Abstract
Purpose
To report four cases of premacular hemorrhage secondary to valsalva retinopathy treated with Nd:YAG membranotomy and discuss techniques as well as the literature.
Design
Retrospective case series.
Methods
A retrospective review was conducted for four patients with vision obstructing hemorrhage secondary to valsalva retinopathy. These patients were all treated with Nd:YAG membranotomy.
Results
Four patients with premacular hemorrhage secondary to valsalva retinopathy were treated with Nd:YAG laser creating a membranotomy to drain the hemorrhage. Power settings ranged from 1.7 to 3.8 mJ. Visual acuity at presentation ranged from 20/400 (1 patient) to count fingers (3 patients). Visual acuity improved in three out of four patients after laser treatment. Final visual acuity ranged from 20/20 to 20/30 in these three patients. One patient was lost to follow up after performing laser membranotomy and therefore visual acuity after treatment was not obtained. No complications were noted.
Conclusion
Nd:YAG membranotomy is a non-invasive, office-based treatment option that may be successfully used to treat premacular hemorrhage secondary to valsalva retinopathy.
Keywords: Valsalva retinopathy, YAG membranotomy, Premacular hemorrhage
Introduction
Premacular hemorrhage is a rare source of painless loss of vision. Causes include valsalva retinopathy,1–8 proliferative diabetic retinopathy,9–11 vein occlusion,1 macroaneurysm,11–16 hematologic disorders17,18 and trauma1,19 among others.7,20 The typical funduscopic appearance is that of a well-circumscribed hemorrhage at the vitreoretinal interface. The blood is believed to accumulate in the potential space under the internal limiting membrane (ILM) especially for valsalva related instances,3,6,21 or between the ILM and hyaloid face.
Management options include observation, Neodymium:YAG laser (Nd:YAG) membranotomy and pars plana vitrectomy. Spontaneous resolution can take several weeks or months depending on the thickness and total amount of blood present. The prolonged presence of sub-ILM blood may lead to the development of significant epiretinal tissue proliferation.8 While pars plana vitrectomy likely has the greatest anatomic success rate, the well-known complications limit immediate use in the majority of situations.7 Nd:YAG hyaloidotomy has been reported to be a relatively safe and effective method of draining premacular hemorrhage into the vitreous cavity.1–3,5,7,8,10,11,14,19,22–26 In this report, we describe several cases of successful use of Nd:YAG laser in the treatment of premacular hemorrhage due to valsalva retinopathy as well as a discussion of the literature and techniques.
Methods
Patient records were reviewed from 1 private retina practice (Retina Consultants of Michigan) and 1 academic retina practice (Henry Ford Health Systems) for those with vision loss secondary to premacular hemorrhage associated with valsalva retinopathy between 2007 and 2011. Four total records were obtained and analyzed. For the discussion, an online PubMed literature search was conducted using keywords, “valsalva retinopathy”, “preretinal hemorrhage”, and “YAG.” Additional sources were obtained for the discussion from the references within the articles obtained. The Institutional Review Board from Henry Ford Health Systems approved this study and the authors adhered to the principles of the Declaration of Helsinki for clinical research.
Description of cases
Case 1
A 26 year-old female presented with complaints of sudden painless vision loss in her right eye following an episode of emesis three days prior. She had no past ocular history. Her past medical history was significant for rheumatoid arthritis and medications were plaquenil, daypro, azulfidine, venlafaxine and birth control pills. On examination, her visual acuity was 20/400 OD eccentrically and 20/20 OS. Intraocular pressures and anterior chamber examination were normal bilaterally. Dilated fundus examination of the right eye showed a large subhyaloid hemorrhage covering most of the macula including the fovea (Fig. 1 A).
