Abstract
Background
Although there is evidence that promoting individual cessation aids increases their utilization, mass media campaigns highlighting the benefit of using help to quit have not been evaluated.
Purpose
To analyze the effects of a Philadelphia adult smoking–cessation media campaign targeting using help in ad taglines from March–November 2012. This study distinctively analyzed the campaign’s impact at both the population level (effects on the average person) and the individual level (effects among those who reported exposure).
Methods
The 16-month mass media campaign aired in Philadelphia PA from December 2010 to March 2012. A representative sample of adult Philadelphia smokers was interviewed by telephone at baseline (n=491) and new samples were interviewed monthly throughout the campaign (n=2786). In addition, a subsample of these respondents was reinterviewed 3 months later (n=877).
Results
On average, participants reported seeing campaign ads four times per week. Among individual respondents, each additional campaign exposure per week increased the likelihood of later reporting using help (OR=1.08, p<0.01), adjusting for baseline use of help and other potential confounders. This corresponded to a 5% increase in the use of help for those with average exposure relative to those with no exposure. Cross-sectional associations between individual campaign exposure and intentions to use help were consistent with these lagged findings. However, there was no evidence of population-level campaign effects on use of help.
Conclusions
Although the campaign was effective at the individual level, its effects were too small to have a population-detectable impact.
Introduction
Clinical studies show that smokers are more likely to quit successfully with evidence-based assistance1,2 (i.e., talking to a doctor,3 using nicotine-replacement therapies (NRTs),4,5 using prescription pills,6 calling a quitline,7 going to a website,8 or enrolling in a program9,10). Indeed, smokers are up to twice as likely to quit successfully using help, as opposed to quitting “cold turkey.”1,11 Nevertheless, most smokers quit without help.12–14 Increasing the use of help could positively impact public health.15,16 Evaluations have shown that media campaigns promoting individual cessation aids can increase their utilization17 (e.g., quitlines,18–21 NRTs,19,22,23 and online programs21).
There is mixed evidence that promoting the use of help increases quit rates (beyond just use of help). In two Australian studies, exposure to NRT ads did not affect quits or smoking prevalence.24,25 However, an American study showed that pharmaceutical ads also increased the number of quits without help.22 In all three cases, pharmaceutical companies sponsored the ads. If instead public health departments sponsored “help” ads, they might be more effective as they have no financial interest in NRT purchases. To make their lack of financial interest more obvious, public health departments might avoid targeting specific products. Thus, a general help ad could remind smokers of types of help, show the absence of a hidden agenda, and present at least one viable option for diverse smokers.
In March 2010, the Philadelphia Department of Public Health (PDPH) received a 2-year grant from the CDC to curb tobacco use as one of 50 regions participating in the CDC’s Communities Putting Prevention to Work (CPPW) program. The PDPH created a mass media campaign intended to increase smokers’ use of help by promoting the benefit of using help to quit in campaign ad taglines. Campaign planners expected that raising awareness that it is easier to quit with help would increase smokers’ use of help. Mass media campaigns have successfully reduced smoking among adults.24,26–30 However, previous campaigns did not target the benefit of using help to quit. Philadelphia’s antismoking media campaign targeted adult smokers through TV, radio, transit, and convenience store ads.
The media campaign promoted the belief “it is easier to quit with help.” This belief was strongly related to the intention to use help in a formative survey of 501 Philadelphia smokers.31 According to the integrative model of behavioral prediction,32 a campaign strategy convincing smokers of this belief could increase intentions and use of help.33 Online pretests of drafts of some of the ads promoting this belief with 1269 smokers informed the final ad selections.31
The campaign aired from late December 2010 through March 2012, and included eight ads (two TV, four radio, and two print ads). As explained in the Methods section, only three of the ads (both TV and one of the radio ads) received sufficient exposure relative to baseline to be analyzed. The TV ads varied in their emphasis on the use of help. The cable TV ad featured a smoker repeatedly saying he would quit, but only succeeding after he “got help.” The voiceover states that it is easier to quit with help and suggests talking to a doctor or a quit coach to learn about treatments. The on-screen tagline shows the quitline number, website address, and the words “Quit with help. Quit for good.” The other TV ad, Rick Stoddard (the only recycled ad, originally developed for Massachusetts), started airing later in the campaign, primarily on broadcast TV, as part of CDC’s television buy for the CPPW. It included the same on-screen tagline without the voiceover. The only radio ad that received wide exposure used an extended version of the TV voiceover (see the Appendix for all three scripts).
