Abstract
For patients with shortened dental arches, many treatment options are available. The existing situation can be maintained by stabilizing the present dentition and improving the occlusion without extending the arch. Alternatively, the shortened dental arch can be extended by either a free-end saddle removable partial denture, cantilevered fixed bridge, or by an implant-supported prosthesis. The free-end saddle removable partial denture can be considered a simple, non-invasive, and relatively cheap treatment option for the shortened dental arch. It was believed that such prosthodontic rehabilitation would be beneficial for the patients in terms of improving oral functions. However, the existing literature indicates that the prognosis of free-end saddle removable partial denture is not predictable, it is problematic, and its contribution to oral functions in patients with shortened dental arches is considered to be dubious. This paper reviews and summarizes the current literature about the outcome of extending the shortened dental arch by a free-end saddle removable partial denture. It also outlines factors that may affect the prognosis of this prosthetic treatment.
Keywords: Free-end saddle, oral functions, partial denture, shortened dental arch, treatment option
INTRODUCTION
The shortened dental arch (SDA) is “a dentition with a reduction of occlusal units starting posteriorly.” An occlusal unit means “a pair of antagonist teeth that supports the occlusion (e.g., premolars and molars).”[1]
According to the SDA concept, all treatment efforts should be concentrated on preserving sound anterior and premolar teeth and avoiding extensive restorative treatment in the molar regions. The occlusion is stabilized and the remaining dentition is rehabilitated without replacement of missing posterior teeth.[1,2]
Clinical trials showed that an SDA comprising the anterior and premolar teeth appeared to have, in the long term, sufficient adaptive capacity to ensure adequate oral function in terms of chewing ability, aesthetics, stability of the dentition, temporomandibular joint (TMJ) function, and functional habits.[3,4,5] However, in many situations, planning the restorative dental treatment according to the SDA concept is contraindicated.[6] Furthermore, some patients, particularly younger ones, may be reluctant to leave their SDAs unrestored.[7,8,9] Also, there are still situations where extending the SDA should be considered, where loss of posterior teeth creates, for example, aesthetic problems, occlusal instability, or chewing difficulties.[10,11] When a decision is made to extend the SDA, this can be achieved by either a free-end saddle removable partial denture (FESRPD), cantilevered fixed bridge, or by an implant-supported prosthesis. The decision about what would provide the most acceptable treatment option, functionally and aesthetically, depends on a variety of factors. Clinical experience has shown that each treatment option for SDA patients has, in some respects, unsatisfactory elements. Furthermore, these options should be approached carefully after thorough assessment and detailed treatment plan. The resultant problems in treatment decision-making in this situation have resulted in it being called “a prosthodontic dilemma.”[12] The removable partial denture (RPD) can be considered a popular and simple treatment option for the SDA.[13] However, the extent to which this treatment modality may contribute to oral function in patients with SDAs is not yet clear.[14] It is also not yet clear which SDA cases are most suitable for the restoration by an FESRPD so that a positive outcome is more likely to be achieved.
The objectives of this paper are to review and summarize the current literature about the outcome of extending the SDA by an FESRPD and also to outline the factors that may affect the prognosis of such prosthetic treatment.
