Abstract
Background
Dorsal wrist ganglia (DWG) are a common, benign soft-tissue mass of the wrist. Excision of DWG is a common procedure performed by hand surgeons and may be performed using either open or arthroscopic techniques. This study aims to evaluate the frequency of stalk visualization with intralesional injection of inert dye in the course of arthroscopic excision along with incidence of recurrence with a minimum of 1-year follow-up.
Methods
Upon IRB approval, a retrospective chart review was performed identifying 27 patients who had consecutively undergone arthroscopic excision of a DWG with the color-aided technique at our institution with a minimum follow-up duration of 12 months. Intraoperative findings were reviewed. Patients were contacted to investigate for incidence of recurrence.
Results
Of the 27-patient cohort, the ganglion stalk was identified in 100 % of the color-aided arthroscopic DWG excisions. Ganglion recurrence was identified in one patient, an incidence of 3.7 %.
Conclusions
The color-aided technique for arthroscopic DWG visualization was found to be a safe and valuable tool for surgeons performing arthroscopic DWG resection. The intraarticular ganglion stalk was identified in 100 % of cases and patients responded well with a low incidence of recurrence.
Keywords: Dorsal wrist ganglion, Arthroscopy, Ganglionectomy, Dye aided, Outcomes
Introduction
Dorsal wrist ganglia (DWG) are the most common benign soft-tissue tumors of the wrist, representing up to 70 % of wrist masses [2,7,17]. Many DWG are managed with conservative treatment, including observation and aspiration. Due to the high incidence of DWG, excision is among the most common procedures performed by hand surgeons. This procedure may be accomplished via open or arthroscopic techniques. Initially described by Osterman and Rafael [13], arthroscopic excision of DWG is evolving to become a desirable technique for the treatment of these common masses due to the potential for smaller incisions and less capsular disruption [5]. Arthroscopic DWG resection has been shown to provide improved range of motion (ROM), aesthetic appearance, incidence of complications, recovery time, pain relief, and overall patient satisfaction [3,5,6]. Regardless of surgical approach, post-operative recurrence of the ganglion is commonly documented and is likely attributed to inadequate excision of the stalk or the presence of multiple occult cysts that remain unresected [6,8,9,11,17]. Kang et al [9]. have evaluated recurrence rates between open and arthroscopic excision of DWG and found no significant difference with a minimum of 1-year follow-up (8.7 % in the open surgery group vs. 10.7 % in the arthroscopic group). Edwards and Johansen [5] performed 55 arthroscopic dorsal wrist ganglionectomies and found zero recurrences after a 2-year follow-up.
Adequate resection of these DWG arthroscopically is dependent on the surgeon's ability to identify the stalk emanating from the dorsal scapholunate ligament. However, variable rates of stalk visualization have been reported in the literature, ranging from 9 to 100 % [5,9,13,14]. Yao and Trindade [17] presented a technique of injection of Indigo Carmine dye (Akorn, Lake Forest, IL, USA) percutaneously into the DWG to facilitate complete stalk visualization. This improves stalk visualization, which potentially aids in the complete excision of the DWG and stalk, and thereby reduces the incidence of recurrence. It was hypothesized that this technique would additionally reduce extensive capsule debridement due to the improved stalk visualization and would reduce the conversion rate to open excision, eliminating associated complications such as scaphoid subluxation, chronic scapholunate instability, hypertrophic scarring, and painful neuroma [11].
In this study, we retrospectively evaluate the frequency of ganglion stalk identification and incidence of recurrence in patients who underwent DWG excision with this color-aided arthroscopic technique with a minimum of 1-year follow-up.
Materials and Methods
Approval was obtained from our institutional review board (IRB) prior to commencement of this retrospective study. A retrospective chart review was performed identifying a consecutive series of 27 patients who had undergone arthroscopic excision of visibly identifiable DWG with the color-aided technique. This involved identification of current procedural terminology (CPT) codes for wrist arthroscopy and dorsal wrist ganglion excision. These procedures were performed at our institution by one fellowship trained hand surgeon. The operative notes for cases meeting the aforementioned criteria were reviewed to confirm the intraoperative injection of Indigo Carmine dye into the ganglion.
