Abstract
Background Depressive disorders are highly prevalent, have a detrimental impact on the quality of life of patients and their relatives and are associated with increased mortality rates, high levels of service use and substantial economic costs. Current treatments are estimated to only reduce about one-third of the disease burden of depressive disorders. Prevention may be an alternative strategy to further reduce the disease burden of depression.
Methods We conducted a meta-analysis of randomized controlled trials examining the effects of preventive interventions in participants with no diagnosed depression at baseline on the incidence of diagnosed depressive disorders at follow-up. We identified 32 studies that met our inclusion criteria.
Results We found that the relative risk of developing a depressive disorder was incidence rate ratio = 0.79 (95% confidence interval: 0.69–0.91), indicating a 21% decrease in incidence in prevention groups in comparison with control groups. Heterogeneity was low (I2 = 24%). The number needed to treat (NNT) to prevent one new case of depressive disorder was 20. Sensitivity analyses revealed no differences between type of prevention (e.g. selective, indicated or universal) nor between type of intervention (e.g. cognitive behavioural therapy, interpersonal psychotherapy or other). However, data on NNT did show differences.
Conclusions Prevention of depression seems feasible and may, in addition to treatment, be an effective way to delay or prevent the onset of depressive disorders. Preventing or delaying these disorders may contribute to the further reduction of the disease burden and the economic costs associated with depressive disorders.
Keywords: Prevention, depression, RCT
Introduction
About 150 million people worldwide are affected with depression at any moment in time, and one in every five women and 1 in every eight men experience an episode of major depression over the course of their life.1–3
Depression is a major factor in quality of life decrements and is also associated with premature death.4 People suffering from depressive disorders experience substantial loss in quality of life.5 Between 1990 and 2010, major depression moved up from 15th to 11th in terms of global disease burden measured in disability-adjusted life years (DALYs)6 and it is projected to become the single leading cause of disease burden by 2030.7 Depressive disorders are associated with high levels of service use and economic costs stemming from productivity losses.8 Although effective treatments are available, it has been estimated that, even under optimal conditions, contemporary treatments can reduce only about one-third of the disease burden associated with major depressive disorder (MDD).9,10
A way to further reduce the disease burden of major depression could be to reduce the influx of new cases that is, to reduce the incidence. This is done by prevention rather than treatment. Strengthening protective factors (e.g. social, cognitive or problem-solving skills) or alleviating prodromal disease stages (e.g. reducing severity of depressive symptoms) have been investigated in a considerable number of preventive studies.11–13 Several studies examining the effects of preventive interventions have found favourable effects on the incidence of new cases,14–20 but several others did not.21–24 Whether the effect of the currently available preventive interventions decays over time, indicating effectiveness only when a person is participating in the preventive intervention, is being investigated.
There are different types of prevention. Universal prevention focuses on the general public or a whole population group regardless of risk status. Selective prevention targets individuals or subgroups that are at higher risk of developing mental disorders than average individuals or subgroups. Indicated prevention focuses on individuals who are identified as having prodromal symptoms or biological markers to mental disorders, but who do not yet meet the diagnostic criteria for a full-blown diagnosis.25,26 In a previous meta-analysis of studies examining the effects of preventive interventions on the incidence of new cases, we found an overall effect of universal, selective and indicated prevention on the incidence of depressive disorders.13 Universal prevention was only examined in two studies and it was therefore impossible to investigate effectiveness.21,27 The studies included in that meta-analysis were conducted among various populations and the interventions differed considerably, which might have influenced the results.
One way to examine whether preventive interventions are effective is to look at the numbers needed to treat (NNT). The NNT indicates the number of people who would have to receive a preventive intervention in order to prevent one new case of depression. This leads to the expectation that NNT is inversely related to the a priori risk of the disorder (i.e. lower NNTs in indicated prevention).
In our earlier meta-analysis we could include 19 trials examining the effects of preventive interventions, whereas we identified 32 studies for the current meta-analysis, using even more stringent criteria for inclusion. It was therefore deemed opportune to update the earlier meta-analysis, thus allowing us to not only estimate the overall effects of preventive interventions with greater precision, but also to examine characteristics of the interventions and participants as moderators of outcome. In addition, the large number of included studies allows us to examine subfields of prevention in more detail and with greater statistical power, such as prevention of postpartum depression, prevention at schools and prevention of depression in people with somatic illnesses. Also, we focus on whether the effect of type of intervention decays over time, thereby investigating if type of intervention works as a protection or inoculation against new onsets of MDD.
Methods
Search strategies and selection of studies
We conducted a comprehensive search of the literature in bibliographical databases. All relevant articles published between 1966 and March 2012 were included.
The searches of these databases were done by combining terms indicative of prevention and depression. We specified the search for both MeSH terms and free-text words, but limiting the search to effectiveness studies (e.g. randomized trials, controlled trials, clinical trials). The full search string for PubMed is reported in Supplementary Appendix A, available as Supplementary Data at IJE online. Furthermore, we examined the references of relevant previous meta-analyses and reviews (see Supplementary Appendix B, available as Supplementary Data at IJE online) and we reviewed the reference lists of retrieved articles.
Studies were included when they used a pretest-posttest randomized controlled design and examined the effects of a preventive, psychological intervention on the incidence of new cases of depressive disorders compared with a control group.
Prevention was defined as reducing the incidence of new cases of MDD. Therefore we selected studies where participants did not meet the diagnostic criteria (according to the DSM-III-R or DSM-IV) at baseline and were ‘at risk’ of becoming depressed at follow-up—as assessed with a diagnostic instrument. We also included studies examining universal, selective and indicated prevention.28 Studies focusing on preventing depressive disorders after a specific live event (e.g. postnatal depression) were also included.
A study was excluded when the participants were receiving a treatment for another mental disorder. Also studies on maintenance treatment or relapse prevention were excluded.
Quality assessment
We used four basic criteria of the ‘risk of bias’ tool to assess possible sources of bias29: sequence generation (the method used to generate the allocation sequence is described in sufficient detail to allow an assessment of whether it should produce comparable groups); allocation concealment (the method used to conceal allocation is described in sufficient detail to see whether intervention allocations were foreseeable in advance of, or during enrolment); blinding of outcome assessors (all measures used to blind personnel as well as study participants to knowledge of which intervention participants were allocated); and incomplete outcome data (methods described whether all randomized participants were used in the analyses). The quality assessment was conducted independently by two reviewers (P.C. and K.v.Z.). Disagreements were solved by consensus.
Analyses
We used the Comprehensive Meta-Analysis Software package, version 2.2.021 (Biostat, Englewood, NJ) for all analyses. First we calculated the incidence rate ratio (IRR) for developing a depressive disorder in the intervention compared with the control group for each study. Then we calculated the pooled mean of the IRRs. We investigated both the fixed and the random-effects model.29 The random-effects model assumes that the included studies are drawn from ‘populations’ of studies that may differ from each other and we feel this is more appropriate to the current study. The effect sizes resulting from included studies are allowed to differ under this model, not only because of the sample error of each study, but also due to true (systematic) variation across studies.
