Abstract
Adaptive optics (AO) is a technology used to improve the performance of optical systems by reducing the effect of wave front distortions. Retinal imaging using AO aims to compensate for higher order aberrations originating from the cornea and the lens by using deformable mirror. The main application of AO retinal imaging has been to assess photoreceptor cell density, spacing, and mosaic regularity in normal and diseased eyes. Apart from photoreceptors, the retinal pigment epithelium, retinal nerve fiber layer, retinal vessel wall and lamina cribrosa can also be visualized with AO technology. Recent interest in AO technology in eye research has resulted in growing number of reports and publications utilizing this technology in both animals and humans. With the availability of first commercially available instruments we are making transformation of AO technology from a research tool to diagnostic instrument. The current challenges include imaging eyes with less than perfect optical media, formation of normative databases for acquired images such as cone mosaics, and the cost of the technology. The opportunities for AO will include more detailed diagnosis with description of some new findings in retinal diseases and glaucoma as well as expansion of AO into clinical trials which has already started.
Keywords: Retinal imaging, Adaptive optics technology
Introduction
Imaging of the human retina has undergone revolutionary changes thanks to which we are able to view miniscule retinal structures and its abnormalities. Current retinal imaging modalities are mostly non-invasive and provide high resolution of the tissue with good topographic orientation. Conventional color fundus imaging, scanning laser ophthalmoscopy (SLO) and optical coherence tomography (OCT) have become routine in clinical practice. Newer technologies are constantly under investigation and often underway.
Retinal cameras for current clinical imaging are generally designed without correcting aberrations beyond defocus. In order to bring the lateral resolution of ophthalmoscopes to the microscopic scale, it is necessary to compensate not only for defocus, but also astigmatism and higher order aberrations. Similarly, current OCT technology provides excellent axial resolution of images but less precise lateral resolution. Adaptive optics (AO) is a technology used to improve the performance of optical systems by reducing the effect of wavefront distortions (aberrations) (Table 1). It was first used in astronomical telescopes and laser communication systems to remove the effects of atmospheric distortion, later in microscopy and optical fabrication to reduce optical aberrations. Adaptive optics works by measuring the distortions in a wavefront and compensating for them with a device that corrects those errors such as a deformable mirror or a liquid crystal array.1–3
Table 1.
Differences between optical coherence tomography and adaptive optics technology.
| Optical coherence tomography | Adaptive optics | |
|---|---|---|
| Principle | Low coherence interferometry | Correction of wave front distortions |
| Detectors/correctors | Reference mirror/spectrally separated detectors | Deformable mirrors |
| Attachment devices | Charge-coupled device (CCD) camera | Scanning laser ophthalmoscope/retinal camera |
| Type of resolution | Axial | Lateral |
| Image type | B-scan | En-face image |
Retinal imaging using AO aims to compensate for higher order aberrations (deviation of light from the ideal shape) originating from the cornea and the lens. This is done by using deformable mirror which serves as wavefront corrector. The first use of retinal AO allowed visualization of single cone photoreceptors. Currently, both cone and rod individual photoreceptors can be imaged using this technology (Fig. 1).4,5 AO systems have been coupled to scanning laser ophthalmoscope (SLO),6 flood-illuminated camera,7 and optical coherence tomography.8
Figure 1.
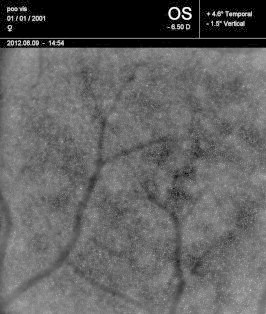
An image of photoreceptor mosaic in a young healthy myopic eye using adaptive optics retinal camera (ImagineEyes, Orsay, France) demonstrating a homogeneous mosaic of retinal cones and rods (Image by Dr. Igor Kozak).
Clinical applications
The main application of AO retinal imaging has been to assess photoreceptor cell density, spacing, and mosaic regularity in normal eyes and various ocular diseases. Analysis of the spatial distribution of the cone photoreceptors provides new information on the physical aspects of visual sampling of the human eye. Apart from photoreceptors, the retinal pigment epithelium (RPE) cells can be seen using reflectance-based AO imaging.9 The retinal nerve fiber layer, retinal vessel wall and lamina cribrosa can also be visualized with AO technology (Fig. 2).10–12 Patient factors, such as unstable fixation, small pupil size, and media opacities, can present challenges with image stabilization and light scatter, resulting in image blur. Considerable image processing effort is required to collect and produce the highest resolution images, including registration, montaging, and quantitative analysis.3 Despite all these challenges, retinal AO has been successfully used in several disease entities in ophthalmology.
