Abstract
Extramedullary pulmonary hematopoiesis is a rare entity with a limited number of case reports in the available literature only. We report the case of a 66-year-old man with known primary myelofibrosis, in whom a Technetium-99m sulfur colloid bone marrow scan with single-photon emission computed tomography (SPECT)/CT revealed a pulmonary hematopoiesis as the cause of pulmonary hypertension and severe tricuspid regurgitation. To the best of our knowledge, this is the first description of Technetium-99m sulfur colloid SPECT/CT imaging in this rare condition.
Keywords: Extramedullary pulmonary hematopoiesis, Pulmonary hypertension, Tricuspid regurgitation, Technetium-99m sulfur colloid bone marrow scan, SPECT/CT
INTRODUCTION
Pulmonary hypertension has an association with chronic myeloproliferative disorders (1). The causes are multifactorial, with extramedullary pulmonary hematopoiesis being described as a rare etiological factor (2). Extramedullary hematopoiesis is the production of blood cells outside of the bone marrow. This occurs in conditions such as myeloproliferative disorders, hemoglobinopathies and marrow infiltrating diseases. In chronic myeloproliferative disorders, extramedullary hematopoiesis in the lungs may be suspected on computed tomography (CT) chest scans in the presence of diffuse ground-glass opacities or interstitial thickening (3). We report the case of a 66-year-old man in whom chest CT scan did not reveal any lung parenchymal abnormality. A pulmonary extramedullary hematopoiesis causing pulmonary hypertension and severe tricuspid regurgitation was diagnosed on Technetium-99m (Tc-99m) sulfur colloid bone marrow scan and single-photon emission computed tomography (SPECT)/CT.
CASE REPORT
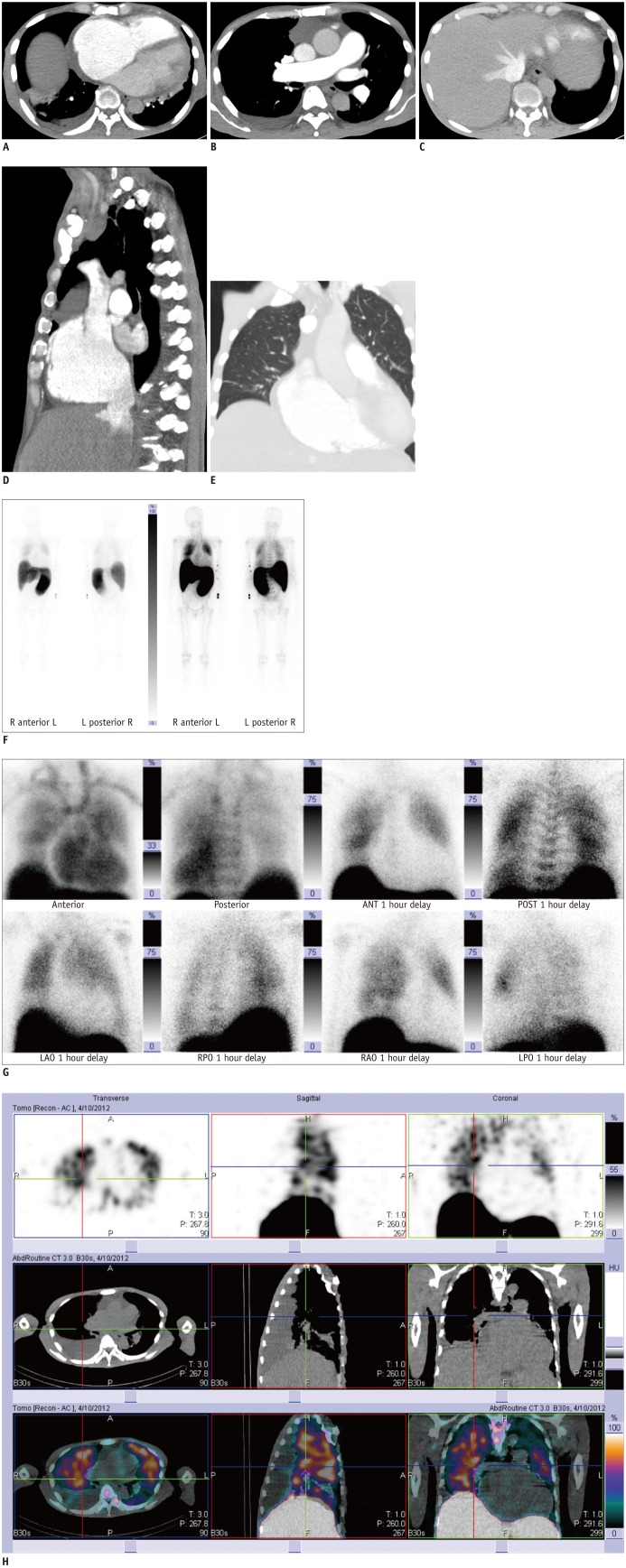
A 66-year-old man with a known primary myelofibrosis (diagnosed in December 2008 at an outside institution) presented to our hospital with complaints of shortness of breath and abdominal bloating in March 2012. He had multiple hospital admissions for the worsening of its dyspnea over the previous two years. On clinical examination, he was dyspneic with an elevated jugular venous pressure and bipedal pitting edema. Moderate hepatomegaly and massive splenomegaly were noted. The total white cell count was markedly raised (41.2 × 109/L) with a low hemoglobin level (5.3 g/dL). The platelet count was normal (371 × 109/L). The chest radiograph showed an enlarged heart. A CT pulmonary angiogram did not show any pulmonary embolism; however, the right atrium and the main pulmonary arteries were dilated, suggesting a pulmonary hypertension with reflux of contrast into the inferior vena cava and hepatic veins (Fig. 1A-D). No parenchymal abnormality was detected in the lung (Fig. 1E). The two-dimensional echocardiography confirmed a severe tricuspid regurgitation with marked right atrial dilatation and moderately impaired right-ventricular systolic function. A Tc-99m sulfur colloid bone marrow scan with SPECT/CT imaging