We also calculated the NNT. This indicates how many people would have to receive a preventive intervention in order to prevent one new case of depression. The NNT was calculated as the inverse of the pooled absolute risk difference.
As a test of homogeneity of effect sizes, we calculated the I2-statistic, which is an indicator of heterogeneity. The I2-statistic30 can be expressed as a percentage, where a value of 0% indicates no heterogeneity, and 25%, 50% and 75% can be interpreted as low, moderate and high levels of heterogeneity.31 We calculated 95% confidence intervals (CIs) around I2, using the non-central chi-square-based approach within the heterogeneity command in Stata.32 We also calculated the Q-statistic and tested the level of significance.
Subgroup and meta-regression analyses were conducted according to the procedures implemented in the Comprehensive-Meta-Analysis software. We used mixed-effects analyses, which pooled studies within subgroups with the random-effects model but tested for differences between subgroup with the fixed-effects model.
Publication bias was tested by inspecting the funnel plot on the primary outcome measure and by Duval and Tweedie’s trim-and-fill procedure33 which yields an estimate of the effect size after the publication bias has been taken into account (again, as implemented in the Comprehensive Meta-Analysis program). Also, we performed Egger’s test.
Results
Searches and inclusion of studies
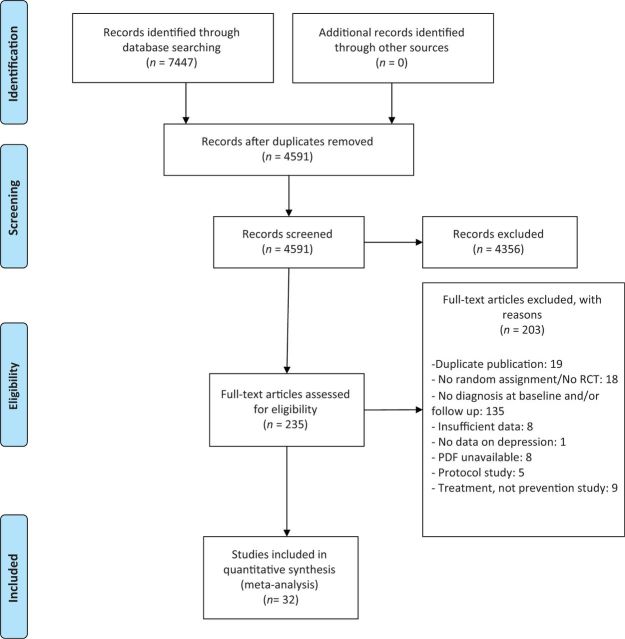
The literature search resulted in a total of 7447 articles found in PubMed (n = 2006), Cochrane Central Register of Controlled Trials (n = 2707), PsychInfo (n = 932) and EMBASE (n = 1802). We removed duplicates, leaving 4591 articles to be examined. We retrieved a total of 235 full-text articles that potentially met our inclusion criteria. Of these, 203 were excluded. Most (n = 135) were excluded because they lacked a diagnosis at the baseline and/or the follow up. Another reason for not including studies was lack of randomization (n = 18). All reasons for exclusion are noted in Figure 1. Control groups primarily consisted of care as usual, with some exceptions such as: placebo pill, booklet or no intervention (Table 1).
Figure 1.
Flow chart of included studies
Table 1.
Selected characteristics of studies examining the effects of interventions on the incidence of new cases of depressive disorders
| Study | Type | Recruitment | Target population | Inclusion criteria | Prevented disorder | Conditions | n | Intervention | FU (mn) | Drop-out (%) | ITT |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Allart et al. 200734 | Ind | Community | Adults | BDI ≥10; no current MDD | MDD | 1. CBT | 61 | 12 CBT group sessions | 12 | 25 | Yes |
| 2. CAU | 41 | ||||||||||
| Arnarson & Craighead 200915 | Ind | Screening at schools | Adolescents | CDI, CASQ ≥; no current DD | MDD | 1. Eclectic | 81 | 14 eclectic group sessions | 12 | 34 | No |
| 2. CAU | 90 | ||||||||||
| Austin et al. 200824 | Sel | Antenatal clinics | Antenatal women | EPDS > 10; ANRQ > 23; hx of DD | Anxiety and PMDD | 1. CBT | 191 | 6 CBT group sessions + 1 booster | 4 | 52 | Yes |
| 2. Booklet | 86 | ||||||||||
| Bot et al. 201035 | Ind | outpatient clinics | People with diabetes | ≥ 55 years; ≥ 16 CES-D | MDD | 1. Stepped care | 58 | 12 weeks | 24 | 36 | No |
| 2. CAU | 56 | ||||||||||
| Brugha et al. 200036 | Sel | Screening | Primiparous women | Risk factor for depression | MDE | 1. CBT | 94 | 6 CBT + PST support group sessions | 3 | 9 | Yes |
| 2. CAU | 96 | ||||||||||
| Clarke et al. 199537 | Ind | schools | Adolescents (15_16 years) | CES-D > 24;no current MDD/DYS | MDD + Dysthymia | 1. CBT | 55 | 15 CBT group sessions | 12 | 27 | No |
| 2. CAU | 70 | ||||||||||
| Clarke et al. 200114 | Ind | HMO | Adolescents (13–18 years) | CES-D > 24; ≥1 DSM-IV | MDD + Dysthymia | 1. CBT | 43 | 15 CBT group sessions | 24 | 17 | Yes |
| 2. CAU | 47 | ||||||||||
| Compas et al. 200938 | Sel | Mental health clinics | Adolescents (9_15 years) | CESD/K-SADS-PL | MDE | 1. CBT | 56 | 12 sessions, four families each group | 24 | 22 | Yes |
| 2. Written info | 53 | ||||||||||
| De Jonge et al. 200940 | Ind | Hospital | Patients with physical illness | CES-D, MINI | MDD | 1. Nurse-led | 47 | Counsel or psychotherapy or case conference | 12 | 33 | Yes |
| 2. CAU | 53 | ||||||||||
| Elliott et al. 200016 | Sel | Screening | Pregnant women | Vulnerable (LQ) | PMDD | 1. PE | 47 | 11 PE sessions + mutual support | 3 | 15 | No |
| 2. CAU | 53 | ||||||||||
| Garber et al. 200917 | Ind | Universities and health centres | Adolescent (13–17) of parents with depression | CESD > 20 and/or 2 mn remission from MDD or both | MDD | 1. CBT | 159 | 8 CBT group sessions + 6 continuation sessions | 9 | 9 | Yes |
| 2. CAU | 157 | ||||||||||
| Garcia et al. 201041 | Sel | Primary care | Primary care patients | 18-65 yrs; SPPI no DSM-IV Axis | Somatoform disorders | 1. Psycho- educational | 52 | Five 120-min group sessions by family doctor | 60 | 21 | No |
| 2. No intervent. | 52 | ||||||||||
| Gillham et al. 200618 | Ind | Through HMO | Early adolescents (11–12 years) | CDI ≥ 7/9; no current MDD DYS | MDD, DYS | 1. CBT | 147 | 12 CBT group sessions | 24 | 41 | Yes |
| 2. CAU | 124 | ||||||||||
| Hagan et al. 200423 | Sel | Neonatal unit | Mothers very preterm babies | No current DD | Postpartum depression | 1. CBT | 101 | 6 CBT group sessions + PE | 12 | 12 | Yes |
