Abstract
Introduction
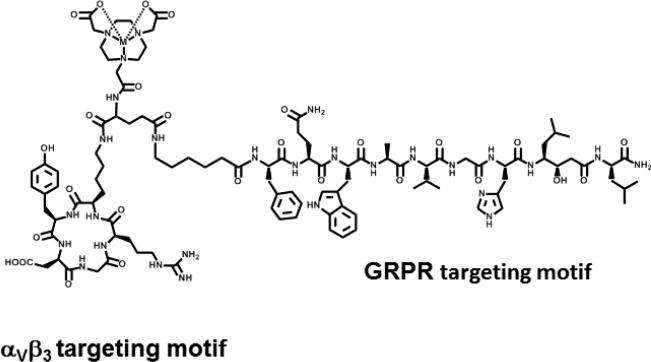
In the present study, we describe a 64Cu-radiolabeled heterodimeric peptide conjugate for dual αvβ3/GRPr (αvβ3 integrin/gastrin releasing peptide receptor) targeting of the form [RGD-Glu-[64Cu-NO2A]-6-Ahx-RM2] (RGD: the amino acid sequence [Arg-Gly-Asp], a nonregulatory peptide used for αvβ3 integrin receptor targeting; Glu: glutamic acid; NO2A: 1,4,7-triazacyclononane-1,4-diacetic acid; 6-Ahx: 6-amino hexanoic acid; and RM2: (D-Phe-Gln-Trp-Ala-Val-Gly-His-Sta-Leu-NH2), an antagonist analogue of bombesin (BBN) peptide used for GRPr targeting).
Methods
[RGD-Glu-6Ahx-RM2] was conjugated to a NOTA (1,4,7-triazacyclononane-1,4,7-triacetic acid) complexing agent to produce [RGD-Glu-[NO2A]-6-Ahx-RM2], which was purified by reversed-phase high-performance liquid chromatography (RPHPLC) and characterized by electrospray ionization–mass spectrometry (ESI-MS). Radiolabeling of the conjugate with 64Cu produced [RGD-Glu-[64Cu-NO2A]-6-Ahx-RM2] in high radiochemical yield (≥95%). In vivo behavior of the radiolabeled peptide conjugate was investigated in normal CF-1 mice and in the PC-3 human prostate cancer experimental model.
Results
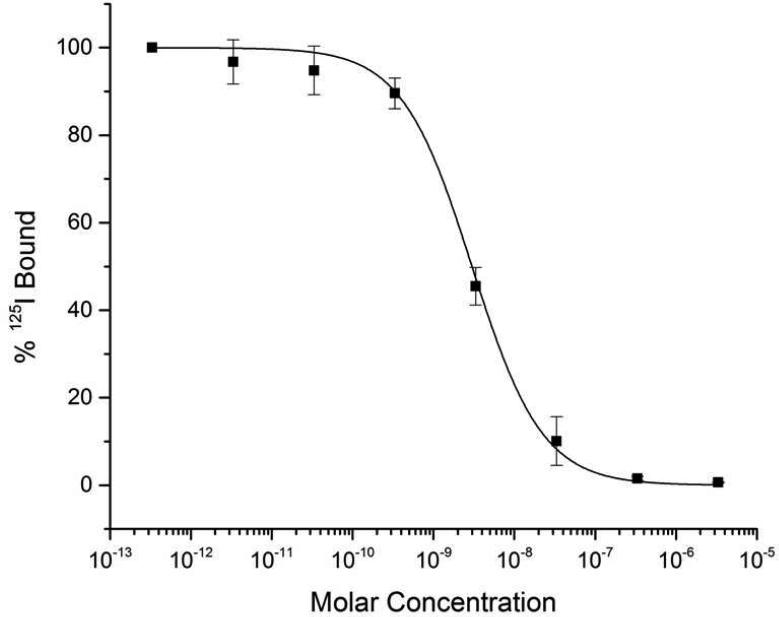
A competitive displacement receptor binding assay in human prostate PC-3 cells using 125I-[Tyr4]BBN as the radioligand showed high binding affinity of [RGD-Glu-[natCu-NO2A]-6-Ahx-RM2] conjugate for the GRPr (3.09 ± 0.34 nM). A similar assay in human, glioblastoma U87-MG cells using 125I-Echistatin as the radioligand indicated a moderate receptor-binding affinity for the αvβ3 integrin (518 ± 37.5 nM). In vivo studies of [RGD-Glu-[64Cu-NO2A]-6-Ahx-RM2] showed high accumulation (4.86 ± 1.01 %ID/g, 1 h post-intravenous injection (p.i.)) and prolonged retention(4.26 ± 1.23 %ID/g, 24 h p.i.) of tracer in PC-3 tumor-bearing mice. Micro-positron emission tomography (microPET) molecular imaging studies produced high-quality, high contrast images in PC-3 tumor-bearing mice at 4 h p.i.
Conclusions
The favorable pharmacokinetics and enhanced tumor uptake of 64Cu-NOTA-RGD-Glu-6Ahx-RM2 warrant further investigations for dual integrin and GRPr-positive tumor imaging and possible radiotherapy.
Keywords: gastrin-releasing peptide, prostate-specific membrane antigen, bombesin, prostate cancer, copper-64
1. Introduction
According to the American Cancer Society, prostate cancer will account for an estimated 238,590 new cases and 29,720 deaths in 2013 [1]. Identification of prostate tumors at an early stage continues to be challenging for oncologists and is of great clinical importance [2, 3]. Although direct mortality from non-metastatic prostate cancer is relatively low, the grave prognosis, excruciating pain, and increasing costs of palliative therapy associated with the chronic and metastatic stages of the disease drives continued and intensified investigations toward the development of novel and more effective means of earlier, accurate detection and therapy. Surgery and various forms of radiation- and chemically-based treatments have sought to eliminate primary tumors and prevent or slow metastatic progression; unfortunately, nearly all prostatic cancers eventually reach a point whereby they become refractory to androgen deprivation therapy and achieve the metastasis which accounts for the majority of the complications and mortalities associated with prostate cancer [4]. Furthermore, treatments themselves may cause side effects due to the inherently imprecise nature in which they are delivered. Likewise, diagnostic methods such as serum prostate specific antigen (PSA) and needle biopsy historically have been controversial in their usefulness for the accurate detection of early stage prostatic neoplasia, resulting in missed diagnoses as well as unnecessary treatments [5, 6].