THE PROBLEM OF FREE-END SADDLE REMOVABLE PARTIAL DENTURE
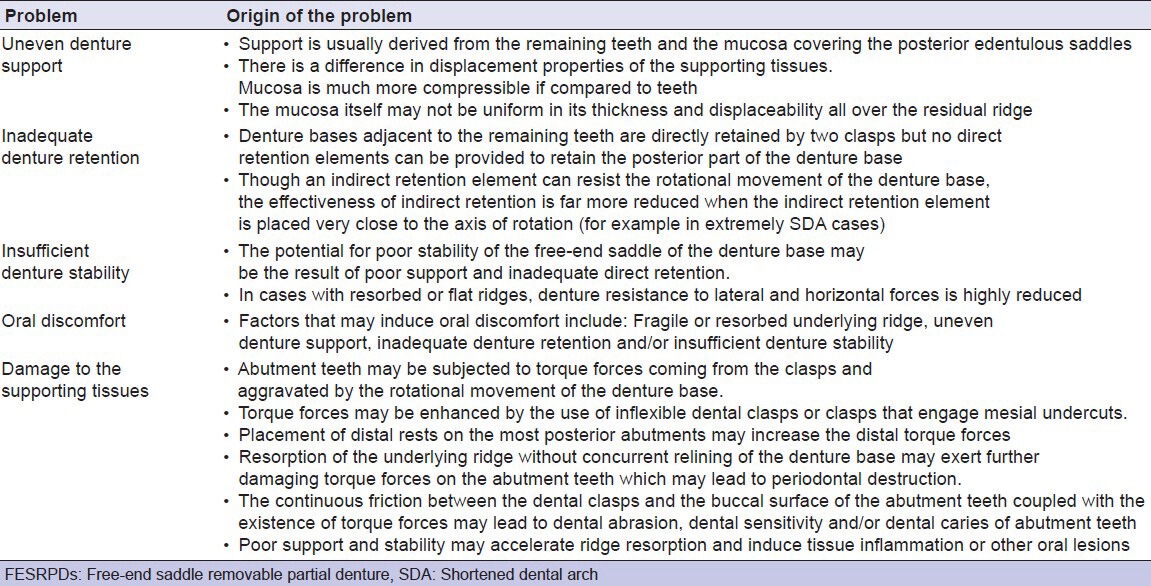
Extrapolating the existing literature shows that FESRPDs are problematic. This is because planning of an FESRPD may present the dentist with difficulty in achieving the aim of providing a satisfactory and comfortable denture because of the different and differing responses of teeth and mucosa to occlusal loads and the associated clinical problems relating to support and stability.[15] According to Ritchie,[16,17] the majority of FESRPDs, especially mandibular dentures, are not worn. The essence of this problem is related to the supporting tissues. In most cases of FESRPDs, denture support tends to be derived mainly from the mucosa covering the edentulous areas. When it is shared by the remaining teeth and associated periodontal membranes plus the mucosa of the saddles, the mixed nature of this support creates difficulty in distributing the masticatory forces in an even way. This is attributable to the difference in the displacement properties between the periodontal membrane and the mucosa; the latter is much more compressible than the periodontal membrane. When occlusal forces are applied to such RPDs in situ, uneven displacement of the supporting tissues tends to occur and the denture may rotate around an axis joining the most distal occlusal rests. These rotational forces affect the stability of the RPD and these, in turn, may generate damaging forces that in the long term may affect the abutment teeth and enhance residual ridge resorption.[18,19,20,21]
The aforementioned problem assumes greater prominence in the mandible where the available area of non-tooth support is significantly more reduced than in the maxilla where the hard palate offers greater distribution of load. As a result, the mandibular FESRPD is considered to result in, relatively speaking, more bone loss in the edentulous saddle areas of the mandible vis-à-vis the maxilla, and thereby aggravates the potential for FESRPDs to rotate about the abutment teeth[16,17,22]. Table 1 summarizes problems of FESRPDs.
Table 1.
A list of problems that may be associated with FESRPDs
CLINICAL INVESTIGATIONS ON THE OUTCOME OF TREATMENT WITH FESRPDS
Clinical surveys indicated a high failure rate of FESRPDs, especially in the mandible.[23,24,25,26,27,28] The ultimate failure may be perceived as the abandonment of wearing the provided dentures for a variety of reasons. Elias and Sheiham[29] indicated that great numbers of FESRPDs are not worn because subjective needs for the replacement of missing teeth in such cases are less than normative needs. This underlines a gap between patients’ and dentists’ perception of this prosthetic restoration. Furthermore, inadequate quality of prescription in designing RPDs for patients with SDAs has been reported.[30]
Kayser et al.[10] considered the prosthodontic intervention to extend the SDA by an FESRPD to be a kind of “overtreatment.” The same authors believed that such treatment does not contribute to the maintenance of a healthy, natural functioning dentition for life. By contrast, the provision of an FESRPD may introduce unfavorable conditions for the remaining dentition.