The primary outcome measure was identification of the ganglion stalk. The secondary outcome measure assessed recurrence of the DWG. Patient information regarding recurrence was retrieved from the patient database. Inclusion criteria entailed patients who had undergone dorsal wrist ganglia excision at our institution from June 2009 to the present, corresponding to implementation of the color-aided excision technique. Patients were excluded if occult ganglia were identified preoperatively on MRI. A minimum of 1-year follow-up was used to assess for DWG recurrence. Patients were contacted via telephone and questioned for any evidence of recurrence of the mass.
Operative Technique
Five milliliters (mL) of a 1:500 dilution of Indigo Carmine dye is injected percutaneously into an identifiable DWG, while the arthroscope is in the 6R portal and looking at the dorsal scapholunate ligament (dSLIL) (Fig. 1). The stalk should be stained blue and easily visualized (Fig. 2). Once the stalk is visualized arthroscopically, the 3–4 portal is made and a full-radius arthroscopic shaver is inserted into this portal to perform the resection. The dSLIL is protected by keeping the sheathed portion of the shaver facing the dSLIL (Fig. 3). All material stained blue is resected with the shaver. Occasionally, external digital pressure on the cyst may help decompress it further. It is not essential to completely excise the cyst sac; as long as the stalk is truncated, there should be minimal risk of recurrence. The cysts may often be followed into the midcarpal joint for definitive resection (Fig. 4). Once complete resection of the cyst and accompanying stalk is confirmed, a 1 cm × 1 cm dorsal capsulectomy is performed to help prevent recurrence. The portals are closed and the patient is splinted simply for comfort for 2 weeks after which normal range of motion exercises are encouraged.
Fig. 1.
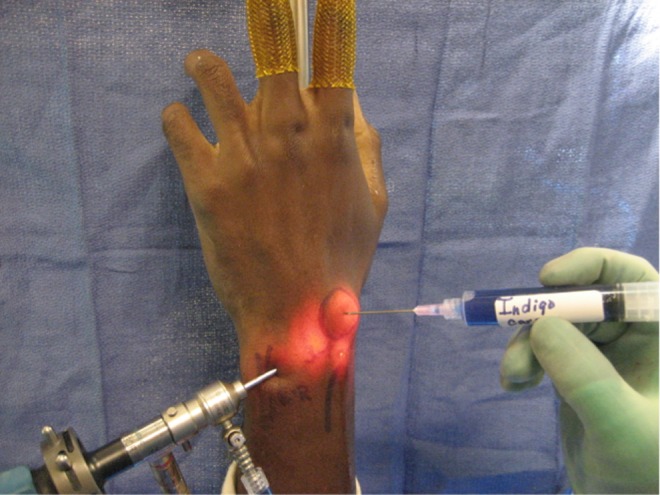
Percutaneous administration of Indigo Carmine into the DWG. The arthroscope is in the 6R portal
Fig. 2.
