Abstract
Background
The volar lunate facet fragment of a distal radius fracture may not be stabilized with volar-locked plating alone due to the small size and distal location of the fragment. Identification and stabilization of this small fragment is critical as unstable fixation may result in radiocarpal and radioulnar joint subluxation. The addition of spring wire fixation with volar plating can provide stable internal fixation of this critical fracture fragment.
Methods
A retrospective review (2006–2011) identified nine patients with distal radius fractures with an associated volar lunate facet fragment that were treated with volar-locked plating and spring wire fixation of the volar lunate facet fragment. Radiographic indices, range of motion, grip strength, and postoperative Patient-related wrist evaluation (PRWE) scores were obtained to assess pain and function.
Results
All distal radius fractures healed, and the volar lunate facet fragment reduction was maintained. The mean follow-up was 54 weeks. Mean active range of motion was 46° wrist flexion, 51° wrist extension, 80° pronation, and 68° supination. The mean grip strength was 21 Kg, achieving 66 % of the uninjured limb. The average PRWE score was 17. No patient required removal of hardware or had evidence of tendon irritation.
Conclusions
The addition of spring wire fixation to volar-locked plating provided stable fixation of the volar lunate facet fragment of distal radius fractures without complication. This technique addresses a limitation of volar-locked plating to control the small volar lunate facet fragment in distal radius fractures otherwise amenable to volar plating.
Level of Evidence
A retrospective case series, Level IV.
Keywords: Lunate, Distal radius, Kirschner wire, Locked plating
Introduction
The advent of volar locking plates has revolutionized the treatment of distal radius fractures. They are effective and have been popularized for treating the more commonly seen dorsally displaced fractures [12, 14, 15]. Over the last decade, volar plating has become the technique of choice for many surgeons in the treatment of distal radius fractures. This modality has been associated with reproducibly good results and relatively few complications [13, 14, 16, 21, 22].
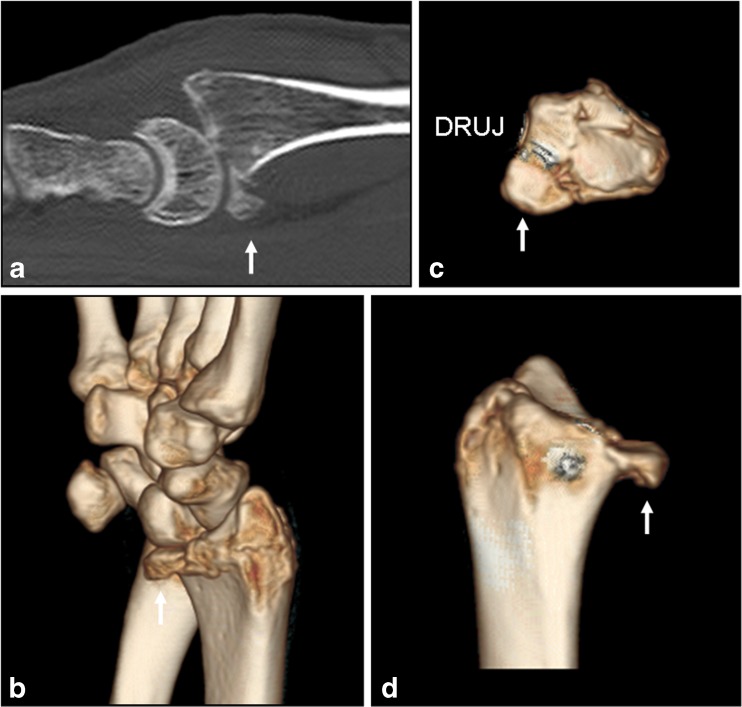
In 2004, Harness and colleagues reported an important limitation of volar plating with the loss of fixation of the volar lunate facet fragment [8]. The volar lunate facet fragment occurs at the distal, volar and ulnar portion of the distal radius. This fragment is critical because the volar radiocarpal and radioulnar ligaments are attached in this location. The fragment also involves the sigmoid notch and can affect the stability of the distal radioulnar joint (DRUJ) [3, 11]. Loss of fixation of this fragment can lead to volar subluxation of the carpus and/or DRUJ instability (Fig. 1) [1, 2].