Clinical trials by the Nijmegen group questioned the contribution of FESRPDs to oral functions. Their work indicated that extending an SDA consisting of three to five occlusal units by an FESRPD did not lead to an evident improvement in oral function in terms of chewing ability, oral comfort, aesthetics, stability of the dentition, TMJ function, and functional habits.[31,32,33,34] Witter and associates[35] challenged what was a strongly held view for the rationale of providing RPDs. They stated that undertaking conventional removable prosthodontic intervention as a routine preventive measure in SDAs to avoid occlusal collapse should be discouraged. It seems that SDAs comprising the anterior and premolar teeth are able to maintain a long-term occlusal stability.[35,36] Moreover, when molar teeth were replaced by an FESRPD in SDA patients or not replaced in accordance with the SDA concept, no significant differences were detected between both treamtent modalities in the incidence of tooth loss at 38 months post treatment.[37] This result was confirmed over a 5 years follow-up.[38]
Leak et al.[39] studied the relationship between oral function and the number of posterior occluding pairs of teeth. The authors concluded that replacement of missing posterior teeth with an RPD would appear to have a small socio-functional impact till the patient has fewer than three posterior functional units.
Randomized controlled trials showed that extending the SDA by cantilevered fixed resin-bonded bridges offered an effective alternative treatment option to conventional mandibular RPDs at a lower biological price.[40,41] In a review of the literature, the old dogma of prescribing the RPD on prophylactic ground, that is, to prevent disorder of oral functions, was questioned. The authors indicated that the feasibility to plan the restorative dental care according to the SDA concept should preclude the indication for an RPD.[42] In line with this view, Aras et al.[43] concluded that an SDA with bilaterally missing molar teeth can be an effective alternative to FESRPDs with regard to masticatory performance despite the significant reduction in maximum occlusal force and occlusal contact area. The results of this study demonstrated no significant differences in masticatory performance between SDA subjects wearing FESRPDs and SDA subjects without an FESRPD. In extremely SDAs, rehabilitation with FESRPDs resulted in improved masticatory performance and masticatory time. However, this was not comparable with mastication levels of completely dentate subjects.[44] Creugers et al.[45] found that mandibular FESRPDs do not affect temporomandibular function and do not contribute to posterior occlusal support in SDAs comprising three to five occlusal units, with a minimum of one occlusal unit at each side. The authors indicated that such treatment option for the SDAs seems to restore only a fraction of occlusal support in terms of occlusal contacts by these dentures. A similar finding was reported by an earlier study.[46]
In a recently published systematic review, the authors concluded that the evidence is not yet sufficient to draw conclusions about the relative effectiveness of fixed partial dentures and RPDs in the restoration of the SDAs.[47]
PATIENTS’ ATTITUDES TOWARD FESRPDs
Jepson et al.[48] found that patients’ compliance with wearing RPDs was significantly related to the presence of anterior replacement teeth. Dentures that were never worn were more likely to have no replacement anterior teeth. Armellini et al.[49,50] reported similar findings and stated that RPDs had a positive impact on the quality of life of subjects with SDAs only when the denture replaced anterior teeth. The study of Nassani et al.[7] revealed that patients place little value on both acrylic and metal-based RPDs that replaced missing molar teeth in an SDA. Ikebe et al.[51] indicated that elderly patients attached higher utility values to cantilevered fixed bridges and metal FESRPDs than to the options of implants and no replacement of missing molar teeth for the SDAs. However, the study population in both the aforementioned studies[7,51] was not SDA subjects and the study design was based on hypothetical clinical scenarios. When patient satisfaction was assessed following restoration of mandibular SDAs in a randomized controlled trial, resin-bonded bridges were considered a more comfortable and acceptable treatment option when compared with bilateral FESRPDs.[52]
