Abstract
A handful of the many changes resulting from the Affordable Care Act underscore the need for a geographic understanding of existing and prospective member communities. Health exchanges require that health provider networks are geographically accessible to underserved populations, and nonprofit hospitals nationwide are required to conduct community health needs assessments every three years. Beyond these requirements, health care providers are using maps and spatial analysis to better address health outcomes that are related in complex ways to social and economic factors.
Kaiser Permanente is applying geographic information systems, with spatial analytics and map-based visualizations, to data sourced from its electronic medical records and from publicly and commercially available datasets. The results are helping to shape an understanding of the health needs of Kaiser Permanente members in the context of their communities. This understanding is part of a strategy to inform partnerships and interventions in and beyond traditional care delivery settings.
Introduction
During the past decade, the use of geographic information systems (GIS) for mapping and spatial analytics has evolved at Kaiser Permanente (KP). With roots in care delivery facilities planning, GIS next became an important part of KP’s effort to illuminate disparities in care and improve quality of care. More recently, the Patient Protection and Affordable Care Act (ACA)1 is reinforcing the need for a geographic understanding of existing and prospective member communities, including health status and outcomes, access to care, and cultural preferences.2 For example, state and federal health exchanges require evidence that health provider networks are geographically accessible to underserved populations.3,4 The ACA also mandates that nonprofit hospitals conduct a community health needs assessment every three years.5 Other health systems have similarly recognized the utility of GIS to understand primary care needs at the community level6 and to galvanize multisector collaborations to better address health outcomes that are related in complex ways to social and economic factors.7
This article highlights two recent projects required by the ACA in which GIS played an important role: 1) measuring network adequacy and 2) conducting community health needs assessments. We also outline a GIS-based approach that uses data from KP’s electronic health record (EHR) to identify neighborhood-level spatial variation in the prevalence of chronic conditions. Developed as a complement to the community health needs assessment process, the resulting hot spot maps protect patient/member confidentiality, while showing that the variation in health outcomes is often spatially correlated with social determinants across the community. Last, we discuss other uses for hot spot mapping, geospatial analytics, and the evolving role of GIS in targeting community-based disease prevention and management efforts.
In health care organizations, great care must be taken when working with protected health information using any technology. The use of GIS technology is no exception, for reasons ranging from compliance with the Health Insurance Portability and Accountability Act (HIPAA) to preventing un-ethical targeting of groups on the basis of race, ethnicity, or sociodemographics. For these reasons, much of our efforts focus on protecting individual confidentiality when working with data from KP members’ EHRs.
Measuring Network Adequacy and Accessibility
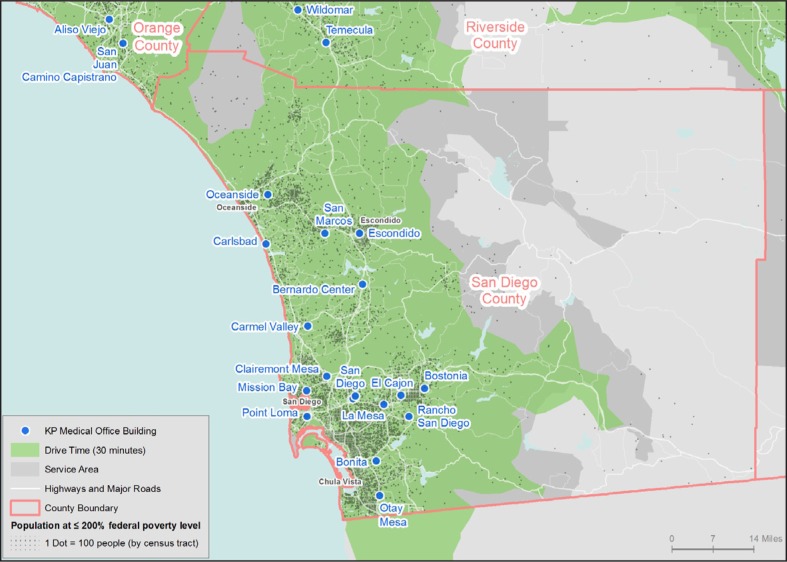
Health exchanges are an important vehicle for making health insurance available via the ACA. The application process requires health plans to report network adequacy in geographically specific ways. For example, the Qualified Health Plan application for California’s Health Benefit Exchange required time (30 minutes) and distance (15 miles) calculations from low-income populations (≤ 200% of federal poverty level) to primary care physicians across all counties where the Health Plan would offer insurance. GIS tools were used to measure accessibility via the street network between the low-income population and KP care delivery locations. Although not originally required, KP’s internal project team requested maps, which were ultimately submitted as part of the application. As an example, the map for San Diego County (Figure 1, enlarged, full-color version is available online at: www.thepermanente-journal.org/images/Spring2014/GIS1.jpg) indicates that very few low-income residents live beyond a 30-minute drive to KP primary care locations.