The development of more target-specific, radiation-based, diagnostics and therapies has shown limited success in clinical trials, notably those that employ the use of radionuclides paired with target-specific bioprobes [7]. For example, the unique over-expression of peptide receptors in human tumors is a driving force for continued clinical interest of tumor imaging and targeted radionuclide therapy [8]. The GRPr is a subtype of the BBN receptor superfamily found to be expressed in a variety of human cancers, such as breast, colon, pancreatic, and prostate cancer. Many of these cancers continue to be targeted with radiolabeled BBN derivatives for site-directed molecular imaging or therapy of disease [9-11]. BBN, a tetradecapeptide analogue of human GRP has very high binding affinity for GRPr [8, 10, 12] and numerous BBN analogues have been synthesized and characterized for GRPr-positive tumor-targeted imaging and therapy [13-18]. Monomeric and dimeric RGD peptides have attracted interest due to their ability to specifically target the αVβ3 integrin, which is expressed on several tumors such as malignant melanomas, glioblastoma, breast, and prostate tumors [3, 19-21]. A number of RGD peptide analogues have been radiolabeled with 99mTc, 111In, 68Ga, 18F and 64Cu radionuclides and evaluated for targeting integrin αVβ3-positive tumors [22-27].
A new and exciting approach for development of peptide-based radiopharmaceuticals is the simultaneous targeting of multiple receptor subtypes with a single, endogenous, radioligand. Many research groups have investigated monovalent GRPr- and αvβ3-targeting radioligands for receptor-targeted prostate cancer imaging and therapy. These compounds have traditionally been modeled after a single, endogenous peptide hormone, small peptide, or antibody, which begets the tendency for them to bind only to those cancer cells which adequately express the target molecule. However, results of new heterodimeric peptide conjugates have continued to show improved molecular imaging properties when compared to monomeric peptide conjugates [28-31]. This is presumably due to an effective increase in the total number of receptors that are available for binding the heterodimer. For example, the total number of receptors available for binding a heterodimeric radioligand is the sum of all GRPr and αVβ3 receptors on the cell surface and should be higher than that of either monovalent GRPr-/ αVβ3 single receptor-targeting radioligands [32].
Because prostate cancer cells seem to differentially express specific receptors depending upon factors that may include chronicity and metastatic nature, it logically follows that a compound capable of targeting more than one biomarker would have the ability of binding to both early and chronic/metastatic stages of prostate cancer, creating the possibility for a more prompt and accurate diagnostic profile for both, but also a much more precise and efficient mode of normal tissue-sparing therapy with far fewer side effects. It is well known that the androgen-independent prostate cancer cell line (PC-3) co-expresses both GRPr and integrin αvβ3[3]. In the present study, we have designed and synthesized a 64Cu-radiolabeled RGD-RM2 heterodimeric peptide antagonist for dual receptor targeting of the form [RGD-Glu-[64Cu-NO2A]-6-Ahx-RM2]. 64Cu-radiolabeled radiopharmaceuticals have been of interest to our group and many others due to the ideal nuclear characteristics of 64Cu; 64Cu [t1/2=12.7h; Eβ+max=0.65MeV (17.9%); Eβ-max=0.57MeV (39%); electron capture (EC) (43.1%)], making it useful for in vivo molecular imaging. 64Cu is a cyclotron-produced radionuclide prepared via a (p,n) reaction on a highly-enriched 64Ni target. The half-life for 64Cu is sufficiently long enough for drug preparation, quality control, drug incorporation, circulation, and patient imaging [33, 34]. RM2 is an antagonist analogue of BBN that has recently been shown to have improved uptake and retention in tumors as compared to agonist GRPr-targeting ligands [35]. In this study, we report detailed in vitro investigations of this GRPr/αvβ3-targeting ligand in human PC-3 and U87-MG cells. In vivo biodistribution and microPET molecular imaging investigations of the RGD-RM2 heterodimer in PC-3 bumor-bearing mice are also described.
2. Materials and Methods
2.1 General
[RGD-Glu-6Ahx-RM2], [Cyclo(Arg-Gly-Asp-DTyr-Lys)-Glu-(6-Ahx-D-Phe-Gln-Trp-Ala-Val-Gly-His-Sta-Leu-NH2)], was purchased from CPC Scientific (Sunnyvale, CA, USA). NOTA bifunctional chelating agent was manually conjugated to the [RGD-Glu-6Ahx-RM2] dimeric peptide analogue via an active ester per a previously described procedure [28] to yield [RGDGlu-[NO2A]-6-Ahx-RM2]. All other reagents/solvents were purchased from Fisher Scientific (Pittsburgh, PA, USA) or Sigma-Aldrich Chemical Company (St. Louis, MO, USA) and used without further purification. 125I-[Tyr4]BBN was purchased from Perkin Elmer (Waltham, MA, USA). 125I-Echistatin was purchased from Perkin Elmer, Inc (Shelton, CT, USA). Copper radionuclide in the form of 64CuCl2 in 0.1 M HCl solution was purchased from the University of Wisconsin-Madison Medical Physics Department, USA.
The peptide conjugate and metallated complexes reported herein were purified using RPHPLC performed on an SCL-10A HPLC system (Shimadzu, Kyoto, Japan) employing a binary gradient system [solvent A=99.9% DI water with 0.1% trifluoroacetic acid (TFA); solvent B= 99.9% acetonitrile containing 0.1% TFA]. Samples were observed using an in-line Shimadzu SPD-10A absorption detector (λ=280 nm) as well as an in-line EG&G Ortec NaI solid crystal scintillation detector (EG&G, Salem, MA, USA). EZStart software (7.4; Shimadzu) was used for data acquisition of both signals. An analytical C-18 reversed-phase column (Phenomenex, Torrance, CA, USA) maintained at 34°C was used to achieve purification of [RGD-Glu-[NO2A]-6-Ahx-RM2] and [RGD-Glu-[nat/64Cu-NO2A]-6-Ahx-RM2] peptide conjugates. A linear gradient of 25:75A/B to 35:65 A/B gradient over 15 min (followed by an additional 10 min at 5:95 A/B) was used to purify the peptides. Purified peptide conjugates were lyophilized in a CentriVap system (Labconco, Kansas City, MO, USA). ESI-MS analyses were performed at the University of Missouri, Department of Chemistry, Columbia, MO, USA.
2.2 Synthesis of [RGD-Glu-[nat/64Cu-NO2A]-6-Ahx-RM2] conjugates
[RGD-Glu-[natCu-NO2A]-6-Ahx-RM2] conjugate was synthesized by the addition of natCuCl2·2H2O in 0.05 N HCl (90 nmol) to purified [RGD-Glu-[NO2A]-6-Ahx-RM2] peptide conjugate (89 nmol) and 0.4 M ammonium acetate (250 μl). The pH of the mixture was adjusted to approximately 7.0 by the addition of 1% NaOH and then incubated for 1 h at 70°C. Ten millimolar diethylenetriaminepentaacetic acid (DTPA) solution (50 μl) was added to scavenge unbound metal. [RGD-Glu-[natCu-NO2A]-6-Ahx-RM2] conjugate was purified by RPHPLC and characterized by ESI-MS prior to in vitro competitive binding assays.