A multicenter randomized clinical trial[53] indicated that restoration of the SDAs with RPDs significantly improved oral health-related quality of life as measured by the Oral Health Impact Profile (OHIP-49) before treatment, and 6 and 12 months after treatment. However, only 10 out of 17 participants who received the RPD treatment completed the 12 months follow-up trial. The provided RPDs were made with conventional cast framework retained by precision attachments. Furthermore, no significant differences in oral health rating were noted between the SDA subjects who were treated by an RPD and the subjects who were treated according to the SDA concept by preservation of a premolar occlusion and non-replacement of molar support.[53]
DISCUSSION
This review summarizes the present literature about the outcome of extending the SDA by an FESRPD. It seems that that the prognosis of FESRPD is not predictable and its contribution to oral functions in patients with SDAs is considered to be dubious. The cantilevered fixed resin-bonded bridges can be considered a more efficient and comfortable treatment alternative for patients with SDAs. In some cases, extending the SDA by an FESRPD may have a positive impact on masticatory function, patient satisfaction, and oral health-related quality of life.[54] However, no significant differences in the outcome of treatment were recorded when the SDA was treated according to the SDA concept or by an FESRPD.[37,43,53,54] Moreover, restoration of the SDAs by FESRPDs incurs more costs to deliver and follow-up the treatment when compared with a functionally oriented treatment according to the SDA concept. This is coupled with increased biological price.[54,55]
Despite these findings, the FESRPD will probably continue to be a preferable treatment option when a decision is made to extend the SDA. This may be attributable to economic considerations,[42] as such treatment is relatively cheap, simple, non-invasive, and within the skills and experience of most dentists. However, in the long term, the costs of maintenance and repair and the potential for failure should be considered. It could be argued that a study into the cost-effectiveness of RPD treatment for patients with SDAs is required. The question to be raised at this point is: Which SDA cases are most suitable for the restoration by an FESRPD? To answer this question, there is a need to identify the factors that may be responsible for the success or failure of this treatment. This may lead to a more guided treatment decision.
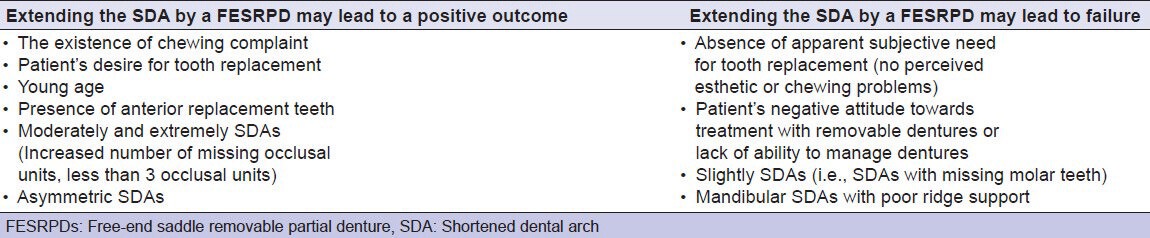
Fueki et al.[56] found that young age, increased number of missing occlusal units, asymmetric dental arch, and the existence of chewing complaint are considered significant predictors for seeking prosthetic restoration in subjects with SDAs. This study illustrated that seeking prosthetic restoration was encountered in 3% of SDA subjects with missing second molar(s), in 58% of SDA subjects with missing first and second molars, and in 93% of SDA subjects with missing premolar(s). The authors concluded that the perceived impairment of chewing ability due to decreased number of occlusal units is a decisive factor for prosthetic restoration of the SDAs. Witter and associates[57] reported that extending the SDA by a fixed or a removable prosthesis depends on the degree of the shortening and the patient's perceived impact on oral health-related quality of life. They stated that there is no evidence to support the prosthetic extension of slightly SDAs (i.e., SDAs with missing molar teeth). Moderately SDAs (i.e., SDAs with missing molar and first premolar teeth) can be extended in exceptional cases, particularly for aesthetic reasons. Extremely SDAs (i.e., SDAs with missing molar and premolar teeth) and asymmetrical extremely SDAs should be prosthetically extended. However, the authors indicated that in such cases, restoration of the SDA should be kept to the level of a moderately SDA, which means that using fixed bridges rather than RPDs may be sufficient to achieve this target. Knezović Zlatarić et al.[58] examined 205 patients with RPDs. 57.4% of the maxillary dentures were class I Kennedy RPDs and 28.8% were class II Kennedy RPDs. In the mandible, 75.2% of the RPDs were class I Kennedy and 17.1% were class II Kennedy. No impact on patients’ evaluation of the quality of their RPDs was related to patient's age, ability of self-supporting lifestyle, social and economic status, marital status, smoking habits, presence of chronic diseases, and the period of use of present RPDs. Also, factors such as Kennedy classification, denture base material, denture base shape, and denture support did not have significant impact on patients’ general satisfaction or comfort of wearing RPDs. However, the outcome of this study revealed that patients with a higher level of education were less satisfied with aesthetics and hygiene of their dentures. Also, less satisfaction with chewing was recorded among males with mandibular RPDs. Furthermore, it was found that greater the number of missing teeth in the mandible, lesser was the oral comfort with the mandibular RPD.
