Abstract
Health literacy is known to affect vulnerable communities such as persons living with HIV/AIDS. The purpose of this review was to provide a current summary of research on the impact of health literacy on the health of persons living with HIV/AIDS and to address future areas of need. Contemporary studies focused on expanding the reach of health literacy in HIV/AIDS to retention in HIV care, use of technology for assessing and intervening to improve health literacy, and health literacy across the globe, for example. A number of studies did not find health literacy to explain health behaviors whereas other studies supported such a relationship. Future issues relevant to health literacy in HIV/AIDS include the aging of the HIV population and associated comorbidities, studies to understand the role of health literacy in specific populations affected by HIV/AIDS, and the continued need to refine the definition and measurement of health literacy.
Keywords: Health literacy, HIV, AIDS, Treatment adherence, Technological interventions, Health literacy measures, Aging, Disparities, Global literacy
Introduction
Health literacy continues to evolve as a concept because it shares commonalities with other fields such as decision-making, patient-provider communication, cognition [1–3], and basic academic skills such as reading and mathematics [4, 5]. Development of a comprehensive definition of health literacy that defines how it is distinct from related domains is a challenge. Despite this challenge, most authors agree that health literacy is a complex phenomenon involving access to and skillful use of health-related information to inform and improve health decision-making, behaviors, and outcomes.
Health literacy is closely related to socioeconomic status and education, thereby increasing risk for low health literacy among those who are most vulnerable. HIV/AIDS disproportionately impacts these high-risk groups (e.g., the poor and members of racial and ethnic minorities) making their low levels of health literacy a factor that complicates their health care [6, 7]. Moreover, due to advances in treatment, HIV-infected individuals now live to ages at which other chronic health problems are more common [8, 9]. While better health and longer life are the goals of HIV treatment, new challenges in achieving adequate health literacy arise as patients age with HIV. Notably, approaches for managing chronic illnesses are often different from those used to manage acute conditions [10] and older adults are at particular risk for low health literacy [6]. As the HIV/AIDS population ages and lives longer with the disease, the issue of low health literacy in this group may be particularly salient. For these reasons, continuing research to understand and improve health literacy among persons living with HIV/AIDS is vital.
Adequate health literacy may be an essential prerequisite to improving the health of HIV-infected individuals. Early studies showed that persons with low health literacy – i.e., those who had limited skill for obtaining and acting in ways to benefit their health – had lower HIV disease related knowledge [11] and were less likely to take and adhere to antiretroviral medications [12, 13]. Whether low health literacy then leads to more advanced disease has not been established and has remained a topic of continued interest [11, 12, 14, 15].
In order to promote continued research on the impact of health literacy on health among persons living with HIV/AIDS, it is important to periodically evaluate the research literature to better understand what is known, what questions remain, and future directions. This review will focus on the current state of knowledge regarding the impact of health literacy on the health outcomes of HIV-infected individuals. Observations and implications for future study in the area will also be explicated.
Methods
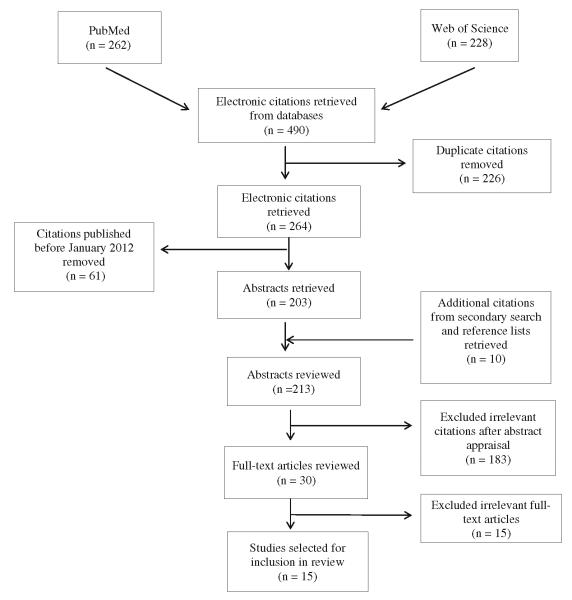
An electronic literature search was conducted in PubMed and Web of Science. In order to obtain the most relevant articles, the terms health literacy and HIV were searched for in the title and abstract in PubMed and as a topic search in Web of Science. Articles were included if the reference reported empirical data that addressed the relation of health literacy to any type of health outcome in persons infected with HIV; there were no limits placed on publication language and all study designs were included.
A secondary search was then conducted to expand the scope of health literacy to include general health knowledge. Additional articles were obtained from performing a manual search of the reference lists from all of the results. To focus on the current knowledge in the field, the final review included the studies published between January 2012 and July 2013.
Results
Fifteen articles met the criteria for inclusion in the review. Three pertained to health literacy and HIV prevention, and ten focused on the impact of health literacy on health outcomes in those with HIV. Figure 1 displays the flow chart that generated the articles for the review. Measures typically used to assess health literacy in these articles were the Test of Functional Health Literacy in Adults (TOFHLA) [16, 17], and the Short-TOFHLA (S-TOFHLA) [17]. Other scales, such as those measuring HIV or antiretroviral therapy (ART) knowledge, were used less often. Outcome measures included medication adherence, HIV viral load, and CD4 cell counts. Where applicable, studies that used both subjective and objective measurements of these outcome measures were included. Studies that statistically tested the relation of health literacy or HIV knowledge to health outcomes were considered of particular importance; these studies are denoted with a double bullet and summarized in Table 1. Taken together, recent studies have evaluated the impact of health literacy on health behaviors and outcomes in HIV by investigating the efficacy of interventions to improve health literacy, by examining the role of social support in understanding medical information, and by pioneering the use of technology to improve health literacy. Discrepant findings on the relation of health literacy to health outcomes can likely be attributed to the varying measures of health literacy and definitions of health outcomes. Key findings are presented below.