| 2. CAU | 98 | ||||||||||
| Joling et al. 201242 | Sel | Memory clinics, general practices, home care settings | Caregivers dementia patients | MINI | depressive or anxiety disorder | 1. Family meetings | 96 | 6 in-person counselling meetings once every 2 to 3 months | 12 | 26 | Yes |
| 2. CAU | 96 | ||||||||||
| Konnert et al. 200943 | Ind | Residents of nursing homes | Nursing home residents (over 60 years) | No MDE, GDS ≥ 9 | MDD | 1. CBT | 20 | 13 CBT sessions | 6 | 33 | No |
| 2. CAU | 23 | ||||||||||
| Lara et al. 200944 | Ind | Hospital, clinic and community health care centre | Pregnant women in Mexico | CES-D ≥ 16 and/or self-report hx of MDD | MDD | 1. CBT | 250 | 8 PE group sessions | 4-9 | 64 | Yes |
| 2. CAU | 127 | ||||||||||
| Martinovic et al. 200645 | Sel | Community + clinic | Adolescents (13–19) with epilepsy | sD; no current DD | MDD | 1. CBT | 15 | 12 CBT group sessions | 9 | 6 | Yes |
| 2. CAU | 15 | ||||||||||
| Muñoz et al. 199546 | Sel | General practice records | GP patients | No MDD in past 6 mn | MDD, dysthymia | 1. CBT | 72 | 8 CBT group sessions (CWD) | 12 | 8 | No |
| 2. CAU | 78 | ||||||||||
| Muñoz et al. 200747 | Ind | Screening | Pregnant Latina women | CES-D ≥ 16; past history of MDD | PMDD | 1. CBT | 21 | 12 CBT group sessions (CWD) | 12 | 9 | No |
| 2. CAU | 20 | ||||||||||
| Robinson et al. 200848 | Sel | Community, universities & hospitals | Post-stroke patients | No current DD, HAM-D < 11; SCID | Poststroke depression | 1. PST | 59 | 6 PST session + 6 booster sessions | 12 | 9 | Yes |
| 2. Placebo | 58 | ||||||||||
| Rovner et al. 200749 | Sel | Screening in outpatient centres | Older patients | No current DD; SADS | MDD or minor depression | 1. PST | 95 | 6 individual PST sessions | 6 | 13 | Nes |
| 2. CAU | 99 | ||||||||||
| Seligman et al. 199950 | Sel | All new students | Undergraduate students | ASQ = bottom quartile, no current MDD | MDD | 1. CBT | 106 | 8 CBT group sessions | 36 | 4 | No |
| 2. CAU | 119 | ||||||||||
| Sheffield et al. 200627 | Uni/Ind | School | All students of 36 schools | High-symptom students, no MDD/DYS | MDD, dysthymia | 1. CBT-Uni | 107 | 8 CBT + 1 PST group lessons | 18 | 15 | No |
| 2. CBT-Ind | 100 | ||||||||||
| 3.CBT-Ind | 110 | ||||||||||
| 4. CAU | 125 | ||||||||||
| Spence et al. 200321 | Uni | School | Students of 18 high schools | ADIS-C | Major depression | 1. CBT | 751 | 8 grp lessons of CBT + ouPST | 12 | 15 | No |
| 2. CAU | 749 | ||||||||||
| Van ‘t Veer-Tazelaar et al. 200951 | Ind | PIKO project | Older adults in primary care | No MDE;CES-D ≥16 | MDD/ anxiety | 1. CBT + PST | 86 | 3 months CBT + nurse calls/visits, then 7 PST sessions | 24 | 24 | Yes |
| 2. CAU | 84 | ||||||||||
| Willemse et al. 200453 | Ind | General practice | Adults (18–65 years) | One MDD core symptom, no MDD in past 6 mn (CIDI) | MDD, dysthymia | 1. CBT | 107 | 1 face-to-face contact + self-help book + 6 short phone consultations (CWD) | 12 | 37 | Yes |
| 2. CAU | 109 | ||||||||||
| Young et al. 200619 | Ind | School | Adolescents (15–16 years) | CES-D ≥ 16; 2 symptoms; no MDD/DYS | MDD, dysthymia (K-SADS) | 1. IPT | 27 | 2 individual + 8 IPT group sessions | 6 | 2 | Yes |
| 2. CAU | 14 | ||||||||||
| Young et al. 201055 | Ind | Two-stage screening | Adolescents (13–17 years) | CES-D 16 – 39; K-SADS-PI | MDD | 1. IPT-AST | 36 | 1. 2 pre-group sessions + 8 90-min group sessions | 18 | 23 | Yes |
| 2. SC | 21 | 2. 30-45 min individual counselling | |||||||||
| Zlotnick et al. 200156 | Sel | Hospitals | Pregnant women | ≥1 risk indicators PDD, no MDD | PMDD | 1. IPT | 17 | 4 IPT group sessions | 3 | 5 | Yes |
| 2. CAU | 18 | ||||||||||
| Zlotnick et al. 200620 | Sel | Hospitals | Pregnant women | High score risk survey, no current MDD | PMDD (LIFE) | 1. IPT | 17 | 4 IPT group sessions | 3 | 13 | No |
| 2. CAU | 46 | ||||||||||
| Zlotnick et al. 201157 | Sel | Primary care clinics + private OBGYN clinic | Pregnant women (18–40 years) | EPDS/SCID | MDD/PMDD | 1. IPT | 28 | 4 IPT + booster session | 3 | 15 | Yes |
| 2. CAU | 26 |
ADIS-C, Anxiety disorders interview schedule children; ANRQ, Antenatal Risk Questionnaire; BDI, Beck Depression Inventory, (C) ASQ, (Children’s) Attributional Style Questionnaire; CAU, care as usual; CBT, cognitive behavioural therapy; CDI, Children’s Depression Inventory; CES-D = Centre for Epidemiological Studies-Depression Scale; CWD, Coping with depression; DAS, Dysfunctional Attitude Scale; DD, depressive disorder, DYS, dysthymia; EPDS, Edinburgh Postnatal Depression Scale; GDS, Geriatric Depression Scale; HAM-D, Hamilton rating scale Depression; HMO = Health Maintenance Program; IND, Indicated; IPT, Interpersonal therapy; K/SADS/PL, Kiddie-Sads-Present and Lifetime Version; LQ, Leverton Questionnaire; MDD, major depressive disorder; MDE, major depressive episode; MINI = Mini-International Neuropsychiatric Interview; mn, months; OBGYN, Obstetrics and gynaecology; PIKO = Prevention Intervention for Frail Elderly; PMDD, postpartum depression; PST, problem solving therapy; SADS, Schedule for Affective Disorders and Schizophrenia; SCID, Structured Clinical Interview for DSM-IV; sD = subthreshold depression; SEL, selective; SPPI = Standardized Polyvalent Psychiatric Interview; VAS, Visual Analogue Scale; Uni, universal.
