Abstract
Background
We describe a patient with tardy ulnar neuropathy and cubitus valgus deformity found to have an intracapsular ulnar nerve.
Methods
An 89-year-old woman presented with severe neuropathic pain in the ulnar digits of the hand, advanced degenerative arthritis of the elbow, and tardy ulnar nerve palsy. Her pain was exacerbated with elbow movement, particularly flexion. She had paralysis of ulnar nerve innervated muscles, hypersensitivity with absence of two-point discrimination in her ulnar 1–1/2 digits, and a fixed ulnar claw deformity. She also had a grossly unstable elbow.
Results
Plain films revealed a cubitus valgus deformity (38°), an absent radial head, a dislocated proximal radioulnar joint and advanced arthritic changes. Ultrasonography revealed an indistinct ulnar nerve within the cubital tunnel which penetrated the joint. Electrophysiological studies revealed evidence of a severe ulnar neuropathy at the level of the elbow. Intraoperatively, an attenuated 2 cm length of the retrocondylar ulnar nerve was observed to be incorporated into the joint capsule tethered by a fibrous/synovial band which was released. A large effusion was drained. The ulnar nerve was transposed subcutaneously. The capsular rent was repaired in layers. She noted immediate and sustained (2 year follow-up) pain relief and regained moderate function in her interossei.
Conclusions
We believe that the chronic cubitus valgus deformity and secondary degenerative elbow joint changes led to an altered course of the nerve and attenuation of the medial joint capsule such that the ulnar nerve spontaneously buttonholed itself intra-articularly.
Keywords: Ulnar nerve, Entrapment, Cubital tunnel, Intracapsular
Introduction
Cubitus valgus is a rare but well-known cause of ulnar neuropathy. In 1878, Panas first described tardy ulnar nerve palsy in patients with cubitus valgus deformity following elbow trauma [19]. Classic descriptions have reinforced the association [1, 3, 4, 7, 10, 13, 15, 20, 22]. The term tardy or delayed ulnar nerve palsy still remains in use though it has broadened over the years to include other causes, including osteoarthritis [18]. It classically occurs years or even decades following trauma and is thought to be due to compression/ stretching of the nerve or friction (particularly with dislocation of the nerve and a shallow sulcus), especially in elbow flexion [9, 26]. We describe a patient with a degenerative cubitus valgus deformity in whom the ulnar nerve was found to be buttonholed into the humero-ulnar joint. This case illustrates the important, interrelated biomechanical effects of the altered carrying angle from a chronic cubitus valgus deformity on the ulnar nerve as well as the medial elbow joint structures.
Case Report
An 89-year-old woman with advanced degenerative osteoarthritis of the dominant left elbow presented with severe pain, atrophy, lack of function, and sensation in her left hand for at least 13 years. She had previously (1998) undergone resection of a ganglion cyst originating from the elbow joint through an anterior approach. The surgeon had considered releasing the ulnar nerve in the cubital tunnel at that time but chose not to. The patient was primarily affected by severe neuropathic pain unresponsive to Pregabalin 50 mg po Q8H. Straightening her left elbow precipitated excruciating, electric shock like pain that radiated down her forearm into the medial two digits. Her past history was significant for right sided surgeries, including shoulder (2009) and elbow (2004) arthroplasties as well as ulnar nerve subcutaneous transposition (1994).
On examination, she was irritable and in great discomfort. She preferred to brace her elbow in a band to prevent movement. Her carrying angle was 38° (Fig. 1). She had an ulnar claw deformity secondary to severe weakness and atrophy affecting the ulnar innervated extrinsic and intrinsic hand muscles. She had a positive Froment’s sign and no two-point discrimination in her ulnar 1–1/2 digits. The dorso-ulnar aspect of the hand was also insensate. A Tinel’s sign could be elicited at the elbow but not at the wrist.