was performed (Symbia, Siemens Medical Solutions, Erlangen, Germany) with a background history of primary myelofibrosis to exclude pulmonary hematopoiesis as the cause of pulmonary hypertension. The planar gamma imaging showed a hepatosplenomegaly with increased tracer accumulation in the spleen, compatible with an increased hematopoietic activity resulting from an underlying myelofibrosis (Fig. 1F). A moderate degree of tracer activity in a diffuse pattern was noted in both thoracic regions (Fig. 1G). The SPECT/CT imaging confirmed the location of an increased thoracic tracer activity in the lungs (Fig. 1H). Imaging findings were consistent with an extramedullary pulmonary hematopoiesis. A lung biopsy was not carried out in view of the increased risk of pulmonary hemorrhage in the presence of pulmonary hypertension. A hydroxyurea treatment was started for the patient to control the markedly raised total leukocyte count and massive splenomegaly. Concurrently, he was referred to a short course radiation-therapy to the lungs with view to achieve control of the pulmonary hematopoiesis.
Fig. 1.
66-year-old man with primary myelofibrosis.
A-D. Chest CT images show contrast-filled dilated main pulmonary artery, dilated right atrium with retrograde opacification of inferior vena cava and hepatic veins due to tricuspid regurgitation. E. Chest CT (lung window-settings) did not show any lung parenchymal abnormality.
F. Tc-99m sulfur-colloid bone marrow scan image shows hepatosplenomegaly and moderately increased tracer activity in both hemithoracic regions. G. Tc-99m sulfur-colloid bone marrow scan (planar spot views) shows moderate degree of tracer uptake in diffuse pattern in both thoracic regions. Cardiac silhouette is enlarged. ANT = anterior, LAO = left anterior oblique, LPO = left posterior oblique, POST = posterior, RAO = right anterior oblique, RPO = right posterior oblique, Tc-99m = Technetium-99m
H. Single-photon emission computed tomography/CT images show pulmonary tracer (Technetium-99m sulfur colloid) activity in both lungs confirming pulmonary hematopoiesis.
DISCUSSION
Extramedullary hematopoiesis is seen in chronic myeloproliferative disorders, such as myelofibrosis. The usual sites of extramedullary hematopoiesis are the liver, spleen and intrathoracic paraspinal regions (3). Lungs and pleura are rare sites of extramedullary hematopoiesis with less than forty cases of pulmonary extramedullary hematopoiesis described in the current literature (4).
A causal association between pulmonary hematopoiesis leading to dyspnea and pulmonary hypertension has been postulated in few case reports and a limited number of cohort studies (1, 2, 5). García-Manero et al. (1) listed hematopoietic infiltration of the pulmonary parenchyma as one of the probable causes of pulmonary hypertension in patients with myelofibrosis. Rumi et al. (6) described the case of a 49-year-old man in whom dyspnea due to pulmonary hematopoiesis was a presenting feature of myelofibrosis.