Fig. 1.
a Sagittal computed tomography and b 3-D reconstruction images of the volar marginal fragment (arrows) with carpal subluxation. c, d 3D reconstructive images demonstrate volar marginal fragment that can involve the distal radial ulnar joint (DRUJ)
Although the volar lunate facet fracture fragment can be an isolated finding, it is often found with comminuted intra-articular fractures of the distal radius. If not identified and recognized preoperatively or intraoperatively, volar locking plates alone may fail to stabilize the fragment as it is too distal and not connected to any larger fragments. Several authors have provided possible solutions for the treatment of distal volar fragments, including the technique of fragment specific fixation [4, 6, 18]. However, this technique has been described as technically demanding and is known to require a significant learning curve for adequate fracture fixation [6, 9, 17]. It may also require multiple incisions or plates to achieve stability for the remaining fracture fragments. Further, these techniques have not been described with the use of a volar plate for fixation of the remaining fracture fragments.
The purpose of our study was to determine if a small bent Kirschner wire (spring wire) could reliably hold the reduction of volar lunate facet fragment if the spring wire is secured under a volar locking plate. This technique allows the familiar volar plating approach to the distal radius fracture and applies spring wire fixation to capture and stabilize the small distal lunate facet fragment. In this study, we describe this technique and report the results of our series of nine patients with distal radius fractures and a volar lunate facet fragment treated with this type of fixation.
Materials and Methods
Between September 2006 and December 2011, nine patients presenting with a distal radius fracture and an associated volar lunate facet fragment were treated with volar-locked plating (DVR plate; Hand Innovations, Miami, FL) and the addition of K-wire fixation of the volar lunate facet fragment by the senior author (DGD). This study was designed as a retrospective chart review. Criteria for entry into this case series included patients with intra-articular distal radius fractures with a volar lunate facet fragment in which volar plating alone could not secure this critical fragment. Approval to conduct this study was obtained from our institutional research and ethics board.
Of these nine patients, four were male and five were female, and their mean age was 42 years (range, 18–72 years). The right wrist was injured in five patients and the left in four; five involved the dominant side. According to the Comprehensive Classification of Fractures of Long Bones (AO classification), all nine were AO type C3 fractures [19]. All fractures contained a volar lunate facet fragment. Surgery was performed on average 5 days from the time of injury. Nine patients with AO type C3 distal radius fractures with a volar lunate facet fragment underwent spring wire fixation and volar plating. Mean follow-up was 51 weeks (range, 13–199 weeks).
Five patients had additional fixation combined with spring wire fixation and volar plating to control other fracture fragments or to neutralize forces across the radiocarpal joint. Four patients had external fixation placed to assist with intraoperative fracture reduction, and the fixator was maintained postoperatively to protect the radiocarpal joint reduction. In addition to external fixation, one patient also received a dorsal K-wire and a radial styloid K-wire and another fracture required a dorsal pin plate and radial styloid K-wire. One patient required a dorsal K- wire alone to capture the dorsal ulnar corner fragment (Table 1). One patient had a segmental radius and ulnar shaft fracture that were treated concomitantly. One patient had bilateral humeral neck fractures that were treated non-operatively.
Table 1.