Based on the current evidence, Table 2 outlines some factors that may affect the outcome of extending the SDA by an RPD. This may be of some help for dental clinicians when managing these cases and a guide for treatment decision making.
Table 2.
Factors that may affect the outcome of extending the SDA by an FESRPD
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared
REFERENCES
- 1.Kayser AF. The Shortened Dental Arch: A therapeutic concept in reduced dentitions and certain high-risk groups. Int J Periodontics Restorative Dent. 1989;9:427–49. [PubMed] [Google Scholar]
- 2.Kayser AF. Shortened dental arches and oral function. J Oral Rehabil. 1981;8:457–62. doi: 10.1111/j.1365-2842.1981.tb00519.x. [DOI] [PubMed] [Google Scholar]
- 3.Witter DJ, van Palenstein Helderman WH, Creugers NH, Käyser AF. The shortened dental arch concept and its implications for oral health care. Community Dent Oral Epidemiol. 1999;27:249–58. doi: 10.1111/j.1600-0528.1998.tb02018.x. [DOI] [PubMed] [Google Scholar]
- 4.Armellini D, von Fraunhofer JA. The shortened dental arch: A review of the literature. J Prosthet Dent. 2004;6:531–5. doi: 10.1016/j.prosdent.2004.08.013. [DOI] [PubMed] [Google Scholar]
- 5.Kanno T, Carlsson GE. A review of the shortened dental arch concept focusing on the work by the Kayser/Nijmegen group. J Oral Rehabil. 2006;33:850–62. doi: 10.1111/j.1365-2842.2006.01625.x. [DOI] [PubMed] [Google Scholar]
- 6.Allen PF. Manchester: The University of Manchester; 1993. Aspects of shortened dental arch therapy. [Google Scholar]
- 7.Nassani MZ, Devlin H, McCord JF, Kay EJ. The shortened dental arch--an assessment of patients’ dental health state utility values. Int Dent J. 2005;55:307–12. doi: 10.1111/j.1875-595x.2005.tb00328.x. [DOI] [PubMed] [Google Scholar]
- 8.Nassani MZ, Locker D, Elmesallati AA, Devlin H, Mohammadi TM, Hajizamani A, et al. Dental health state utility values associated with tooth loss in two contrasting cultures. J Oral Rehabil. 2009;36:601–9. doi: 10.1111/j.1365-2842.2009.01975.x. [DOI] [PubMed] [Google Scholar]
- 9.Nassani MZ, Kay EJ. Tooth loss--an assessment of dental health state utility values. Community Dent Oral Epidemiol. 2011;39:53–60. doi: 10.1111/j.1600-0528.2010.00563.x. [DOI] [PubMed] [Google Scholar]
- 10.Kayser AF, Witter DJ, Spanauf AJ. Overtreatment with removable partial denture in shortened dental arches. Aust Dent J. 1987;32:178–82. doi: 10.1111/j.1834-7819.1987.tb01851.x. [DOI] [PubMed] [Google Scholar]
- 11.Allen PF, Witter DJ, Wilson NH, Kayser AF. Shortened dental arch therapy: Views of consultants in restorative dentistry in the United Kingdom. J Oral Rehabil. 1996;23:481–5. doi: 10.1111/j.1365-2842.1996.tb00883.x. [DOI] [PubMed] [Google Scholar]
- 12.Devlin H. Replacement of missing molar teeth-a prosthodontic dilemma. Br Dent J. 1994;176:31–3. doi: 10.1038/sj.bdj.4808354. [DOI] [PubMed] [Google Scholar]
- 13.Nassani MZ, Devlin H, Tarakji B, McCord JF. A survey of dentists’ practice in the restoration of the shortened dental arch. Med Oral Patol Oral Cir Bucal. 2010;15:85–9. doi: 10.4317/medoral.15.e85. [DOI] [PubMed] [Google Scholar]