Figure 1.
Network access to Kaiser Permanente (KP) primary care sites. Enlarged, full-color version is available at: www.thepermanentejournal.org/images/Spring2014/GIS1.jpg.
Similarly, the federal requirements measure access to care providers by focusing on high-need zip codes. These zip codes have been designated as a Health Professional Shortage Area by the US Department of Health and Human Services Health Resources and Services Administration or have a high percentage (≥30%) of the population living at or below 200% of the federal poverty level. The number of primary care physicians in the Health Plan who practice in or adjacent to these high-need zip codes are compared with the number of Essential Community Providers, as defined by the Health Resources and Services Administration.8 This measure ensures that the Health Plan provides at-risk populations with sufficient geographic access to care providers, and GIS analysis was necessary to answer the question of zip code adjacency. Although measures of network adequacy may evolve in the face of more virtual access to care (eg, telemedicine, care coordination, and broadband access in rural areas), geographically based measures of network adequacy will continue to require GIS technology for accurate measurement and reporting.
Supporting Community Health Needs Assessment
Since 1994, the state of California has required that nonprofit hospitals develop and implement community health needs assessments.9 Starting in 2013, the ACA requires community health needs assessments for nonprofit hospitals nationwide to be repeated every three years to identify changes in health needs.1 This requirement aligns well with KP’s mission to provide high-quality, affordable health care services and to improve the health of our members and the communities we serve.
Building on years of experience with community health needs assessments in California and inspired by the ACA mandate, KP conducted a project to support the community health needs assessment process. A crossfunctional team from KP identified indicators and benchmarks, developed toolkits to outline workflows, and partnered with the Institute for People, Place & Possibility in Columbia, MO, and the Center for Applied Research and Environmental Systems at the University of Missouri, Columbia, to build a Web-based reporting and mapping tool. The resulting data platform (www.CHNA.org/KP) streamlines access to a broad set of data indicators, helping planners to explore and to learn about the health needs of a community, and to produce tables, charts, interactive maps, and reports to communicate their findings.10 The community health needs assessment indicators are organized into categories: demographics, social and economic factors (eg, crime, education, poverty), physical environment (eg, fast food, parks, and air quality), clinical care (eg, access to preventive care), health behaviors (eg, eating fruits and vegetables), and health outcomes (eg, diabetes prevalence). Together these indicators provide insight on health outcomes and clinical care as well as upstream factors that also have an impact on health. In partnership with the Centers for Disease Control and Prevention in Atlanta, GA, the Institute for People, Place & Possibility, and the Center for Applied Research and Environmental Systems, KP has provided the CHNA.org platform as a free GIS community asset to support community health needs assessment efforts nationwide.11
Data challenges still exist, however. Although many states are recognizing the limitations of publicly available health data and taking initial steps to address these limitations (eg, All Payer All Claims Database in Oregon and California’s Free the Data initiative), many important public health statistics are still reported only at the state or county levels. From a national perspective, these statistics provide useful benchmarks, as they can be trended over time and indicate regional variation. However, overaggregation can mask underlying disparities,12 limiting efforts to target interventions and detect changes at the local level.
