Abstract
Dental management of children with attention-deficit hyperactivity disorder (ADHD) often requires the need for pharmacological behavior management techniques such as the use of sedation. The purpose of this article is to describe a clinical case involving accidental aspiration of an Endodontic instrument during root canal therapy under sedation. To our knowledge, this is the first case report of aspiration of an Endodontic instrument and should serve to heighten the awareness with regard to aspiration during dental procedures under sedation. It also emphasizes the need for proper isolation techniques in patients treated under sedation, thereby preventing such complications.
Keywords: Attention-deficit hyperactivity disorder, aspiration, bronchoscopy, conscious sedation, endodontic instrument, rubber dam
INTRODUCTION
The second most common reason for foreign body aspiration in the lung is from a dental procedure.[1] Any object routinely placed into or removed from the oral cavity during a dental or a surgical procedure can be aspirated or even ingested.[2] The risk is higher in elderly adults and in children who are under sedation, because of the diminished protective reflexes.[1,2]
Pharmacological methods of behavior management such as the use of sedatives have been used in Pediatric dentistry to reduce fear and anxiety. Often, children younger than six years of age and those with developmental delay require deep levels of sedation to gain control over their behavior.[3] Pediatric dentists who are treating children under sedation must be aware that sedation represents a continuum and the patient may move easily from a level of sedation to a deeper level, which may result in the loss of the patient's protective reflexes.[4,5] Hence, practitioners intending to produce a given level of sedation must be able to diagnose and manage the physiological consequences in patients whose level of sedation becomes deeper than initially intended. With an increase in the level of sedation the patient is placed in a more favorable situation for aspiration. Such cases remain a real threat to the pediatric dentist, due to the challenges involved in treating young children and the difficulty in airway management.
Attention-deficit hyperactivity disorder (ADHD) is the most common neurobehavioral disorder in childhood. The core symptoms of ADHD include inattention, hyperactivity, and impulsivity.[6] Prevalence in the population has been reported to range from 1.7 to 17.8%.[7] Behavioral manifestations of the disorder frequently impair the patient's ability to perform home care adequately, making them more prone to trauma.[8] Those children who occasionally fail to cooperate with the basic behavior management techniques may require advanced management techniques, such as the use of protective stabilization, sedation, and general anesthesia.
The purpose of this case report is to describe the aspiration of an Endodontic instrument in an eight-year-old child during root canal treatment, under conscious sedation. It also throws lights on how a prompt and accurate diagnosis, with immediate treatment, aided in preventing serious complications. The article emphasizes the need for proper isolation techniques to be followed in treating children who are under sedation.
CASE REPORT
An eight-year-old, male child, who was diagnosed as a case of Attention Deficient Hyperactive Disorder (ADHD) was treated in a private dental hospital for a fractured right central incisor (tooth 11). Considering the history of previous dental treatment that had failed and with further discussion with the child's pediatrician, it was decided that the best treatment option for the patient was to provide dental treatment using sedation. In the next dental visit the child was given a combination of Chloral hydrate 25 mg/kg, Hydroxyzine 1 mg/kg, and Meperidine 1 mg/kg for sedation. The patient was placed in a supine position and physically immobilized using a Papoose Board (Olympic Medical Corp, Seattle, Wash) before treatment was initiated. A mouth prop was inserted and access opening done in tooth 11, followed by placement of the calcium hydroxide intracanal medicament (Calcicure, Voco, Germany). During the next visit, the child was sedated using the same combination. As the patient exhibited slight discomfort with the placement of the rubber dam, the procedure was carried out without isolation. During the biomechanical preparation, the patient suddenly moved his head, due to which an endodontic instrument (Pro Taper hand file, Dentsply) slipped from the dentist's hand and the patient swallowed it. The procedure was stopped immediately and measures were taken to retrieve the file from the posterior region of oral cavity. The initial assessment by the dentist revealed that the patient was choking and had cough with no obvious signs of respiratory distress. The operator made a provisional diagnosis of foreign body aspiration.