Figure 2.

An image of the same eye as in Fig. 1 using the same instrument but focusing on the inner retina showing retinal nerve fibers and details of retinal blood vessels (Image by Dr. Igor Kozak).
Diabetic retinopathy
Diabetic retinopathy (DR) is a microangiopathy resulting in blood rheological abnormalities as a consequence of chronic hyperglycemia.11,12 Rather than purely a vascular disease it is now considered a neurovascular disorder. It has been observed that excess plasma glucose may not account for all cellular and functional changes in the progression of DR. In addition to high glucose, the dysregulated levels of excitotoxic metabolites, nutrients, hormones and several other factors, have been found to play a role in neurodegeneration in DR.13 The neurodegeneration in DR consists of apoptosis affecting the photoreceptors, bipolar and ganglion cells.14
Retinal microvascular and perfusion changes in patients with diabetes have been observed even in the eyes with no or minimal clinical retinopathy.15,16 These changes have been demonstrated by SLO-based AO imaging without the use of contrast enhancing agents in both cross-sectional17 and longitudinal assessment.18 Non-invasive assessment of the capillary network has been performed using AO-OCT and AO retinal camera.19,20 Recently, a subtle decrease of parafoveal cone density was found in diabetic patients in comparison with age-matched control subjects. The cone density decline was moderately associated with a disturbance in the glucose metabolism.21 AO has been used to visualize photoreceptors after macular laser photocoagulation with pattern laser. In small observation, no evidence of reduced photoreceptor density around the laser lesions, no apparent size reduction of the lesions relative to the initial application diameters, and, thus no direct evidence of photoreceptor migration or healing were found.22
Age-related macular degeneration
Age-related macular degeneration (AMD) is a multifactorial disease that can cause severe vision loss due to either tissue loss in the macula or development of subfoveal choroidal neovascular membranes.23 While the changes in late stages of AMD are known, there is interest to image, characterize and monitor very early stages of the disease. The idea is to be able to measure disease burden, such as lipofuscin or drusen volume, in order to predict the course of the disease.24–26
Few studies report on the use of AO to monitor drusen progression and assess their direct effect on the overlying photoreceptors (Fig. 3).27,28 En face AO IR imaging was used to study and characterize regressing drusen in AMD.29 An increase in photoreceptor disruption was visualized within the macula in direct correlation with the stage of AMD progression leading to a decrease in visual acuity. Large coalescent drusen and areas of geographic atrophy in advanced stage dry AMD exhibited a significant decrease in visible photoreceptor density.30 Adaptive SLO has been reported to provide adequate resolution for quantitative measurement of cone spacing at the margin of geographic atrophy and over drusen in eyes with AMD. Although cone spacing was observed to be often normal at baseline and remained normal over time, these regions showed focal areas of decreased cone reflectivity.31 Geographic atrophy was studied using AO-OCT which showed that the inner segment/outer segment junctions lost reflectivity at the margins of GA, while visual function was still demonstrated. This was shown to be due to changes in photoreceptor orientation near the GA border (Fig. 4).32 AO near infrared imaging has been reported to improve the resolution of the changes affecting the RPE in GA when compared to SLO.33
Figure 3.
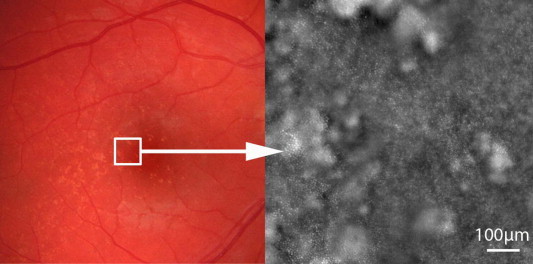
LEFT PANEL: A fundus color image of an eye with early age-related macular degeneration shows numerous small yellowish drusen. RIGHT PANEL: A small retinal area of the same eye imaged by adaptive optics retinal camera (ImagineEyes, Orsay, France) demonstrating preservation of photoreceptors overlying the drusen (Images by Prof. Michel Paques, Quinze-Vingts Hospital, Paris, France).