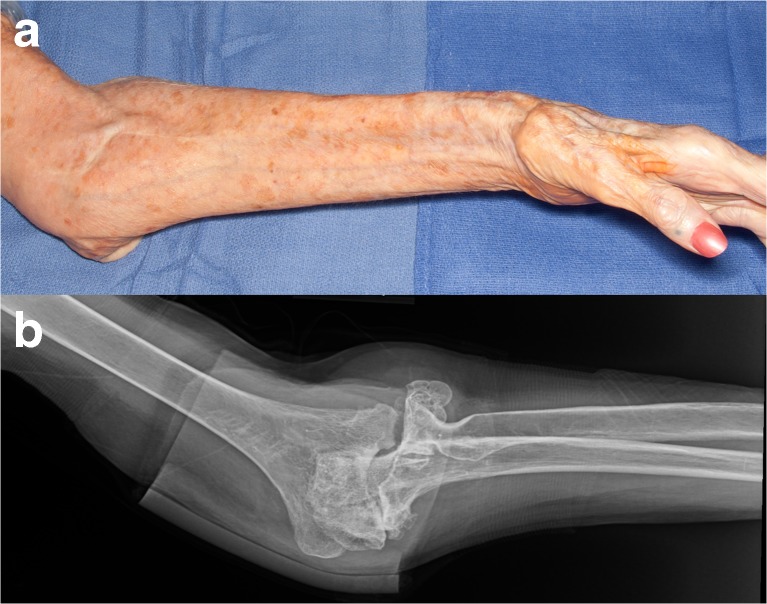
Fig. 1.
Preoperative appearance. a Clinical photograph of the left arm and forearm. The carrying angle was measured at 38°. The left hand shows extensive first dorsal interosseous muscle atrophy. A well-healed scar anterior to the elbow can also be appreciated. b The anteroposterior plain radiograph of the left elbow confirms the extreme cubitus valgus deformity. The head of the left radius cannot be seen. The radial shaft has been displaced medially
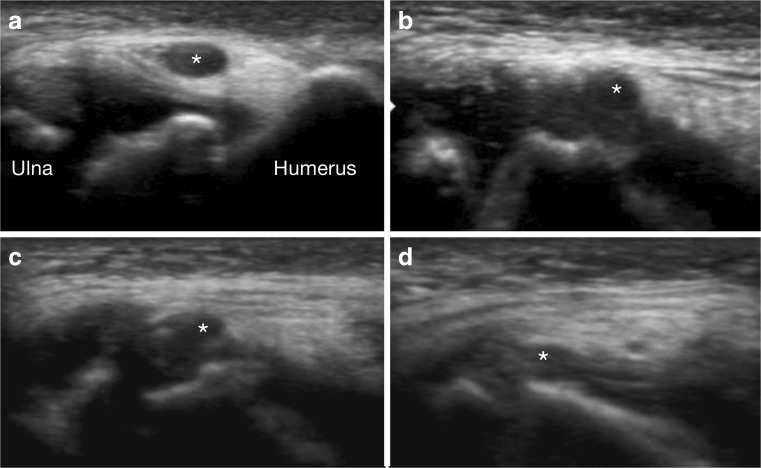
Plain films of the left elbow (Fig. 1) revealed a marked cubitus valgus deformity, an absent radial head, and a dislocated proximal radio-ulnar joint which caused the radius to lie anterior and medial to its normal position. An ultrasound (USG) examination revealed that the left ulnar nerve was enlarged proximal to the cubital tunnel but indistinct behind the osteophytes along the medial aspect of the humero-ulnar joint (Fig. 2) giving the impression that the nerve entered the joint but disappeared within it. There was a large elbow joint effusion.
Fig. 2.
Ultrasound. Transverse images of the ulnar nerve (asterisk) moving proximal to distal (a–d). Proximally, the ulnar nerve is enlarged and hypoechoic (a). More distal, the nerve becomes attenuated and disappears into the humero-ulnar joint (d)
Electrodiagnostic studies documented severe ulnar neuropathy at the level of the left elbow. The ulnar motor nerve conduction velocity was 24 m/s and the amplitude of the compound motor action potential at the abductor digiti minimi on the left side was 2.5 mV. Inching studies showed localized conduction slowing at the level of the left elbow. Needle EMG revealed fibrillations, reduced recruitment, and complex motor units in the first dorsal interosseous and flexor carpi ulnaris. The ulnar sensory nerve action potentials were absent.