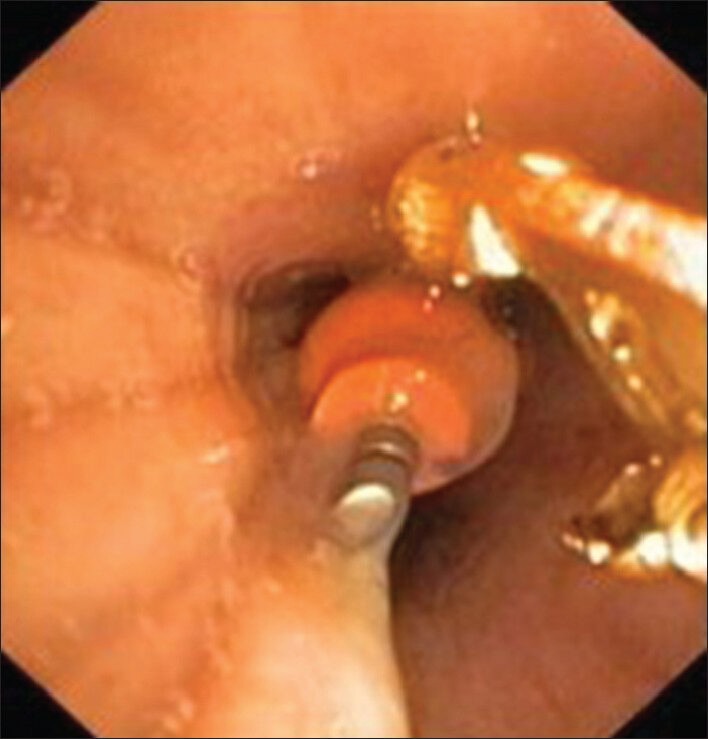
The patient was immediately admitted to the Emergency Room for evaluation. A posteroanterior radiograph of the chest demonstrated the presence of a sharp foreign body at the level of the T4 vertebral body [Figure 1]. A diagnostic Computed Tomography scan (CT) was taken, which showed the endodontic instrument impacted on the left main bronchi [Figure 2]. Bronchoscopy done under General Anesthesia revealed that the endodontic instrument had pierced the mucosal folds tangentially, and was embedded in the wall of the left bronchial mucosa, buried up to the handle [Figure 3]. Using a bronchoscopic grasper, the handle of the endodontic instrument was grasped, gently pulling it out of the mucosal fold [Figure 4]. The site of penetration of the mucosa was inspected for bleeding and perforation. The endodontic instrument was then retrieved along with the withdrawal of the bronchoscope, under full visualization throughout the retrieval process. The patient was subsequently discharged with no complaints of discomfort on follow-up.
Figure 1.
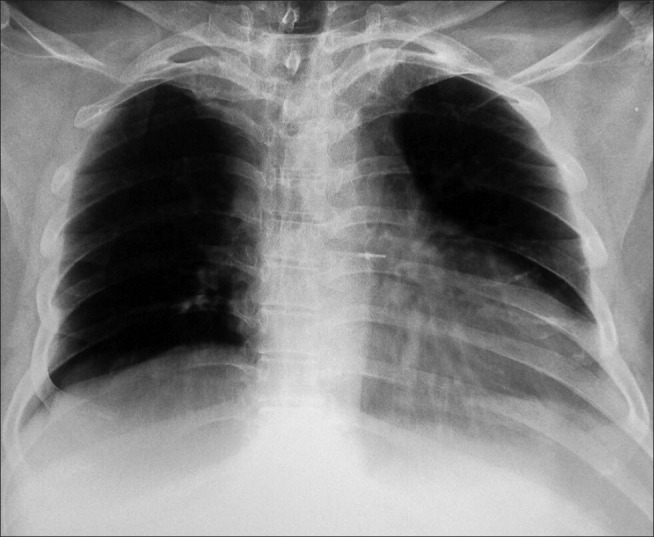
Lateral chest view with the impacted endodontic file lodged at the T4 level
Figure 2.