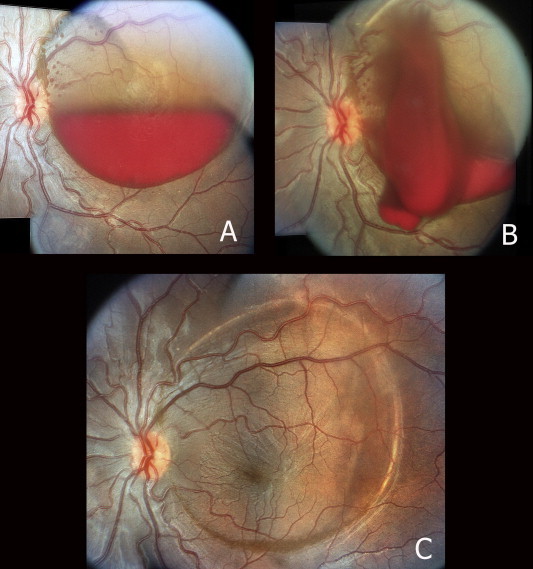
Figure 1.
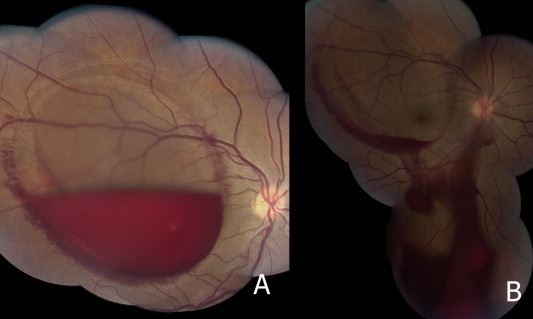
(A) Montage color fundus photograph from case 1 demonstrating a boat-shaped premacular hemorrhage due to valsalva retinopathy. (B) Color montage following Neodymium:YAG (Nd:YAG) hyaloidotomy, the hemorrhage drains inferiorly into vitreous.
Nd:YAG was applied in single shots to the hyaloid face beginning at 1.7 mJ without appreciable effect. The laser power was titrated through 2.9 mJ without effect. Finally, a single shot at 3.8 mJ led to successful photodisruption. The majority of blood immediately drained into the inferior vitreous (Fig. 1 B) with near complete recovery of vision.
Three days after the procedure, the vision in her right eye was 20/25. Dilated fundus examination showed inferior vitreous hemorrhage with complete clearing in front of the macula. One month later, she was 20/25+ with further clearing of vitreous hemorrhage. The retina remained flat and no complications were encountered. Three years after her initial presentation, vision improved further to 20/20 and examination showed wrinkling of the detached ILM over the macula without evidence of epiretinal membrane or subretinal fibrosis (Fig. 2A and B).
Figure 2.
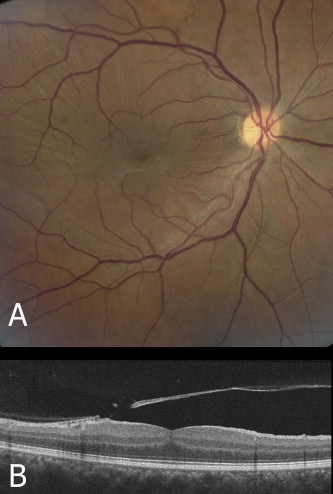
(A) Color fundus photograph three years after successful Nd:YAG hyaloidotomy of the patient in Case 1, there is wrinkling of posterior hyaloid. (B) Corresponding vertical optical coherence tomography scan shows the detached internal limiting membrane (attached to posterior hyaloid) with an opening secondary to Nd:YAG membranotomy without underlying retinal damage.
Case 2
A 35 year-old woman who was 35 weeks pregnant with twins presented with a 10 day history of sudden painless loss of vision in her right eye which developed after a prolonged episode of sneezing and coughing. Her past ocular history was significant for photorefractive keratectomy 11 years prior. Her past medical history was significant for a normal pregnancy and upper respiratory infection. Prenatal vitamins were her only medication.