Fig. 1.
Systematic literature review flow diagram
Table 1.
Summary of reviewed studies
| Reference | Study design | Participants | Health literacy/HIV knowledge measures |
Literacy or knowledge categorization |
Health outcome measure | Association between health literacy & health outcomes? |
|---|---|---|---|---|---|---|
| [21••] Jones et al., 2012 |
Cross-sectional survey |
210 adults (mean age=47 years) |
Knowledge of CD4 count and viral load |
Dichotomized: knew both their CD4 count and viral load or did not know both measures |
Viral load dichotomized: undetectable (<20 copies/mL) or detectable (>20 copies/mL); CD4 count analyzed as continuous variable |
Greater knowledge predicted higher CD4 count and undetectable viral loads |
| [22••] Nelsen et al., 2012 |
Instrument validation |
287 adults (mean age= 50.8 +9.9 years) |
Intention to Adhere to HIV Treatment Scale |
Analyzed as continuous variable | Viral load dichotomized: undetectable (<400 copies/mL) or detectable (>400 copies/mL) |
Higher intention to adhere to treatment and HIV knowledge increased the odds of viral suppression |
| [25••] Nachega et al., 2012 |
Cross-sectional survey |
2035 adults | ATLIS | Dichotomous knowledge questions |
Self-report 30-day medication adherence; Dichotomous measure, missed >1 tablet |
Higher ART adherence rates in those who had discussed adherence with their health care providers and knew about medication effectiveness and HIV drug resistance |
| [30••] Kalichman et al., 2013 |
Intervention | 446 adults | TOFHLA | Dichotomized: marginal literacy (85-90 %) or lower literacy (<85 %) |
Viral load dichotomized: undetectable (<50 copies/mL) or detectable (>50 copies/mL); Unannounced pill count adherence analyzed continuously |
Differential improvement in outcomes based on intervention type and health literacy |
| [37••] Ownby et al., 2012 |
Intervention | 118 adults (mean age= 47.1+8.69 years) |
TOFHLA | Analyzed as continuous variable | MEMs percent correct; Analyzed as continuous variable |
Increase in information predicted better medication adherence |
| [41••] Ownby et al., 2013 |
Instrument validation |
122 adults (mean age= 47.1+8.69 years) |
HIV-HL | Analyzed as continuous variable | MEMs percent taken, correct, & scheduled; Analyzed as continuous variable |
Significant, positive correlation between HIV-HL and MEMS measures |
| [49••] Colbert et al., 2013 |
Cross-sectional survey |
302 adults (mean age= 43.9+7.94) |
S-TOFHLA | Dichotomized: inadequate/marginal (<75) or adequate (>75) |
MEMs percent days correct; Dichotomized: adherent (>85 %) or non-adherent (<85 %) |
No significant association between health literacy and medication adherence |
| [50••] Navarra et al., 2013 |
Cross-sectional survey |
50 adolescents (mean age=19.7+ 3.13 years) |
TOFHLA | Dichotomized: inadequate (<75) or adequate (>75) |
3 day self-report adherence; Dichotomized: <100 % adherent or 100 % adherent; undetectable (<400 copies/mL) or detectable (>400 copies/mL) |
No significant association between health literacy and medication adherence nor viral suppression |
ATLIS: AIDS Treatment for Life International Survey; HIV-HL: HIV-Related Health Literacy Scale; MEMS: Medication Event Monitoring System; TOFHLA: Test of Functional Health Literacy in Adults; S-TOFHLA: Short Test for Functional Health Literacy in Adults
Observational Studies Relating Health Literacy to Health Behaviors
Health Literacy and Retention in HIV Care
Linkage and retention in HIV care is an essential component of effective disease management [18, 19]. Research on health literacy and retention in care has only recently emerged but suggests that patients’ health literacy may be important [20]. A key index of engagement in care is the extent to which patients attend appointments for routine care. Jones et al. [21••] reported that adequate health literacy, defined as a patients’ knowledge of their viral load and CD4 count, more than doubled the odds of attending more than 75 % of scheduled appointments for HIV care. Along with a good provider relationship, HIV knowledge was also associated with higher CD4 counts and greater odds of viral suppression [21••].
HIV Knowledge, Treatment-Seeking Intention, and HIV Suppression
In developing a measure for intention to adhere to HIV treatment, Nelsen and colleagues [22••] administered a survey to 287 adults infected with HIV (89.0 % male, mean age=50.8 years) at two HIV clinics in Houston, Texas. The survey measured both intention and HIV knowledge and demonstrated good internal consistency and predictive validity for both constructs. Importantly, greater intention and HIV knowledge were associated with better HIV viral suppression (HIV-1 viral load <400 RNA copies/mL) [22••]. This study underscores how objective health outcomes are impacted not only by HIV knowledge but also the patient’s intention to adhere to treatment.
Health Literacy and Social Support
It has been suggested that social support may be a mechanism to compensate for low health literacy [23]. However, in HIV-infected populations, the evidence currently available does not support this observation. In a study of 474 participants with lower health literacy skills, those who requested assistance in reading, interpreting, and understanding medical information were compared to those who did not ask for help [24•]. Those who requested assistance had lower health literacy and numeracy and less education. This group also reported greater utilization of multiple adherence strategies. Despite this, participants who asked for assistance had significantly poorer medication adherence and significantly less frequent suppression of HIV replication. These findings indicate that even though persons with low health literacy may ask for help navigating medical information, this help may not be sufficient. This counterintuitive finding could be the result of several factors. Low health literacy is inextricably linked to socioeconomic status suggesting that other people that these patients rely on for assistance may also be challenged by limited health literacy. Additionally, patients do not necessarily disclose difficulties in reading or understanding medical information due to such social evaluative factors as shame or embarrassment. Moreover, participants requesting assistance had lower health literacy and therefore may have been at risk for intentional non-adherence; the adherence strategies used by these participants would be ineffective when knowingly choosing to skip a medication dose. As noted earlier, health literacy requires cognitive/decision-making skills. The extent to which the type of assistance measured in this study can impact these skills is not well understood and may be important for future studies.