Figure 4.
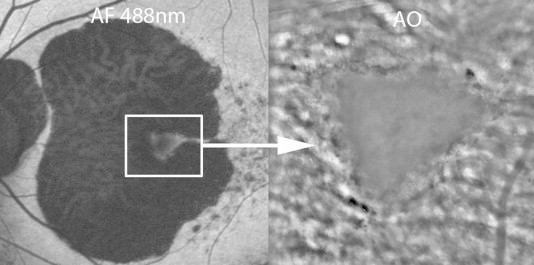
LEFT PANEL: A fundus autofluorescence image of an eye with late age-related macular degeneration shows an extensive area of geographic atrophy with preservation of foveal tissue. RIGHT PANEL: An area of foveal tissue imaged by adaptive optics retinal camera (ImagineEyes, Orsay, France) demonstrating hyper- and hyporeflective areas and general absence of photoreceptors (Images by Prof. Michel Paques, Quinze-Vingts Hospital, Paris, France).
First attempts have been made to image mosaic of the retinal pigment epithelium (RPE) cells in the living human eye.34 This was demonstrated by combining fluorescence imaging methods with adaptive optics scanning light ophthalmoscopy (FAOSLO). Most recently this technique was improved by the focusing method to address poor compensation of the longitudinal chromatic aberration and has been used to obtain the first in vivo glimpse of the RPE mosaic in AMD.35
Retinal dystrophies
Retinal dystrophies are a group of progressive retinal degenerations that eventually lead to loss of vision. Symptoms associated with cone dysfunction include reduction of visual acuity, impaired color vision, and photophobia. Patients with predominantly rod dysfunction complain of nyctalopia.36 The primary cell type affected in this group of diseases is the photoreceptors which can be visualized with AO-based imaging instruments. Therefore AO technology has been used to study retinal dystrophies and degenerations.
One of the first observations was made in patients with color vision deficit where AO found a reduction of one type of cone rather than total absence of particular cone type as previously thought.37 Another significant observation is that both cone and rod photoreceptors vary in their intensity over time.38,39 An interesting study has demonstrated that there is a discrepancy between cone structure and function. In a group of patients with inherited retinal degenerations, cone density was found to be reduced by up to 62% below normal at or near the fovea in eyes with visual acuity and sensitivity that remained within normal limits. Despite a significant correlation with foveal cone spacing, visual acuity and sensitivity seemed to be insensitive indicators of the integrity of the foveal cone mosaic.40 Recently, numerous retinal dystrophies have been imaged using AO retinal imaging but most reports are limited to few cases or imaging of family members with a specific condition.41–46
AO-based retinal imaging can provide a sensitive structural outcome measures for clinical trials with new therapies for inherited retinal degenerations. For example, in patients with retinitis pigmentosa receiving ciliary neurotrophic factor, AO scanning laser ophthalmoscopy revealed a relative preservation of cone structure despite an absence of significant functional improvement.47 Alternatively, this technology can be applied for proper selection of patients for specific clinical trials.48
Glaucoma
Glaucoma is the leading cause of irreversible, preventable blindness worldwide. Primary open angle glaucoma (POAG) is a chronic optic neuropathy characterized by progressive loss of retinal ganglion cells, usually associated with ocular hypertension, leading to structural damage of the inner retinal layers, as shown by progressive regional or diffuse thinning of the retinal nerve fiber layer (RNFL). Axonal tissue loss in the RNFL has been reported to be one of the earliest detectable glaucomatous changes.49
Three areas of study using AO technology have been of interest in glaucoma. It is a study of fine structure of the RNFL, study of the lamina cribrosa and the study of the outer retina. In one of the first studies, AO-OCT outperformed high resolution OCT in visualization of the RNFL in living eyes.10 Another study using AO scanning laser ophthalmoscopy, measured the individual nerve fiber bundles width in normal adult controls. In all the eyes, the AOSLO images showed hyperreflective bundles, representing the nerve fiber bundles, in the RNFL. Dark lines among the hyperreflective bundles were considered to represent Müller cell septa.50 The same group showed reduced nerve fiber bundle widths both in clinically normal and abnormal areas of glaucomatous eyes associated with visual field defects. AO SLO thus may be useful for detecting early nerve fiber bundle abnormalities associated with loss of visual function.51
AOSLO has been found useful imaging technology for assessing lamina cribrosa. In a recent study, the laminar pore area was found to be affected by axial length and IOP.52 A 3-D reconstruction of the monkey lamina cribrosa was achieved combining en face AOSLO and spectral domain OCT imaging.53