On examination, her corrected visual acuity was counting fingers OD and 20/30-OS. Anterior segment examination was unremarkable bilaterally. Dilated fundus exam of the right eye showed a boat-shaped preretinal hemorrhage covering the macula as well as a larger area of subretinal hemorrhage along the superotemporal arcade (Fig. 3A). Due to the premacular hemorrhage, it was not possible to determine if subretinal hemorrhage extended under the central macula. OCT showed dense preretinal hemorrhage leading to shadowing which precluded analysis of the subretinal space (Fig. 3D). Dense subretinal fluid can be seen adjacent to the area not obscured by the shadow effect.
Figure 3.
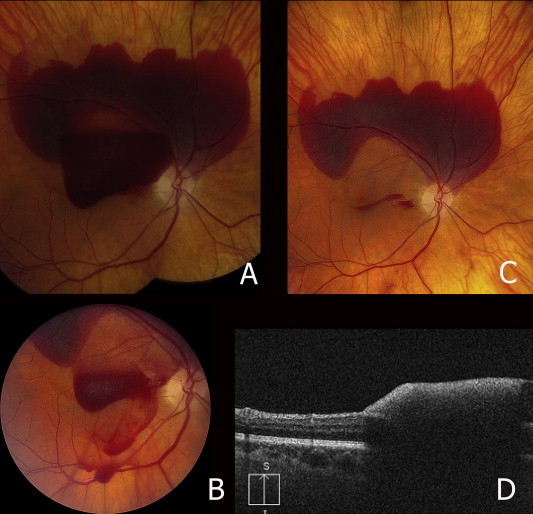
(A) Color fundus montage photograph of case 2 showing premacular hemorrhage and a larger area of subretinal hemorrhage along superotemporal arcade. (B) Color fundus montage immediately following Nd:YAG membranotomy with active drainage of blood. (C) Three days later, color fundus photograph shows that the fovea is uncovered and the subretinal blood appears stable. (D) Corresponding vertical OCT shows shadow effect of the preretinal hemorrhage obstructing the image of the underlying retina and subretinal space.
Nd:YAG photodisruption was applied. Initial settings were single shot at 2.5 mJ power without effect. Power was then titrated to 3.4 mJ, after which a single shot caused the desired membranotomy. Immediate drainage of the blood into the inferior vitreous cavity was noted (Fig. 3B). The subretinal hemorrhage along the superotemporal arcades did not extend into the macula and did not appear to descend after deflation of the sub-ILM fluid pocket. Three days later, visual acuity in the right eye improved to 20/25+. Fundus examination showed that the premacular hemorrhage had almost completely resolved and subretinal hemorrhage along the superotemporal arcade appeared stable (Fig. 3C).
Case 3
A 31 year-old female presented to a general ophthalmologist complaining of sudden onset of painless loss of vision in her left eye after an episode of emesis earlier that day. Her past ocular and medical histories were unremarkable and she took no medications. Visual acuity was 20/20 OD and counting fingers OS. Dilated fundus examination of the left eye revealed a well-circumscribed preretinal hemorrhage in the macula with intraretinal hemorrhages along the superotemporal arcade (Fig. 4A). The patient was lost to follow-up for 3 weeks when return visit showed that visual acuity OS remained counting fingers. Dilated examination showed fibrinoid debris above partially dehemoglobinized blood in the sub-hyaloid space in front of the macula (Fig. 4B). Successful membranotomy in the posterior hyaloid was performed using the Nd:YAG laser (Fig. 4C and D). Most of the hemorrhage however remained intact in a large clot and did not drain. The patient was subsequently lost to follow up.
Figure 4.
(A) Color fundus photograph of case 3 showing a well-circumscribed premacular hemorrhage with intraretinal hemorrhages along the superotemporal arcade and along the peripheral border of the pre-retinal blood. (B) Color fundus photograph 3 weeks later demonstrating the blood dehemoglobinized and clotted. (C and D) Color fundus photograph immediately after Nd:YAG membranotomy shows blood flowing through membranotomy site, but drainage was minimal due to coagulation.