Health Literacy in HIV/AIDS across the Globe
Data on the relationship of health literacy to HIV/AIDS treatment knowledge and behaviors in the global arena are scarce. Nachega and colleagues [25••] measured health knowledge as part of the AIDS Treatment for Life International Survey (ATLIS) in five global regions including the United States, Brazil, Europe, Asia Pacific, and Africa. Health outcomes were measured using a single item that asked if respondents recalled missing one or more ART tablets in the past 30 days. Aside from reporting differences between countries, the authors found significantly greater ART adherence rates amongst participants who had discussed adherence issues with their health care providers (57 % vs. 50 %), in those who understood that suboptimal adherence can result in medications losing effectiveness (55 % vs. 36 %), and those who understood the meaning of HIV drug resistance (83 % vs. 72 %).
Validated health literacy measures for use in contexts outside of the United States are essential yet virtually nonexistent. Research has been done to adapt measures of general literacy into other languages [26•] along with measures specific to HIV knowledge, such as the HIV Knowledge 27 Scale for use in Mozambique [27•]. Health literacy research among PLWH globally is increasing. Thorough validation of measures that address not only linguistic translations but also meet equivalence standards for a particular cultural context are essential to move this area forward.
Interventions to Improve Health Behaviors and Health Outcomes in Persons Living with HIV/AIDS
Interventions Targeting PLWH with Low Health Literacy
A number of studies show that health literacy is associated with antiretroviral medication adherence [12, 28, 29]. Kalichman et al. [30••] developed an intervention aimed to improve medication adherence and HIV viral load for HIV-infected persons with moderate to low health literacy. This study randomly assigned 446 HIV-infected individuals on antiretroviral therapy to pictograph-guided adherence counseling (intervention components presented as pictograph-guided instructions with minimal wording), standard adherence counseling (educational information with text and illustrations), and a general health improvement counseling control group; all conditions used the Social-Cognitive Theory of behavior change [31, 32]. Participants were grouped as having marginal (TOFHLA score between 85 and 90 % correct) or lower health literacy (TOFHLA score <85 % correct).
A greater proportion of participants with marginal literacy were considered virally suppressed (<50 copies/mL) in the pictograph-guided (40 %) and standard adherence conditions (45 %) than in the general health improvement condition (33 %), while lower literacy participants had better viral suppression in the standard adherence (35 %) and general health improvement conditions (40 %) compared to those who received pictograph-guided counseling (28 %) [30••]. For the medication adherence outcome, marginal health literacy participants had greater adherence in the pictograph-guided and standard adherence conditions compared to the general health improvement counseling; lower health literacy participants had greater adherence in the general health improvement condition than in either of the two adherence counseling groups. Taken together, Kalichman et al. [30••] surmised that those with only modest health literacy deficits may best be served by brief and focused adherence counseling, whereas those with greater literacy deficits benefit from more intensive provider-directed adherence interventions. It should be noted that cognitive impairment has been consistently associated with lower adherence in HIV [13, 33] and can further reduce adherence in those with low health literacy [34]. Cognition may have been a relevant factor in the above study. Since no measure of cognitive functioning was included in this study, it is not possible to determine the extent to which participants’ cognitive function may have influenced findings.
Culturally Tailored Interventions
Previous research has reported on the mediating effects of health literacy on the relationship between race and HIV medication adherence in underserved and underrepresented populations of HIV-infected individuals [1, 14, 35]. African Americans comprise one such group. Rikard et al. [36•] detailed the development of a peer-to-peer, culturally-tailored HIV/AIDS health literacy toolkit designed to disseminate HIV/AIDS health information using teach-back methods. Development of the toolkit was initiated from the understanding that health literacy should include factors such as culture. This study details methods for effective engagement with African American community members and community service organizations to inductively create a tool accepted by and relevant to that community. Although this qualitative study did not report outcomes from implementation of the toolkit, it identified factors affecting prevention and treatment efforts in the African-American community. Studies such as these can guide further research into culturally-tailored interventions in improving health literacy.
The Use of Technology to Improve Health Literacy
The mainstream use of portable devices such as laptops, tablet computers, and smartphones has expanded the tools for interventions aimed at improving health literacy. Ownby et al. [37••] targeted participants’ health literacy as a strategy to increase antiretroviral medication adherence using a computer-delivered intervention program based on the Information-Motivation-Behavioral Skills Model (IMB) [38]. Touch screen computers delivered a one hour multimedia presentation supplemented with multiple choice questions to assess patients’ learning. The TOFHLA [16] was used to measure health literacy, medication adherence was recorded with the Medication Event Monitoring System (MEMS; Aardex Group Ltd, Sion, Switzerland) and elements of the IMB were measured using the LifeWindows IMB scale [39]. After the intervention, adherence significantly improved among participants with baseline levels of adherence less than 95 % even after adjusting for participants’ cognitive functioning and baseline health literacy. Further, results suggested that those with lower baseline levels of adherence showed the greatest increases in adherence after the intervention [37••]. Overall, participants had relatively high baseline levels of medication adherence that may have diminished intervention effects, and the study did not include a control group. However, the study successfully established the feasibility and proof of concept of employing a computer-based intervention to improve health literacy; the intervention was also shown to be cost effective [40•].