- 14.Ikebe K, Hazeyama T, Takahashi T, Matsuda KI, Gonda T, Nokubi T. Masticatory performance and prostheses in subjects with shortened dental arches. Nihon Hotetsu Shika Gakkai Zasshi. 2007;51:710–6. doi: 10.2186/jjps.51.710. [DOI] [PubMed] [Google Scholar]
- 15.Picton DC, Wills DJ. Viscoelastic properties of the periodontal ligament and mucosa membrane. Journal Prosthet Dent. 1978;40:263–72. doi: 10.1016/0022-3913(78)90031-8. [DOI] [PubMed] [Google Scholar]
- 16.Ritchie GM. Partial denture design. 2. Lower free-end saddle dentures. Dent Update. 1982;9:429–39. 442. [PubMed] [Google Scholar]
- 17.Ritchie GM. Partial denture design. 3. Maxillary free-end saddle dentures. (496-7).Dent Update. 1982;9:493–4. 499. [PubMed] [Google Scholar]
- 18.Carlsson GE, Hedegard B, Koivumaa KK. Studies in partial dental prosthesis. II. An investigation of mandibular partial dentures with double extension saddles. Acta Odontol Scand. 1961;19:215–37. doi: 10.3109/00016356108997705. [DOI] [PubMed] [Google Scholar]
- 19.Nairn RI. The problem of free-end denture bases. J Prosthet Dent. 1966;16:522–32. doi: 10.1016/0022-3913(66)90056-4. [DOI] [PubMed] [Google Scholar]
- 20.Fish SF. Partial dentures. 6. Free-end saddle dentures. Br Dent J. 1970;128:495–502. doi: 10.1038/sj.bdj.4802486. [DOI] [PubMed] [Google Scholar]
- 21.Ben-Ur Z, Aviv I, Maharshak B. Factors affecting displacement of free-end saddle removable partial dentures. Quintessence Int. 1991;22:23–7. [PubMed] [Google Scholar]
- 22.Neill DJ. The problem of the lower free-end removable partial denture. J Prosthet Dent. 1958;8:623–34. [Google Scholar]
- 23.Anderson JN, Lammie GA. A clinical survey of partial dentures. Br Dent J. 1952;92:59–67. [Google Scholar]
- 24.Anderson JN, Bates JF. The cobalt-chromium partial denture. A clinical survey. Br Dent J. 1959;107:57–62. [Google Scholar]
- 25.Tomlin HR, Osborne J. Cobalt-chromium partial dentures. A clinical survey. Br Dent J. 1961;110:307–10. [Google Scholar]
- 26.Roberts BW. A survey of chrome-cobalt partial dentures. N Z Dent J. 1978;74:203–9. [PubMed] [Google Scholar]
- 27.Wetherell JD, Smales RJ. Partial denture failures: A long-term clinical survey. J Dent. 1980;8:333–40. doi: 10.1016/0300-5712(80)90049-4. [DOI] [PubMed] [Google Scholar]
- 28.Vanzeveren C, D’Hoore W, Bercy P, Leloup G. Treatment with removable partial dentures: A longitudinal study. Part I. J Oral Rehabil. 2003;30:447–58. doi: 10.1046/j.1365-2842.2003.01106.x. [DOI] [PubMed] [Google Scholar]
- 29.Elias AC, Sheiham A. The relationship between satisfaction with mouth and number and position of teeth. J Oral Rehabil. 1998;25:649–61. doi: 10.1046/j.1365-2842.1998.00313.x. [DOI] [PubMed] [Google Scholar]
- 30.Nassani MZ, Devlin H, Tarakji B, McCord JF. Designing cobalt chromium removable partial dentures for patients with shortened dental arches – A pilot survey. J Oral Rehabil. 2011;38:608–14. doi: 10.1111/j.1365-2842.2010.02190.x. [DOI] [PubMed] [Google Scholar]
- 31.Witter DJ, Van Elteren P, Kayser AF, Van Rossum MJ. The effect of removable partial dentures on the oral function in shortened dental arches. J Oral Rehabil. 1989;16:27–33. doi: 10.1111/j.1365-2842.1989.tb01314.x. [DOI] [PubMed] [Google Scholar]