Case 4
A 17 year-old female presented with complaints of sudden painless loss of vision in her left eye for 1 day. She had no pertinent past medical history and was not taking medication. Her visual acuity was 20/30 OD and counting fingers OS. Fundus examination of the left eye showed a well-circumscribed pre-retinal hemorrhage obstructing the fovea (Fig. 5). Fluorescein angiography showed central blocking without evidence of leakage or other vascular abnormalities in the fundus.
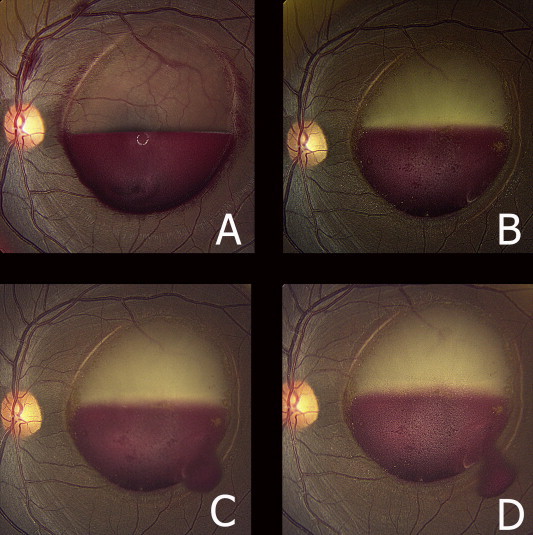
Figure 5.
(A) Montage color photograph of case 4 demonstrating dense premacular hemorrhage. (B) Color montage photograph shows successful Nd:YAG membranotomy performed 6 weeks following initial presentation. (C) Color fundus photograph 4 months after Nd:YAG membranotomy shows complete resolution of hemorrhage with early wrinkling of the ILM.
Given the classic clinical appearance, a diagnosis of valsalva retinopathy was made. The patient and her parents elected to observe initially. The patient returned after 6 weeks when her vision remained counting fingers and posterior segment examination showed persistent hemorrhage obscuring the central macula (Fig. 5A). Nd:YAG was applied to the inferior portion of the hemorrhage with 2 shots at 2.5 mJ (Fig. 5 B). One day after the procedure, the patient noted significant visual improvement and 6 weeks later visual acuity measured 20/30. Four month follow up showed that the vision improved to 20/30+ with early wrinkling of the elevated ILM (Fig. 5 C). No complications were encountered.
Discussion
Nd:YAG membranotomy was first described by Faulborn in 1988 to drain premacular subhyaloid hemorrhage into the vitreous cavity.27 Since, there have been many case reports and series in the literature describing similar Nd:YAG membranotomy, with energy levels ranging from 2.5 to 50 mJ, with relatively good success.1–4,6,7,11,14,25–29
Premacular hemorrhage may lead to sudden vision loss due to a number of underlying etiologies. In valsalva retinopathy, the increase in venous pressure is theorized to rupture smaller capillaries in the superficial retina30 resulting in sub-ILM hemorrhage or bleeding into the subhyaloid space. Spontaneous resolution of premacular hemorrhage is possible but absorption may take many months.31 During this period, intraretinal tissue migration and proliferation may lead to permanent structural damage. Pathological specimens have shown tissues more similar to proliferative vitreoretinopathy than idiopathic epiretinal membranes including trans-differentiated retinal pigment epithelium (RPE) cells within the retina underneath the ILM.3 Furthermore, longstanding vitreous hemorrhage is felt to predispose to fibrovascular tissue contraction. In cases of hemorrhage besides valsalva, early treatment may allow for more rapid visualization and treatment of underlying pathology.7 This suggests that early removal of the blood with laser or vitrectomy may be warranted for reasons other than early visual recovery.7,8,31,32
The timing for treatment is critical, as successful displacement of hemorrhage is dependent on its ability to flow through the membranotomy by remaining liquid. As with previous publications,7,32,33 our case 3 demonstrates that pre-retinal hemorrhage may clot leading to failure of Nd:YAG displacement despite successful creation of an opening in the hyaloid/ILM. Case four shows that under certain circumstances, even 6 weeks after initial hemorrhage, the blood can remain liquid enough to drain fully following Nd:YAG membranotomy. Once blood has clotted, vitrectomy with manual blood removal would likely be required for early visual recovery. However, in theory, intravitreal injection of tissue plasminogen activator (TPA) may liquefy the hemorrhage well enough to allow subsequent laser displacement. While we were unable to find a publication describing this technique, TPA has been successfully used along with intraocular air injection for clotted premacular hemorrhage secondary to diabetic retinopathy.9