Technology has also expanded the way in which health literacy can be measured. The 20-item, computer delivered HIV Health Literacy Scale (HIV-HL) was developed to create an automatically administered and scored health literacy measure specifically focused on HIV/AIDS [41••]; medication adherence using MEMS caps was measured as a secondary outcome. Patients were asked to interpret medication labels and respond to questions about the content of a video vignette portraying a simulated patient-provider interaction. The questionnaire demonstrated good content validity and was correlated with the TOFHLA [16, 17] and HIV-related knowledge [39]. The HIV-HL was effective at identifying participants with low health literacy (AUC=0.77, z=2.57, p=0.01). Additionally, the HIV-HL was significantly correlated with medication adherence [41••]. This study provides evidence for implementing technology to measure health literacy using real-world health encounters.
The use of computer-delivered interventions for HIV prevention is also increasing in countries other than the United States. For example, the Sharing Medical Adherence Responsibilities Together (SMART) Couples multimedia intervention [42, 43], which utilized social-action theory [44] as the conceptual framework to improve medication adherence, has recently been translated into Xhosa and adapted for a South African population to deliver a culturally-tailored intervention in the region of the world most affected by HIV [45•].
Lack of Associations between Health Literacy and Health Outcomes
Despite a number of studies reporting a significant relation between health literacy and outcomes, some recent studies have not supported this finding. Nelsen et al. [46•] conducted a study with 244 adult participants (92 % male; mean age=51.8 years) from two HIV clinics in Houston, Texas. A self-reported survey measured HIV knowledge (four questions), awareness of disease biomarkers (one free-response question), and health literacy (one question) [46•]. Using self-reported adherence as an outcome, this study did not find a significant association between HIV knowledge, biomarker awareness, or health literacy and medication adherence. Health literacy was measured using a single question (“How confident are you filling out medical forms by yourself?”) with responses on a 5-point Likert rating scale; although previous studies have reported the predictive validity of this single-item measure and more comprehensive health literacy measures [47, 48], this single-item measure may not be an adequate measure of health literacy. Aside from the self-reported nature of the survey, failure to find significant differences between adherent and non-adherent participants might have resulted from the homogeneity of the sample’s gender, age, and source of participants (all participants were recruited from similar HIV clinics).
Colbert, Sereika, and Erlen [49••] also did not find an association between health literacy and medication adherence. Using a score of 75 % or less on the S-TOFHLA to categorize patients as having inadequate health literacy, the study did not find group differences in medication adherence as measured by self-report and MEMS caps. Potentially, the categorization of patients using a 75 % S-TOFHLA cutoff and the inclusion of a self-reported outcome may have contributed to the lack of association between health literacy and medication adherence reported in this study.
Several recent studies with HIV-infected adolescents have also failed to confirm the relation between health literacy and outcomes. Navarra, Neu, Toussi et al. [50••] used the TOFHLA [16] and the Rapid Estimate of Adult Literacy in Medicine-teen (REALM-teen) [51] to evaluate the relation between health literacy and three-day self-reported medication adherence in 50 HIV-infected adolescents (mean age=19.7 years). Using a multivariate logistic regression model that included health literacy, positive outcome expectancy, reading level, and substance use as predictors, they found that health literacy did not predict self-report adherence (OR=0.954, 95 % CI: 0.893-1.018, p=0.15). Potentially, the use of self-reported estimates of adherence, with 100 % adherence as the cutoff between being adherent and non-adherent, may have introduced enough measurement error to yield a lack of association between health literacy and medication adherence.
Konkle-Parker et al. [52••] used the IMB model [37••, 53] as the conceptual basis for an intervention to improve treatment adherence and disease status. Although health literacy per se was not the basis for the intervention, the goals of increased HIV knowledge, problem solving to overcome adherence barriers and education on the use of adherence tools (e.g., pill boxes) are aligned with key elements of health literacy. Participants’ health literacy with the S-TOFHLA [17] was characteriezed but it was not used in analyses. A total of 72 participants were randomized to the intervention or to usual care; the LifeWindows IMB Skills ART Adherence Questionnaire [38] was administered before and after the intervention to measure the patients’ 1) adequacy of information on HIV medication adherence, 2) degree of personal and social motivation to adhere to medication regimens, and 3) ability to implement the behaviors to adhere to the medication regimen. Self-reported adherence on a visual analogue scale and refill rate were used to measure adherence; medical appointments, viral loads, and CD4+ levels were also used as outcomes. Despite the soundness of the study’s design, there was a high level of attrition (51 %) along with some participants in the treatment group not receiving the full intervention because of missed visits. The investigators report no significant differences on any outcome variable between the treatment groups and attributed these findings to low power to detect differences.
Conclusions
The impact of health literacy on health outcomes among persons living with HIV/AIDS continues to be a growing area of research. The most recent literature in this area supports the notion that health literacy can affect knowledge of one’s disease; however, whether or not this knowledge then directly influences health behaviors among persons living with HIV/AIDS is less clear. While recent studies have shown that antiretroviral medication adherence improves after increasing HIV knowledge [36•, 45•], and that greater health literacy and/or HIV knowledge is associated with better health outcomes [21••, 22••, 25••, 41••], others have not found evidence in support of these associations [46•, 49••, 50••]. However, methodological differences in measures of both health literacy and medication adherence may have contributed to these disparate findings. Self-reported medication adherence and simple screening items for health literacy can have limited validity and are less desirable than other measures when attempting to understand whether interventions to improve health literacy are efficacious. Failure to control for key factors in adherence, such as cognitive status or social support, may also affect study outcomes, especially in studies with the limited power associated with small sample sizes.