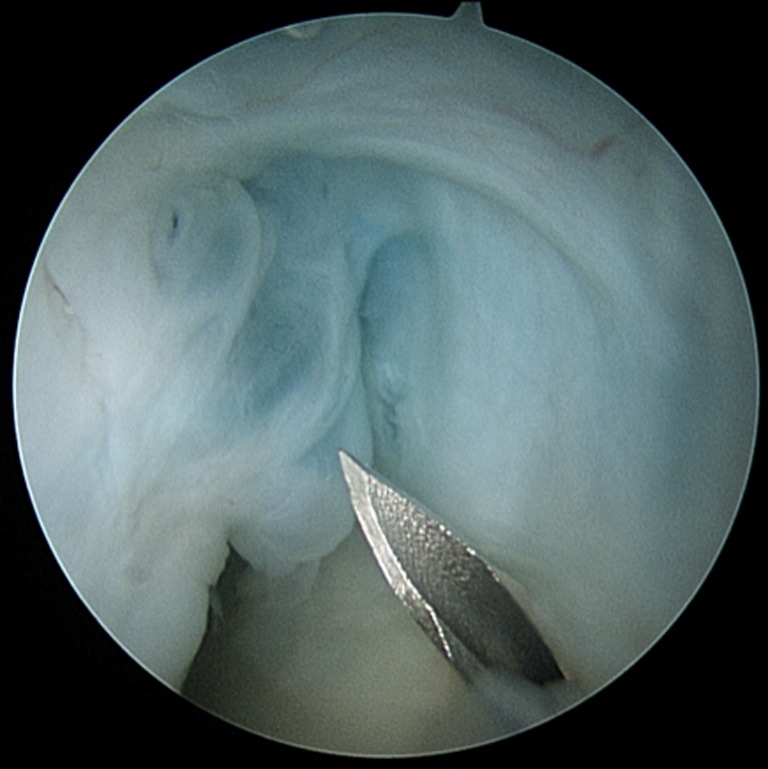
Color-assisted view of the ganglion stalk with Indigo Carmine (base of the stalk identified by the needle)
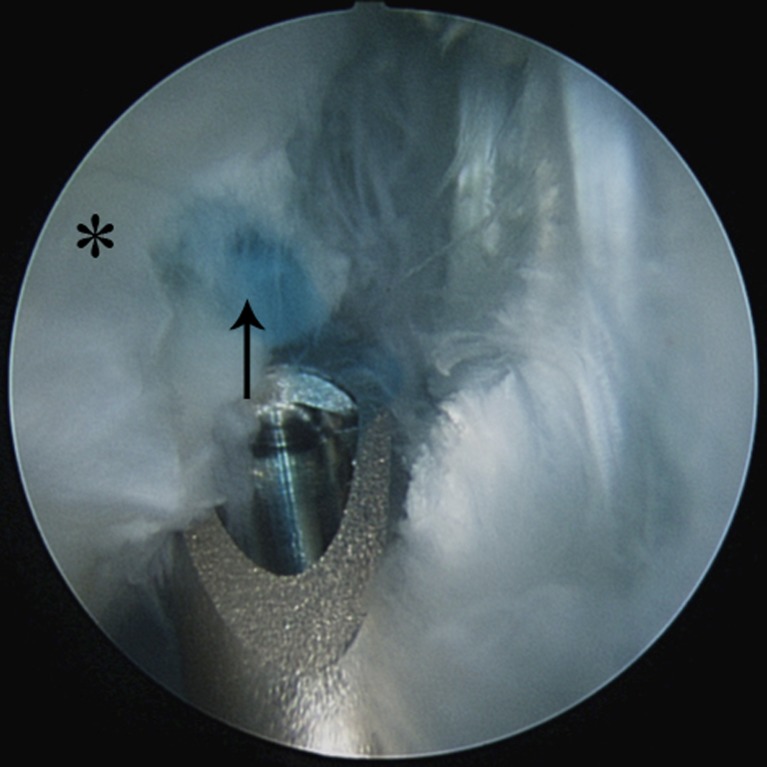
Fig. 3.