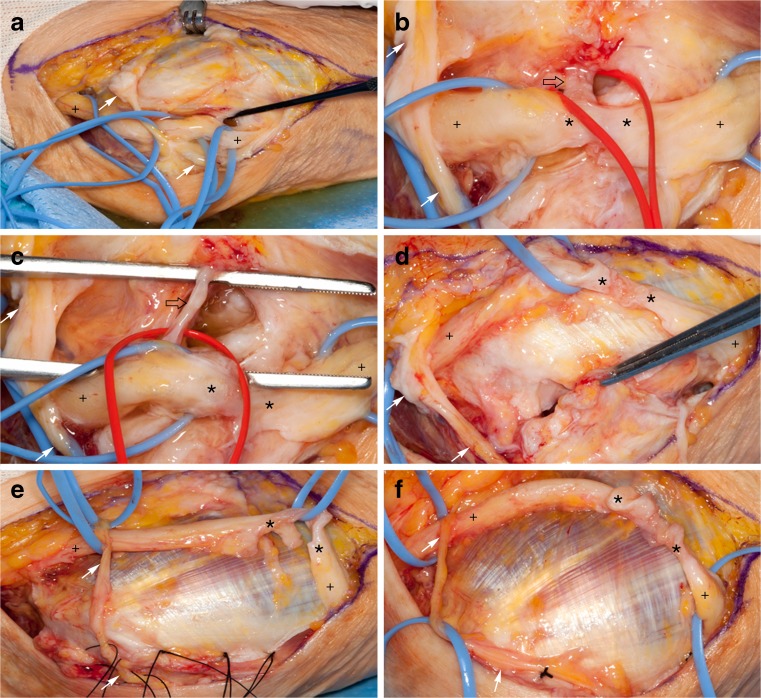
Surgery was performed to help with the refractory neuropathic pain. Intraoperatively, the nerve was severely scarred in the retrocondylar portion. Here, the nerve was attenuated to 40 % of its diameter over a segment 2 cm long (Fig. 3) and was incorporated into the joint capsule. A rent was produced in the capsule while attempting to mobilize the ulnar nerve. A copious amount of viscous green synovial fluid was evacuated. Microbiological, cytological, and biochemical analyses were noncontributory. The nerve was tethered into the joint by a fibrous band (Fig. 3b, c) which on biopsy revealed fibrosis and synovial tissue. The ulnar nerve was transposed subcutaneously after freeing it over a length of 15 cm around the elbow joint and excising the medial intermuscular septum. The rent was repaired in layers using a double-breasted suturing technique to bury the deeper stitch line. The superficial stitch line was similarly reinforced by mobilizing and then suturing the fascia over the common flexor–pronator origin and behind the medial epicondyle to achieve a multilayered closure. Finally, an additional flap was placed to conceal this stitch line by mobilizing the skin flap posterior to the skin incision. The elbow was immobilized in a plaster slab for 3 weeks.
Fig. 3.
a–f. Intraoperative photographs (proximal to left; distal to right). a The ulnar nerve (plus signs) in the cubital tunnel has been dissected circumferentially in preparation for subcutaneous transposition. During the neurolysis, a hole (black probe) within the capsule of the elbow joint was encountered which yielded thick greenish “machine oil” fluid. The medial antebrachial cutaneous nerve (white arrows) has been identified and preserved. b The ulnar nerve was densely attached to the capsule of the elbow joint and a fibrotic part of it (black open arrow) was entering the joint. This communication was seen at the level of the greatest attenuation (asterisks) within the ulnar nerve. c Further circumferential dissection of the nerve increased the diameter of the rent in the elbow joint capsule. Biopsy of the scarred capsular communication (black open arrow) showed fibrosis along with synovial tissue. d, e The ulnar nerve was mobilized anteriorly and the capsular rent repaired in layers with interrupted 3–0 silk sutures after mobilizing the deep fascia over the common flexor–pronator origin. The zone of injury (asterisks) can be clearly seen to be attenuated by greater than 50 % of the native nerve diameter. f The ulnar nerve lies lax in its final transposed position over the flexor–pronator fascia
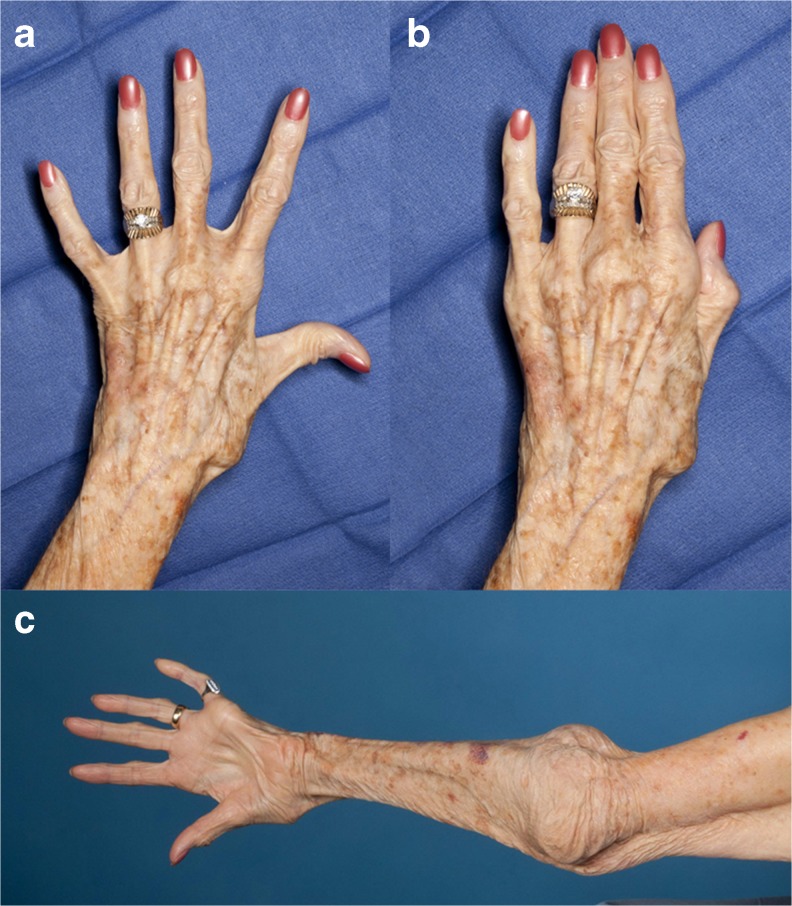
At the first postoperative visit, 3 weeks later, the patient was pain free. She had gained some function of her palmar and dorsal interossei (Fig. 4). At 2 years follow-up, she still had an unstable elbow and a dense residual ulnar neuropathy but was pain free.
Fig. 4.