- 32.Witter DJ, Van Elteren P, Kayser AF, Van Rossum GMJM. Oral comfort in shortened dental arches. J Oral Rehabil. 1990;17:137–43. doi: 10.1111/j.1365-2842.1990.tb01402.x. [DOI] [PubMed] [Google Scholar]
- 33.Witter DJ, De Haan AF, Kayser AF, Van Rossum GM. A 6-year follow-up study of oral function in shortened dental arches. Part I: Occlusal stability. J Oral Rehabil. 1994;21:113–25. doi: 10.1111/j.1365-2842.1994.tb01131.x. [DOI] [PubMed] [Google Scholar]
- 34.Witter DJ, De Haan AF, Kayser AF, Van Rossum GM. A 6-year follow-up study of oral function in shortened dental arches. Part II: Craniomandibular dysfunction and oral comfort. J Oral Rehabil. 1994;21:353–66. doi: 10.1111/j.1365-2842.1994.tb01150.x. [DOI] [PubMed] [Google Scholar]
- 35.Witter DJ, Creugers NH, Kreulen CM, De Haan AF. Occlusal stability in shortened dental arches. J Dent Res. 2001;80:432–6. doi: 10.1177/00220345010800020601. [DOI] [PubMed] [Google Scholar]
- 36.Sarita PT, Kreulen CM, Witter DJ, Van’t Hof M, Creugers NH. A study on occlusal stability in shortened dental arches. Int J Prosthodont. 2003;16:375–80. [PubMed] [Google Scholar]
- 37.Walter MH, Weber A, Marré B, Gitt I, Gerss J, Hannak W, et al. The randomized shortened dental arch study: Tooth loss. J Dent Res. 2010;89:818–22. doi: 10.1177/0022034510366817. [DOI] [PubMed] [Google Scholar]
- 38.Walter MH, Hannak W, Kern M, Mundt T, Gernet W, Weber A, et al. The randomized shortened dental arch study: Tooth loss over five years. Clin Oral Investig. 2012 doi: 10.1007/s00784-012-0761-x. [In Press] [DOI] [PubMed] [Google Scholar]
- 39.Leake JL, Hawkins R, Locker D. Social and functional impact of reduced posterior dental units in older adults. J Oral Rehabil. 1994;21:1–10. doi: 10.1111/j.1365-2842.1994.tb01119.x. [DOI] [PubMed] [Google Scholar]
- 40.Jepson NJ, Moynihan PJ, Kelly PJ, Watson GW, Thomason JM. Caries incidence following restoration of shortened lower dental arches in a randomized controlled trial. Br Dent J. 2001;191:140–4. doi: 10.1038/sj.bdj.4801122. [DOI] [PubMed] [Google Scholar]
- 41.Thomason JM, Moynihan PJ, Steen N, Jepson NJ. Time to survival for the restoration of the shortened lower dental arch. J Dent Res. 2007;86:646–50. doi: 10.1177/154405910708600712. [DOI] [PubMed] [Google Scholar]
- 42.Wöstmann B, Budtz-Jørgensen E, Jepson N, Mushimoto E, Palmqvist S, Sofou A, et al. Indications for removable partial dentures: A literature review. Int J Prosthodont. 2005;18:139–45. [PubMed] [Google Scholar]
- 43.Aras K, Hasanreisoğlu U, Shinogaya T. Masticatory performance, maximum occlusal force, and occlusal contact area in patients with bilaterally missing molars and distal extension removable partial dentures. Int J Prosthodont. 2009;22:204–9. [PubMed] [Google Scholar]
- 44.Arce-Tumbay J, Sanchez-Ayala A, Sotto-Maior BS, Senna PM, Campanha NH. Mastication in subjects with extremely shortened dental arches rehabilitated with removable partial dentures. Int J Prosthodont. 2011;24:517–9. [PubMed] [Google Scholar]
- 45.Creugers NH, Witter DJ, Van’t Spijker A, Gerritsen AE, Kreulen CM. Occlusion and temporomandibular function among subjects with mandibular distal extension removable partial dentures. Int J Dent 2010. 2010 doi: 10.1155/2010/807850. 807850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shinogaya T, Toda S. Rehabilitation of occlusal support by removable partial dentures with free-end saddles. Eur J Prosthodont Restor Dent. 2003;11:107–13. [PubMed] [Google Scholar]