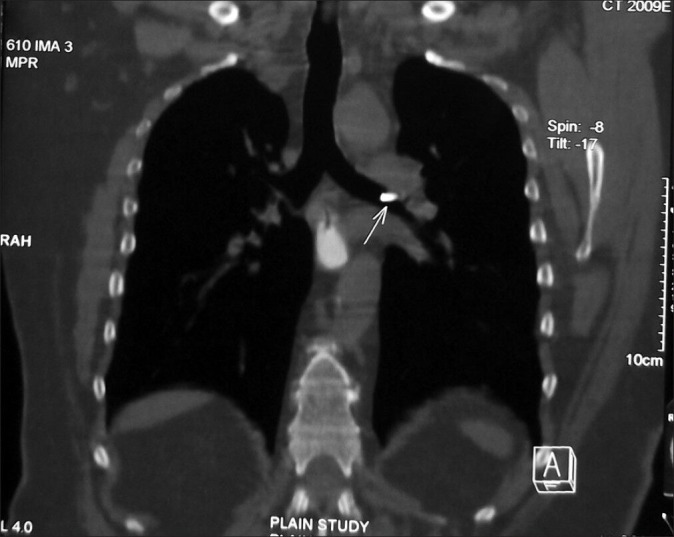
Diagnostic CT image showing the endodontic file in the left main bronchus
Figure 3.

Bronchoscopy image of the file embedded in the wall of the left bronchial mucosa
Figure 4.
Photograph of the bronchus showing the bronchoscope grasper engaging the endodontic file during retrieval
DISCUSSION
Children who exhibit various behavior management problems are commonly treated by advanced management techniques. Attention-deficit hyperactivity disorder is considered to be the most common neurobehavioral disorder among school-aged children.[6,7] Dental management of children who exhibit disruptive behavior may necessitate administration of sedation or general anesthesia. A combination of Chloral hydrate, Hydroxyzine, and Meperidine is the most commonly used agent for sedation in these children. This combination provides effective sedation, with quick recovery, and few side effects.[9]
For the endodontic instruments, the reported incidence of aspiration was 0.001 per 100 000 root canal treatments and the incidence of ingestion was 0.12 per 100 000 root canal treatments.[10] Entry of a foreign body to the respiratory tract is potentially life-threatening and requires prompt management. When aspirated foreign bodies are not diagnosed and treated early they can lead to serious complications.[11] Although these events occur infrequently, the potential morbidity associated with a single incident is too high to ignore. This is especially true from the standpoint of the amount of medical care that is needed to manage these incidents, the high financial cost to the dentist, and the potential for malpractice litigation.[12]
Aspirations are more likely to occur when treating a population of young patients, who lack cooperative behavior associated with physical, medical, and mental disabilities.[13] These patients are more commonly treated under pharmacological behavior management techniques, which predispose them to a high risk of aspiration due to their altered state of consciousness. When treating these children under sedation, the pediatric dentists should be aware of the degree of sedation attained by the drug and the significance of the drug interactions, which may potentiate the level of sedation.
In recognition of the expanding need for both the elective and emergency use of sedative agents in delivering painless treatment to children, the guidelines for the use of sedative agents and proper isolation techniques that are to be followed are considered important. Although a literature review has few case reports on the aspiration of a foreign body in children under sedation, there are no previous studies investigating the prevalence of such aspirations and the use of isolation techniques in patients treated under sedation.[2,13,14,15]
In case of aspiration, a radiographic examination and localization of the foreign body forms the first line of management. A radiographic examination helps to detect the presence/absence of the foreign body. Computerized tomography (CT) has an added advantage over conventional radiographs in localization of the foreign body. A CT scan is helpful in visualizing the radiopaque foreign bodies and the alveolar collapse. It can also demonstrate airway foreign bodies that are radiolucent on plain radiographs. CT scans can depict a foreign body within the lumen of the tracheobronchial tree, as also the three-dimensional position of the foreign body. Once an aspirated foreign body is detected by radiological studies, or if the clinical suspicion is high, the patient should undergo bronchoscopy to confirm the diagnosis and to remove the foreign body. If the object can be removed during bronchoscopy, further invasive procedures may be avoided. A bronchoscope provides a safe retrieval, affords good control of the airway, provides good visualization, and allows manipulation of foreign bodies with a wide variety of forceps.[16] The present article reports the first case of an Endodontic protaper file impacted in the left bronchial mucosa, which had been retrieved uneventfully.