Postoperative appearance. Clinical photographs of the left hand and forearm taken on postoperative day 20. The patient has gained finger abduction (a) and adduction (b) indicating at least partial recovery of ulnar nerve function. c Clinical photograph taken from a posterior vantage point at 9 months follow-up. The fingers are actively abducted and the radius is dislocated anteriorly in this position. The olecranon can be seen prominently. There is no fluid collection at the incision site which has healed well
Discussion
An intra-articular position is a rare, but known complication occurring after trauma or reduction. Several case reports have described the fractured medial epicondyle, especially in children, dislocating with the ulnar nerve within the elbow joint [5, 21, 27]. We identified only one case of a spontaneously occurring intra-articular ulnar nerve in a patient with severe deforming elbow arthritis related to rheumatoid arthritis (carrying angle unknown) [14].
In our case, we believe that the cubitus valgus deformity which resulted from advanced, chronic changes of degenerative osteoarthritis set into motion a series of biomechanical events. Cubitus valgus results in a lateral displacement of the humero-ulnar axis. This creates a torque (moment) which places extra stress on the medial collateral ligament. Over time, or with chronic overuse/microtrauma, inflammation and synovitis occurs, leading to medial collateral ligament rupture, attenuation of the joint capsule, and elbow instability. The same factors by themselves, or combined with ones previously discussed, can also lead to (tardy) ulnar neuropathy. Increased valgus stress (without bony deformity), such as in overhead athletes, may lead to medial collateral ligament laxity, ulnar nerve symptoms, or both. Ganglion cysts are well described in patients with degenerative joint disease of the elbow [2, 11] and even cubitus valgus [10]. The extraneural ganglion cyst in our patient was both a manifestation of the altered mechanics but could have been a potentiator of the process. We believe that the intracapsular location of the ulnar nerve is an extreme of the same biomechanical principles. In our case, the same capsular defect could have provided the potential opening through which the nerve could have buttonholed itself. Elbow flexion which has detrimental effects on pressures on the ulnar nerve [9, 16] may have increased the laxity or opening in the joint, especially in a setting of a stiff elbow and likely low capsular compliance [8]. Elbow motion seemed to provoke symptoms, potentially from the bony impingement on the nerve. Due to the associated pain, it is probable that the patient began immobilizing her elbow and adhesions developed which made subsequent movement even more painful. Motion may have partially denuded the ulnar nerve between the bony surfaces. From a mechanistic point of view, it would have been interesting to perform dynamic clinical and USG testing of the elbow, but this was not feasible or practical due to her pain. While our patient had partial attritional rupture of the ulnar nerve, the case of Moore and Weiland [14] had a complete rupture. Both of these patients had dramatic improvement in pain following surgery.