Ulbig et al. described a case series of 21 patients who underwent Nd:YAG laser treatment for premacular hemorrhage. Most eyes demonstrated good visualization of the macula within one month. Those patients with premacular hemorrhage from valsalva or Terson’s syndrome demonstrated best results.7 Complications up to six months after laser treatment were negligible with only one retinal detachment in a myopic patient with bilateral breaks and a single additional eye that developed a macular hole. In the latter patient, the photodisruptive effect may have been too near the macula. Khan et al. reported no ocular complications for 11 patients after laser membranotomy at 6 month follow-up.2 In a case series published by Gabel et al., energy levels up to 50 mJ were used with no retinal injury. The preretinal blood is thought to provide a buffer that protects the underlying retina from the laser energy.28 Sabella et al. identified the location of the laser photodisruption on spectral domain OCT and concluded that there was no damage to the underlying retina. We were also able to identify the ILM/hyaloid defect with spectral domain OCT (Fig. 2) and again, there was no obvious disruption of the retinal layers. In our case, the defect is close to the border of the ILM displacement where traction on the surface ILM led to structural changes unrelated to photodisruption. This tractional phenomenon is noted at the border of the ILM detachment at many sites prior to and after photodisruption in our case and can be found in previously published cases.4,29
Epiretinal membrane (ERM) and contraction of the ILM are known to occur following laser disruption of premacular hemorrhage. Kwok et al. analyzed one such membrane subsequently removed surgically and found hemosiderin deposits under the contracted ILM with fine glial ERM on the outer surface.3 It is likely this type of membrane is not laser induced, but rather a secondary effect of hemorrhagic displacement of the ILM. Case 1 also demonstrates one such membrane (Fig. 2) that remained asymptomatic. OCT demonstrates that the membrane in this case is detached from the retina surface likely minimizing symptoms for the time being.
Due to potential retinal damage, it has been advocated that Nd:YAG therapy only be considered in premacular hemorrhages of at least 3 disc diameters in size. This helps to increase the cushion effect of the hemorrhage in order to avoid inadvertent retinal damage by the photodisruptive laser.7 In our opinion, there are several important criteria to safely deliver Nd:YAG to the ILM/hyaloid face in valsalva retinopathy. First is to choose the most appropriate location. Liquid hemorrhage will drain by gravity; therefore, the easiest location to rapidly empty the trapped blood is to create a hole at the inferior aspect of the fluid pocket. That being said, a buffer is necessary between the laser spot and the underlying retina to protect the retina from the forthcoming shockwave. Therefore, a region distant enough from the inferior border where there is significant hemorrhagic elevation is required. Furthermore, a location away from the fovea is also prudent which can create difficulty when the inferior position of the hemorrhage is over the fovea. Depending on the configuration and location of the hemorrhage, it may at times be safer and therefore preferable to apply the laser to a lateral aspect of the hemorrhage and then use head positioning to drain the blood into the vitreous cavity. Case 2 demonstrates laser membranotomy on the nasal aspect of the hemorrhage in order to avoid the fovea (Fig. 3B), which required left sided head positioning to drain the maximum amount of blood. Next, the power settings certainly vary for individual situations. Common sense dictates that it is best to use the least amount of power to create an adequate opening. We suggest beginning with 2.0–2.5 mJ for situations with clear media and titrating upwards as required. Puthalath et al.25 described using “stretch burns” to the hyaloid prior to a penetrating photodisruption; however, we did not find that step necessary in our cases. Media opacities such as cataract, posterior capsular opacity, and vitreous hemorrhage will significantly alter the required power settings. The choice of lens is also individual. The Area Centralis® (Volk Optical, Inc; Mentor, OH) was used for cases 1–2 while a plano macular contact lens was used for cases 3–4.