Patient data
| Case | Age/gender | Hand | Fixation | Length of follow-up (weeks) | Wrist ROM F/E | Wrist ROM P/S | Grip strength* (% of uninjured) | PRWE score |
|---|---|---|---|---|---|---|---|---|
| 1 | 39/M | Right/RHD | Extended volar plate with three spring wire pins | 100 | 50/60 | 80/60 | 37 Kg (69 %) | 20 |
| 2 | 21/M | Left/RHD | External fixation, radial styloid K-wire, dorsal pin plate, volar plate with two spring wire pins | 13 | 45/45 | 70/70 | n/a | 0 |
| 3 | 40/M | Right/RHD | External fixation, dorsal K-wire, radial styloid K-wire, volar plate with two spring wire pins | 199 | 50/50 | 80/80 | 43 Kg (89 %) | 7.5 |
| 4 | 21/F | Right/RHD | External fixation, dorsal K-wire, radial styloid K-wire, one spring wire pins | 44 | 55/60 | 90/80 | 30 Kg (100 %) | 2 |
| 5 | 78/F | Right/RHD | Dorsal K-wire, volar plate with one spring wire pin | 22 | 50/50 | 80/80 | 14 Kg (63 %) | 16 |
| 6 | 18/F | Left/RHD | Volar plate with one spring wire pin | 15 | 45/45 | 80/55 | 5 Kg (41 %) | 30 |
| 7 | 56/F | Left/RHD | External fixation, volar plate with two spring wire pins | 15 | 40/60 | 70/70 | 8 Kg (29 %) | 25 |
| 8 | 72/F | Left/RHD | Volar plate with two spring wire pins | 48 | 40/40 | 85/60 | 9 Kg (81 %) | 41 |
| 9 | 38/M | Left/RHD | External fixation, volar plate with one spring wire pin | 13 | 40/60 | 85/60 | 22 Kg (55 %) | 9 |
M male, F female, RHD right hand dominant, F/E flexion/extension, P/S pronation/supination, PRWE patient-related wrist examination, CTS carpal tunnel syndrome
*Value obtained in eight of nine patients
Operative Technique
All surgical procedures were performed with the use of an upper extremity tourniquet and fluoroscopic assistance. A standard flexor carpi radialis (FCR) approach to the distal radius was used as described by Orbay and Fernandez [14]. The extended FCR approach and brachioradialis tenotomy were also used when needed to assist with reduction of the intra-articular fractures [14]. The exposure of the distal radius was critical to effectively handle the small volar lunate facet fragment. The dissection requires careful elevation of the distal pronator quadratus to the most ulnar aspect of the distal radius, exposing the DRUJ capsule, while also preserving the muscular attachment of the pronator quadratus on the ulnar side of the radial shaft where the bone receives significant blood supply. Once the distal radius was exposed, manual reduction of the fracture, focusing on the volar–ulnar corner, was completed first. Traction was very helpful in obtaining the reduction. In four patients, an external fixator (Synthes Inc, West Chester, PA, USA) was placed to assist with traction and manual reduction of the distal radius fracture, using ligamentotaxis. The fixator also was used to distract the radiocarpal joint to permit articular reduction. The volar lunate facet fracture location, fragment size, and comminution were then evaluated. When the volar–ulnar piece was too distal and/or too small for support from a volar locking plate and its distal locking pegs or screws (DVR plate; Hand Innovations, Miami, FL), the technique of spring wire fixation in addition to volar plating was then utilized.
Prior to the application of the volar locking plate, spring wire fixation of the volar lunate facet fragment was performed. Using one or two small K-wires (0.028″ or 0.035), depending on fragment size, the wires were placed into the distal volar lip angled to the opposite intact, proximal dorsal cortex. In our study, four patients received one wire; four had two wires placed, and one patient had three wires. Fluoroscopy was utilized to check the reduction and alignment of the volar–ulnar fragment and the distal radius. Observation of the volar ‘teardrop’ angle of about 70° is a useful parameter to assess the reduction in more comminuted fractures [3]. An open dorsal arthrotomy was performed in seven cases to be certain of the intra-articular reduction. Once reduction and alignment was confirmed, the K-wires were then advanced into the intact proximal, opposite cortex of the dorsal radius (Fig. 2).
Fig. 2.