In most of case reports describing pulmonary extramedullary hematopoiesis, the diagnosis was suspected on the chest CT scan due to abnormalities such as ground-glass opacities (4) or interstitial septal thickening (6). Ground-glass opacities per se are non-specific CT findings with more common differentials of congestive cardiac failure and lung infection in patients presenting with dyspnea. In the setting of myelofibrosis, additional possibilities include pulmonary extramedullary hematopoiesis, thromboembolism or chemotherapy-induced lung toxicity (7). In our case, the unique finding was the absence of any lung parenchymal abnormality on CT scan.
An increased lung uptake of Tc-99m sulfur colloid is not specific to an extramedullary pulmonary hematopoiesis. It can occur after liver and bone marrow transplantation, hepatic veno-occlusive disease, liver cirrhosis, liver metastases or hepatic chemotherapy toxicity (8). A possible mechanism is the stimulation of reticulo-endothelial elements in the lung interstitium or an induction of pulmonary macrophages. Our patient did not have any other complicating factors apart from myelofibrosis.
The localization of increased tracer activity in the lungs was sufficiently demonstrated on SPECT/CT imaging. In addition, SPECT/CT imaging also aided in confirming absence of tracer activity within the pleural spaces, thus excluding any pleural site of extramedullary hematopoiesis. We believe that SPECT/CT imaging, if available, should be included in the imaging protocol of suspected pulmonary hematopoiesis, as it can localize tracer activity in the lungs or pleura, which is not possible on a two-dimensional planar imaging. A histopathological confirmation of pulmonary hematopoiesis could not be obtained as a lung biopsy was not performed in our patient. However, pulmonary hematopoiesis was considered the most likely diagnosis in the absence of other complicating factors which could have resulted in an increased lung uptake of Tc-99m sulfur colloid.
In summary, extramedullary pulmonary hematopoiesis in myelofibrosis leading to pulmonary hypertension and tricuspid regurgitation is a rare condition. This case report highlights the utility of Tc-99m sulfur colloid bone marrow scan in cases of unexplained pulmonary hypertension with underlying myeloproliferative disorders. We believe that an inclusion of SPECT/CT imaging helps to confirm and characterize the pulmonary involvement. It should be performed in addition to a routine planar gamma camera imaging.
References
- 1.García-Manero G, Schuster SJ, Patrick H, Martinez J. Pulmonary hypertension in patients with myelofibrosis secondary to myeloproliferative diseases. Am J Hematol. 1999;60:130–135. doi: 10.1002/(sici)1096-8652(199902)60:2<130::aid-ajh8>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 2.Dingli D, Utz JP, Krowka MJ, Oberg AL, Tefferi A. Unexplained pulmonary hypertension in chronic myeloproliferative disorders. Chest. 2001;120:801–808. doi: 10.1378/chest.120.3.801. [DOI] [PubMed] [Google Scholar]
- 3.Georgiades CS, Neyman EG, Francis IR, Sneider MB, Fishman EK. Typical and atypical presentations of extramedullary hemopoiesis. AJR Am J Roentgenol. 2002;179:1239–1243. doi: 10.2214/ajr.179.5.1791239. [DOI] [PubMed] [Google Scholar]
- 4.Trow TK, Argento AC, Rubinowitz AN, Decker R. A 71-year-old woman with myelofibrosis, hypoxemia, and pulmonary hypertension. Chest. 2010;138:1506–1510. doi: 10.1378/chest.10-0973. [DOI] [PubMed] [Google Scholar]
- 5.Schwarz C, Bittner R, Kirsch A, Loddenkemper C, Mairinger T, Schonfeld N, et al. A 62-year-old woman with bilateral pleural effusions and pulmonary infiltrates caused by extramedullary hematopoiesis. Respiration. 2009;78:110–113. doi: 10.1159/000150913. [DOI] [PubMed] [Google Scholar]
- 6.Rumi E, Passamonti F, Boveri E, De Amici M, Astori C, Braschi M, et al. Dyspnea secondary to pulmonary hematopoiesis as presenting symptom of myelofibrosis with myeloid metaplasia. Am J Hematol. 2006;81:124–127. doi: 10.1002/ajh.20509. [DOI] [PubMed] [Google Scholar]
- 7.Bajwa AA, Usman F, Wolfson D, Laos LF, Cury JD. A 62-year-old woman with dyspnea, leukocytosis, and diffuse ground-glass opacities. Chest. 2010;137:1470–1473. doi: 10.1378/chest.09-2602. [DOI] [PubMed] [Google Scholar]
- 8.Jacobson AF, Marks MA, Kaplan WD. Increased lung uptake on technetium-99m-sulfur colloid liver-spleen scans in patients with hepatic venoocclusive disease following bone marrow transplantation. J Nucl Med. 1990;31:372–374. [PubMed] [Google Scholar]