Synthesis of the radionuclide conjugate was achieved by the reaction of [RGD-Glu-[NO2A]-6-Ahx-RM2] (50 μg, 200 μl 0.4 M ammonium acetate) with 64CuCl2·2H2O (74-111 MBq, 9.15 × 108 Bq/mol) for 1 h at 70°C (pH=7.0). Addition of 50 μl of 10 mM DTPA solution was used to scavenge any remaining unreacted copper metal. The resulting 64Cu-peptide conjugate was purified using RP-HPLC and collected into 100 μl of 1 mg/ml bovine serum albumin (BSA) prior to in vitro and in vivo assays. Acetonitrile was removed under a steady stream of nitrogen and the radiochemical purity was assessed by RP-HPLC.
2.3 In vitro receptor binding assays
The IC50 value of [RGD-Glu-[natCu-NO2A]-6-Ahx-RM2] was evaluated in GRPr-expressing, human, PC-3, prostate cancer cells according to published procedure [34]. Experiments were performed four times, in triplicate. The IC50 values were calculated using GraphPad Software.
Similarly, the binding affinity of [RGD-Glu-[natCu-NO2A]-6-Ahx-RM2] was determined by a competitive cell binding assay in αvβ3-expressing glioblastoma U87-MG cells using 125I-Echistatin as the radioligand. Briefly, U87-MG cells (9 × 104 cells/well) were seeded in Millipore 96-well filter multiscreen DV plates (0.65 μm pore size) and incubated at 25°C for 2 h with approximately 30,000 cpm of 125I-Echistatin in the presence of increasing concentrations (10-12 to 10-5 M) of [RGD-Glu-[natCu-NO2A]-6-Ahx-RM2] in 0.2 mL of binding medium. After the incubation, the plates were filtered through a multiscreen vacuum manifold and rinsed twice with 0.5 mL of ice-cold pH 7.4, 0.2% BSA/0.01 M PBS. The hydrophilic polyvinylidenedifluoride (PVDF) filters were collected and the radioactivity was measured in a Wallac 2480 automated gamma counter (PerkinElmer, NJ). The IC50 values were calculated as previously described (vide infra). As a control, the IC50 of cyclo-RGD was also measured in U87-MG cells using 125I-Echistatin as the radioligand.
2.4 In vivo biodistribution studies
All animal studies were conducted in compliance with the highest standards of care as outlined in the NIH Guide for the Care and Use of Laboratory Animals and the Policy and Procedures for Animal Research at the Truman VA Hospital, Columbia, Missouri, USA. Female CF-1 and Institute of Cancer Research severe combined immunodeficient (SCID) female mice (4–5 weeks of age) were supplied from Taconic Farms (Germantown, NY, USA). PC-3 cells were injected into the subcutaneous flanks of female SCID mice according to published procedure [28]. Tumors were allowed to grow two to three weeks postinoculation, developing tumors ranging in mass from 0.05 g to 0.34 g. Biodistribution studies in CF-1 and SCID mice were performed by injection of ~20 μCi (~0.75 MBq, 8.08x10-14-2.02x10-13 mol, 9.16x1018 Bq/mol) of [RGD-Glu-[64Cu-NO2A]-6-Ahx-RM2] (100 μL, 0.9% NaCl) into the tail vein. Mice were euthanized at 1 h, 4 h or 24 h p.i. and tissues, organs, and urine were collected, weighed, and counted in a NaI well counter. The percent injected dose (%ID) and the percent injected dose per gram (%ID/g) were calculated. The whole blood volume was assumed to be 6.5% of the total body weight, allowing for the %ID in whole blood.
2.5 microPET/microCT imaging studies
Maximum intensity microPET coronal images were obtained on a Siemens INVEON small-animal, dedicated PET unit (Siemens, Nashville, TN, USA) at 4 h. p.i. according to published procedure [28]. Micro-computed tomography (microCT) coronal images were also obtained on the Siemens INVEON small-animal CT unit (Nashville, TN, USA) immediately following microPET imaging for the purpose of fusing the anatomic and molecular data. The microCT images were acquired for approximately 8 min, and concurrent image reconstruction was achieved using a conebeam (Feldkamp) filtered, back-projection algorithm. The raw, reconstructed microPET datasets (with a matrix size of 512x512x159) were imported into the INVEON Research Workstation software for subsequent image fusion with the microCT image data and 3D visualization.
3. Results and Discussion
Integrins are only moderately expressed on the surfaces of some prostate tumors. For example, the αvβ3 integrin receptor density per cell is approximately 2.8 x 103 on PC-3 prostate cancer cells [36]. The GRPr density per PC-3 cell, on the other hand, is approximately 2.5 x 105 [37]. Because each of these two receptor subtypes are expressed only minimally on normal human cells, the ability to design radiolabeled monovalent or bivalent BBN/RGD derivatives that exhibit high-affinity for GRP/αvβ3 receptor subtypes on human prostate cancers provides significant opportunity for molecular imaging and targeted radionuclide therapy. 64Cu-radiolabeled RGD/BBN heterodimers and monovalent RGD and BBN agonist/antagonist ligands have been extensively investigated for use as SPECT/PET imaging probes of human prostate cancer tumors which express both integrin αVβ3 and GRPr. Heterodimers targeting αVβ3 and GRPr have been shown to be superior to monovalent GRPr/αvβ3-targeting ligands, which can be limited by one or the other molecular targets/biomarkers being expressed either in very low numbers or not at all [29-31, 38]. Herein we have described the synthesis, characterization, and the pharmacological evaluation of an antagonist heterodimer, [RGD-Glu-[64Cu-NO2A]-6-Ahx-RM2], for dual targeting of integrin αVβ3 and GRPr. To our knowledge, this is the first heterodimer based upon a GRPr-targeting antagonist ligand, which, until now, have remained largely unexplored.