The use of technology as both an assessment and an intervention tool was well represented in the recent literature. Computer-delivered health literacy assessments provide opportunity to measure health literacy beyond mere reading and numeracy ability by allowing simulations of real-world health encounters. Such stimuli provide greater ecological validity to measures. Interventions delivered via technology can reduce costs associated with providing face-to-face interventions and can potentially be adapted to mobile platforms as an ecological momentary assessment. Recent evidence suggests that health literacy evaluation and interventions delivered via technology are quite promising for future research.
Few studies were conducted within the time frame of this review that focused on specific populations at risk for low health literacy or those disproportionately affected by HIV/AIDS, although studies reported on the development of measures and interventions in different populations [26•, 27•, 36•]. One study with HIV-infected adolescents reported no relationship between health literacy and medication adherence [50••]. More studies focused on special populations (e.g., adolescents and young adults, older adults, racial/ethnic minorities) are urgently needed. HIV/AIDS affects a wide range of individuals and factors that may affect their health behaviors and outcomes may be related to their individual characteristics and barriers experienced by them.
Observations and Future Directions
For HIV-infected persons with access to antiretroviral treatments, HIV/AIDS has become a chronic condition requiring a lifetime commitment to managing the disease. Chronic disease care models advocate for patient teams that work in coordination with providers, patients, and families. These teams can teach and provide support for managing the disease, mitigating symptoms, and dealing with the social and emotional consequences of HIV [54]. Chronic disease, particularly in older adults, is rarely isolated but instead is co-morbid with a number of other chronic conditions [55]. This may be especially true for persons living and aging with HIV/AIDS since studies show the appearance of conditions common in older adults in the general population at significantly younger ages among HIV-infected individuals [56, 57]. No studies in this review were located with a focus on health literacy as a predictor or mediator/moderator of health behavior or outcomes for those with chronic conditions in addition to HIV/AIDS. Evidence shows that older adults in the general population and those with multimorbidities are at greater risk for low health literacy and may be more negatively affected by low health literacy [58]. With half of the HIV/AIDS population expected to be 50 years of age and older by 2015, health literacy should be a central component of studies with this population.
Cognitive functioning is integral in the study of aging and multimorbidity. Approximately 50 % of persons living with HIV/AIDS have some level of cognitive impairment and rates of impairment increase with age. Studies show that health literacy shares commonalities with and cannot be completely separated from cognitive functioning [1, 2]. For example, the acquisition of health information is likely affected by attention, working memory, and executive functions, and subsequent carrying out of health behaviors is further influenced by prospective memory [59] and executive functions [32]. Since health literacy is closely aligned with cognitive skill, health literacy studies with persons living with HIV/AIDS would benefit from the inclusion of measures of cognitive ability. Such studies would be informative both in terms of how health literacy is affected in populations at risk for cognitive impairment and in efforts to understand in what ways the concept of health literacy may be defined by cognitive functions.
Consistent measurement of health literacy in groups affected by HIV/AIDS is also needed. In many cases, it may be prudent to measure health literacy specific to HIV/AIDS, particularly when HIV-related health behaviors and health outcomes are of interest. The HIV-HL Scale reviewed here [41••] offers a number of advantages and builds upon growing support for technology-based assessments. General measures of health literacy (e.g., TOHFLA or REALM) may be less sensitive to detect changes in HIV-specific disease outcomes. In contrast, however, general health literacy measures may be preferable (or a valuable addition) for studies incorporating multiple chronic conditions in addition to HIV/AIDS as discussed above.
Health literacy is a complex construct that shares traits with other important foci of study. It can also impact a number of areas of health behaviors and outcomes. Methods to study these complexities require sophisticated models that can account for latent constructs that better represent the intricacies inherent in the lives of real patients. Persons living with HIV/AIDS would be better served through studies that attempt to approximate these relationships among those most impacted by low health literacy.
Footnotes
Compliance with Ethics Guidelines Conflict of Interest Andrew J. Wawrzyniak, Raymond L. Ownby, Katryna McCoy, and Drenna Waldrop-Valverde declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent This article does not contain any studies with human or animal subjects performed by any of the authors.
Contributor Information
Andrew J. Wawrzyniak, School of Nursing & Health Studies, University of Miami, 5030 Brunson Drive, Coral Gables, FL 33146, USA awawrzyniak@med.miami.edu
Raymond L. Ownby, Department of Psychiatry and Behavioral Medicine, Nova Southeastern University, 3000 South University Drive, Room 1477, Fort Lauderdale, FL 33328, USA ro71@nova.edu
Katryna McCoy, Nell Hodgson Woodruff School of Nursing, Emory University, 1520 Clifton Road NE, Atlanta, GA 30322, USA katryna.mccoy@emory.edu.