Characteristics of included studies
A total of 32 studies with 6214 participants (3312 in the prevention groups and 2902 in the control groups) met all inclusion criteria.14–21,23,24,27,35–57 In one study three different intervention groups were examined27 so we were able to include 34 comparisons between preventive interventions and control groups. Table 1 shows selected characteristics of the included studies. Sheffield et al. (2006) investigated an universal preventive intervention and two indicated preventive interventions. One other study examined universal prevention, whereas indicated prevention and selected prevention were each investigated by 15 other studies.
The majority of studies (21) focused on preventing MDD, 9 studies aimed at postpartum depression (PMDD) and 4 dealt with mood mixed disorder (e.g. a combination of MDD, dysthymia and/or minor depression). These were diagnosed by diagnostic instruments, such as the Structured Clinical Interview for DSM-IV (SCID) (Table 1), which use DSM-III-R or DSM-IV criteria. Most studies did not inform whether they excluded or included participants with a history of depressive disorders (n = 20). Four studies reported using participants with first episode of depression. Eight studies reported including participants with a history of depression, however participants did not experience a depressive disorder at the time of the baseline measure. Eight studies focused on adults in general, 1 study focused on adults with diabetes, 6 studies on pregnant women and 3 studies on (new) mothers, but most studies focused on adolescents or students (n = 14). Fifteen interventions were based on the principle of cognitive behavioural therapy. Some studies based their intervention on other psychological approaches, such as problem-solving therapy (n = 2) or interpersonal group therapy (n = 5). The number of sessions ranged from 4 to 15. Most studies used interventions which consisted of 12 sessions (n = 7), 2 studies used preventive interventions which consisted of 4 sessions and 2 studies used preventive interventions consisting of 15 sessions.
Eleven studies were conducted in Europe, 14 in the USA and 9 elsewhere. The follow-up periods of these studies varied between 2 and 60 months (median = 9 months). Only one study reported a follow-up of 5 years34 and one study reported a follow-up of 36 months.35 One study24 reported a follow-up period of 2 months and 8 studies reported a follow-up period of 3 months. Most studies, however, also reported a follow-up period of 6 or 12 months (n = 28). Drop-out rates in the studies varied between 2% and 64%. Intention-to-treat-analyses were done by most studies (n = 19).
Quality of the articles was relatively high. Quality of studies was assessed on four criteria: allocation concealment, incomplete outcome data, blinding of outcome assessors, and sequence generation. Sixteen studies reported that blinding of the allocation of interventions was done adequately. Eight studies met all four criteria, 18 studies met two or three criteria and six studies met no or only one criterion.
Overall incidence rate ratios
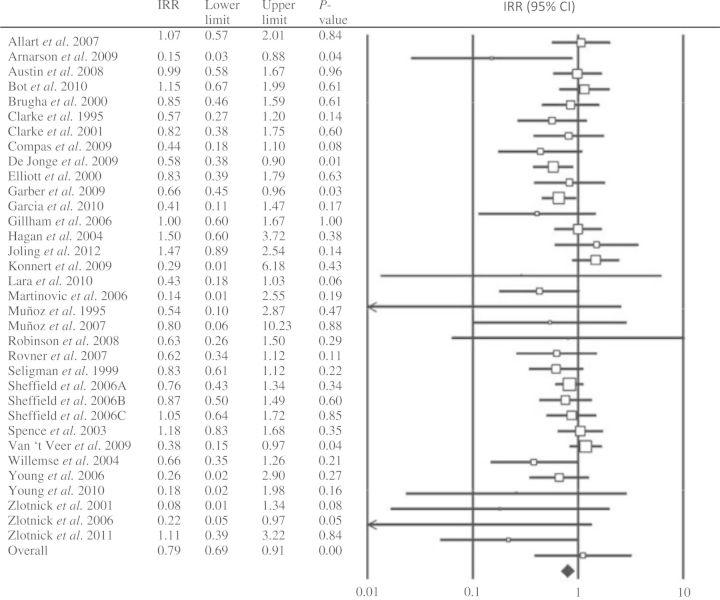
We calculated the mean IRR by combining the IRRs at different follow-up times into a single estimate. When looking at the fixed-effects model, the IRR for all 34 comparisons from the 32 studies was 0.82 [95% confidence interval (CI) = 0.73–0.91; P = 0.000]. Focusing on the random-effects model, the IRR for all 34 comparisons from the 32 studies was 0.79 (95% CI = 0.69–0.91; P = 0.001). Heterogeneity was low (I2 = 24%). Because the differences between the fixed- and the random-effects models were small, we only report the results for the random-effects model (Table 2 and Figure 2).
Table 2.
Meta-Analyses of studies examining the effects of preventive interventions on the incidence of depressive disorders: Incidence rate ratios, heterogeneity and numbers needed to treat (NNT) at 2 months to 5 years
| N | IRR | 95% CI | I2 | 95% CI | P | NNT | 95% CI | P | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Depressive disorders | 34 | 0.79 | 0.69–0.91 | 24 | 0–50 | 20 | 13–37 | |||
| Sheffield excluded | 31 | 0.77 | 0.66–0.90 | 29 | 0–54 | 16 | 11–30 | |||
| At first follow up | 34 | 0.79 | 0.69–0.92 | 29 | 0–54 | 21 | 14–45 | |||
| At last follow up | 34 | 0.78 | 0.68–0.89 | 29 | 0–53 | 17 | 12–30 | |||
| Follow up Period | <5 months | 11 | 0.81 | 0.55–1.18 | 29 | 0–65 | 15 | 8–77 | ||
| 6 months | 6 | 0.51 | 0.30–0.86 | 41 | 0–76 | 15 | 5–14 | |||
| 7–12 months | 12 | 0.82 | 0.66–1.01 | 37 | 0–68 | 25 | 14–100 | |||
| >13 months | 5 | 0.89 | 0.66–1.21 | 0 | 0–79 | 24 | 9–34 | |||
| Subgroup analyses | ||||||||||
| Type of therapy | CBT | 19 | 0.86 | 0.76–0.98 | 0 | 0–49 | 0.106 | 71 | 33–500 | 0.003 |
| IPT | 5 | 0.36 | 0.13–0.96 | 32 | 0–74 | 7 | 4–20 | |||
| Other | 10 | 0.68 | 0.49–0.95 | 52 | 1–77 | 12 | 7–37 | |||
| Age | Students | 14 | 0.81 | 0.67–0.97 | 25 | 0–60 | 0.231 | 22 | 13–71 | 0.419 |
| Adults | 16 | 0.84 | 0.66–1.01 | 30 | 0–62 | 22 | 11–333 | |||
| Elderly | 4 | 0.55 | 0.36–0.85 | 0 | 0–85 | 11 | 7–32 | |||
| Target groupa | School-based | 14 | 0.81 | 0.68–0.97 | 25 | 0–22 | 0.586 | 21 | 12–71 | 0.759 |
| Perinatal depression | 9 | 0.81 | 0.59–1.11 | 22 | 0–63 | 20 | 10–71 | |||
| General Medical | 10 | 0.69 | 0.54–0.89 | 0 | 0–62 | 15 | 9–42 | |||
| Other | 1 | |||||||||
| Prevention typea | IND | 17 | 0.74 | 0.61–0.90 | 14 | 0–51 | 0.507 | 13 | 9–26 | 0.284 |
| SEL | 15 | 0.81 | 0.65–1.01 | 26 | 0–60 | 21 | 12–91 | |||
| UNI | 2 | |||||||||
| Number of sessionsa | 1–7 | 10 | 0.81 | 0.61–1.07 | 51 | 0–76 | 0.775 | 20 | 11–125 | 0.159 |
| 8–11 | 11 | 0.85 | 0.68–1.07 | 0 | 0–60 | 42 | 18–143 | |||
| ≥12 | 12 | 0.75 | 0.58–0.97 | 9 | 0–48 | 14 | 9–31 | |||
| nr | 1 | |||||||||
| Publication country | USA | 14 | 0.67 | 0.54–0.82 | 0 | 0–55 | 0.051 | 13 | 9–25 | 0.002 |
| Europe | 11 | 0.77 | 0.57–1.04 | 47 | 0–73 | 16 | 9–91 | |||
| Other | 9 | 0.94 | 0.79–1.10 | 0 | 0–65 | 143 | 36–71 | |||
| Quality score | <3 | 12 | 0.79 | 0.59–1.06 | 53 | 10–76 | 0.894 | 14 | 7.87–71 | 0.234 |
| 3 or 4 | 22 | 0.77 | 0.67–0.90 | 0 | 0–46 | 29 | 19–71 | |||
Abbreviations: CBT, cognitive behavioral therapy; IND, indicated prevention; IPT, Interpersonal therapy; IRR, incidence rate ratio; I2, heterogeneity; MDD, major depressive disorder; N, number of studies; NNT, numbers needed to treat; NR, not reported; PMDD, postpartum major depressive disorder; SEL, selective prevention; UNI, universal prevention.