Mapping Neighborhood-Level Geographic Variation in Health Outcomes
In Summer 2012, we piloted an internal project to address the lack of neighborhood-level insight regarding health outcomes across seven KP Regions in eight states (CA, CO, GA, HI, MD, OR, VA, and WA) and the District of Columbia. We used data derived from KP’s EHR to produce neighborhood-level hot spot maps of disease prevalence in KP member communities for high-impact chronic conditions: adult and child obesity, asthma, diabetes, heart disease, and hypertension. We also analyzed self-reported physical activity measures, referred to as “Exercise as a Vital Sign,” for several Regions. To protect member privacy while providing actionable insights, we scored neighborhoods by how their prevalence rate compared with the regional KP average rate, but no absolute rates were communicated and no member-level data were presented.
Using GIS tools, we geocoded each member’s home address and aggregated member-level health outcomes to the census tract, providing an initial level of protection for member/patient identifiable information. Regions of KP range in size from a few hundred thousand to more than 3 million members, representing up to 30% or more of the total population in some census tracts. Table 1 lists the number of tracts by Region. Although perhaps imperfect for our purposes, census tracts are intended to be socioeconomically homogeneous, and they have origins in public health applications.13 This level of aggregation provided a balance between detailed geographic measurement, adequate sample size, and individual privacy.12 After aggregating member-level chronic conditions data into census tract rates, we used a documented approach with origins in analysis of medication adherence14 to determine 1) whether individual tract rates stood out compared with other tracts in the Region and then 2) whether there were entire neighborhood rates that stood out compared with the KP Region.
Table 1.
Number of census tracts analyzed in each Kaiser Permanente (KP) Region
| KP Region | Number of census tracts |
|---|---|
| Colorado | 1049 |
| Georgia | 1019 |
| Hawaii | 305 |
| Mid-Atlantic states | 2016 |
| Northern California | 2504 |
| Northwest | 586 |
| Southern California | 4637 |
The analysis standardized rates across census tracts to account for variability in KP member density. The resulting tract-level standardized rates (Z scores) incorporate the number of members in each tract along with the rate to indicate how many standard deviations each tract rate is from the regional rate. This highlights individual tract rates that are statistically significantly different from the overall regional rate.
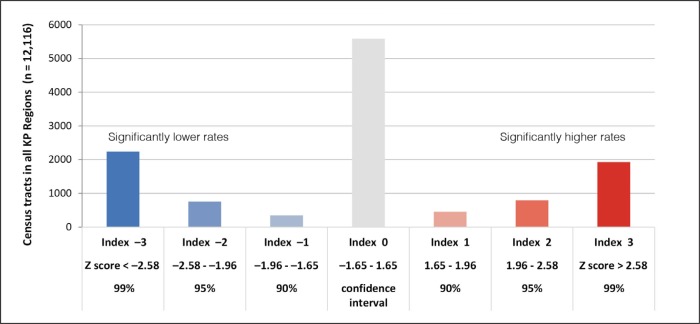
To determine if there were entire neighborhoods, or groups of census tracts, with significantly higher or lower rates, it was important to first define neighborhoods. Neighborhoods were ultimately defined around each census tract as either 1) all additional census tracts within two miles, for densely populated urban areas, or 2) the two additional closest census tracts, measured from the centroid, for sparsely populated rural areas. On the basis of these neighborhood definitions, we created models in ArcGIS for Desktop (Esri, Redlands, CA) to run the Hot Spot Analysis (Getis-Ord Gi* statistic) on the standardized tract rates for each chronic condition for each Region. The Getis-Ord Gi* statistic is a Z score identifying statistically significant spatial clustering of higher and lower values. When applied to the standardized chronic condition prevalence rates, the results identify multitract hot spots where neighborhood rates significantly differ from the overall regional rate. To further protect member confidentiality, we then recategorized the hot spot Z scores into a hot spot index value for each census tract, as specified in Figure 2. Each hot spot index value corresponds to a standard deviation and confidence interval. These classifications allowed us to share actionable relative prevalence data and maps, while completely masking the actual rates.
Figure 2.
Hot spot index categories for prevalence of adult obesity.
KP = Kaiser Permanente.