Excision of the cyst and stalk is performed using a motorized shaver. The back of the shaver protects the dorsal scapholunate ligament (asterisk, *). The dye may be seen entering the dorsal scapholunate ligament (arrow)
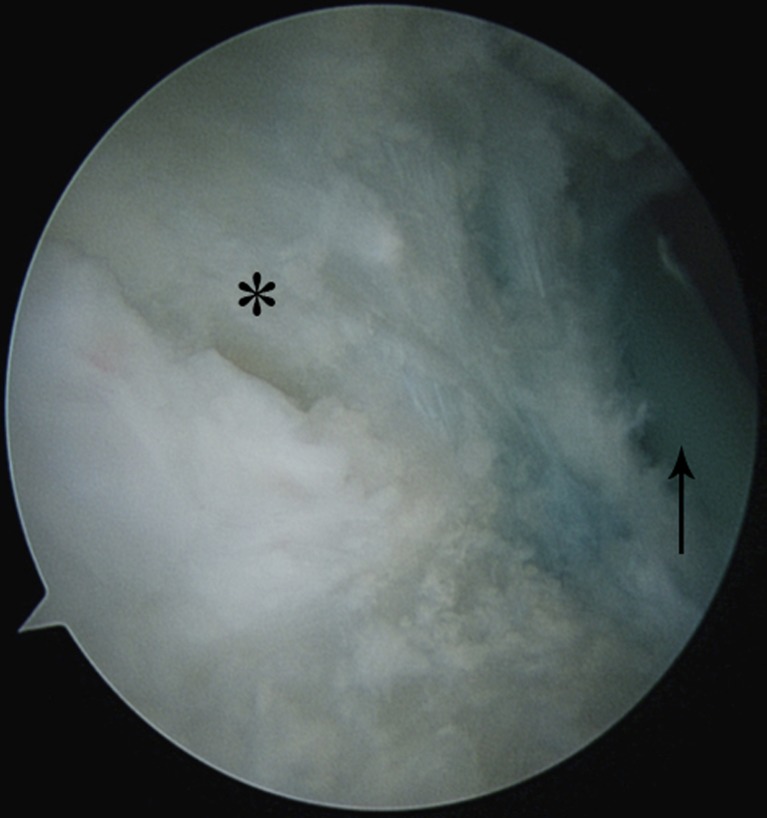
Fig. 4.
View of the dorsal scapholunate ligament following complete excision of the stalk and cyst. The dorsal scapholunate ligament is identified by the asterisk (*) and the extensor tendons are identified by the arrow
Results
Twenty-seven patients who underwent arthroscopic excision of dorsal wrist ganglia with the color-aided technique were identified. This cohort consisted of 20 females and 7 males with an average age of 33 years (range 17–63). The ganglion stalk was documented to be completely visualized in all 27 cases (100 %) following the indigo carmine injection. Of this identified patient population, one patient experienced recurrence 8 months after surgery. Telephone communication was successful with all 27 patients with an average post-operative duration of 25 months (range 12–42 months). Incidence of recurrence was calculated to be 3.7 %. No intraoperative complications were identified.
Discussion
With the evolution of wrist arthroscopy as a well-accepted method for the excision of DWG, this color-aided visualization technique provides an option for improved visualization of the ganglion stalk, thereby improving the efficacy of this procedure. Visualization of the stalk is essential to confirm complete excision of the ganglion stalk. However, variable rates of stalk visualization have been reported in the literature, ranging from 9 to 100 %. Osterman and Raphael [13] reported 79 % visualization of the ganglion stalk. Kang et al [9]. reported identification of the stalk in 41 of 41 arthroscopic resections, but the clarity and completeness of visualization are not reported. Edwards and Johansen [5] in contrast have identified the stalk in 4 of 45 cases (9 %). Comparably, Rizzo et al [14]. report stalk visibility in 12 of 41 cases of resection. Yamamoto et al [16]. described a new sonography-aided technique for arthroscopic resection of DWG and report identification of the ganglion stalk in all 22 patients (100 %). In our experience, the ganglion stalk was completely visualized in 100 % of the cases with prior injection of indigo carmine dye.
Clear visualization of the stalk will increase surgeon confidence that the stalk has been adequately visualized and resected. This may be achieved by the use of this simple and safe introduction of the inert Indigo Carmine dye [17]. A nearly identical technique, substituting methylene blue dye has also been described [10]. This improved visualization will prevent the need for extensive capsular debridement and will decrease the rate of conversion to open excision, thereby reducing associated complications [17]. In our personal experience, there was a 0 % conversion rate to open excision. Surgical methods also involve the debridement of the dorsal capsule surrounding the stalk. However, without clear identification of the stalk, the area of pathologic or redundant capsular tissue is debrided at the surgeon's discretion [10]. Iatrogenic scapholunate and lunatotriquetral ligament injuries and subsequent instabilities have been reported to be associated with arthroscopic DWG excision [5,13], further supporting the need to avoid excessive debridement and potential destabilization of the wrist.