In this series, we described the successful use of the Nd:YAG laser to drain three out of four acute cases of premacular hemorrhage due to valsalva retinopathy. One case had partial drainage due to delayed treatment and clotting of subhyaloid blood. Nd:YAG laser treatment offers a simple, relatively safe, non-invasive treatment option for drainage of premacular hemorrhage.
Conflict of interest
The authors declared that there is no conflict of interest.
Footnotes
Peer review under responsibility of Saudi Ophthalmological Society, King Saud University.
This work is supported in part by The CONNECT Network, Inc. None of the authors have proprietary/financial interest related to this manuscript.
References
- 1.Celebi S., Kukner A.S. Photodisruptive Nd:YAG laser in the management of premacular subhyaloid hemorrhage. Eur J Ophthalmol. 2001;11(3):281–286. doi: 10.1177/112067210101100312. [DOI] [PubMed] [Google Scholar]
- 2.Khan M.T., Saeed M.U., Shehzad M.S., Qazi Z.A. Nd:YAG laser treatment for valsalva premacular hemorrhages: 6 month follow up: alternative management options for preretinal premacular hemorrhages in Valsalva retinopathy. Int Ophthalmol. 2008;28(5):325–327. doi: 10.1007/s10792-007-9138-6. [DOI] [PubMed] [Google Scholar]
- 3.Kwok A.K., Lai T.Y., Chan N.R. Epiretinal membrane formation with internal limiting membrane wrinkling after Nd:YAG laser membranotomy in valsalva retinopathy. Am J Ophthalmol. 2003;136(4):763–766. doi: 10.1016/s0002-9394(03)00442-2. [DOI] [PubMed] [Google Scholar]
- 4.Meyer C.H., Mennel S., Rodrigues E.B., Schmidt J.C. Persistent premacular cavity after membranotomy in valsalva retinopathy evident by optical coherence tomography. Retina. 2006;26(1):116–118. doi: 10.1097/00006982-200601000-00024. [DOI] [PubMed] [Google Scholar]
- 5.Perez-Rico C., Montes-Mollon A., Castro-Rebollo M. Optical coherence tomography features of sub-internal limiting membrane hemorrhage and temporary premacular cavity following Nd-YAG laser membranotomy in valsalva retinopathy. Jpn J Ophthalmol. 2008;52(6):513–515. doi: 10.1007/s10384-008-0592-0. [DOI] [PubMed] [Google Scholar]
- 6.Shukla D., Naresh K.B., Kim R. Optical coherence tomography findings in valsalva retinopathy. Am J Ophthalmol. 2005;140(1):134–136. doi: 10.1016/j.ajo.2004.12.026. [DOI] [PubMed] [Google Scholar]
- 7.Ulbig M.W., Mangouritsas G., Rothbacher H.H. Long-term results after drainage of premacular subhyaloid hemorrhage into the vitreous with a pulsed Nd:YAG laser. Arch Ophthalmol. 1998;116(11):1465–1469. doi: 10.1001/archopht.116.11.1465. [DOI] [PubMed] [Google Scholar]