Drenna Waldrop-Valverde, Nell Hodgson Woodruff School of Nursing, Rollins School of Public Health, Department of Behavioral Sciences and Health Education, Emory University, 1520 Clifton Road NE, Atlanta, GA 30322, USA.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of major importance
- 1.Waldrop-Valverde D, Jones DL, Gould F, Kumar M, Ownby RL. Neurocognition, health-related reading literacy, and numeracy in medication management for HIV infection. AIDS Patient Care STDS. 2010;24(8):477–84. doi: 10.1089/apc.2009.0300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wolf MS, Curtis LM, Wilson EA, et al. Literacy, cognitive function, and health: results of the LitCog study. J Gen Intern Med. 2012;27(10):1300–7. doi: 10.1007/s11606-012-2079-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yost KJ, Dewalt DA, Lindquist LA, Hahn EA. The association between health literacy and indicators of cognitive impairment in a diverse sample of primary care patients. Patient Educ Couns. 2013 doi: 10.1016/j.pec.2013.07.006. doi:10.1016/j.pec.2013.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baker DW. The meaning and the measure of health literacy. J Gen Intern Med. 2006;21(8):878–83. doi: 10.1111/j.1525-1497.2006.00540.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nutbeam D. The evolving concept of health literacy. Soc Sci Med. 2008;67(12):2072–8. doi: 10.1016/j.socscimed.2008.09.050. [DOI] [PubMed] [Google Scholar]
- 6.Kutner M, Greenberg E, Jin Y, Paulsen C. Education USDoE. National Center for Education Statistics; Washington, DC: 2006. The health literacy of america’s adults: Results from the 2003 national assessment of adult literacy (NCES 2006–483) [Google Scholar]
- 7.Dewalt DA, Berkman ND, Sheridan S, Lohr KN, Pignone MP. Literacy and health outcomes: a systematic review of the literature. J Gen Intern Med. 2004;19(12):1228–39. doi: 10.1111/j.1525-1497.2004.40153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nath A. HIV and aging. J Neurovirol. 2012;18(4):245–6. doi: 10.1007/s13365-012-0111-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sackoff JE, Hanna DB, Pfeiffer MR, Torian LV. Causes of death among persons with AIDS in the era of highly active antiretroviral therapy: New York City. Ann Intern Med. 2006;145(6):397–406. doi: 10.7326/0003-4819-145-6-200609190-00003. [DOI] [PubMed] [Google Scholar]
- 10.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness. JAMA. 2002;288(14):1775–9. doi: 10.1001/jama.288.14.1775. [DOI] [PubMed] [Google Scholar]
- 11.Kalichman SC, Benotsch E, Suarez T, et al. Health literacy and health-related knowledge among persons living with HIV/AIDS. Am J Prev Med. 2000;18(4):325–31. doi: 10.1016/s0749-3797(00)00121-5. [DOI] [PubMed] [Google Scholar]
- 12.Kalichman SC, Rompa D. Functional health literacy is associated with health status and health-related knowledge in people living with HIV-AIDS. J Acquir Immune Defic Syndr. 2000;25(4):337–44. doi: 10.1097/00042560-200012010-00007. [DOI] [PubMed] [Google Scholar]
- 13.Waldrop-Valverde D, Ownby RL, Wilkie FL, et al. Neurocognitive aspects of medication adherence in HIV-positive injecting drug users. AIDS Behav. 2006;10(3):287–97. doi: 10.1007/s10461-005-9062-6. [DOI] [PubMed] [Google Scholar]
- 14.Paasche-Orlow MK, Cheng DM, Palepu A, et al. Health literacy, antiretroviral adherence, and HIV-RNA suppression: a longitudinal perspective. J Gen Intern Med. 2006;21(8):835–40. doi: 10.1111/j.1525-1497.2006.00527.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kalichman SC, Rompa D. Emotional reactions to health status changes and emotional well-being among HIV-positive persons with limited reading literacy. J Clin Psychol Med Settings. 2000;7(4):203–11. [Google Scholar]
- 16.Parker RM, Baker DW, Williams MV, Nurss JR. The test of functional health literacy in adults: a new instrument for measuring patients’ literacy skills. J Gen Intern Med. 1995;10(10):537–41. doi: 10.1007/BF02640361. [DOI] [PubMed] [Google Scholar]
- 17.Baker D, Williams M, Parker R, Gazmararian J, Nurss J. Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999;38(1):33–42. doi: 10.1016/s0738-3991(98)00116-5. [DOI] [PubMed] [Google Scholar]
- 18.Mugavero MJ, Amico KR, Westfall AO, et al. Early retention in HIV care and viral load suppression: implications for a test and treat approach to HIV prevention. J Acquir Immune Defic Syndr. 2012;59(1):86–93. doi: 10.1097/QAI.0b013e318236f7d2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gardner EM, McLees MP, Steiner JF, Del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis. 2011;52(6):793–800. doi: 10.1093/cid/ciq243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mallinson RK, Relf MV, Dekker D, et al. Maintaining normalcy: a grounded theory of engaging in HIV-oriented primary medical care. ANS Adv Nurs Sci. 2005;28(3):265–77. doi: 10.1097/00012272-200507000-00008. [DOI] [PubMed] [Google Scholar]
- 21 ••.Jones D, Cook R, Rodriguez A, Waldrop-Valverde D. Personal HIV knowledge, appointment adherence and HIV outcomes. AIDS Behav. 2013;17(1):242–9. doi: 10.1007/s10461-012-0367-y. Higher HIV knowledge, defined as a patient knowing their CD4 count and viral load, more than doubled the odds of appointment adherence and was associated with higher CD4 counts and greater viral suppression.
- 22 ••.Nelsen A, Trautner BW, Petersen NJ, et al. Development and validation of a measure for intention to adhere to HIV treatment. Aids Patient Care STDS. 2012;26(6):329–34. doi: 10.1089/apc.2011.0318. Aside from establishing the internal consistency and validity of measure to assess intention to adhere to treatment and HIV knowledge, the study reported better HIV suppression in those with greater levels of intention and knowledge.
- 23.Lee SY, Arozullah AM, Cho YI. Health literacy, social support, and health: a research agenda. Soc Sci Med. 2004;58(7):1309–21. doi: 10.1016/S0277-9536(03)00329-0. [DOI] [PubMed] [Google Scholar]
- 24 •.Kalichman S, Pellowski J, Chen Y. Requesting help to understand medical information among people living with HIV and poor health literacy. AIDS Patient Care STDS. 2013;27(6):326–32. doi: 10.1089/apc.2013.0056. AIDS Patient Care and STDS. 2013;27(6):326–332. doi: 10.1089/apc.2013.0056. This study found that social support in comprehending medical information increased the use of adherence improvement strategies but had worse medication treatment adherence and worse viral replication suppression.