Surgical technique of spring wire fixation. (1) Lateral view of distal radius demonstrates adequate reduction of the fracture fragments. (2) Using small 0.035″ Kirschner wire, the volar marginal fragment is captured, and wire is advanced to far cortex. (3) The K-wire is then bent to match the curve of the volar rim and cut long enough to be secured under volar plate. (4) The rest of the distal radius fragments are secured with standard volar plating technique
On a technical aside, smaller diameter wires (0.028 or 0.035″) were chosen as they are more malleable and are bent easily to match the curvature of the volar lip providing sufficient and balanced fixation, even with finger manipulation. Two wires are preferred to control any coronal plane rotation of the fragment, but the size of the fragment determines if more than one K-wire can be used. Bone grafting with cancellous allograft may also be advantageous to help control the reduction of the volar fracture as well. It is imperative to make sure that the wires used to hold the volar–ulnar fragment do not interfere with reduction of the dorsal lunate facet. If the wires cannot be placed through the volar fragment without interfering with the dorsal lunate facet fracture, the K-wires in the volar fragment may be used as joysticks while the entire lunate facet is reduced (volar and dorsal fragments). The distal volar wire may then be advanced into the intact proximal, dorsal radius. K-wires are placed using oscillation mode on the driver to limit soft tissue injury.
Once the volar fragment was reduced, the K-wire was backed out 10 mm and bent carefully around the volar lip of the radius. It was also bent to match the curve of the volar radius along the pronator quadratus fossa, this process created the spring wire. The spring wire was tapped back into place. If more than one spring wire was used, the wire was molded in the same manner. They were then cut long enough so that they would be captured under the volar plate. The volar plate was then positioned onto the radial shaft, making sure that it would not protrude into the flexor tendons. The plate was then screwed down onto the shaft, which captured and provided support to the spring wire (Fig. 3). This step should be done carefully as comminuted fractures may become over-reduced and the volar lip can be forced into an extended position (decreased teardrop angle) during plate compression. The remaining fracture fragments, in particular, the dorsal lunate facet and the radial styloid, may then be reduced and secured with distal locking screws or pegs.
Fig. 3.
a Anteroposterior and b lateral preoperative films of a 38-year-old man with an intra-articular, unstable distal radius fracture with a volar marginal fragment (arrow). Postoperative x-rays, c anteroposterior and d lateral, after spring wire fixation of the volar marginal fragment and volar-locked plating demonstrate stable fixation of this critical fracture fragment
The reduction and stability of the fracture were examined by fluoroscopy and physical examination by directly palpating the stability of the fragment during loading of the fragment in flexion–extension and volar–dorsal translation. The distal radioulnar joint (DRUJ) was examined for stability in supination, pronation, and in neutral rotation. If external fixation was applied, it was maintained for at least 4 weeks postoperatively.
Postoperative Management
A postoperative sugar-tong splint was applied in neutral rotation, and finger motion was begun immediately. The patient was then changed into a short-arm splint between 7 and 10 days or when comfortable. A central arc of pronation, supination, flexion and extension (30–45° in each direction) was maintained for the first few weeks, and then the splint was discontinued. The external fixation was removed between 4 and 6 weeks, and a short-arm splint was applied for comfort. Range of motion (ROM) of the wrist and forearm were continued upon removal of the external fixator.
Evaluation
Standard posteroanterior, lateral, and radial tilt lateral radiographs were obtained at each postoperative visit. Articular alignment and specifically a change in the reduction after surgery, if observed, were recorded at the final postoperative examination. The presence of fracture union was evaluated at each visit by the senior author and ‘union’ was defined as osseous bridging across the fracture site on at least two radiographs.
The treating physician, resident or physician assistant evaluated wrist motion and grip strength at serial postoperative visits, and these were recorded at the final visit. The ROM of the injured and the uninjured extremity was measured with a standard goniometer. Measurements were obtained for wrist flexion, wrist extension, forearm pronation, and supination. Grip strength was measured with a Jamar dynamometer. These values are reported as the mean and the standard deviation (Table 1).