- 8.Gibran S.K., Kenawy N., Wong D., Hiscott P. Changes in the retinal inner limiting membrane associated with Valsalva retinopathy. Br J Ophthalmol. 2007;91(5):701–702. doi: 10.1136/bjo.2006.104935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chung J., Park Y.H., Lee Y.C. The effect of Nd:YAG laser membranotomy and intravitreal tissue plasminogen activator with gas on massive diabetic premacular hemorrhage. Ophthalmic Surg Lasers Imaging. 2008;39(2):114–120. doi: 10.3928/15428877-20080301-06. [DOI] [PubMed] [Google Scholar]
- 10.Ezra E., Dowler J.G., Burgess F. Identifying maculopathy after neodymium: YAG membranotomy for dense diabetic premacular hemorrhage. Ophthalmology. 1996;103(10):1568–1574. doi: 10.1016/s0161-6420(96)30461-2. [DOI] [PubMed] [Google Scholar]
- 11.Raymond L.A. Neodymium:YAG laser treatment for hemorrhages under the internal limiting membrane and posterior hyaloid face in the macula. Ophthalmology. 1995;102(3):406–411. doi: 10.1016/s0161-6420(95)31008-1. [DOI] [PubMed] [Google Scholar]
- 12.Zhao P., Hayashi H., Oshima K. Vitrectomy for macular hemorrhage associated with retinal arterial macroaneurysm. Ophthalmology. 2000;107(3):613–617. doi: 10.1016/s0161-6420(99)00127-x. [DOI] [PubMed] [Google Scholar]
- 13.Dahreddine M., Eldirani H., Mutsinzi E., Hirsch A. Retinal arterial macroaneurysm complicated by premacular hemorrhage: treatment by YAG laser disruption. J Fr Ophtalmol. 2011;34(2):131e1–131e5. doi: 10.1016/j.jfo.2010.09.018. [DOI] [PubMed] [Google Scholar]
- 14.Dori D., Gelfand Y., Erlik N., Miller B. Nd:YAG laser treatment for premacular hemorrhage. Ophthalmic Surg Lasers. 1998;29(12):998–1000. [PubMed] [Google Scholar]
- 15.Iijima H., Satoh S., Tsukahara S. Nd:YAG laser photodisruption for preretinal hemorrhage due to retinal macroaneurysm. Retina. 1998;18(5):430–434. doi: 10.1097/00006982-199805000-00008. [DOI] [PubMed] [Google Scholar]
- 16.Tassignon M.J., Stempels N., Van Mulders L. Retrohyaloid premacular hemorrhage treated by Q-switched Nd-YAG laser. A case report. Graefes Arch Clin Exp Ophthalmol. 1989;227(5):440–442. doi: 10.1007/BF02172895. [DOI] [PubMed] [Google Scholar]
- 17.Hlozanek M., Dotrelova D., Vrabcova T.L., Osmera J. Nd:YAG laser membranotomy treatment of premacular hemorrhage in two children with hematologic disease. Eur J Ophthalmol. 2006;16(3):478–480. doi: 10.1177/112067210601600321. [DOI] [PubMed] [Google Scholar]
- 18.Khadka D., Sharma A.K., Shrestha J.K. Nd:Yag laser treatment for sub-hyaloid hemorrhage in childhood acute leukemia. Nepal J Ophthalmol. 2012;4(1):102–107. doi: 10.3126/nepjoph.v4i1.5860. [DOI] [PubMed] [Google Scholar]
- 19.Aralikatti A.K., Haridas A.S., Smith J.M. Delayed Nd:YAG laser membranotomy for traumatic premacular hemorrhage. Arch Ophthalmol. 2006;124(10):1503. doi: 10.1001/archopht.124.10.1503. [DOI] [PubMed] [Google Scholar]
- 20.Monshizadeh R., Tariq Bhatti M., Levine L., Tabandeh H. Photodisruption of dense preretinal hemorrhage with Nd:YAG in a child with Terson’s syndrome. J AAPOS. 2002;6(1):56–58. doi: 10.1067/mpa.2002.120645. [DOI] [PubMed] [Google Scholar]