- 25 ••.Nachega JB, Morroni C, Zuniga JM, et al. HIV treatment adherence, patient health literacy, and health care provider-patient communication: results from the 2010 AIDS treatment for life international survey. J Int Assoc Physicians AIDS Care. 2012;11(2):128–33. doi: 10.1177/1545109712437244. In addition to differences in HIV knowledge and ART adherence between countries, this study found better ARTadherence rates in those who had discussed adhence with their health care providers, understood that suboptimal adherence may decrease medication effectiveness, knew about the negative impact of drug resistance.
- 26 •.Ciampa PJ, Vaz LME, Blevins M, et al. The association among literacy, numeracy, HIV knowledge and health-seeking behavior: a population-based survey of women in rural Mozambique. Plos One. 2012;7(6):e39391. doi: 10.1371/journal.pone.0039391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27 •.Ciampa PJ, Skinner SL, Patricio SR, et al. Comprehensive knowledge of HIV among women in rural mozambique: development and validation of the HIV knowledge 27 scale. Plos One. 2012;7(10):e48676. doi: 10.1371/journal.pone.0048676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kalichman SC, Catz S, Ramachandran B. Barriers to HIV/AIDS treatment and treatment adherence among African-American adults with disadvantaged education. J Natl Med Assoc. 1999;91(8):439–46. [PMC free article] [PubMed] [Google Scholar]
- 29.Kalichman SC, Pope H, White D, et al. Association between health literacy and HIV treatment adherence: further evidence from objectively measured medication adherence. J Int Assoc Phys AIDS Care. 2008;7(6):317–23. doi: 10.1177/1545109708328130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30 ••.Kalichman SC, Cherry C, Kalichman MO, et al. Randomized clinical trial of HIV treatment adherence counseling interventions for people living with HIV and limited health literacy. J Acquir Immune Defic Syndr. 2013;63(1):42–50. doi: 10.1097/QAI.0b013e318286ce49. Those with modest health literacy deficits had greater viral suppression and medication adherence after focused adherence counseling interventions specific to improving HIV medication regiment adherence; lower health literacy patients had better health outcomes from a more intensive, provider-directed general health knowledge intervention.
- 31.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 32.Bandura A. Self-Efficacy in Changing Societies. Cambridge University Press; New York , NY: 1995. [Google Scholar]
- 33.Hinkin CH, Hardy DJ, Mason KI, et al. Medication adherence in HIV-infected adults: effect of patient age, cognitive status, and substance abuse. AIDS. 2004;18(Suppl 1):S19–25. doi: 10.1097/00002030-200418001-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Waldrop-Valverde D, Jones DL, Weiss S, Kumar M, Metsch L. The effects of low literacy and cognitive impairment on medication adherence in HIV-positive injecting drug users. AIDS Care. 2008;20(10):1202–10. doi: 10.1080/09540120801927017. [DOI] [PubMed] [Google Scholar]
- 35.Osborn CY, Paasche-Orlow MK, Davis TC, Wolf MS. Health literacy: an overlooked factor in understanding HIV health disparities. Am J Prev Med. 2007;33(5):374–8. doi: 10.1016/j.amepre.2007.07.022. [DOI] [PubMed] [Google Scholar]
- 36 •.Rikard RV, Thompson MS, Head R, McNeil C, White C. Problem posing and cultural tailoring: developing an HIV/AIDS health literacy toolkit with the African American community. Health Promo Pract. 2012;13(5):626–36. doi: 10.1177/1524839911416649. Describes the development of a culturally tailored health literacy training program geared toward the African American community.
- 37 ••.Ownby RL, Waldrop-Valverde D, Caballero J, Jacobs RJ. Baseline medication adherence and response to an electronically delivered health literacy intervention targeting adherence. Neurobehav HIV Med. 2012;4:113–21. doi: 10.2147/NBHIV.S36549. An interactive computer-based intervention designed to improve health literacy was associated with better adherence, with larger post-intervention increases in adherence among those with lower baseline adherence.
- 38.Fisher JD, Fisher WA, Amico KR, Harman JJ. An information-motivation-behavioral skills model of adherence to antiretroviral therapy. Health Psychol. 2006;25(4):462–73. doi: 10.1037/0278-6133.25.4.462. [DOI] [PubMed] [Google Scholar]
- 39.The LifeWindows Project Team . The LifeWindows information motivation behavioral skills ART adherence questionnaire (LWIMB-AAQ) Center for Health, Intervention, and Prevention, University of Connecticut; Storrs: 2006. [Google Scholar]
- 40 •.Ownby RL, Waldrop-Valverde D, Jacobs RJ, Acevedo A, Caballero J. Cost effectiveness of a computer-delivered intervention to improve HIV medication adherence. BMC Med Inform Decis Mak. 2013;13:29. doi: 10.1186/1472-6947-13-29. A computer-delivered intervention to improve adherence showed favorable cost/benefit ratios when intervention effects persisted for as little as three months.
- 41 ••.Ownby RL, Waldrop-Valverde D, Hardigan P, et al. Development and validation of a brief computer-administered HIV-related health literacy scale (HIV-HL) AIDS Behav. 2013;17(2):710–8. doi: 10.1007/s10461-012-0301-3. The HIV-HL employs real-world, multimedia-based questions delivered via computer to measure health literacy; the HIV-HL had good internal reliability and external validity and was able to identify participants with low health literacy. The measure was positively correlated to medicadtion ahderence.