aWhen subgroup included less than 3 studies analysis was done without that subgroup.
Figure 2.
The effects of preventive interventions on the incidence of depressive disorders; incidence rate ratios and numbers needed to treat. Lines represent IRR and 95% CI; the size of the square indicates the weight of each study
There was one study27 that compared three interventions with one control group. Since these comparisons were not independent from each other, we examined whether removal of these comparisons would increase heterogeneity. The overall analyses of 32 studies resulted in a mean IRR of 0.77 (95% CI: 0.66–0.90, P = 0.005), with low heterogeneity (I2 = 29%). This was comparable to the mean IRR found in the total sample.
Since the IRR could differ at varying follow-up periods, we conducted several sensitivity analyses. We examined the IRR for each follow-up period separately (<5 months; 6 months, 7–12 months, ≥13 months; Table 2). We also conducted a separate analysis in which we used only the last follow-up period reported in each study (0.78; 95% CI: 0.68–0.89; P = 0.001; I2 = 29), and another analysis with only the first follow-up period of each study (0.79; 95% CI: 0.69–0.92; P = 0.002; I2 = 29). As can be seen in Table 2, we found few indications that the outcomes differed very much from the IRR in which all follow-up periods were pooled.
We also conducted meta-regression analyses to see whether there was any effect decay over time. First, we examined the association between IRR and the first follow-up period reported in the study. We did not find an association between IRR and first follow-up period (the point estimate of the slope was 0.003; 95% CI: −0.007 to 0.013), although there was a trend (P = 0.06) suggesting that the effects of the interventions are lower at longer follow-up periods (median: 7.5 months; range: 2–60 months). In the second meta-regression analysis we used the last follow-up period reported in the studies. Again, these results did not show an association between IRR and last-follow-up occasion (P = 0.06; the point estimate of the slope was −0.000; 95% CI: −0.01 to 0.01), suggesting that the longer it takes before the last follow-up period, the lower the incidence of depression is (median = 12; range = 3–60 months).
Inspection of the funnel plot (Supplementary Appendix C, available as Supplementary data at IJE online) and Duval and Tweedie’s trim-and-fill procedure attested to the possible presence of publication bias. After adjustment for publication bias, the effect size was increased from 0.82 to 0.86 (95% CI: 0.74–1.00; number of trimmed studies: 10). The Egger’s test also indicated an asymmetric funnel plot [intercept: −1.24, 95% CI: −1.95 to −0.53, degree of freedom (df) 32, P = 0.001]. The fail-safe n was 175, indicating that 175 studies with an effect size of 0 would have to be included to not find a publication bias.
Subgroup analyses
We conducted a series of subgroup analyses (Table 2). We examined whether the IRR differed according to type of prevention (indicated, universal or selective), type of intervention (CBT, IPT or other), age group (adolescent, adults or elderly), number of sessions (1–7, 8–11, ≥12; one study did not report the number of intervention sessions), country of publication (USA, EU or other), and target group (school-based, general medical, perinatal or other).
The IRR did not differ in any of the subgroups (Table 2). The difference between CBT and IPT interventions, found by Cuijpers et al. in 2008, could not be replicated in the current meta-analyses. This null finding might be caused by the low number of studies using IPT as an intervention (n = 5).
However, when looking at NNT, as indicated in Table 2, there was a difference between number needed to treat of CBT (NNT = 71), IPT (NNT = 7) and other (NNT = 12) interventions (P = 0.003), suggesting that preventive interventions using IPT are more effective than preventive interventions using CBT.
In most subgroup analyses the heterogeneity was low to moderate. No heterogeneity was found in several subgroups of studies: subgroups using CBT, those focusing on the elderly and those using a target population of general medical patients.42 Also, no heterogeneity was found in subgroups having 8–11 sessions, having a publication score of 3 or 4 or from studies not published in Europe.
Discussion
We examined whether preventive interventions are effective in reducing the incidence of MDD. Results showed that preventive interventions lowered the incidence of depression by 21%, compared with controls. This is in agreement with the results of the previous meta-analyses conducted by Cuijpers et al. in 2008. A reduction in incidence of 21% can be considered clinically relevant. In the current meta-analysis we only included studies that used diagnostic criteria at baseline and follow-up, to exclude cases of depression at baseline and assess diagnostic status at follow-up. Using these rigorous criteria and the relatively large number of trials, this meta-analysis offers more robust evidence on the impact of preventive interventions on the incidence of new depressions than any previous meta-analysis.
The current meta-analyses did not show IPT to be more effective than CBT. This is in contrast to the findings of our earlier meta-analyses. Examining the NNT, however, shows that IPT (NNT = 7) is more effective than CBT (NNT = 71). Furthermore, there is no overlap in the 95% confidence intervals, reinforcing our suggestion that IPT might have a greater prophylactic effect than CBT. This result is consistent with our results from the previous meta-analysis conducted in 2008. It should, however, be interpreted with caution, since the number of studies using IPT (5) was considerably lower than the studies using CBT (20). If IPT is indeed more effective, this might be related to the fact that this type of intervention focuses more directly on the current problems and high-risk situations. This might be exactly what people in high-risk situations or with subthreshold symptoms need.