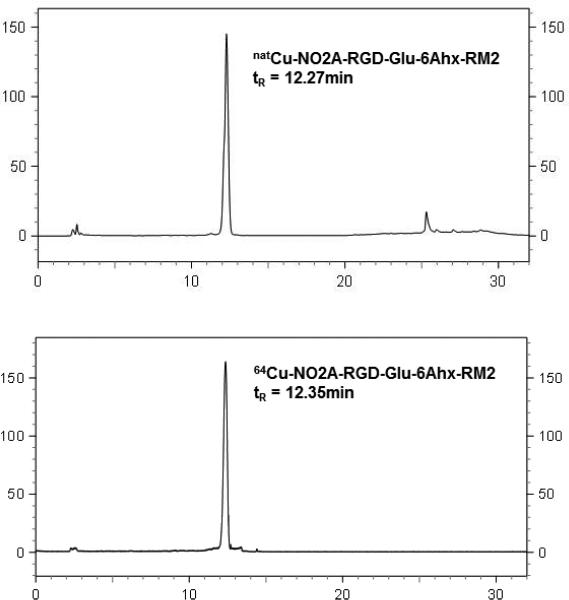
In this study, the NOTA bifunctional chelator was manually conjugated to the [RGD-Glu-6Ahx-RM2] peptide and the resulting [RGD-Glu-[NO2A]-6-Ahx-RM2] conjugate was metallated with natural copper. [RGD-Glu-[NO2A]-6-Ahx-RM2] and [RGD-Glu-[natCu-NO2A]-6-Ahx-RM2] conjugates were purified by RP-HPLC. The ESI-MS analyses of [RGD-Glu-[NO2A]-6-Ahx-RM2] and [RGD-Glu-[natCu-NO2A]-6-Ahx-RM2] were consistent with the molecular weights calculated for each analogue (Table 1). The chemical structure of [RGD-Glu-[Cu-NO2A]-6-Ahx-RM2] is shown in Figure 1. The [RGD-Glu-[NO2A]-6-Ahx-RM2] conjugate was radiolabeled with positron-emitting 64Cu in high radiochemical yield (≥95%). The retention times for [RGD-Glu-[natCu-NO2A]-6-Ahx-RM2] and [RGD-Glu-[64Cu-NO2A]-6-Ahx-RM2] are 12.27 and 12.35 min, respectively, and indicate the structural similarity between the macroscopic and tracer level conjugates (Fig. 2).
TABLE 1.
Mass spectrometry, IC50, and RP-HPLC data for [RGD-Glu-[NO2A]-6-Ahx-RM2] and [RGD-Glu-[nat/64Cu-NO2A]-6-Ahx-RM2].
| Calculated molecular mass, [RGD-Glu-[NO2A]-6-Ahx-RM2] | 2241.17 Da |
| Calculated molecular mass, [RGD-Glu-[natCu-NO2A]-6-Ahx-RM2] | 2302.08 Da |
| Electrospray ionization molecular mass, [RGD-Glu-[NO2A]-6-Ahx-RM2] | 2242.39 Da |
| Electrospray ionization molecular mass, [RGD-Glu-[natCu-NO2A]-6-Ahx-RM2] | 2303.64 Da |
| Molecular Formula [RGD-Glu-[NO2A]-6-Ahx-RM2] | C105H156N28O27 |
| Molecular Formula [RGD-Glu-[Cu-NO2A]-6-Ahx-RM2] | C105H154CuN28O27 |
| [RGD-Glu-[natCu-NO2A]-6-Ahx-RM2] RP-HPLC tR | 12.27 min |
| [RGD-Glu-[64Cu-NO2A]-6-Ahx-RM2] RP-HPLC tR | 12.35 min |
| IC50, [RGD-Glu-[natCu-NO2A]-6-Ahx-RM2], PC-3 | 3.09±0.34 nM |
| IC50, [RGD-Glu-[natCu-NO2A]-6-Ahx-RM2], U87-MG | 518±37.5 nM |
FIGURE 1.
Chemical structure of [RGD-Glu-[nat/64Cu-NO2A]-6-Ahx-RM2] antagonist.
FIGURE 2.
HPLC chromatographic profiles of [RGD-Glu-[natCu-NO2A]-6-Ahx-RM2] (tR = 12.27 min) and [RGD-Glu-[64Cu-NO2A]-6-Ahx-RM2] (tR = 12.35 min).
In vitro competitive binding studies for [RGD-Glu-[natCu-NO2A]-6-Ahx-RM2] were performed on human androgen-independent prostate cancer PC-3 cells. A typical sigmoidal curve for displacement of 125I-[Tyr4]-BBN from PC-3 cells as a function of increasing concentration of [RGD-Glu-[natCu-NO2A]-6-Ahx-RM2] was obtained (Fig. 3). The IC50 value of the heterodimer was determined to be 3.09 ± 0.34 nM and is similar to the NO2A-RGD-BBN agonist, natCu-NO2A-RGD-Glu-6Ahx-BBN, previously reported by Jackson and coworkers [28]. Similarly, to assess the binding affinity of [RGD-Glu-[natCu-NO2A]-6-Ahx-RM2] for αVβ3, a competitive displacement was performed in αvβ3-expressing, human, glioblastoma U87-MG cells using 125IEchistatin as the radioligand. These results showed an IC50 of 518 ± 37.5 nM, indicating only moderate specific binding to the integrin receptor. Comparably, the IC50 for cyclo-RGD in U87-MG cells was 162 ± 5.5 nM. Li and co-workers have evaluated the binding affinities of RGD, BBN-RGD, and FB-BBN-RG for the αVβ3 receptor on U87-MG cells and have determined the IC50s to be 202 ± 28, 428 ± 57, and 282 ± 34 nM, respectively, showing only moderate binding to the αVβ3 receptor as well [39]. To evaluate the binding affinity of [RGD-Glu-[natCu-NO2A]-6-Ahx-RM2] for αVβ3 receptors on PC-3 cells, a cell line known to express the integrin in only moderate to low numbers, competitive binding assays using 125I-Echistatin as the radioligand were also performed. [RGD-Glu-[natCu-NO2A]-6-Ahx-RM2] showed minimal displacement of 125IEchistatin from PC-3 cells. These results are similar to those observed for natCu-NO2A-RGDGlu-6Ahx-BBN agonist, and suggest the driving mechanism for ligand binding to PC-3 cells to be primarily GRPr-mediated [28]. Previous studies for a 99mTc-radiolabeled dual-targeting MC1/αVβ3 radioligand showed an IC50 of 403 nM for the αVβ3 integrin receptor in an M21 human, melanoma cell line. The authors of that study attribute the successful molecular imaging investigations in a human M21 mouse model to a combination of very high αVβ3 integrin receptor density and very high binding affinity to the MC1 receptor (2.0 nM), although relatively poor αVβ3 binding affinity was observed [40].
FIGURE 3.