Patients undergoing sedation should be treated with proper isolation techniques to avoid the risk of aspiration. The easiest and most common procedure to prevent any such complications is the use of the rubber dam.[17] Although this particular case was treated with a rubber dam in the initial setting, the rubber dam was removed due to reported discomfort by the patient. With decreasing level of cooperation, the rubber dam placement becomes difficult to place. No informed consent, verbal or written, can exonerate the non-use of rubber dam, under any circumstances.[18] An alternative is to place a 4 × 4 inch gauze protective barrier in the oral cavity, distal to the area where small items are being manipulated.[19] The limited use of the rubber dam always implies a serious risk on the quality of Endodontic treatment. This case highlights the need for proper isolation techniques in patients who are treated under sedation, which is yet to be completely implemented.
Patient positioning during dental treatment also acts as an important risk factor for aspiration. In the treatment of upper molars and incisors, the patients are generally forced to lie in a horizontal supine position, which may make it easier for dental objects or instruments to tumble across the dorsum of the tongue into the pharynx.[20]
CONCLUSION
Over the years, professionals in the field of dentistry have worked hard to prevent and minimize adverse events in the work environment through education and training of the dental personnel. Accidents still happen, however, it is essential that clinicians and their staff remain calm, so as to make prompt decisions and take appropriate actions that will not only prevent potentially serious complications, but may ultimately save their patient's lives. Emphasizing the importance of proper isolation techniques helps to prevent most of the complications.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared
REFERENCES
- 1.Tiwana KK, Morton T, Tiwana PS. Aspiration and ingestion in dental practice: A 10-year institutional review. J Am Dent Assoc. 2004;135:1287–91. doi: 10.14219/jada.archive.2004.0404. [DOI] [PubMed] [Google Scholar]
- 2.Leith R, Fleming P, Redahan S, Doherty P. Aspiration of an avulsed primary incisor: A case report. Dent Traumatol. 2008;24:e24–6. doi: 10.1111/j.1600-9657.2008.00593.x. [DOI] [PubMed] [Google Scholar]
- 3.American Academy on Pediatrics; American Academy on Pediatric Dentistry. Guideline for monitoring and management of pediatric patients during and after sedation for diagnostic and therapeutic procedures. Pediatr Dent. 2008-2009;30:143–59. [PubMed] [Google Scholar]
- 4.Holroyd I. Conscious sedation in pediatric dentistry. A short review of the current UK guidelines and the technique of inhalational sedation with nitrous oxide. Paediatr Anaesth. 2008;18:13–7. doi: 10.1111/j.1460-9592.2007.02387.x. [DOI] [PubMed] [Google Scholar]
- 5.American Academy on Pediatric Dentistry Ad Hoc Committee on Sedation and Anesthesia; American Academy on Pediatric Dentistry Council on Clinical Affairs. Policy on the use of deep sedation and general anesthesia in the pediatric dental office. Pediatr Dent. 2008-2009;30:66–7. [PubMed] [Google Scholar]