Any complications were documented and categorized as minor (those managed non-surgically) or major (those requiring surgical intervention).
Questionnaire
Wrist pain and disability in activities of daily living were assessed postoperatively using the patient-related wrist evaluation tool as described by MacDermid et al. On a scale of 0–100, a lower score is more ideal representing less wrist pain and increased function [10].
Source of Funding
There was no external funding source for this investigation.
Results
All distal radius fractures healed, and the volar lunate facet fragment reduction was maintained with the spring wire fixation and volar-locked plating. No change of articular alignment or malposition of hardware was noted at final follow-up.
The range of wrist motion, grip strength, and PRWE scores are shown in Table 1. Mean active ROM was 46° (SD 5) wrist flexion, 51° (SD 8) wrist extension, 80° (SD 6) forearm pronation, and 68° (SD10) forearm supination. Of those recorded (n = 8), mean grip strength was 21 kg (SD 14), achieving 66 % of the uninjured side. DRUJ instability was not found in any of the patients.
The PRWE was performed in nine patients, and the average score was 17 (range, 0–41). One patient with bilateral humeral fractures at the time of composition of this paper was still non-weight bearing through her upper extremities. When her score was eliminated, the average score of the remaining six patients was 14.
There were no major or minor complications with regard to the fixation and repair of the distal radius fractures. One patient required a carpal tunnel release 8 months after distal radius repair. No patient required removal of hardware or had evidence of flexor or extensor tendon irritation. There were no complications related to the external fixators.
Discussion
The addition of fixation with a spring wire to volar-locked plating provides stable fixation of the volar lunate facet fragment of distal radius fractures. In our series, there were no cases of postoperative volar carpal subluxation or DRUJ instability. The final radiographs confirmed congruent reduction and healing of the volar lunate facet fragment in all cases. There were no complications, and the patients achieved functional ROM and grip strength. Furthermore, subjective data from the PRWE scores indicate minimal functional disability and pain.
Numerous techniques for reducing and fixating distal radius fractures exist [5]. No single technique or system is appropriate for all fracture configurations. The anatomy of the fracture, the experience of the surgeon, and patient variables, such as bone quality or concomitant injuries, play a role in the decision for fixation of distal radius fractures. This is further illustrated in the present study with five patients in our series requiring additional fixation for adequate control of all fracture fragments.
The volar lunate facet fracture fragment of the distal radius has been difficult to treat [1, 8, 16]. Describing a series of seven patients who lost fixation of the volar lunate facet fragment with volar plating alone, Harness et al. highlighted the importance of the reduction and fixation of this fragment. They reported that standard volar plates may not effectively be able to do this given the distal nature and anatomic constraints of the fragment [8]. They suggest that addition of other fixation may be necessary [8].
Several authors have provided possible solutions for fixation of the volar lunate facet fragment. Early reports of K-wire fixation have been described to control the volar lunate facet fragment, but these were not done in conjunction with volar-locked plating [7, 20].
In 1999, Chin and Jupiter described a technique of tension-wire fixation of the volar lunate facet fragment that was performed on four patients. In their technique, after K-wire fixation of the larger distal radius fragments, they secured the volar lunate facet fragment to the proximal radial metaphysis using a 26-gage stainless steel wire. They passed the wire through the metaphysis and then through the volar capsule adjacent to the fracture fragment. They achieved adequate fixation and bony healing in all four patients [4]. While this is a valuable technique, it may be difficult to use this technique when applying a volar plate for fixation of the other fracture fragments, or if there is significant metaphyseal fragmentation.
Another approach to the distal radius that addresses the volar ulnar corner, including a volar lunate facet fragment, is the use of fragment specific fixation. This fixation technique contains pin plates and wire forms to address fracture fragments in each column [6, 9]. The use of this system allows for fixation of the volar lunate facet fragment. However, this technique of distal radius fixation has been described as technically demanding and is known to require a significant learning curve for adequate fracture fixation [6, 17].