- 42.Remien RH, Stirratt MJ, Dolezal C, et al. Couple-focused support to improve HIV medication adherence: a randomized controlled trial. AIDS. 2005;19(8):807–14. doi: 10.1097/01.aids.0000168975.44219.45. [DOI] [PubMed] [Google Scholar]
- 43.Remien RH, Stirratt MJ, Dognin J, et al. Moving from theory to research to practice. Implementing an effective dyadic intervention to improve antiretroviral adherence for clinic patients. J Acquir Immune Defic Syndr. 2006;43(Suppl 1):S69–78. doi: 10.1097/01.qai.0000248340.20685.7d. [DOI] [PubMed] [Google Scholar]
- 44.Ewart CK. Social action theory for a public health psychology. Am Psychol. 1991;46(9):931–46. doi: 10.1037//0003-066x.46.9.931. [DOI] [PubMed] [Google Scholar]
- 45 •.Remien RH, Mellins CA, Robbins RN, et al. Masivukeni: development of a multimedia based antiretroviral therapy adherence intervention for counselors and patients in South Africa. AIDS Behav. 2013;17(6):1979–91. doi: 10.1007/s10461-013-0438-8. This article describes the foundations of a social-action theory multimedia intervention adapted for South African PLWHA.
- 46 •.Nelsen A, Gupta S, Trautner B, et al. Intention to adhere to HIV treatment: a patient-centred predictor of antiretroviral adherence. HIV Med. 2013;14(8):472–80. doi: 10.1111/hiv.12032. Health literacy, measured by a single item, and general HIV knowledge, measured by 4 questions, nor a free-response question pertaining to HIV biomarkers were not significant predictors of HAARTadherence in a predominantly male, middle-aged sample of PLWHA, mainly recruited from a VA Medical Center; the characteristics of the sample may limit generalizability to more diverse populations and the health literacy measures may not be measuring all salient health literacy constructs.
- 47.Wallace LS, Rogers ES, Roskos SE, Holiday DB, Weiss BD. Brief report: screening items to identify patients with limited health literacy skills. J Gen Intern Med. 2006;21(8):874–7. doi: 10.1111/j.1525-1497.2006.00532.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chew LD, Griffin JM, Partin MR, et al. Validation of screening questions for limited health literacy in a large VA outpatient population. J Gen Intern Med. 2008;23(5):561–6. doi: 10.1007/s11606-008-0520-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49 ••.Colbert AM, Sereika SM, Erlen JA. Functional health literacy, medication-taking self-efficacy and adherence to antiretroviral therapy. J Adv Nurs. 2013;69(2):295–304. doi: 10.1111/j.1365-2648.2012.06007.x. This study did not find a significant association between health literacy and ART adherence, but used a cutoff of 75 % to classify patients as having inadequate/marginal or adequate health literacy; these cutoffs differ from other studies.
- 50 ••.Navarra AM, Neu N, Toussi S, Nelson J, Larson EL. Health literacy and adherence to antiretroviral therapy among HIV-infected youth. J Assoc Nurses AIDS Care. 2013 doi: 10.1016/j.jana.2012.11.003. In press. doi:10.1016/j.jana.2012.11.003. This study on 50 adolescents and young adults did not find an association between health literacy and medication adherence, but had dichotomized self-reported medication adherence into adherence/non-adherence with 100 % adherence as the cutoff between groups; potentially, a ceiling effect on medication adherence rates may have contributed to the lack of a significant association.
- 51.Davis TC, Wolf MS, Arnold CL, et al. Development and validation of the rapid estimate of adolescent literacy in medicine (REALM-Teen): a tool to screen adolescents for below-grade reading in health care settings. Pediatrics. 2006;118(6):e1707–14. doi: 10.1542/peds.2006-1139. [DOI] [PubMed] [Google Scholar]
- 52 ••.Konkle-Parker DJ, Erlen JA, Dubbert PM, May W. Pilot testing of an HIV medication adherence intervention in a public clinic in the Deep South. J Am Acad Nurse Pract. 2012;24(8):488–98. doi: 10.1111/j.1745-7599.2012.00712.x. This study attempted to use an intervention to increase health literacy by targeting information, motivation, and behavior in improving medication adherence as its primary outcome; unfortunately, due to high attrition, no significant differences were found on any variable between the intervention group and the usual care group.
- 53.Fisher JD, Amico KR, Fisher WA, Harman JJ. The information-motivation-behavioral skills model of antiretroviral adherence and its applications. Curr HIV/AIDS Rep. 2008;5(4):193–203. doi: 10.1007/s11904-008-0028-y. [DOI] [PubMed] [Google Scholar]
- 54.Wagner EH, Groves T. Care for chronic diseases. BMJ. 2002;325(7370):913–4. doi: 10.1136/bmj.325.7370.913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Valderas JM, Starfield B, Sibbald B, Salisbury C, Roland M. Defining comorbidity: implications for understanding health and health services. Ann Fam Med. 2009;7(4):357–63. doi: 10.1370/afm.983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Pathai S, Lawn SD, Gilbert CE, et al. Accelerated biological ageing in HIV-infected individuals in South Africa: a case-control study. AIDS. 2013;27(15):2375–84. doi: 10.1097/QAD.0b013e328363bf7f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Galescu O, Bhangoo A, Ten S. Insulin resistance, lipodystrophy and cardiometabolic syndrome in HIV/AIDS. Rev Endocr Metab Disord. 2013;14(2):133–40. doi: 10.1007/s11154-013-9247-7. [DOI] [PubMed] [Google Scholar]
- 58.Wolf MS, Gazmararian JA, Baker DW. Health literacy and functional health status among older adults. Arch Intern Med. 2005;165(17):1946–52. doi: 10.1001/archinte.165.17.1946. [DOI] [PubMed] [Google Scholar]
- 59.Doyle KL, Loft S, Morgan EE, et al. Prospective memory in HIV-associated neurocognitive disorders (HAND): the neuropsychological dynamics of time monitoring. J Clin Exp Neuropsychol. 2013;35(4):359–72. doi: 10.1080/13803395.2013.776010. [DOI] [PMC free article] [PubMed] [Google Scholar]