrine DJ, Reece GP, Gillenwater AM, Gritz ER. Multidimensional analysis of body image concerns among newly diagnosed patients with oral cavity cancer. Head & Neck. 2010;32(3):301–309. doi: 10.1002/hed.21181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cella DF, Tulsky DS, Gray G, et al. The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. J Clin Oncol. 1993 Mar;11(3):570–579. doi: 10.1200/JCO.1993.11.3.570. [DOI] [PubMed] [Google Scholar]
- 18.Fisher RA. On the interpretation of χ2 from contingency tables, and the calculation of P. Journal of the Royal Statistical Society. 1922;85(1):87–94. [Google Scholar]