Inhibitory concentration half maximum (IC50) [RGD-Glu-[natCu-NO2A]-6-Ahx-RM2] (IC50 = 3.09 ± 0.34 nM) in human, prostate, PC-3 cells.
Table 2 summarizes the results of biodistribution studies for [RGD-Glu-[64Cu-NO2A]-6-Ahx-RM2] in normal CF-1 mice at 1, 4 and 24 h p.i. Rapid blood clearance of tracer was demonstrated with only 0.09±0.03% of the injected dose being retained at 4 h p.i. The primary mode of clearance for the tracer was the renal-urinary excretion pathway, with more than 75% ID having cleared the urine at 1 h p.i. [RGD-Glu-[64Cu-NO2A]-6-Ahx-RM2] quickly cleared GRPr-negative organs and showed minimal uptake in hepatic tissue. In addition, pancreatic accumulation at the same time interval was 4.70±1.04% ID/g and was reduced to 0.71±0.08 % ID/g at 4 h p.i. It is well-known that mouse pancreatic tissue expresses the GRPr in very high density. Therefore, high accumulation of radioactivity in pancreatic tissue is oftentimes an indicator of effective GRPr targeting for radiolabeled bombesin conjugates. The liver uptake of [RGD-Glu-[64Cu-NO2A]-6-Ahx-RM2] was low, with the highest uptake being 1.42±0.17% ID/g at 4 h p.i. (1.32±0.27% ID/g at 1 h p.i). This again suggests that the Cu(II)/NO2A metal complex was effectively stable under in vivo conditions [41].
TABLE 2.
Biodistribution studies of [RGD-Glu-[64Cu-NO2A]-6-Ahx-RM2] in CF-1 normal mice at 1, 4 and 24 h p.i. (%ID/g ± SD, n = 5).
| 1h | 4h | 24h | |
|---|---|---|---|
| Heart | 0.39±0.12 | 0.54±0.40 | 0.39±0.04 |
| Lung | 0.98±0.17 | 0.83±0.35 | 0.78±0.19 |
| Liver | 1.32±0.27 | 1.42±0.17 | 1.38±0.19 |
| Kidneys | 3.54±0.56 | 2.53±0.37 | 1.15±0.07 |
| Spleen | 1.00±0.27 | 0.69±0.12 | 0.61±0.15 |
| Stomach | 1.63±0.41 | 1.08±0.47 | 0.64±0.22 |
| S.Intestine | 2.20±0.56 | 1.43±0.55 | 0.72±0.20 |
| L.Intestine | 1.01±0.14 | 2.30±0.40 | 0.91±0.20 |
| Muscle | 0.32±0.11 | 0.15±0.05 | 0.10±0.03 |
| Bone | 0.88±0.26 | 0.71±0.16 | 0.39±0.11 |
| Brain | 0.05±0.02 | 0.04±0.01 | 0.08±0.03 |
| Pancreas | 4.70±1.04 | 0.71±0.08 | 0.38±0.08 |
| Blood* | 0.24±0.04 | 0.09±0.03 | 0.13±0.02 |
| Urine* | 75.2±3.47 | 82.5±2.86 | 84.7±2.68 |
| Bladder | 2.34±1.15 | 1.31±0.46 | 0.39±0.36 |
Data presented as %ID
The results of the [RGD-Glu-[64Cu-NO2A]-6-Ahx-RM2] biodistribution in PC-3 tumor-bearing SCID mice are presented in Table 3. Radioactivity cleared efficiently from the bloodstream, with only 0.55±0.13% ID remaining in whole blood at 1 h p.i. The primary route of excretion was very much comparable to that seen in the normal, CF-1 mice. At 1, 4 and 24 h p.i., uptake of the conjugate in renal tissue was found to be 5.06±1.13, 4.76±1.92, and 2.43±0.81% ID/g, respectively. Moderately high uptake of radioactivity was observed in the liver as compared to that seen in normal CF-1 biodistribution investigations, with results ranging from 2.65±0.55% ID/g at 1 h p.i. to 2.44±0.39% ID/g at 24 p.i. Furthermore, pancreatic accumulation of 64Cu-NO2A-RGD-Glu-6Ahx-RM2 in PC-3 tumor-bearing mice was nearly two-fold higher in comparison to that observed in normal CF-1 mice at 1 h p.i. For example, uptake in pancreas was 8.09±1.29% ID/g at 1 h p.i. for tumor-bearing mice. Uptake in xenografted PC-3 tumors achieved maximal concentration (6.37±1.23% ID/g) at 4 h p.i. At 24 h p.i., tumor concentration of the tracer surpassed that of all normal tissues with retention of 4.26±1.23% ID/g. It is worth noting that the washout of the radioactivity from the tumor tissue was much slower than the washout from other GRPr positive organs such as the pancreas and intestines. For example, while ~87% of the radioactivity was retained in the tumors at 24 h p.i., only ~8% of the radioactivity was retained in normal pancreas at the same time interval. In comparison, the agonist 64Cu-NO2A-RGD-Glu-6Ahx-BBN conjugate showed ~24% of the radioactivity to be retained in normal pancreas at the 24 h time-point [28]. Furthermore, the amount of retained radioactivity in tumor tissue was found only to be ~60%. These results suggest that antagonist-based constructs, which show faster washout from non-target organs and higher tumor uptake and retention, are superior to their agonist “cousins”. Both heterodimeric conjugates, however, show prolonged tumor-associated radioactivity that is sufficient for molecular imaging studies and, possibly, targeted radiotherapy. Last of all, due to the rapid clearance of radioactivity from the body, high tumor to background ratios were found. For instance, tumor to blood and tumor to muscle ratios increased from 8.8 and 10.9 at 1 h to 20.9 and 14.1 at 4 h, respectively.
TABLE 3.