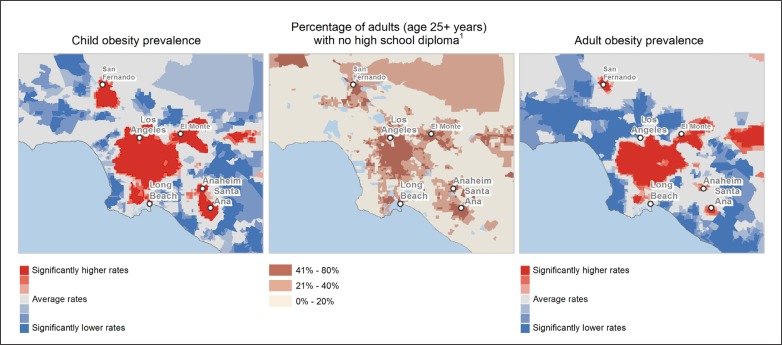
This method revealed neighborhoods with significant spatial clustering of similar tract rates, which were either significantly higher or lower than the regional average. These results indicated that the variation in some chronic conditions across KP member communities mirrored key drivers (eg, obesity and low educational attainment; Figure 3, enlarged version is available online at: www.thepermanente-journal.org/images/Spring2014/GIS3.jpg). Although some of these associations have been previously described in published studies,15–17 this approach systematically identified and quantified the geographic variation and generated compelling visualizations that both protected individual member data and were easily understood by nontechnical audiences.
Figure 3.
Comparison of education level for the overall population and health outcomes for Kaiser Permanente (KP) members across Los Angeles, CA. Enlarged version is available at: www.thepermanentejournal.org/images/Spring2014/GIS3jpg.
Additional Cases Using Geographic Information Systems
The hot spot modeling method and maps described earlier were initially developed to complement a robust ACA-mandated community health needs assessment process, but KP clinicians are finding new uses for them. We have recently used this approach to 1) inform planning efforts for prediabetes interventions in Georgia and the Northwest, 2) support the case for investment in an at-home healthy meals delivery program for patients with heart failure after discharge in the San Francisco Bay Area, and 3) identify KP communities where fewer people get a flu vaccine to target efforts to increase vaccination rates in Southern California.
In the future, GIS could play a vital role in improving clinical operations. In the spirit of the work done at the University of Florida Family Data Center, we are mapping heart attack risk in KP member communities across San Diego to help target deployment of a mobile health van.7 In addition, an early prototype has indicated some value for using GIS-based route planning tools to help optimize the work of home health care providers. Although this application is nascent at KP, related work has documented benefits such as reduced cost via reduced travel time for providers as well as improved patient satisfaction.18
Evolving Opportunities
Care transformation is likely to happen on multiple scales, from the clinical care team to the community. Insight and information based on GIS could help by supplementing decision support for care teams, informing partnerships with planning and public health agencies, and empowering communities to improve their health collectively.
GIS can supplement decision support for clinical care teams. Care teams are increasingly prescribing walking as a therapy for chronic conditions. After-visit summaries or patient-facing tools could include suggestions for walking routes or other healthy lifestyle resources near the patient’s home or work. GIS also have been used to investigate patterns of community-acquired methicillin-resistant Staphylococcus aureus, for which geographic area proved to be a significant risk factor for children presenting with this infection.19 The authors suggested that this information could guide antibiotic selection before culture results are available.19
GIS maps and analyses support a common language that can inform partnerships with local planning and public health agencies and affect policy change. Health in All Policies: A Guide for State and Local Governments outlines ways in which decisions made in sectors such as transportation, education, and economic development affect health. The policy suggests that “better health can support the goals of these multiple sectors.”20 Regional Equity Atlases, such as those available for Portland, OR; Denver, CO; and Atlanta, GA, provide another example of the use of GIS to communicate interrelationships between planning sectors, social determinants, and health outcomes that can help galvanize policy change.
Finally, and perhaps most important, GIS can help empower community members to improve their health collectively. Learning what is already working in some neighborhoods can inform strategies in neighborhoods that face similar social determinants. Increasingly, crowdsourcing is used to allow people to vote online, in a geographically specific way, on investments that are important to them. Portland Bike Share is one example.21 The same could be done for understanding which neighborhood-level investments would help people become or stay healthy, be it a grocery store, improved park, or better access to transportation.