- 21.Meyer C.H., Mennel S., Rodrigues E.B., Schmidt J.C. Is the location of valsalva hemorrhages submembranous or subhyaloidal? Am J Ophthalmol. 2006;141(1):231. doi: 10.1016/j.ajo.2005.08.040. [DOI] [PubMed] [Google Scholar]
- 22.Abouzeid H., Wolfensberger T.J. Nd:YAG laser for treatment of premacular subhyaloid hemorrhage. Klin Monbl Augenheilkd. 2011;228(4):389–390. doi: 10.1055/s-0031-1273237. [DOI] [PubMed] [Google Scholar]
- 23.Adel B., Israel A., Friedman Z. Dense subhyaloid hemorrhage or subinternal limiting membrane hemorrhage in the macula treated by Nd:YAG laser. Arch Ophthalmol. 1998;116(11):1542–1543. doi: 10.1001/archopht.116.11.1542. [DOI] [PubMed] [Google Scholar]
- 24.Kaynak S., Eryildirim A., Kaynak T. Nd:YAG laser posterior hyaloidotomy in subhyaloid hemorrhage. Ophthalmic Surg. 1994;25(7):474–476. [PubMed] [Google Scholar]
- 25.Puthalath S., Chirayath A., Shermila M.V. Frequency-doubled Nd:YAG laser treatment for premacular hemorrhage. Ophthalmic Surg Lasers Imaging. 2003;34(4):284–290. [PubMed] [Google Scholar]
- 26.Zaman F., Irwin R., Godley B.F. Nd:YAG laser treatment for macular preretinal hemorrhage. Arch Ophthalmol. 1999;117(5):694–695. doi: 10.1001/archopht.117.5.694. [DOI] [PubMed] [Google Scholar]
- 27.Faulborn J. Behandlung einer diabetischen praemaculaeren Blutung mit dem Oswitched Neodym:YAG laser. Spektrum Augenheilkd. 1988;2:33–35. [Google Scholar]
- 28.Gabel V.P., Birngruber R., Gunther-Koszka H., Puliafito C.A. Nd:YAG laser photodisruption of hemorrhagic detachment of the internal limiting membrane. Am J Ophthalmol. 1989;107(1):33–37. doi: 10.1016/0002-9394(89)90811-8. [DOI] [PubMed] [Google Scholar]
- 29.Sabella P., Bottoni F., Staurenghi G. Spectral-domain OCT evaluation of Nd:YAG laser treatment for Valsalva retinopathy. Graefes Arch Clin Exp Ophthalmol. 2010;248(4):599–601. doi: 10.1007/s00417-009-1252-x. [DOI] [PubMed] [Google Scholar]
- 30.Duane T.D. Valsalva hemorrhagic retinopathy. Am J Ophthalmol. 1973;75(4):637–642. doi: 10.1016/0002-9394(73)90815-5. [DOI] [PubMed] [Google Scholar]
- 31.O’Hanley G.P., Canny C.L. Diabetic dense premacular hemorrhage. A possible indication for prompt vitrectomy. Ophthalmology. 1985;92(4):507–511. doi: 10.1016/s0161-6420(85)34014-9. [DOI] [PubMed] [Google Scholar]
- 32.Mansour A. Nd:YAG laser photodisruption of hemorrhagic detachment of the internal limiting membrane. Am J Ophthalmol. 1989;107(5):566–568. doi: 10.1016/0002-9394(89)90519-9. [DOI] [PubMed] [Google Scholar]
- 33.Cheung C.M., Benson M.T. Post-chemotherapy premacular subhyaloid haemorrhage. Eye (Lond) 2003;17(1):97–99. doi: 10.1038/sj.eye.6700273. author reply 114. [DOI] [PubMed] [Google Scholar]