Also, results did not suggest that indicated prevention (IRR = 0.74) was more effective than selective prevention (IRR = 0.81). However, only two studies investigated universal prevention and those were therefore excluded from analysis.
This does not necessarily imply that universal intervention might not be effective in high-risk subgroups. Rose58 proposed that there are two strategies to prevention: a population strategy of prevention, which targets a whole population regardless of individual differences in risk status; and an individual strategy of prevention, which targets individuals at high risk for an adverse health outcome.59 Our meta-analysis is mainly focused on individual prevention. If we used less rigorous inclusion criteria (e.g. no diagnostic instrument to determine whether participants have a diagnosis) we might find results similar to another meta-analysis conducted in 2012.60 This analysis found a beneficial effect in the prevention of postpartum depression in a range of interventions, individually based as well as multiple contacts. This shows that population-based strategies for prevention are interesting from a public health point of view and have the potential of reducing the incidence of depression considerably. However, our study also makes clear that there are no studies yet that show that population-based strategies actually reduce the incidence of depressive disorders.
Although prevention of depression seems to be effective, the NNT appears high (20 in the overall analysis), which is comparable to the NNT in the earlier analyses by Cuijpers (NNT = 22). There are, however, no normative thresholds for lower or higher NNT.13 Considering the impact depressive disorders have on social, economic and physical life and the clinical relevance, it seems an acceptable number. As discussed earlier, universal prevention might have a very different approach and yield very different results compared with selective and indicated prevention. Also, there were only two studies using universal prevention in this analysis. Therefore, it might be a consideration to not include universal prevention in other reviews like the current review. Other research did not show that the implemented intervention reduced the depressive symptoms in adolescents at high risk. The intervention was implemented in everyday life situations. The sample consisted of non-referred adolescents from the community. This study was, however, not included in the current meta-analysis because the researchers did not use a diagnostic instrument to diagnose depressive disorders at follow-up.61 However, the study shows that it is important to investigate the risk factors for depression, which could be due to premorbid vulnerability or due to the experience of previous episodes of depression. Future research should take history of depression into account.
Furthermore, the control/comparison groups in the included studies consisted mostly of treatments like care-as-usual or waiting-list. These are passive rather than active forms of ‘treatments’. There is, therefore, no control for face-to-face time and attention. These are, however, nonspecific aspects of structured interventions like IPT or CBT. If future research included more active comparators, it would greatly improve the strength with which conclusions can be drawn about the specific prophylactic value of learning-based psychotherapies.
Most follow-up periods were between 6 and 12 months (28); only 2 studies had follow-up periods beyond 2 years. Therefore, it is not clear whether preventive interventions actually prevented the incidence of depression or simply delayed the onset of depressive episodes. We performed analyses per follow-up (<5, 6, 7–12, ≥13 months). Comparing the effects of preventive interventions and first follow-up months showed a small positive association, indicating that the more months pass, the more effective the preventive intervention is. However, comparing the effects of preventive interventions and last follow-up period, this had a very small negative association. This might indicate that the effects of the preventive intervention became smaller over longer follow-up periods, uggesting that the preventive interventions delay the onset of disorders rather than preventing them altogether. However, only few studies had longer follow-up periods than 2 years. From a clinical point of view, preventing new onsets of depression would obviously be preferable since it would completely avoid the burden of disease in all prevented cases. However, delaying the onset is also important. Every year a disorder is delayed is a year without suffering.
We acknowledge several limitations of this study. First, several studies examined different populations and used different types of interventions. That said, according to the I2 statistic, heterogeneity was low to moderate, indicating that it may be a fairly homogeneous set of studies. Second, the follow-up periods differed between studies. We therefore examined the various follow-up periods. However, we also conducted regression analysis with only the first follow-up occasion and regression analysis with only the last follow-up occasion to see whether there was any effect of decay over time. Third, the numbers of studies in some of the subgroup-analyses were rather small and show only correlations. Therefore results should be interpreted with caution.
In conclusion, it is encouraging that we found positive effects of preventive interventions on the incidence of major depression, which are clinically relevant. Prevention of depressive disorders is possible, and may, in addition to treatment, be an important way to further reduce the burden of disease due to a very prevalent and disabling condition: depression.
Supplementary Data
Supplementary data is available at IJE online.
Funding
C.R. received funding from NIHM centre grant P30 MH90333 for his activity.
Conflict of interest: None declared.
KEY MESSAGES:
Depressive disorders are highly prevalent and current treatments are estimated to reduce about one-third of the disease burden.
Current research shows that prevention of depression seems feasible and might be an effective way to delay or prevent the onset of depressive disorder, thereby reducing the disease burden of depression.
A meta-analysis was conducted of randomized controlled trials examining the effects of preventive, psychological interventions in participants with no diagnosed depression at baseline on the incidence of diagnosed depressive disorders at follow-up.
However, many studies did not report whether the depression of participants was first-onset or a recurrent episode. Also, several studies examined different populations, used different types of interventions and had different follow-up periods.
Supplementary Material
References
- 1.Kessler RC, McGonagle KA, Zhao S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Arch Gen Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. [DOI] [PubMed] [Google Scholar]