Biodistribution studies of [RGD-Glu-[64Cu-NO2A]-6-Ahx-RM2] in PC-3 tumor-bearing SCID mice at 1, 4 and 24 h p.i. (%ID/g ± SD, n = 5).
| 1h | 4h | 24h | |
|---|---|---|---|
| Heart | 0.99±0.53 | 0.73±0.26 | 0.79±0.11 |
| Lung | 1.65±0.29 | 1.56±0.26 | 1.21±0.22 |
| Liver | 2.65±0.55 | 3.22±0.92 | 2.44±0.39 |
| Kidneys | 5.06±1.13 | 4.76±1.92 | 2.43±0.81 |
| Spleen | 2.56±0.90 | 3.13±1.65 | 2.17±0.72 |
| Stomach | 2.21±0.47 | 2.04±1.29 | 0.74±0.47 |
| S.Intestine | 3.64±0.61 | 3.12±1.62 | 1.25±0.59 |
| L.Intestine | 1.39±0.47 | 4.20±1.55 | 2.37±2.13 |
| Muscle | 0.44±0.11 | 0.45±0.21 | 0.26±0.13 |
| Bone | 0.89±0.14 | 0.84±0.41 | 0.68±0.50 |
| Brain | 0.08±0.02 | 0.09±0.05 | 0.08±0.03 |
| Pancreas | 8.09±1.29 | 1.95±0.93 | 0.64±0.26 |
| Blood* | 0.55±0.13 | 0.30±0.08 | 0.36±0.08 |
| Urine* | 69.4±5.28 | 76.1±6.48 | 79.1±2.66 |
| Tumor | 4.86±1.01 | 6.37±1.68 | 4.26±1.23 |
Data presented as %ID
The results of microPET/microCT imaging studies in PC-3 tumor-bearing, SCID mice using [RGD-Glu-[64Cu-NO2A]-6-Ahx-RM2] are presented in Figure 4. PC-3 xenografted tumors were clearly visible at the 4 h time-point, producing high-quality, high-contrast microPET images with excellent tumor-to-background ratios. Previous studies in our laboratory have produced high-quality microPET images in tumor-bearing murine models. However, many of the microPET images we have produced are at the 15-18 h time-point in order to allow maximum excretion and clearance from non-target tissues of the abdomen. These studies, on the other hand, show only minimal collateral radioactivity in non-target tissues at 4 h p.i., indicating the propensity of the RGD sequence to possibly facilitate excretion and clearance from these tissues to create high-quality, high-contrast images at an earlier time-point.
FIGURE 4.
Maximum intensity microPET tumor and microCT skeletal fusion coronal whole-body image of a PC-3 tumor bearing SCID mouse at 4 h after tail vein injection of [RGD-Glu-[64Cu-NO2A]-6-Ahx-RM2].
4. Conclusion
Maecke and co-workers have recently investigated a 64Cu-radiolabeled, antagonist-like targeting vector, [CB-TE2A-PEG4-RM2] (CB-TE2A; 4,11-bis(carboxymethyl)-1,4,8,11-tetraazabicyclo[6.6.2]hexadecane), having high selectivity for the GRPr [35]. Cross-bridged, cyclam-based ligand frameworks (CB-TE2A) appended to many biologically-active targeting vectors have been shown to offer improved kinetic stability under in vivo conditions when compared to other poly(aminocarboxylate)-containing ligand frameworks [13, 42-47]. This new tracer produced high-quality, high-contrast microPET images in a PC-3 tumor-bearing mouse model at 12 h p.i. Based upon high tumor uptake and retention, favorable pharmacokinetics, and high in vivo stability, they have introduced this new monovalent targeting vector into human clinical trials in Europe [35]. In the present study, we have produced a [RGD-Glu-[64Cu-NO2A]-6-Ahx-RM2] heterodimer which contains structural motifs recognizing both integrin αvβ3 and GRPr. The αvβ3 and GRPr are validated biomarkers present on the surfaces of most prostate cancer cells. MicroPET imaging investigations at 4 h p.i. produced high-quality, high-contrast, whole-body images with minimal tracer present in surrounding, collateral, abdominal tissues. The high selectivity and retention of this tracer for tumor tissue suggests that a 67Cu-radiolabeled agent of this type may also be useful for targeted radiotherapy for prostate cancer primary tumors and metastatic disease. Furthermore, results from this study support previous studies produced by other research groups that suggest the superiority of radiolabeled antagonists over agonists to be used for molecular imaging of human cancers.
Acknowledgments
This material was the result of work supported with resources and the use of facilities at the Truman VA, Columbia, MO, 65201 and the University of Missouri School of Medicine, Columbia, MO 65211, USA. Dr. Kubra Durkan acknowledges financial support from the Scientific and Technological Research Council of Turkey (TUBITAK) Science Fellowships and Grant Programmes Department (BIDEB). This work was also funded in part by The United States Department of Veterans’ Affairs, VA Merit Bridge Funding Award Mechanism.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.American Cancer Society Cancer Facts & Figures. 2013 [Google Scholar]
- 2.Okarvi SM. Peptide-based radiopharmaceuticals and cytotoxic conjugates: Potential tools against cancer. Cancer Treatment Reviews. 2008;34:13–26. doi: 10.1016/j.ctrv.2007.07.017. [DOI] [PubMed] [Google Scholar]
- 3.Sutherland M, Gordon A, Shnyder S, Patterson L, Sheldrake H. RGD-Binding Integrins in Prostate Cancer: Expression Patterns and Therapeutic Prospects against Bone Metastasis. Cancers. 2012;4:1106–45. doi: 10.3390/cancers4041106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sullivan PW, Nelson JB, Mulani PM, Sleep D. Quality of life as a potential predictor for morbidity and mortality in patients with metastatic hormone-refractory prostate cancer. Qual Life Res. 2006;15:1297–306. doi: 10.1007/s11136-006-0003-2. [DOI] [PubMed] [Google Scholar]
- 5.Howrey BT, Kuo YF, Lin YL, Goodwin JS. The impact of PSA screening on prostate cancer mortality and overdiagnosis of prostate cancer in the United States. J Gerontol A Biol Sci Med Sci. 2013;68:56–61. doi: 10.1093/gerona/gls135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.D'Amico AV. Prostate-cancer mortality after PSA screening. N Engl J Med. 2012;366:2229. doi: 10.1056/NEJMc1204298. author reply 30-1. [DOI] [PubMed] [Google Scholar]