In human patients with glaucoma, investigators reported a loss in cone density along with the thinning of the inner retina. Defects in the cone mosaic co-localized to the areas of reduced visual sensitivity measured by visual field testing.54 In separate patients, the same authors observed that the areas of reduced visual field sensitivity were not different from normal areas in their inner photoreceptor segment lengths, whereas the outer photoreceptor lengths were shorter and more variable in retinal areas associated with sensitivity loss. These same areas showed a disruption in visibility of Verhoeff’s membrane.55
Animal imaging in retinal research
Progress in imaging of animal retina has been going hand in hand with developments in imaging technology. Rodent models are instrumental in the study of retinal disease mechanisms and in the development of treatments for human retinal dystrophies. The majority of studies using rodent disease models rely upon retinal histopathology to follow disease progression and the effect of candidate therapies. Histopathology yields high resolution images and morphometric estimates of surviving retinal cells; however, it does not allow longitudinal studies in the same animals. In vivo imaging of the rodent retina offers the possibility to visualize disease processes and progression in individual animals and to reduce the effects of animal to animal variation, background lighting and genetic background.56
The resolution of in vivo imaging is limited by the optical quality of the rodent eye. Compared with the human eye, rodent eyes have smaller axial lengths, higher optical powers, larger average refractive errors and larger numerical apertures. Rats typically have a large hyperopic refractive error. Many studies have used fluorescence microscopy, fundus photography, two photon microscopy, confocal microscopy, or scanning laser ophthalmoscopy to image the living rodent retina, allowing the visualization of structures such as blood vessels, capillaries, nerve fiber bundles, photoreceptors, retinal ganglion cells, retinal pigment epithelial cells and microglial cells.57–59 Resolution in all of these studies could be improved by correcting the eye’s aberrations with AO so that many fine features that could previously be resolved only in excised retina could now be imaged in vivo. Adaptive optics ophthalmoscopes have enabled near diffraction-limited imaging of cellular structures (such as individual photoreceptors, ganglion cells, and RPE cells) in living human and non-human primates as well as the resolution of subcellular features (such as ganglion cell axons and dendrites) in living non-human primates.60–63
Fluorescence scanning laser ophthalmoscope equipped with adaptive optics (fAOSLO) has enabled visualization of cellular and subcellular features in the rat retina, such as fine capillaries and individual fluorescently-labeled ganglion cell dendrites and axons.56 Using the same technology it was possible to image individual RPE cells in vivo in monkeys34 Reflectance imaging with AO also allows for the imaging of other cell types, such as astrocytes or pericytes. Imaging of retinal ganglion cells (RGCs) remains extremely difficult because they are almost transparent and therefore invisible in optical systems. In animal models, contrast agents can be used to improve the visualization of RGCs but these techniques are not feasible in humans.64 High resolution cone mosaic has been achieved with AO in chick retina with important implications for future studies of myopia.65
Conclusions
Recent interest in adaptive optics technology in eye research has resulted in growing number of reports and publications utilizing this technology in both animals and humans. With the availability of first commercially available instruments we are making transformation of AO technology from a research tool to diagnostic instrument. The current challenges include imaging eyes with less than perfect optical media, formation of normative databases for acquired images such as cone mosaics, and the cost of the technology. The opportunities for AO will include more detailed diagnosis with description of some new findings in retinal diseases and glaucoma as well as expansion of AO into clinical trials which has already started. This can allow for more sensitive monitoring and evaluation of response to newly developed treatments.
Conflict of interest
The authors declared that there is no conflict of interest.
Footnotes
The author has no proprietary interest in any product or technology mention in this article.
Peer review under responsibility of Saudi Ophthalmological Society, King Saud University.