- 6.Clinical practice guideline: Diagnosis and evaluation of the child with attention-deficit/hyperactivity disorder. American Academy of Pediatrics. Pediatrics. 2000;105:1158–70. doi: 10.1542/peds.105.5.1158. [DOI] [PubMed] [Google Scholar]
- 7.Bimstein E, Wilson J, Guelmann M, Primosch R. Oral characteristics of children with attention-deficit hyperactivity disorder. Spec Care Dentist. 2008;28:107–10. doi: 10.1111/j.1754-4505.2008.00021.x. [DOI] [PubMed] [Google Scholar]
- 8.Katz-Sagi H, Redlich M, Brinsky-Rapoport T, Matot I, Ram D. Increased dental trauma in children with attention deficit hyperactivity disorder treated with methylphenidate--a pilot study. J Clin Pediatr Dent. 2010;34:287–9. doi: 10.17796/jcpd.34.4.p6714ln2g658322u. [DOI] [PubMed] [Google Scholar]
- 9.Chowdhury J, Vargas KG. Comparison of chloral hydrate, meperidine, and hydroxyzine to midazolam regimens for oral sedation of pediatric dental patients. Pediatr Dent. 2005;27:191–7. [PubMed] [Google Scholar]
- 10.Susini G, Pommel L, Camps J. Accidental ingestion and aspiration of root canal instruments and other dental foreign bodies in a French population. Int Endod J. 2007;40:585–9. doi: 10.1111/j.1365-2591.2007.01249.x. [DOI] [PubMed] [Google Scholar]
- 11.Kuo SC, Chen YL. Accidental swallowing of an Endodontic file. Int Endod J. 2008;41:617–22. doi: 10.1111/j.1365-2591.2008.01392.x. [DOI] [PubMed] [Google Scholar]
- 12.Seals ML, Andry JM, Kellar PN. Pulmonary aspiration of a metal casting: Report of case. J Am Dent Assoc. 1988;117:587–8. doi: 10.14219/jada.archive.1988.0050. [DOI] [PubMed] [Google Scholar]
- 13.Adewumi A, Kays DW. Stainless steel crown aspiration during sedation in pediatric dentistry. Pediatr Dent. 2008;30:59–62. [PubMed] [Google Scholar]
- 14.Holan G, Ram D. Aspiration of an avulsed primary incisor. A case report. Int J Paediatr Dent. 2000;10:150–2. doi: 10.1046/j.1365-263x.2000.00185.x. [DOI] [PubMed] [Google Scholar]
- 15.Ulku R, Baskan Z, Yavuz I. Open surgical approach for a tooth aspirated during dental extraction: A case report. Aust Dent J. 2005;50:49–50. doi: 10.1111/j.1834-7819.2005.tb00085.x. [DOI] [PubMed] [Google Scholar]
- 16.Oguzkaya F, Akcali Y, Kahraman C, Bilgin M, Sahin A. Tracheobronchial foreign body aspirations in childhood: A 10-years experience. Eur J Cardiothorac Surg. 1998;14:388–92. doi: 10.1016/s1010-7940(98)00205-x. [DOI] [PubMed] [Google Scholar]
- 17.Lynch CD, McConnell RJ. Attitudes and use of rubber dam by Irish general dental practitioners. Int Endod J. 2007;40:427–32. doi: 10.1111/j.1365-2591.2007.01212.x. [DOI] [PubMed] [Google Scholar]
- 18.Selbst AG. Understanding informed consent and its relationship to the incidence of adverse treatment events in conventional endodontic therapy. J Endod. 1990;16:387–90. doi: 10.1016/S0099-2399(06)81911-4. [DOI] [PubMed] [Google Scholar]
- 19.Cameron SM, Whitlock WL, Tabor MS. Foreign body aspiration in dentistry: A review. J Am Dent Assoc. 1996;127:1224–9. doi: 10.14219/jada.archive.1996.0415. [DOI] [PubMed] [Google Scholar]
- 20.Obinata K, Satoh T, Towfik AM, Nakamura M. An investigation of accidental ingestion during dental procedures. J Oral Sci. 2011;53:495–500. doi: 10.2334/josnusd.53.495. [DOI] [PubMed] [Google Scholar]