- 2.Wang PS, Aguilar-Gaxiola S, Alonso J, et al. Worldwide use of mental health services for anxiety, mood, and substance disorders: results from 17 countries in the WHO world mental health (WMH) surveys. Lancet. 2007;370:841–50. doi: 10.1016/S0140-6736(07)61414-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.O'Kearney R, Kang K, Christensen H, Griffiths KA. Controlled trial of a school-based Internet program for reducing depressive symptoms in adolescent girls. Depress Anxiety. 2009;26:65–72. doi: 10.1002/da.20507. [DOI] [PubMed] [Google Scholar]
- 4.Cuijpers P, Smit F. Excess mortality in depression: a meta-analysis of community studies. J Affect Disord. 2002;72:227–36. doi: 10.1016/s0165-0327(01)00413-x. [DOI] [PubMed] [Google Scholar]
- 5.De Graaf R, Bijl RV, Ravelli A, Smit F, Vollebergh WA. Predictors of first incidence of DSM-III-R psychiatric disorders in the general population: findings from the Netherlands Mental Health Survey and Incidence Study. Acta Psychiatr Scand. 2002;106:303–13. doi: 10.1034/j.1600-0447.2002.01397.x. [DOI] [PubMed] [Google Scholar]
- 6.Murray CJL, Vos T, Lozano R, et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2197–223. doi: 10.1016/S0140-6736(12)61689-4. [DOI] [PubMed] [Google Scholar]
- 7.Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442. doi: 10.1371/journal.pmed.0030442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smit F, Cuijpers P, Oostenbrink J, Batelaan N, de Graaf R, Beekman A. Excess costs of common mental disorders: population based cohort study. J Ment Health Policy Econ. 2006;9:193–200. [PubMed] [Google Scholar]
- 9.Andrews G, Wilkinson DD. The prevention of mental disorders in young people. Med J Aust. 2002;177:S97–S100. doi: 10.5694/j.1326-5377.2002.tb04865.x. [DOI] [PubMed] [Google Scholar]
- 10.Chisholm D, Sanderson K, Ayuso-Mateos JL, Saxena S. Reducing the global burden of depression population-level analysis of intervention cost-effectiveness in 14 world regions. Br J Psychiatry. 2004;184:393–403. doi: 10.1192/bjp.184.5.393. [DOI] [PubMed] [Google Scholar]
- 11.Petersen I, Bhana A, Swartz L. Mental health promotion and the prevention of mental disorders in South Africa. Afr J Psychiatry. 2012;15:411–16. doi: 10.4314/ajpsy.v15i6.50. [DOI] [PubMed] [Google Scholar]
- 12.Cuijpers P, van Straten A, Smit F. Preventing the incidence of new cases of mental disorders: a meta-analytic review. J Nerv Ment Disord. 2005;193:119–25. doi: 10.1097/01.nmd.0000152810.76190.a6. [DOI] [PubMed] [Google Scholar]
- 13.Cuijpers P, van Straten A, Smit F, Mihalopoulos C, Beekman ATF. Preventing the onset of depressive disorders: a meta-analytic review of psychological interventions. Am J Psychiatry. 2008;165:1272–80. doi: 10.1176/appi.ajp.2008.07091422. [DOI] [PubMed] [Google Scholar]
- 14.Clarke GN, Hornbrook M, Lynch F, et al. A randomized trial of a group cognitive intervention for preventing depression in adolescent offspring of depressed parents. Arch Gen Psychiatry. 2001;58:1127–34. doi: 10.1001/archpsyc.58.12.1127. [DOI] [PubMed] [Google Scholar]
- 15.Arnarson EO, Craighead WE. Prevention of depression among icelandic adolescents. Behav Res Ther. 2009;47:577–85. doi: 10.1016/j.brat.2009.03.011. [DOI] [PubMed] [Google Scholar]
- 16.Elliott SA, Leverton TJ, Sanjack M, et al. Promoting mental health after childbirth: a controlled trial of primary prevention of postnatal depression. Br J Clin Psychol. 2000;39:223–41. doi: 10.1348/014466500163248. [DOI] [PubMed] [Google Scholar]
- 17.Garber J, Clarke GN, Weersing VR, et al. Prevention of depression in at-risk adolescents. A randomized controlled trial. JAMA. 2009;301:2215–24. doi: 10.1001/jama.2009.788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gillham JE, Hamilton J, Freres DR, Patton K, Gallop R. Preventing depression among early adolescents in the primary care setting: a randomized controlled study of the penn resiliency program. J Abnorm Child Psychol. 2006;34:203–19. doi: 10.1007/s10802-005-9014-7. [DOI] [PubMed] [Google Scholar]
- 19.Young JF, Mufson L, Davies M. Efficacy of interpersonal psychotherapy-adolescent skills training: an indicated preventive intervention for depression. J Child Psychiatry. 2006;47:1254–62. doi: 10.1111/j.1469-7610.2006.01667.x. [DOI] [PubMed] [Google Scholar]
- 20.Zlotnick C, Miller IW, Pearlstein T, Howard M, Sweeney P. A preventive intervention for pregnant women on public assistance at risk for postpartum depression. Am J Psychiatry. 2006;163:1443–45. doi: 10.1176/appi.ajp.163.8.1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Spence SH, Sheffield JK, Donovan CL. Preventing adolescent depression: An evaluation of the problem solving for life program. J Consult Clin Psychol. 2003;71:3–13. doi: 10.1037//0022-006x.71.1.3. [DOI] [PubMed] [Google Scholar]
- 22.Priest SR, Henderson J, Evans SF, Hagan R. Stress debriefing after childbirth: a randomized controlled trial. Med J Aust. 2003;178:542–45. doi: 10.5694/j.1326-5377.2003.tb05355.x. [DOI] [PubMed] [Google Scholar]
- 23.Hagan R, Evans SF, Pope S. Preventing postnatal depression in mothers of very preterm infants: a randomized controlled trial. BJOG. 2004;111:641–47. doi: 10.1111/j.1471-0528.2004.00165.x. [DOI] [PubMed] [Google Scholar]
- 24.Austin MP, Frilingos M, Lumley J, et al. Brief antenatal cognitive behaviour therapy group intervention for the prevention of postnatal depression and anxiety: A randomized controlled trial. J Affect Disord. 2008;105:35–44. doi: 10.1016/j.jad.2007.04.001. [DOI] [PubMed] [Google Scholar]
- 25.Munoz RF, Cuijpers P, Smit F, Barrera AZ, Leykin Y. Prevention of Major Depression. Annu Rev Clin Psychol. 2010;6:181–212. doi: 10.1146/annurev-clinpsy-033109-132040. [DOI] [PubMed] [Google Scholar]
- 26.Greenberg MT, Domitrovich C, Bumbarger B. Preventing Mental Disorders in School-Age Children: A Review of the Effectiveness of Prevention Programs. University Park, PA: Prevention Research Center for the Promotion of Human Development, Pennsylvania State University; 2000. [Google Scholar]
- 27.Sheffield JK, Spence SH, Rapee RM, et al. Evaluation of universal, indicated, and combined cognitive-behavioral approaches to the prevention of depression among adolescents. J Consult Clin Psychol. 2006;74:66–79. doi: 10.1037/0022-006X.74.1.66. [DOI] [PubMed] [Google Scholar]
- 28.Mrazek PJ, Haggerty RJ. Reducing Risks for Mental Disorders: Frontiers for Preventive Intervention Research. Washington, DC: National Academies Press; 1994. [PubMed] [Google Scholar]
- 29.Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1.0. www.cochrane-handbook.org (10 November 2012, date last accessed) [Google Scholar]
- 30.Ionnadis JPA, Patsopoulos NA, Evangelou E. Uncertainty in heterogeneity estimates in meta-analyses. BMJ. 2007;335:914–16. doi: 10.1136/bmj.39343.408449.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–60. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Orsini N, Higgins J, Bottai M, Buchan I. Heterogi: Stata Module to Quantify Heterogeneity in a Meta-Analysis, Revised 25 January 2006. Boston, MA: Boston College Department of Economics; 2005. http://EconPapers.repec.org/RePEc:boc:bocode:s449201 (10 November 2012, date last accessed) [Google Scholar]