References
- 1.Beckers J.M. Adaptive optics for astronomy: principles, performance, and applications. Annu Rev Astronomy Astrophys. 1993;31(1):13–62. [Google Scholar]
- 2.Godara P., Dubis A.M., Roorda A., Duncan J.L., Carroll J. Adaptive optics retinal imaging: emerging clinical applications. Optom Vis Sci. 2010;87:930–941. doi: 10.1097/OPX.0b013e3181ff9a8b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lombardo M., Serrao S., Devaney N. Adaptive optics technology for high-resolution retinal imaging. Sensors. 2013;13:334–366. doi: 10.3390/s130100334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim J.E., Chung M. Adaptive optics for retinal imaging. Retina. 2013;33(8):1483–1486. doi: 10.1097/IAE.0b013e31828cd053. [DOI] [PubMed] [Google Scholar]
- 5.Miller D.T., Williams D.R., Morris G.M., Liang J. Images of cone photoreceptors in the living human eye. Vision Res. 1996;36:1067–1079. doi: 10.1016/0042-6989(95)00225-1. [DOI] [PubMed] [Google Scholar]
- 6.Roorda A., Romero-Borja F., Donnelly W., III Adaptive optics scanning laser ophthalmoscopy. Opt Express. 2002;10:405–412. doi: 10.1364/oe.10.000405. [DOI] [PubMed] [Google Scholar]
- 7.Rha J., Jonnal R.S., Thorn K.E. Adaptive optics flood- illumination camera for high speed retinal imaging. Opt Express. 2006;14:4552–4569. doi: 10.1364/oe.14.004552. [DOI] [PubMed] [Google Scholar]
- 8.Zawadski R.J., Cense B., Zhang Y. Ultrahigh-resolution optical coherence tomography with monochromatic and chromatic aberration correction. Opt Express. 2008;16:8126–8143. doi: 10.1364/oe.16.008126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Roorda A., Zhang Y., Duncan J.L. High-resolution in vivo imaging of the RPE mosaic in eyes with retinal disease. Invest Ophthalmol Vis Sci. 2007;48:2297–2303. doi: 10.1167/iovs.06-1450. [DOI] [PubMed] [Google Scholar]
- 10.Kocaoglu O.P., Cense B., Jonnal R.S. Imaging retinal nerve fiber bundles using optical coherence tomography with adaptive optics. Vision Res. 2011;51:1835–1844. doi: 10.1016/j.visres.2011.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Takayama K., Ooto S., Hangai M. High-resolution imaging of the retinal nerve fiber layer in normal eyes using adaptive optics scanning laser ophthalmoscopy. PLoS One. 2012;7(3):e33158. doi: 10.1371/journal.pone.0033158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ivers K.M., Li C., Patel N. Reproducibility of measuring lamina cribrosa pore geometry in human and nonhuman primates with in vivo adaptive optics imaging. Invest Ophthalmol Vis Sci. 2011;52:5473–5480. doi: 10.1167/iovs.11-7347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Moore J., Bagley S., Ireland G. Three dimensional analysis of microaneurysms in the human diabetic retina. J Anat. 1999;194:89–110. doi: 10.1046/j.1469-7580.1999.19410089.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee S.N., Chhablani J., Chan C.K. Characterization of microaneurysm closure after laser photocoagulation in diabetic macular edema. Am J Ophthalmol. 2013;155(5):905–912. doi: 10.1016/j.ajo.2012.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ola M.S., Nawaz M.I., Siddiquei M.M. Recent advances in understanding the biochemical and molecular mechanism of diabetic retinopathy. J Diab Complicat. 2012;26:56–64. doi: 10.1016/j.jdiacomp.2011.11.004. [DOI] [PubMed] [Google Scholar]
- 16.Van Dijk H.W., Kok P.H., Garvin M. Selective loss of inner retinal layer thickness in type 1 diabetic patients with minimal diabetic retinopathy. Invest Ophthalmol Vis Sci. 2009;50:3404–3409. doi: 10.1167/iovs.08-3143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tam J., Dhamdere K.P., Tiruveedhula P. Disruption of the retinal parafoveal capillary network in type 2 diabetes before the onset of diabetic retinopathy. Invest Ophthalmol Vis Sci. 2011;52:9257–9266. doi: 10.1167/iovs.11-8481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tam J., Dhamdere K.P., Tiruveedhula P. Subclinical capillary