The corollary to this explanation relates to a mechanism proposed by our group to show the effects of longstanding cubitus varus deformity resulting in lateral collateral ligament changes and posterolateral rotatory instability. The triceps line of pull is consequently shifted medially, which in turn displaces and/or compresses the ulnar nerve. This can lead to ulnar neuropathy and dislocation of the ulnar nerve and a portion of the medial triceps [17, 23–25].
In our case, the goal of surgery was to improve pain. Given the patient’s age, the longstanding nature of the bony deformity, and neurologic deficit, additional reconstruction was not felt to be indicated. Still, we were quite gratified by the immediate and sustained resolution of the pain and surprised by the minor improvement in neurologic function (Fig. 4). We were also pleased that a synovial fistula did not develop with its attendant risks of septic arthritis and the subsequent need for débridements, antibiotics, and ultimately regional myocutaneous flap coverage [6, 12]. We recognize that in other situations, additional bony and ligamentous reconstruction may have been deemed appropriate to correct the complex deformity as well.
Conclusions
We believe that the combination of findings associated with cubitus valgus deformity in this patient is understandable on a biomechanical basis.
Acknowledgments
Statement of Human and Animal Rights
This case report is not an experiment. It elaborates the observed course of a procedure which is the standard of care. The pathogenesis of the problem requiring surgery is being discussed.
Statement of Informed Consent
This case report does not identify the patient in any manner. All photographs and imaging studies have been suitably de-identified.
Conflict of Interest
Manish S. Sharma declares that he has no conflict of interest. John A. Skinner declares that he has no conflict of interest. Robert J. Spinner declares that he has no conflict of interest.
References
- 1.Adson AW. The surgical treatment of progressive ulnar paralysis. Minn Med. 1918;1:455–60. [Google Scholar]
- 2.Bowen TL, Stone KH. Posterior interosseous nerve paralysis caused by a ganglion at the elbow. J Bone Joint Surg Br. 1966;48:774–6. [PubMed] [Google Scholar]
- 3.Brickner WM. Late ulnar nerve palsy following elbow fracture in the adult. J Bone Joint Surg Am. 1924;6:477–81. [Google Scholar]
- 4.Conway FM. Traumatic ulnar neuritis. With especial reference to the late or tardy ulnar paralysis. Ann Surg. 1933;97:425–33. doi: 10.1097/00000658-193303000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cotton FJ. Elbow dislocation and ulnar nerve injury. J Bone Joint Surg Br. 1929;11:348–52. [Google Scholar]
- 6.Damert HG, Altmann S, Schneider W. Soft-tissue defects following olecranon bursitis. Treatment options for closure. Chirurg. 2009;80(448):450–4. [Article in German] [DOI] [PubMed]
- 7.Davidson AJ, Horwitz MT. Late or tardy ulnar-nerve paralysis. J Bone Joint Surg Am. 1935;17:844–56. [Google Scholar]
- 8.Gallay SH, Richards RR, O’Driscoll SW. Intraarticular capacity and compliance of stiff and normal elbows. Arthroscopy. 1993;9:9–13. doi: 10.1016/S0749-8063(05)80336-6. [DOI] [PubMed] [Google Scholar]
- 9.Gelberman RH, Yamaguchi K, Hollstien SB, et al. Changes in interstitial pressure and cross-sectional area of the cubital tunnel and of the ulnar nerve with flexion of the elbow. An experimental study in human cadavera. J Bone Joint Surg Am. 1998;80:492–501. doi: 10.2106/00004623-199804000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Hunt JR. Tardy or late paralysis of the ulnar nerve. A form of chronic progressive neuritis developing many years after fracture dislocation of the elbow joint. JAMA. 1916;66:11–5. doi: 10.1001/jama.1916.02580270015003. [DOI] [Google Scholar]