- 33.Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56:455–63. doi: 10.1111/j.0006-341x.2000.00455.x. [DOI] [PubMed] [Google Scholar]
- 34.Allart-van Dam E, Hosman CMH, Hoogduin CAL, Schaap CPDR. Prevention of depression in subclinically depressed adults: Follow-up effects on the ‘Coping with Depression’ course. J Affect Disord. 2007;97:219–28. doi: 10.1016/j.jad.2006.06.020. [DOI] [PubMed] [Google Scholar]
- 35.Bot M, Pouwer F, Ormel J, Slaets JPJ, de Jonge P. Education and psychological aspects: Predictors of incident major depression in diabetic outpatients with subthreshold depression. Diabetic Med. 2010;27:1295–1301. doi: 10.1111/j.1464-5491.2010.03119.x. [DOI] [PubMed] [Google Scholar]
- 36.Brugha TS, Wheatley S, Taub NA, et al. Pragmatic randomized trial of antenatal intervention to prevent post-natal depression by reducing psychosocial risk factors. Psychol Med. 2000;30:1273–81. doi: 10.1017/s0033291799002937. [DOI] [PubMed] [Google Scholar]
- 37.Clarke GN, Hawkins W, Murphy M, Sheeber LB, Lewinsohn PM, Seeley JR. Targeted prevention of unipolar depressive disorder in an at-risk sample of high school adolescents: A randomized trial of a group cognitive intervention. J Am Acad Child Adolesc Psychiatry. 1995;34:312–21. doi: 10.1097/00004583-199503000-00016. [DOI] [PubMed] [Google Scholar]
- 38.Compas BE, Forehand R, Keller G, et al. Randomized controlled trial of a family cognitive-behavioral preventive intervention for children of depressed parents. J Consult Clin Psych. 2009;77:1007–20. doi: 10.1037/a0016930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Compas BE, Forehand R, Thigpen JC, et al. Family group cognitive-behavioral preventive intervention for families of depressed parents: 18- and 24-month outcomes. J Consult Clin Psych. 2011;79:488–99. doi: 10.1037/a0024254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.De Jonge P, Bel Hadj F, Boffa D, et al. Prevention of major depression in complex medically ill patients: preliminary results from a randomized, controlled trial. Psychosomatics. 2009;50:227–33. doi: 10.1176/appi.psy.50.3.227. [DOI] [PubMed] [Google Scholar]
- 41.Garcia-Campayo J, Arevalo E, Claraco LM, Alda M, Lopez del Hoyo Y. A prevention programme for somatoform disorders is effective for affective disorders. J Affect Disord. 2010;122:124–32. doi: 10.1016/j.jad.2009.06.031. [DOI] [PubMed] [Google Scholar]
- 42.Joling KJ, Van Marwijk HWJ, Smit F, et al. Does a family meetings intervention prevent depression and anxiety in family caregivers of dementia patients? A randomized trial. PLoS One. 2012;7:e30936. doi: 10.1371/journal.pone.0030936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Konnert C, Dobson K, Stelmach L. The prevention of depression in nursing home residents: A randomized clinical trial or cognitive-behavioral therapy. Aging Ment Health. 2009;13:288–99. doi: 10.1080/13607860802380672. [DOI] [PubMed] [Google Scholar]
- 44.Lara MA, Navarro C, Navarrete L. Outcome results of a psycho-educational intervention in pregnancy to prevent PPD: a randomized control trial. J Affect Disord. 2009;122:109–17. doi: 10.1016/j.jad.2009.06.024. [DOI] [PubMed] [Google Scholar]
- 45.Martinovic Z, Simonovic P, Djokic R. Preventing depression in adolescents with epilepsy. Epilepsy Behav. 2006;9:619–24. doi: 10.1016/j.yebeh.2006.08.017. [DOI] [PubMed] [Google Scholar]
- 46.Munoz RF, Ying YW, Bernal G, et al. Prevention of depression with primary care patients: A randomized controlled trial. Am J Community Psychol. 1995;23:199–222. doi: 10.1007/BF02506936. [DOI] [PubMed] [Google Scholar]
- 47.Munoz RF, Le HN, Ippen CG, et al. Prevention of postpartum depression in low-income women: development of the mamas y bebes/mothers and babies course. Cogn Behav Pract. 2007;14:70–83. [Google Scholar]
- 48.Robinson RG, Jorge RE, Moser DJ, et al. Escitalopram and problem-solving therapy for prevention of poststroke depression: A randomized controlled trial. JAMA. 2008;299:2391–400. doi: 10.1001/jama.299.20.2391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rovner BW, Casten RJ, Hegel MT, Leiby BE, Tasman WS. Preventing depression in age-related macular degeneration. Arch Gen Psychiatry. 2007;64:886–92. doi: 10.1001/archpsyc.64.8.886. [DOI] [PubMed] [Google Scholar]
- 50.Seligman MEP, Schulman P, DeRubeis RJ, Hollon SD. The prevention of depression and anxiety. Prev Treat. 1999;2:1–24. [Google Scholar]
- 51.Van‘t Veer PJ, Van Marwijk HWJ, Van Oppen P, et al. Stepped-care prevention of anxiety and depression in late life. Arch Gen Psychiatry. 2009;66:297–304. doi: 10.1001/archgenpsychiatry.2008.555. [DOI] [PubMed] [Google Scholar]
- 52.Van‘t Veer PJ, Van Marwijk HWJ, Van Oppen P, et al. Prevention of late-life anxiety and depression has sustained effects over 24 months: A pragmatic randomized trial. Am J Geriatr Psychiatry. 2011;19:230–39. doi: 10.1097/jgp.0b013e3181faee4d. [DOI] [PubMed] [Google Scholar]
- 53.Willemse GRWM, Smit F, Cuijpers P, Tiemens BG. Minimal-contact psychotherapy for sub-threshold depression in primary care. Br J Psychiatry. 2004;185:416–21. doi: 10.1192/bjp.185.5.416. [DOI] [PubMed] [Google Scholar]
- 54.Young JF, Gallop R, Mufson L. Mother-child conflict and its moderating effects on depression outcomes in a preventive intervention for adolescent depression. J Clin Child Adolesc. 2009;38:696–704. doi: 10.1080/15374410903103577. [DOI] [PubMed] [Google Scholar]
- 55.Young JF, Mufson L, Gallop R. Preventing depression: a randomized trial of interpersonal psychotherapy-adolescent skill training. Depress Anxiety. 2010;27:426–33. doi: 10.1002/da.20664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zlotnick C, Johnson SL, Miller IW, Pearlstein T, Howard M. Postpartum depression in women receiving public assistance: pilot study of an interpersonal-therapy-oriented group intervention. Am J Psychiatry. 2001;158:638–40. doi: 10.1176/appi.ajp.158.4.638. [DOI] [PubMed] [Google Scholar]
- 57.Zlotnick C, Capezza NM, Parker D. An interpersonally based intervention for low-income pregnant women with intimate partner violence: a pilot study. Arch Womens Men Health. 2011;14:55–65. doi: 10.1007/s00737-010-0195-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rose G. Sick individuals and sick populations. Int J Epidemiol. 1985;14:32–38. doi: 10.1093/ije/14.1.32. Reprinted Int J Epidemiol 2001;30:427–32. [DOI] [PubMed] [Google Scholar]
- 59.McLaren L, McIntyre L, Kirkpatrick S. Rose’s population strategy of prevention need not increase social inequalities in health. Int J Epidemiol. 2010;39:372–77. doi: 10.1093/ije/dyp315. [DOI] [PubMed] [Google Scholar]
- 60.Dennis CL, Dowswell T. Psychosocial and psychological interventions for preventing postpartum depression. Cochrane Database Syst Rev. 2013;2:CD001134. doi: 10.1002/14651858.CD001134.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Stallard P, Sayal K, Phillips R, et al. Classroom based cognitive behavioural therapy in reducing symptoms of depression in high risk adolescents: pragmatic cluster randomised controlled trial. BMJ. 2012;345:e6058. doi: 10.1136/bmj.e6058. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.