changes in non-proliferative diabetic retinopathy. Optom Vis Sci. 2012;89:E692–E703. doi: 10.1097/OPX.0b013e3182548b07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang Q., Kocaoglu O.P., Cense B. Imaging retinal capillaries using ultrahigh-resolution optical coherence tomography and adaptive optics. Invest Ophthalmol Vis Sci. 2011;52:6292–6299. doi: 10.1167/iovs.10-6424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lombardo M., Parravano M., Serrao S. Analysis of retinal capillaries in patients with type 1 diabetes and nonproliferative diabetic retinopathy using adaptive optics imaging. Retina. 2013;33(8):1630–1639. doi: 10.1097/IAE.0b013e3182899326. [DOI] [PubMed] [Google Scholar]
- 21.Lombardo M., Parravano M., Lombardo G. Adaptive optics imaging of parafoveal cones in type 1 diabtes. Retina. 2013 doi: 10.1097/IAE.0b013e3182a10850. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 22.Han D.P., Croskrey J.A., Dubis A.M. Adaptive optics and spectral- domain optical coherence tomography of human photoreceptor structure after short-duration [corrected] pascal macular grid and panretinal laser photocoagulation. Arch Ophthalmol. 2012;130(4):518–521. doi: 10.1001/archophthalmol.2011.2878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bressler N.M. Age-related macular degeneration is the leading cause of blindness. JAMA. 2004;291:1900–1901. doi: 10.1001/jama.291.15.1900. [DOI] [PubMed] [Google Scholar]
- 24.Freeman S.R., Kozak I., Cheng L. Optical coherence tomography-raster scanning and manual segmentation in determining drusen volume in age-related macular degeneration. Retina. 2010;30(3):431–435. doi: 10.1097/IAE.0b013e3181bd2f94. [DOI] [PubMed] [Google Scholar]
- 25.Sparrow J.R., Blonska A., Flynn E. Quantitative fundus autofluorescence in mice: correlation with HPLC quantitation of RPE lipofuscin and measurement of retina outer nuclear layer thickness. Invest Ophthalmol Vis Sci. 2013;54(4):2812–2820. doi: 10.1167/iovs.12-11490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Greenberg J.P., Duncker T., Woods R.L. Quantitative fundus autofluorescence in healthy eyes. Invest Ophthalmol Vis Sci. 2013;54(8):5684–5693. doi: 10.1167/iovs.13-12445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Querques G., Massamba N., Guigui B. In vivo evaluation of photoreceptor mosaic in early onset large colloid drusen using adaptive optics. Acta Ophthalmologica. 2012;90:e327–e328. doi: 10.1111/j.1755-3768.2011.02228.x. [DOI] [PubMed] [Google Scholar]
- 28.Godara P., Siebe C., Rha J. Assessing the photoreceptor mosaic over drusen using adaptive optics and SD-OCT. Ophthalmic Surg Lasers Imaging. 2011;41:S104–S108. doi: 10.3928/15428877-20101031-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Querques G., Kamami-Levy C., Georges A. Appearance of regressing drusen on adaptive optics in age-related macular degeneration. Ophthalmology. 2013 doi: 10.1016/j.ophtha.2013.10.006. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 30.Boretsky A., Khan F., Burnett G. In vivo imaging of photoreceptor disruption associated with age-related macular degeneration: a pilot study. Lasers Surg Med. 2012;44:603–610. doi: 10.1002/lsm.22070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zayit-Soudry S., Duncan J.L., Syed R. Cone structure imaged with adaptive optics scanning laser ophthalmoscopy in eyes with nonneovascular age-related macular degeneration. Invest Ophthalmol Vis Sci. 2013;54(12):7498–7509. doi: 10.1167/iovs.13-12433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Panorgias A., Zawadzki R.J., Capps A.G. Multimodal assessment of microscopic morphology and retinal function in patients with geographic atrophy. Invest Ophthalmol Vis Sci. 2013;54(6):4372–4384. doi: 10.1167/iovs.12-11525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gocho K., Sarda V., Falah S. Adaptive optics imaging of geographic atrophy. Invest Ophthalmol Vis Sci. 2013;54(5):3673–3680. doi: 10.1167/iovs.12-10672. [DOI] [PubMed] [Google Scholar]