Recurrence rates of arthroscopic DWG excision with a minimum of 1-year follow-up have been cited by a number of studies with varying patient cohorts, ranging from 0 to 12.3 % [4–6,12–15]. Recurrence rate of open excision has been reported as 8.7 % in a prospective study of 31 patients by Kang et al [9].. This study of color-aided arthroscopic excision reports a recurrence rate of 3.7 % based on a 27-patient cohort, which represents one recurrence.
The overall incidence of complications associated with any wrist arthroscopy has been reported as 4.7 % [1]. However, there was no surgical complication in this study. No additional risks have been associated with the injection of the inert Indigo Carmine dye.
This technique helps to facilitate a more ideal resection that is limited to the pathologic tissue, preventing post-operative joint instability. Furthermore, this color-aided technique is safe and a potentially valuable tool for surgeons seeking improved confidence that the ganglion stalk has been clearly visualized. Confirmation of complete excision of the stalk may help decrease the risk of recurrence leading to improved results with arthroscopic DWG resection. Although our recurrence rate of 3.7 % was similar to that seen in other studies, this was represented by only one recurrence due to the small size of this cohort. Interestingly, the patient with the recurrence was the very first patient we treated with this technique, suggesting there may be a small learning curve associated with the use of this technique.
Based upon our clinical experience with this technique, we do not recommend arthroscopic excision of MRI-diagnosed occult ganglia as inconsistent visualization of the ganglion stalk may lead to recurrence. Alternatively, we recommend open resection of occult ganglia in the event these patients fail conservative management options.
Complete visualization of the DWG stalk is essential to confirm complete excision of the DWG. The technique of using color-assisted visualization supports this endeavor in a safe and practical method.
This study has limitations. The sample size of patients with adequate follow-up is limited, and there is no control group without color-aided arthroscopic resection. The lack of a control group limits our ability to directly compare our outcomes, and we are unable to definitively conclude that this technique is superior to DWG excision without dye assistance. Compared to historical controls, our recurrence rates are comparable if not slightly better than arthroscopic ganglion excision without the benefit of color-assisted visualization. Also, the morbidity of this adjunctive tool is low, and we feel the potential benefits as discussed above outweigh any risk. Further assessment with prospective, randomized controlled studies is warranted.
The color-aided technique for arthroscopic DWG visualization was found to be a safe and valuable tool for surgeons performing arthroscopic DWG resection. The ganglion stalk was identified in 100 % of the procedures and the patients responded well with a low incidence of recurrence.
Acknowledgments
Conflict of interest
Both authors declare that they have no conflict of interest.
Informed consent statement
Informed consent was obtained from all patients for being included in the study. No patient-identifying information is included in the manuscript. IRB approval was obtained for retrospective review.