Conclusion
Use of GIS at KP has evolved over the years and has recently become important for regulatory aspects of health care reform related to network adequacy and community health needs assessment. As part of these efforts, we identified systemic variation in the prevalence of chronic conditions across KP member communities at the census tract and neighborhood levels. This geographic variation is not random, suggesting that geographically informed interventions may be part of a multifaceted solution. Furthermore, these results are generating interest in other parts of KP to understand the effects of place and to respond accordingly. These findings reinforce Ethan Berke, MD’s call for “place as a vital sign.”22 GIS make it possible to give geographic context to data from an EHR, understand individual health in the context of community health, and begin to assess the importance of place as a vital sign. Within KP, the use of GIS is growing, results are compelling, and engagement is high.
Acknowledgments
The authors would like to thank Pamela Schwartz, MPH, and Jean Nudelman, MPH, for leadership in developing the Community Health Needs Assessment platform and for providing constructive feedback during refinement of the hot spot methodology.
Kathleen Louden, ELS, of Louden Health Communications provided editorial assistance.
Footnotes
Disclosure Statement
The author(s) have no conflicts of interest to disclose.
American community survey [Internet] Washington, DC: US Department of Commerce, US Census Bureau; 2013. Dec 31, [cited 2014 Jan 6]. Available from: http://factfinder2.census.gov/faces/nav/jsf/pages/searchresults.xhtml?refresh=t.
Limitations
Anywhere you have extreme poverty and no national health insurance, no promise of health care regardless of social standing, that’s where you see the sharp limitations of market-based health care.
— Paul Farmer, b 1959, American medical anthropologist
References
- 1. The Patient Protection and Affordable Care Act of 2010. Public Law 111-148, 111th Congress, 124 Stat 119, HR 3590, enacted 2010 Mar 23.
- 2.Kehoe B. Mapping out care delivery with an assist from GIS. Hosp Health Netw. 2011 Jan;85(1):16–7. [PubMed] [Google Scholar]
- 3.California health benefit exchange [Internet] Sacramento, CA: National Business Coalition on Health; 2012November16[amended 2012 Dec 28; cited 2013 Aug 27; ]. Available from: www.healthexchange.ca.gov/Solicitations/Documents/FINAL%20SOLICITATION%2011-16-12%20updated%2012-28-12.pdf25 [Google Scholar]
- 4.Supplementary response: inclusion of essential community providers [Internet] Baltimore, MD: Centers for Medicare & Medicaid Services; 2013. Mar 8, p. 3. [cited 2013 Aug 27; ]. Available from: www.cms.gov/CCIIO/Programs-and-Initiatives/Files/Downloads/ecp_supplemental_response_Form_03_08_13.pdf. [Google Scholar]
- 5.New requirements for 501(c)(3) hospitals under the Affordable Care Act [Internet] Washington, DC: Internal Revenue Service; updated 2013 Nov 7. [cited 2013 Aug 27; ]. Available from: www.irs.gov/Charities-&-Non-Profits/Charitable-Organizations/New-Requirements-for-501%28c%29%283%29-Hospitals-Under-the-Affordable-Care-Act. [Google Scholar]
- 6.Dulin MF, Ludden TM, Tapp H, et al. Using Geographic Information Systems (GIS) to understand a community’s primary care needs. J Am Board Fam Med. 2010 Jan-Feb;23(1):13–21. doi: 10.3122/jabfm.2010.01.090135. DOI: http://dx.doi/org/10.3122/jabfm.2010.01.090135. [DOI] [PubMed] [Google Scholar]
- 7.Hardt NS, Muhamed S, Das R, Estrella R, Roth J. Neighborhood-level hot spot maps to inform delivery of primary care and allocation of social resources. Perm J. 2013 Winter;17(1):4–9. doi: 10.7812/TPP/12-090. DOI: http://dx.doi.org/10.7812/TPP/12-090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Essential community providers [Internet] Rockville, MD: Health Resources and Services Administration, HIV/AIDS Programs; 2013. [cited 2013 Dec 5; ]. Available from: http://hab.hrsa.gov/affordablecareact/ecp.html. [Google Scholar]
- 9. Not-for-profit hospital community benefit legislation. SB 697, CA Stat of 1994 ch 812, §127340–127365.