- 34.Morgan J.I.W., Dubra A., Wolfe R. In vivo autofluorescence imaging of the human and macaque retinal pigment epithelial cell mosaic. Invest Ophthalmol Vis Sci. 2008;50(3):1350–1359. doi: 10.1167/iovs.08-2618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rossi E.A., Rangel-Fonseca P. In vivo imaging of retinal pigment epithelium cells in age related macular degeneration. Biomed Opt Express. 2013;4(11):2527–2539. doi: 10.1364/BOE.4.002527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Thiadens A.A., Phan T.M., Zekveld-Vroon R.C. Clinical course, genetic etiology, and visual outcome in cone and cone-rod dystrophy. Ophthalmology. 2012;119:819–826. doi: 10.1016/j.ophtha.2011.10.011. [DOI] [PubMed] [Google Scholar]
- 37.Carroll J., Neitz M., Hofer H. Functional photoreceptor loss revealed with adaptive optics: an alternate cause of color blindness. Proc Natl Acad Sci USA. 2004;101(22):8461–8466. doi: 10.1073/pnas.0401440101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jonnal R.S., Besecker J.R., Derby J.C. Imaging outer segment renewal in living human cone photorecptors. Opt Express. 2010;18:5257–5270. doi: 10.1364/OE.18.005257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cooper R.F., Dubis A.M., Pavaskar A. Spatial and temporal variation of rod photoreceptor reflectance in the human retina. Biomed Opt Express. 2011;2:2577–2589. doi: 10.1364/BOE.2.002577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ratnam K., Carroll J., Porco T.C. Relationship between foveal cone structure and clinical measures of visual function in patients with inherited retinal degenerations. Invest Ophthalmol Vis Sci. 2013 Aug 28;54(8):5836–5847. doi: 10.1167/iovs.13-12557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kay D.B., Land M.E., Cooper R.F. Outer retinal structure in Best vitelliform macular dystrophy. JAMA Ophthalmol. 2013 Sep;131(9):1207–1215. doi: 10.1001/jamaophthalmol.2013.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Park S.P., Hong I.H., Tsang S.H. Disruption of the human cone photoreceptor mosaic from a defect in NR2E3 transcription factor function in young adults. Graefes Arch Clin Exp Ophthalmol. 2013;251(10):2299–2309. doi: 10.1007/s00417-013-2296-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chen Y., Ratnam K., Sundquist S.M. Cone photoreceptor abnormalities correlate with vision loss in patients with Stargardt disease. Invest Ophthalmol Vis Sci. 2011:3281–3292. doi: 10.1167/iovs.10-6538. 17;52(6) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Duncan J.L., Talcott K.E., Ratnam K. Cone structure in retinal degeneration associated with mutations in the peripherin/RDS gene. Invest Ophthalmol Vis Sci. 2011;52(3):1557–1566. doi: 10.1167/iovs.10-6549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Vincent A., Wright T., Garcia-Sanchez Y. Phenotypic characteristics including in vivo cone photoreceptor mosaic in KCNV2-related “cone dystrophy with supernormal rod electroretinogram”. Invest Ophthalmol Vis Sci. 2013;54(1):898–908. doi: 10.1167/iovs.12-10971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Syed R., Sundquist S.M., Ratnam K. High-resolution images of retinal structure in patients with choroideremia. Invest Ophthalmol Vis Sci. 2013;54(2):950–961. doi: 10.1167/iovs.12-10707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Talcott K.E., Ratnam K., Sundquist S. Longitudinal study of cone photoreceptors during retinal degeneration and in response to ciliary neurotrophic factor treatment. Invest Ophthalmol Vis Sci. 2011;52:2219–2226. doi: 10.1167/iovs.10-6479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Carroll J., Kay D.B., Scoles D. Adaptive optics retinal imaging – clinical opportunities and challenges. Curr Eye Res. 2013;38(7):709–721. doi: 10.3109/02713683.2013.784792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Quigley H.A. Glaucoma. Lancet. 2011;377:1367–1377. doi: 10.1016/S0140-6736(10)61423-7. [DOI] [PubMed] [Google Scholar]