- 47.Abt E, Carr AB, Worthington HV. Interventions for replacing missing teeth: Partially absent dentition. Cochrane Database Syst Rev. 2012;2:CD003814. doi: 10.1002/14651858.CD003814.pub2. [DOI] [PubMed] [Google Scholar]
- 48.Jepson NJ, Thomason JM, Steele JG. The influence of denture design on patient acceptance of partial dentures. Br Dent J. 1995;178:296–300. doi: 10.1038/sj.bdj.4808742. [DOI] [PubMed] [Google Scholar]
- 49.Armellini DB, Heydecke G, Witter DJ, Creugers NH. Effect of removable partial dentures on oral health-related quality of life in subjects with shortened dental arches: A 2-center cross-sectional study. Int J Prosthodont. 2008;21:524–30. [PubMed] [Google Scholar]
- 50.Armellini DB, Heydecke G, Witter DJ, Creugers NH. Effects of removable partial dentures on the quality of life in people with shortened dental arches. Ned Tijdschr Tandheelkd. 2009;116:687–93. [PubMed] [Google Scholar]
- 51.Ikebe K, Hazeyama T, Kagawa R, Matsuda K, Maeda Y. Subjective values of different treatments for missing molars in older Japanese. J Oral Rehabil. 2010;37:892–9. doi: 10.1111/j.1365-2842.2010.02123.x. [DOI] [PubMed] [Google Scholar]
- 52.Jepson N, Allen F, Moynihan P, Kelly P, Thomason M. Patient satisfaction following restoration of shortened mandibular dental arches in a randomized controlled trial. Int J Prosthodont. 2003;16:409–14. [PubMed] [Google Scholar]
- 53.Wolfart S, Heydecke G, Luthardt RG, Marré B, Freesmeyer WB, Stark H, et al. Effects of prosthetic treatment for shortened dental arches on oral health-related quality of life, self-reports of pain and jaw disability: Results from the pilot-phase of a randomized multicentre trial. J Oral Rehabil. 2005;32:815–22. doi: 10.1111/j.1365-2842.2005.01522.x. [DOI] [PubMed] [Google Scholar]
- 54.Fueki K, Yoshida E, Igarashi Y. A systematic review of prosthetic restoration in patients with shortened dental arches. Jpn Dent Sci Rev. 2011;47:167–74. [Google Scholar]
- 55.McKenna G, Allen PF, Woods N, O’Mahony D, Damata C, Cronin M, et al. A preliminary report of the cost-effectiveness of tooth replacement strategies for partially dentate elders. Gerodontology. 2012 doi: 10.1111/j.1741-2358.2012.00665.x. doi: 10.1111/j 1741-2358.2012.00665.x. [DOI] [PubMed] [Google Scholar]
- 56.Fueki K, Igarashi Y, Maeda Y, Baba K, Koyano K, Akagawa Y, et al. Factors related to prosthetic restoration in patients with shortened dental arches: A multicentre study. J Oral Rehabil. 2011;38:525–32. doi: 10.1111/j.1365-2842.2010.02183.x. [DOI] [PubMed] [Google Scholar]
- 57.Witter DJ, Hoefnagel RA, Snoek PA, Creugers NH. Extension of (extremely) shortened dental arches by fixed or removable partial dentures. Ned Tijdschr Tandheelkd. 2009;116:609–14. [PubMed] [Google Scholar]
- 58.Knezović Zlatarić D, Celebić A, Valentić-Peruzović M, Jerolimov V, Pandurić J. A survey of treatment outcomes with removable partial dentures. J Oral Rehabil. 2003;30:847–54. doi: 10.1046/j.1365-2842.2003.01039.x. [DOI] [PubMed] [Google Scholar]