- 10.CHNA data platform: background [Internet] Oakland, CA: Kaiser Permanente; 2013. [cited 2013 Aug 27; ]. Available from: http://assessment.communitycommons.org/KP/Background.aspx. [Google Scholar]
- 11.Resources for implementing the community health needs assessment process [Internet] Atlanta, GA: Centers for Disease Control and Prevention, Office of the Associate Director for Policy; 2013. Sep 11, [cited 2013 Aug 27; ]. Available from: www.cdc.gov/policy/chna/ [Google Scholar]
- 12.Krieger N, Chen JT, Waterman PD, Soobader MJ, Subramanian SV, Carson R. Geocoding and monitoring of US socioeconomic inequalities in mortality and cancer incidence: does the choice of area-based measure and geographic level matter?: the Public Health Disparities Geocoding Project. Am J Epidemiol. 2002 Sep 1;156(5):471–82. doi: 10.1093/aje/kwf068. DOI: http://dx.doi.org/10.1093/aje/kwf068. [DOI] [PubMed] [Google Scholar]
- 13.Krieger N. A century of census tracts: health & the body politic (1906–2006) J Urban Health. 2006 May;83(3):355–61. doi: 10.1007/s11524-006-9040-y. DOI: http://dx.doi.org/10.1007/s11524-006-9040-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hoang C, Kolenic G, Kline-Rogers E, Eagle KA, Erickson SR. Mapping geographic areas of high and low drug adherence in patients prescribed continuing treatment for acute coronary syndrome after discharge. Pharmacotherapy. 2011 Oct;31(10):927–33. doi: 10.1592/phco.31.10.927. DOI: http://dx.doi.org/10.1592/phco.31.10.927. [DOI] [PubMed] [Google Scholar]
- 15.Link BG, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav. 1995 Spec No:80–94. [PubMed] [Google Scholar]
- 16.Geraghty EM, Balsbaugh T, Nuovo J, Tandon S. Using Geographic Information Systems (GIS) to assess outcome disparities in patients with type 2 diabetes and hyperlipidemia. J Am Board Fam Med. 2010 Jan-Feb;23(1):88–96. doi: 10.3122/jabfm.2010.01.090149. DOI: http://dx.doi.org/10.3122/jabfm.2010.01.00149. [DOI] [PubMed] [Google Scholar]
- 17.Garg A, Jack B, Zuckerman B. Addressing the social determinants of health within the patient-centered medical home: lessons from pediatrics. JAMA. 2013 May 15;309(19):2001–2. doi: 10.1001/jama.2013.1471. DOI: http://dx.doi.org/10.1001/jama.2013.1471. [DOI] [PubMed] [Google Scholar]
- 18.Nowak M, Hewitt M, Nataraj N. Planning strategies for home health care delivery [Internet] Chicago, IL: Loyola eCommons; 2013. [cited 2013 Dec 30; ]. Available from: http://ecommons.luc.edu/isom_facpubs/4. [Google Scholar]
- 19.Tirabassi MV, Wadie G, Moriarty KP, et al. Geographic information system localization of community-acquired MRSA soft tissue abscesses. J Pediatr Surg. 2005 Jun;40(6):962–6. doi: 10.1016/j.jpedsurg.2005.03.010. DOI: http://dx.doi.org/10.1016/j.jpedsurg.2005.03.010. [DOI] [PubMed] [Google Scholar]
- 20.Rudolph L, Caplan J, Ben-Moshe K, Dillon L. Health in all policies: a guide for state and local governments. Washington, DC and Oakland, CA: American Public Health Association and Public Health Institute; 2013. [cited 2013 Nov 8] Available from: www.apha.org/NR/rdonlyres/882690FE-8ADD-49E0-8270-94C0ACD14F91/0/HealthinAllPoliciesGuide169pages.PDF. [Google Scholar]
- 21.Portland Bike Share [Internet] Portland, OR: Portland Bike Share; 2013. [cited 2013 Nov 8; ]. Available from: http://portlandbikesharestationmap.com. [Google Scholar]
- 22.Berke EM. Geographic Information Systems (GIS): recognizing the importance of place in primary care research and practice. J Am Board Fam Med. 2010 Jan-Feb;23(1):9–12. doi: 10.3122/jabfm.2010.01.090119. DOI: http://dx.doi.org/10.3122/jabfm.2010.01.090119. [DOI] [PMC free article] [PubMed] [Google Scholar]