- 11.Kato H, Hirayama T, Minami A, et al. Cubital tunnel syndrome associated with medial elbow Ganglia and osteoarthritis of the elbow. J Bone Joint Surg Am. 2002;84-A:1413–9. doi: 10.2106/00004623-200208000-00017. [DOI] [PubMed] [Google Scholar]
- 12.Méndez-Fernández MA. Treatment of chronic recurrent synovial fistulae with myofascial flaps. Br J Plast Surg. 1993;46:303–6. doi: 10.1016/0007-1226(93)90008-Y. [DOI] [PubMed] [Google Scholar]
- 13.Miller EM. Late ulnar nerve palsy. Surg Gynecol Obstet. 1924;38:37–46. [Google Scholar]
- 14.Moore JR, Weiland AJ. Bilateral attritional rupture of the ulnar nerve at the elbow. J Hand Surg [Am] 1980;5:358–60. doi: 10.1016/S0363-5023(80)80175-4. [DOI] [PubMed] [Google Scholar]
- 15.Mouchet A. Paralysies tardives du nerf cubital a la suite des fractures du condyle externe de l’humerus. J Chir. 1914;12:437–56. [Article in French]
- 16.Ochi K, Horiuchi Y, Nakamichi N, et al. Association between the elbow flexion test and extraneural pressure inside the cubital tunnel. J Hand Surg [Am] 2011;36:216–21. doi: 10.1016/j.jhsa.2010.11.013. [DOI] [PubMed] [Google Scholar]
- 17.O’Driscoll SW, Spinner RJ, McKee MD, et al. Tardy posterolateral rotatory instability of the elbow due to cubitus varus. J Bone Joint Surg Am. 2001;83-A(9):1358–69. doi: 10.2106/00004623-200109000-00011. [DOI] [PubMed] [Google Scholar]
- 18.Paine KW. Tardy ulnar palsy. Can J Surg. 1970;13:255–61. [PubMed] [Google Scholar]
- 19.Panas J. Sur une cause peu connue de paralysie du nerf cubital. Archives Generales de Medecine. 1878;2 (VII Serie) [Article in French]
- 20.Platt H. The pathogenesis and treatment of traumatic neuritis of the ulnar nerve in the post-condylar groove. Br J Surg. 1926;13:409–31. doi: 10.1002/bjs.1800135103. [DOI] [Google Scholar]
- 21.Reed MW, Reed DN. Acute ulnar nerve entrapment after closed reduction of a posterior fracture dislocation of the elbow: a case report. Pediatr Emerg Care. 2012;28:570–2. doi: 10.1097/PEC.0b013e318258bfba. [DOI] [PubMed] [Google Scholar]
- 22.Regan JR. The surgical treatment of delayed ulnar neuritis. Am J Surg. 1938;41:501–38. doi: 10.1016/S0002-9610(38)90976-6. [DOI] [Google Scholar]
- 23.Spinner RJ, O’Driscoll SW, Davids JR, et al. Cubitus varus associated with dislocation of both the medial portion of the triceps and the ulnar nerve. J Hand Surg [Am] 1999;24:718–26. doi: 10.1053/jhsu.1999.0718. [DOI] [PubMed] [Google Scholar]
- 24.Spinner RJ, An KN, Kim KJ, et al. Medial or lateral dislocation (snapping) of a portion of the distal triceps: a biomechanical, anatomic explanation. J Shoulder Elbow Surg. 2001;10:561–7. doi: 10.1067/mse.2001.118006. [DOI] [PubMed] [Google Scholar]
- 25.Spinner RJ, O’Driscoll SW, Jupiter JB, et al. Unrecognized dislocation of the medial portion of the triceps: another cause of failed ulnar nerve transposition. J Neurosurg. 2000;92:52–7. doi: 10.3171/jns.2000.92.1.0052. [DOI] [PubMed] [Google Scholar]
- 26.Vanderpool DW, Chalmers J, Lamb DW, et al. Peripheral compression lesions of the ulnar nerve. J Bone Joint Surg Br. 1968;50:792–803. [PubMed] [Google Scholar]
- 27.Watson-Jones R. Primary nerve lesions in injuries of the elbow and wrist. J Bone Joint Surg Am. 1930;12:121–40. [Google Scholar]