The technique of spring wire fixation offers several advantages. First, the technique captures and stabilizes the critical volar lunate facet fragment using inexpensive standard K-wires. Initially pinning the distal fragment to the intact radius allows one to reduce and stabilize the remaining distal radius fracture fragments using standard volar-locked plating techniques with any volar plating system. Second, the small wires allow distal access to the fragment without disruption of the critical volar carpal ligaments. Third, and potentially most importantly, as the volar plate is secured to the distal radius over the molded wire, it provides stability to the volar lunate facet fragment to resist volar displacement.
There are several limitations to our study. One is that it is a small case series due to the limited inclusion criteria. Given the small sample size, we made no attempt to compare the results of this technique to others. Also given, the significant injuries of the patients (AO C3) and multiple modalities for fracture fixation were also implemented such as external fixation and dorsal ulnar corner pinning. These additional methods of fixation may also have contributed to the successful results. While the radiographic results were good, the slightly elevated PRWE scores may be due to the more severe injuries, variability in the age of the patients, their baseline activity level, and in the severity of associated trauma (bilateral upper extremity injuries). While we did not find any complications related to the internal fixation, we also realize that attritional tendon injuries often occur years after the fracture and our mean follow-up is just under 1 year. A prospective, randomized trial comparing various techniques to capture the volar lunate facet fragment would be useful. However, the incidence of this specific fracture fragment occurring alone is unknown and would likely be difficult to acquire enough patients to do so.
In conclusion, spring wire fixation in addition to volar-locked plating allows adequate reduction and stabilization of the critical volar lunate facet fragment. This technique is fast, inexpensive, and can be used with any volar plating system. It addresses a limitation of volar-locked plating and potentially extends the indications to control the small volar lunate facet fragment in distal radius fractures otherwise amenable to volar plating.
Acknowledgments
Conflict of Interest Statements
Amy M. Moore and David G. Dennison have no conflicts to disclose.
Statement of Human and Animal Rights and Use of Informed Consent
This human study was conducted with institutional approval regarding animal and human rights and the use of informed consent or the waiving of informed consent as deemed appropriate by our institutional review board.
References
- 1.Apergis E, Darmanis S, Theodoratos G, et al. Beware of the ulno-palmar distal radial fragment. J Hand Surg. 2002;27:139–145. doi: 10.1054/jhsb.2001.0712. [DOI] [PubMed] [Google Scholar]
- 2.Bellinghausen HW, Gilula LA, Young LV, et al. Post-traumatic palmar carpal subluxation. Report of two cases. J Bone Joint Surg. 1983;65A:998–1006. [PubMed] [Google Scholar]
- 3.Berger RA, Landsmeer JM. The palmar radiocarpal ligaments: a study of adult and fetal human wrist joints. J Hand Surg [Am] 1990;15:847–854. doi: 10.1016/0363-5023(90)90002-9. [DOI] [PubMed] [Google Scholar]
- 4.Chin KR, Jupiter JB. Wire-loop fixation of volar displaced osteochondral fractures of the distal radius. J Hand Surg [Am] 1999;24:525–533. doi: 10.1053/jhsu.1999.0525. [DOI] [PubMed] [Google Scholar]
- 5.Freeland AE, Luber KT. Biomechanics and biology of plate fixation of distal radius fractures. Hand Clin. 2005;21:329–339. doi: 10.1016/j.hcl.2005.03.002. [DOI] [PubMed] [Google Scholar]