Human and animal rights statement
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Footnotes
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
References
- 1.Ahsan ZS, Yao J. Complications of wrist arthroscopy. Arthroscopy. 2012;28(6):855–9. doi: 10.1016/j.arthro.2012.01.008. [DOI] [PubMed] [Google Scholar]
- 2.Angelides AC, Wallace PF. The dorsal ganglion of the wrist: its pathogenesis, gross and microscopic anatomy, and surgical treatment. J Hand Surg. 1976;1(3):228–35. doi: 10.1016/S0363-5023(76)80042-1. [DOI] [PubMed] [Google Scholar]
- 3.Aslani H, Najafi A, Zaaferani Z. Prospective outcomes of arthroscopic treatment of dorsal wrist ganglia. Orthopedics. 2012;34(3):395–400. doi: 10.3928/01477447-20120222-13. [DOI] [PubMed] [Google Scholar]
- 4.Chen ACY, Lee WC, Hsu KY, et al. Arthroscopic ganglionectomy through an intrafocal cystic portal for wrist ganglia. Arthroscopy. 2010;26(5):617–22. doi: 10.1016/j.arthro.2009.08.021. [DOI] [PubMed] [Google Scholar]
- 5.Edwards SG, Johansen JA. Prospective outcomes and associations of wrist ganglion cysts resected arthroscopically. J Hand Surg [Am] 2009;34(3):395–400. doi: 10.1016/j.jhsa.2008.11.025. [DOI] [PubMed] [Google Scholar]
- 6.Gallego S, Mathoulin C. Arthroscopic resection of dorsal wrist ganglia: 114 cases with minimum follow-up of 2 years. Arthroscopy. 2010;26(12):1675–82. doi: 10.1016/j.arthro.2010.05.008. [DOI] [PubMed] [Google Scholar]
- 7.Geissler WB. Arthroscopic excision of dorsal wrist ganglia. Tech Hand Upper Extrem Surg. 1998;2(3):196–201. doi: 10.1097/00130911-199809000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Geissler WB. Excision of dorsal wrist ganglia. Wrist Arthroscopy; 2005. p. 139–44.
- 9.Kang L, Akelman E, Weiss A-PC. Arthroscopic versus open dorsal ganglion excision: a prospective, randomized comparison of rates of recurrence and of residual pain. J Hand Surg [Am] 2008;33(4):471–5. doi: 10.1016/j.jhsa.2008.01.009. [DOI] [PubMed] [Google Scholar]
- 10.Lee BJ, Sawyer GA, Dasilva MF. Methylene blue-enhanced arthroscopic resection of dorsal wrist ganglions. Tech Hand Upper Extrem Surg. 2011;15(4):243–6. doi: 10.1097/BTH.0b013e3182206c49. [DOI] [PubMed] [Google Scholar]
- 11.Luchetti R, Badia A, Alfarano M, Orbay J, Indriago I, Mustapha B. Arthroscopic resection of dorsal wrist ganglia and treatment of recurrences. J Hand Surg (Br) 2000;25(1):38–40. doi: 10.1054/jhsb.1999.0290. [DOI] [PubMed] [Google Scholar]
- 12.Mathoulin C, Hoyos A, Pelaez J. Arthroscopic resection of wrist ganglia. Hand Surg. 2004;09(02):159–64. doi: 10.1142/S0218810404002169. [DOI] [PubMed] [Google Scholar]
- 13.Osterman AL, Raphael J. Arthroscopic resection of dorsal ganglion of the wrist. Hand Clin. 1995;11(1):7–12. [PubMed] [Google Scholar]
- 14.Rizzo M, Berger RA, Steinmann SP, Bishop AT. Arthroscopic resection in the management of dorsal wrist ganglions: results with a minimum 2-year follow-up period. J Hand Surg [Am] 2004;29(1):59–62. doi: 10.1016/j.jhsa.2003.10.018. [DOI] [PubMed] [Google Scholar]
- 15.Shih J-T, Hung S-T, Lee H-M, Tan C-M. Dorsal ganglion of the wrist: results of treatment by arthroscopic resection. Hand Surg. 2002;7(1):1–5. doi: 10.1142/S0218810402000856. [DOI] [PubMed] [Google Scholar]
- 16.Yamamoto M, Kurimoto S, Okui N, Tatebe M, Shinohara T, Hirata H. Sonography-guided arthroscopy for wrist ganglion. J Hand Surg [Am] 2012;37(7):1411–5. doi: 10.1016/j.jhsa.2012.04.012. [DOI] [PubMed] [Google Scholar]
- 17.Yao J, Trindade MCD. Color-aided visualization of dorsal wrist ganglion stalks aids in complete arthroscopic excision. Arthroscopy. 2011;27(3):425–9. doi: 10.1016/j.arthro.2010.10.017. [DOI] [PubMed] [Google Scholar]