- 7.Pool SE, Krenning EP, Koning GA, van Eijck CH, Teunissen JJ, Kam B, et al. Preclinical and clinical studies of peptide receptor radionuclide therapy. Semin Nucl Med. 2010;40:209–18. doi: 10.1053/j.semnuclmed.2009.12.001. [DOI] [PubMed] [Google Scholar]
- 8.Reubi JC. Peptide receptors as molecular targets for cancer diagnosis and therapy. Endocrine Reviews. 2003;24:389–427. doi: 10.1210/er.2002-0007. [DOI] [PubMed] [Google Scholar]
- 9.Markwalder R, Reubi JC. Gastrin-releasing peptide receptors in the human prostate: Relation to neoplastic transformation. Cancer Res. 1999;59:1152–9. [PubMed] [Google Scholar]
- 10.Smith CJ, Volkert WA, Hoffman TJ. Gastrin releasing peptide (GRP) receptor targeted radiopharmaceuticals: A concise update. Nucl Medicine Biol. 2003;30:861–8. doi: 10.1016/s0969-8051(03)00116-1. [DOI] [PubMed] [Google Scholar]
- 11.Varvarigou A, Bouziotis P, Zikos C, Scopinaro F, De Vincentis G. Gastrin-releasing peptide (GRP) analogueues for cancer imaging. Cancer Biother Radiopharm. 2004;19:219–29. doi: 10.1089/108497804323072002. [DOI] [PubMed] [Google Scholar]
- 12.Nock BA, Nikolopoulou A, Galanis A, Cordopatis P, Waser B, Reubi JC, et al. Potent bombesin-like peptides for GRP-receptor targeting of tumors with 99mTc: A preclinical study. J Med Chem. 2005;48:100–10. doi: 10.1021/jm049437y. [DOI] [PubMed] [Google Scholar]
- 13.Chen X, Park R, Hou Y, Tohme M, Shahinian AH, Bading JR, et al. MicroPET and autoradiographic imaging of GRP receptor expression with 64Cu-DOTA-[Lys3]bombesin in human prostate adenocarcinoma xenografts. J Nucl Med. 2004;45:1390–7. [PubMed] [Google Scholar]
- 14.Smith CJ, Sieckman GL, Owen NK, Hayes DL, Mazuru DG, Kannan R, et al. Radiochemical investigations of gastrin-releasing peptide receptor-specific [99mTc(X)(CO)3-Dpr-Ser-Ser-Ser-Gln-Trp-Ala- Val-Gly-His-Leu-Met-(NH2)] in PC-3, tumor-bearing, rodent models: Syntheses, radiolabeling, and in vitro/in vivo studies where Dpr = 2,3-diaminopropionic acid and X = H2O or P(CH2OH)3. Cancer Res. 2003;63:4082–8. [PubMed] [Google Scholar]
- 15.Prasanphanich AF, Retzloff L, Lane SR, Nanda PK, Sieckman GL, Rold TL, et al. In vitro and in vivo analysis of [64Cu-NO2A-8-Aoc-BBN(7-14)NH2]: a site-directed radiopharmaceutical for positron-emission tomography imaging of T-47D human breast cancer tumors. Nucl Med Biol. 2009;36:171–81. doi: 10.1016/j.nucmedbio.2008.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yang Y-S, Zhang X, Xiong Z, Chen X. Comparative in vitro and in vivo evaluation of two 64Cu- labeled bombesin analogues in a mouse model of human prostate adenocarcinoma. Nuclear Medicine and Biology. 2006;33:371–80. doi: 10.1016/j.nucmedbio.2005.12.011. [DOI] [PubMed] [Google Scholar]
- 17.Gourni E, Bouziotis P, Benaki D, Loudos G, Xanthopoulos S, Paravatou-Petsotas M, et al. Structural Assessment and Biological Evaluation of Two N3S Bombesin Derivatives. Journal of Medicinal Chemistry. 2009;52:4234–46. doi: 10.1021/jm900360d. [DOI] [PubMed] [Google Scholar]
- 18.Scopinaro F, Vincentis G, Varvarigou A, Laurenti C, Iori F, Remediani S, et al. 99mTc-bombesin detects prostate cancer and invasion of pelvic lymph nodes. Eur J Nucl Med Mol Imaging. 2003;30:1378–82. doi: 10.1007/s00259-003-1261-7. [DOI] [PubMed] [Google Scholar]
- 19.Schottelius M, Laufer B, Kessler H, Wester H-, Jr. Ligands for Mapping αvβ3-Integrin Expression in Vivo. Accounts of Chemical Research. 2009;42:969–80. doi: 10.1021/ar800243b. [DOI] [PubMed] [Google Scholar]
- 20.Fani M, Maecke HR, Okarvi SM. Radiolabeled peptides: valuable tools for the detection and treatment of cancer. Theranostics. 2012;2:481–501. doi: 10.7150/thno.4024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liu S. Radiolabeled Multimeric Cyclic RGD Peptides as Integrin αvβ3 Targeted Radiotracers for Tumor Imaging. Molecular Pharmaceutics. 2006;3:472–87. doi: 10.1021/mp060049x. [DOI] [PubMed] [Google Scholar]
- 22.Line BR, Mitra A, Nan A, Ghandehari H. Targeting tumor angiogenesis: comparison of peptide and polymer-peptide conjugates. J Nucl Med. 2005;46:1552–60. [PubMed] [Google Scholar]
- 23.Dijkgraaf I, Kruijtzer JAW, Frielink C, Corstens FHM, Oyen WJG, Liskamp RMJ, et al. αvβ3 Integrin- targeting of intraperitoneally growing tumors with a radiolabeled RGD peptide. International Journal of Cancer. 2007;120:605–10. doi: 10.1002/ijc.22297. [DOI] [PubMed] [Google Scholar]
- 24.Blom E, Velikyan I, Estrada S, Hall H, Muhammad T, Ding C, et al. (68)Ga-Labeling of RGD peptides and biodistribution. Int J Clin Exp Med. 2012;5:165–72. [PMC free article] [PubMed] [Google Scholar]
- 25.Chen X, Park R, Shahinian AH, Tohme M, Khankaldyyan V, Bozorgzadeh MH, et al. 18F-labeled RGD peptide: initial evaluation for imaging brain tumor angiogenesis. Nuclear Medicine and Biology. 2004;31:179–89. doi: 10.1016/j.nucmedbio.2003.10.002. [DOI] [PubMed] [Google Scholar]
- 26.Beer AJ, Niemeyer M, Carlsen J, Sarbia M, Nährig J, Watzlowik P, et al. Patterns of αvβ3 Expression in Primary and Metastatic Human Breast Cancer as Shown by 18F-Galacto-RGD PET. Journal of Nuclear Medicine. 2008;49:255–9. doi: 10.2967/jnumed.107.045526. [DOI] [PubMed] [Google Scholar]
- 27.Wu Y, Zhang X, Xiong Z, Cheng Z, Fisher DR, Liu S, et al. microPET Imaging of Glioma Integrin αvβ3 Expression Using 64Cu-Labeled Tetrameric RGD Peptide. Journal of Nuclear Medicine. 2005;46:1707–18. [PubMed] [Google Scholar]