- 50.Takayama K., Ooto S., Hangai High-resolution imaging of the retinal nerve fiber layer in normal eyes using adaptive optics scanning laser ophthalmoscopy. PLoS One. 2012 doi: 10.1371/journal.pone.0033158. doi: 10.1371/journal.pone.0033158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Takayama K., Ooto S., Hangai M. High-resolution imaging of retinal nerve fiber bundles in glaucoma using adaptive optics scanning laser ophthalmoscopy. Am J Ophthalmol. 2013;155(5):870–881. doi: 10.1016/j.ajo.2012.11.016. [DOI] [PubMed] [Google Scholar]
- 52.Akagi T., Hangai M., Takayama K. In vivo imaging of lamina cribrosa pores by adaptive optics scanning laser ophthalmoscopy. Invest Ophthalmol Vis Sci. 2012;53(7):4111–4119. doi: 10.1167/iovs.11-7536. [DOI] [PubMed] [Google Scholar]
- 53.Sredar N., Ivers K.M., Queener H.M. 3D modeling to characterize lamina cribrosa surface and pore geometries using in vivo images from normal and glaucomatous eyes. Biomed Opt Express. 2013;4(7):1153–1165. doi: 10.1364/BOE.4.001153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Choi S.S., Zawadzki R.J., Lim M.C. Evidence of outer retinal changes in glaucoma patients as revealed by ultrahigh-resolution in vivo retinal imaging. Br J Ophthalmol. 2011;95(1):131–141. doi: 10.1136/bjo.2010.183756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Werner J.S., Keltner J.L., Zawadzki R.J., Choi S.S. Outer retinal abnormalities associated with inner retinal pathology in nonglaucomatous and glaucomatous optic neuropathies. Eye (Lond) 2011;25(3):279–289. doi: 10.1038/eye.2010.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Geng Y., Greenberg K.P., Wolfe R. In vivo imaging of microscopic structures in the rat retina. Invest Ophthalmol Vis Sci. 2009;50(12):5872–5879. doi: 10.1167/iovs.09-3675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Thanos S., Indorf L., Naskar R. In vivo FM: using conventional fluorescence microscopy to monitor retinal neuronal death in vivo. Trends Neurosci. 2002;25:441–444. doi: 10.1016/s0166-2236(02)02246-4. [DOI] [PubMed] [Google Scholar]
- 58.Seeliger M.W., Beck S.C., Pereyra-Muñoz N. In vivo confocal imaging of the retina in animal models using scanning laser ophthalmoscopy. Vision Res. 2005;45:3512–3519. doi: 10.1016/j.visres.2005.08.014. [DOI] [PubMed] [Google Scholar]
- 59.Biss D.P., Sumorok D., Burns S.A. In vivo fluorescent imaging of the mouse retina using adaptive optics. Opt Lett. 2007;32:659–661. doi: 10.1364/ol.32.000659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Gray D.C., Merigan W., Wolfing J.I. In vivo fluorescence imaging of primate retinal ganglion cells and retinal pigment epithelial cells. Opt Express. 2006;14:7144–7158. doi: 10.1364/oe.14.007144. [DOI] [PubMed] [Google Scholar]
- 61.Geng Y., Dubra A., Yin L. Adaptive optics retinal imaging in the living mouse eye. Biomed Opt Express. 2012;3(4):715–734. doi: 10.1364/BOE.3.000715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bueno J.M., Giakoumaki A., Gualda E.J. Analysis of the chicken retina with an adaptive optics multiphoton microscope. Biomed Opt Express. 2011;2(6):1637–1648. doi: 10.1364/BOE.2.001637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Williams D.R. Imaging single cells in the living retina. Vision Res. 2011;51(13):1379–1396. doi: 10.1016/j.visres.2011.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Prasse M., Rauscher F.G., Wiedemann P. Optical properties of retinal tissue and the potential of adaptive optics to visualize retinal ganglion cells in vivo. Cell Tissue Res. 2013;353(2):269–278. doi: 10.1007/s00441-013-1602-1. [DOI] [PubMed] [Google Scholar]
- 65.Headington K., Choi S.S., Nickla D., Doble N. Single cell imaging of the chick retina with adaptive optics. Curr Eye Res. 2011;36(10):947–957. doi: 10.3109/02713683.2011.587934. [DOI] [PMC free article] [PubMed] [Google Scholar]