- 6.Gerostathopoulos N, Kalliakmanis A, Fandridis E, et al. Trimed fixation system for displaced fractures of the distal radius. J Trauma. 2007;62:913–918. doi: 10.1097/01.ta.0000219948.92935.cd. [DOI] [PubMed] [Google Scholar]
- 7.Halbrecht JL, Stuchin SA. Unusual fragment displacement in a distal radius fracture. J Hand Surg. 1988;13:746–749. doi: 10.1016/S0363-5023(88)80140-0. [DOI] [PubMed] [Google Scholar]
- 8.Harness NG, Jupiter JB, Orbay JL, et al. Loss of fixation of the volar lunate facet fragment in fractures of the distal part of the radius. J Bone Joint Surg Am. 2004;86-A:1900–1908. doi: 10.2106/00004623-200409000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Konrath GA, Bahler S. Open reduction and internal fixation of unstable distal radius fractures: results using the trimed fixation system. J Orthop Trauma. 2002;16:578–585. doi: 10.1097/00005131-200209000-00007. [DOI] [PubMed] [Google Scholar]
- 10.MacDermid JC, Turgeon T, Richards RS, et al. Patient rating of wrist pain and disability: a reliable and valid measurement tool. J Orthop Trauma. 1998;12:577–586. doi: 10.1097/00005131-199811000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Melone CP., Jr Articular fractures of the distal radius. Orthop Clin N Am. 1984;15:217–236. [PubMed] [Google Scholar]
- 12.Orbay JL. The treatment of unstable distal radius fractures with volar fixation. Hand Surg. 2000;5:103–112. doi: 10.1142/S0218810400000223. [DOI] [PubMed] [Google Scholar]
- 13.Orbay J. Volar plate fixation of distal radius fractures. Hand Clin. 2005;21:347–354. doi: 10.1016/j.hcl.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 14.Orbay JL, Fernandez DL. Volar fixation for dorsally displaced fractures of the distal radius: a preliminary report. J Hand Surg [Am] 2002;27:205–215. doi: 10.1053/jhsu.2002.32081. [DOI] [PubMed] [Google Scholar]
- 15.Orbay JL, Fernandez DL. Volar fixed-angle plate fixation for unstable distal radius fractures in the elderly patient. J Hand Surg [Am] 2004;29:96–102. doi: 10.1016/j.jhsa.2003.09.015. [DOI] [PubMed] [Google Scholar]
- 16.Rozental TD, Blazar PE. Functional outcome and complications after volar plating for dorsally displaced, unstable fractures of the distal radius. J Hand Surg [Am] 2006;31:359–365. doi: 10.1016/j.jhsa.2005.10.010. [DOI] [PubMed] [Google Scholar]
- 17.Saw N, Roberts C, Cutbush K, et al. Early experience with the TriMed fragment-specific fracture fixation system in intraarticular distal radius fractures. J Hand Surg [Am] 2008;33B:53–58. doi: 10.1177/1753193407087887. [DOI] [PubMed] [Google Scholar]
- 18.Smith RS, Crick JC, Alonso J, et al. Open reduction and internal fixation of volar lip fractures of the distal radius. J Orthop Trauma. 1988;2:181–187. doi: 10.1097/00005131-198802030-00002. [DOI] [PubMed] [Google Scholar]
- 19.Stabler A, Baumeister RG. Berger H [Carpal instability and secondary degenerative changes in lesions of the radio-carpal ligaments with various etiology] Handchir Mikrochir Plast Chir. 1990;22:289–295. [PubMed] [Google Scholar]
- 20.Takami H, Takahashi S, Ando M. Comminuted intra-articular fracture of the distal radius with rotation of the palmar medial articular fragment: case reports. J Trauma. 1992;32:404–407. doi: 10.1097/00005373-199203000-00021. [DOI] [PubMed] [Google Scholar]
- 21.Wright TW, Horodyski M, Smith DW. Functional outcome of unstable distal radius fractures: ORIF with a volar fixed-angle tine plate versus external fixation. J Hand Surg [Am] 2005;30:289–299. doi: 10.1016/j.jhsa.2004.11.014. [DOI] [PubMed] [Google Scholar]
- 22.Yu YR, Makhni MC, Tabrizi S, et al. Complications of low-profile dorsal versus volar locking plates in the distal radius: a comparative study. J Hand Surg [Am] 2011;36:1135–1141. doi: 10.1016/j.jhsa.2011.04.004. [DOI] [PubMed] [Google Scholar]