- 28.Jackson AB, Nanda PK, Rold TL, Sieckman GL, Szczodroski AF, Hoffman TJ, et al. 64Cu-NO2A-RGD-Glu-6-Ahx-BBN(7-14)NH2: A heterodimeric targeting vector for positron emission tomography imaging of prostate cancer. Nucl Med Biol. 2012;39:377–87. doi: 10.1016/j.nucmedbio.2011.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Liu Z, Li ZB, Cao Q, Liu S, Wang F, Chen X. Small-animal PET of tumors with 64Cu-labeled RGD- bombesin heterodimer. J Nucl Med. 2009;50:1168–77. doi: 10.2967/jnumed.108.061739. [DOI] [PubMed] [Google Scholar]
- 30.Liu Z, Niu G, Wang F, Chen X. 68Ga-labeled NOTA-RGD-BBN peptide for dual integrin and GRPR- targeted tumor imaging. E J Nucl Med and Mol Imag. 2009;36:1483–94. doi: 10.1007/s00259-009-1123-z. [DOI] [PubMed] [Google Scholar]
- 31.Liu Z, Yan Y, Liu S, Wang F, Chen X. 18F, 64Cu, and 68Ga labeled RGD-bombesin heterodimeric peptides for PET imaging of breast cancer. Bioconjugate Chem. 2009;20:1016–25. doi: 10.1021/bc9000245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chen K, Conti PS. Target-specific delivery of peptide-based probes for PET imaging. Advanced Drug Delivery Reviews. 2010;62:1005–22. doi: 10.1016/j.addr.2010.09.004. [DOI] [PubMed] [Google Scholar]
- 33.Anderson CJ, Welch MJ. Radiometal-labeled agents (non-technetium) for diagnostic imaging. Chemical Reviews. 1999;99:2219–34. doi: 10.1021/cr980451q. [DOI] [PubMed] [Google Scholar]
- 34.Prasanphanich AF, Nanda PK, Rold TL, Ma L, Lewis MR, Garrison JC, et al. [64Cu-NOTA-8-Aoc-BBN(7-14)NH2] targeting vector for positron-emission tomography imaging of gastrin-releasing peptide receptor-expressing tissues. PNAS. 2007;104:12462–7. doi: 10.1073/pnas.0705347104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Abiraj K, Mansi R, Tamma M-L, Fani M, Forrer F, Nicolas G, et al. Bombesin Antagonist–Based Radioligands for Translational Nuclear Imaging of Gastrin-Releasing Peptide Receptor–Positive Tumors. Journal of Nuclear Medicine. 2011;52:1970–8. doi: 10.2967/jnumed.111.094375. [DOI] [PubMed] [Google Scholar]
- 36.Shi J, Kim YS, Zhai S, Liu Z, Chen X, Liu S. Improving tumor uptake and pharmacokinetics of64Cu-labeled cyclic RGD peptide dimers with Gly3 and PEG4 linkers. Bioconjugate Chem. 2009;20:750–9. doi: 10.1021/bc800455p. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Maddalena ME, Fox J, Chen J, Feng W, Cagnolini A, Linder KE, et al. 177Lu-AMBA biodistribution, radiotherapeutic efficacy, imaging, and autoradiography in prostate cancer models with low GRP-R expression. Journal of Nuclear Medicine. 2009;50:2017–24. doi: 10.2967/jnumed.109.064444. [DOI] [PubMed] [Google Scholar]
- 38.Liu Z, Yan Y, Chin FT, Wang F, Chen X. Dual integrin and gastrin-releasing peptide receptor targeted tumor imaging using18F-Labeled PEGylated RGD-bombesin heterodimer 18F-FB-PEG3-Glu-RGD-BBN. Journal of Medicinal Chemistry. 2009;52:425–32. doi: 10.1021/jm801285t. [DOI] [PubMed] [Google Scholar]
- 39.Li ZB, Wu Z, Chen K, Ryu EK, Chen X. 18F-labeled BBN-RGD heterodimer for prostate cancer imaging. J Nucl Med. 2008;49:453–61. doi: 10.2967/jnumed.107.048009. [DOI] [PubMed] [Google Scholar]
- 40.Yang J, Guo H, Miao Y. Technetium-99m-labeled Arg-Gly-Asp-conjugated alpha-melanocyte stimulating hormone hybrid peptides for human melanoma imaging. Nuclear Medicine and Biology. 2010;37:873–83. doi: 10.1016/j.nucmedbio.2010.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lane SR, Nanda P, Rold TL, Sieckman GL, Figueroa SD, Hoffman TJ, et al. Optimization, biological evaluation and microPET imaging of copper-64-labeled bombesin agonists, [64Cu-NO2A-(X)-BBN(7-14)NH2], in a prostate tumor xenografted mouse model. Nucl Med Biol. 2010;37:751–61. doi: 10.1016/j.nucmedbio.2010.04.016. [DOI] [PubMed] [Google Scholar]
- 42.Bass LA, Wang M, Welch MJ, Anderson CJ. In vivo transchelation of copper-64 from TETA- octreotide to superoxide dismutase in rat liver. Bioconjugate Chem. 2000;11:527–32. doi: 10.1021/bc990167l. [DOI] [PubMed] [Google Scholar]
- 43.Boswell CA, Sun X, Niu W, Weisman GR, Wong EH, Rheingold AL, et al. Comparative in Vivo Stability of Copper-64-Labeled Cross-Bridged and Conventional Tetraazamacrocyclic Complexes. J Med Chem. 2004;47:1465–74. doi: 10.1021/jm030383m. [DOI] [PubMed] [Google Scholar]
- 44.Rogers BE, Bigott HM, McCarthy DW, Della Manna D, Kim J, Sharp TL, et al. MicroPET imaging of a gastrin-releasing peptide receptor-positive tumor in a mouse model of human prostate cancer using a 64 Cu-labeled bombesin analogueue. Bioconjugate Chem. 2003;14:756–63. doi: 10.1021/bc034018l. [DOI] [PubMed] [Google Scholar]
- 45.Rogers BE, Manna DD, Safavy A. In Vitro and In Vivo Evaluation of a 64Cu-Labeled Polyethylene Glycol-Bombesin Conjugate. Cancer Biother Radio. 2004;19:25–34. doi: 10.1089/108497804773391649. [DOI] [PubMed] [Google Scholar]
- 46.Sprague JE, Peng Y, Sun X, Weisman GR, Wong EH, Achilefu S, et al. Preparation and biological evaluation of copper-64-labeled Tyr3-octreotate using a cross-bridged macrocyclic chelator. Clin Cancer Res. 2004;10:8674–82. doi: 10.1158/1078-0432.CCR-04-1084. [DOI] [PubMed] [Google Scholar]
- 47.Sun X, Wuest M, Weisman GR, Wong EH, Reed DP, Boswell CA, et al. Radiolabeling and in vivo behavior of copper-64-labeled cross-bridged cyclam ligands. J Med Chem. 2002;45:469–77. doi: 10.1021/jm0103817. [DOI] [PubMed] [Google Scholar]