The PDPH complemented the media campaign with other efforts to increase quitting. These included two periods of free NRT distribution via 1-800-QUIT-NOW (November 2010 and 2011). Other complementary activities included expanding public and private insurance coverage for smoking-cessation medications and implementing a public health detailing program to improve doctors’ ability to help patients quit smoking.34 This evaluation focuses solely on the media component of the intervention.
The study objective was to test the effectiveness of taglines in a local mass media campaign to increase smokers’ use of help. The overall evaluation design was distinctive for including three types of evidence for making inferences about campaign effects. The first was monthly rolling, cross-sectional data showing the secular trend of smokers’ use of help. Second, as even a positive secular trend might be due to non-campaign forces, associations between monthly campaign advertising and behavior were also considered. Both of these analyses assessed population-level effects. The third approach, focusing on individual differences, associated self-reported exposure with use of help. Two major concerns for analyses relying on self-reports are potential confounders and causal direction (i.e., those using help are more likely to recall exposure). To address these concerns, the individual difference analyses tested lagged effects, adjusting for baseline outcomes and other potential confounders. It is important to note that population- and individual-level analyses ask distinct questions; they ask, respectively, whether the campaign affected the average person, and whether the campaign affected those exposed to it. In other words, population-level analyses miss effects if exposure is limited; individual analyses miss effects that diffuse to indirectly exposed individuals. This evaluation design benefited from doing both.
Methods
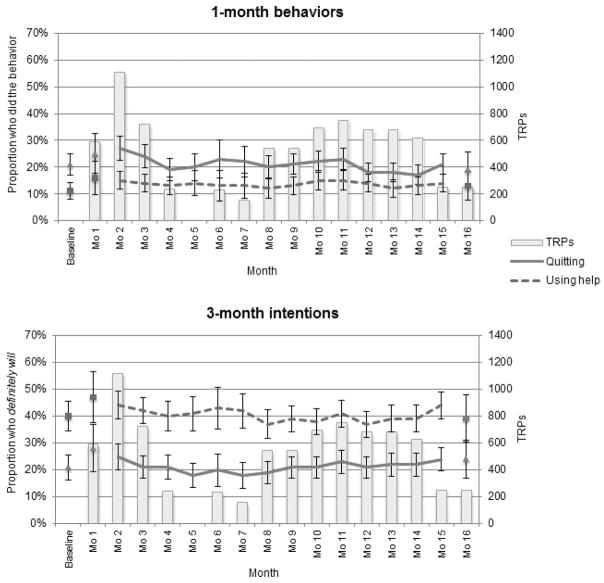
The main survey was administered to a substantial precampaign sample (n=498, December 2010) and then to 16 smaller monthly samples of adult smokers (n=2856 for the total campaign through March 2012, Figure 1). Social Science Research Solutions (SSRS) recruited and interviewed a representative sample monthly through random digit dialing of landline phones. To be eligible, participants had to be current smokers or quitters in the past 30 days. Recent quitters only represented 2% of the sample (n=77) and were removed. The response rate was estimated at 27% (American Association of Public Opinion Research Response Rate 3). SSRS also attempted to recontact respondents who were interviewed in 9 of the 16 months. On average, 50% of the approached smokers participated in the second interview (n=877). The University of Pennsylvania and City of Philadelphia IRB committees deemed this study exempt. Verbal consent was obtained before each interview.
Figure 1.
Sample sizes for the evaluation of rolling, cross-sectional and cohort smoker samples and monthly campaign media buys: Philadelphia antismoking campaign, 2010–2012
Targeted rating points (TRPs) are a standard estimate of how many people were potentially in the target audience (for this campaign, adults aged 25– 54 years) for purchased advertising.
Measures
Exposure
The primary independent variable was campaign exposure. With individual ads going on and off the air and the smaller recontact sample size, ad-level analyses could not be calculated reliably. Creating a single measure was necessary for conducting lagged analyses. Exposure was measured in two ways: (1) combined recall for effective ads and (2) combined targeted rating points (TRPs).
Individual exposure was measured through aided recall. The eight ads were described and respondents were asked if they recalled hearing or seeing each of them in the past month, and how often (0–7 days per week). Aided recall may lead to over-reporting because the description may sound familiar or participants might feel obliged to agree. To estimate the magnitude of over-reporting,35 estimates of recall before the ads aired were collected. While the ads aired for 5 of the 8 ads, recall estimates were not greater than baseline. Those ads were not included in total campaign exposure. Thus only the three effective ads, two TV ads and one radio ad, were included in the combined campaign exposure measure (0–21 exposures per week). Over-reporting might also taint these estimates; however, they likely yield conservative, rather than inflated, effect estimates.
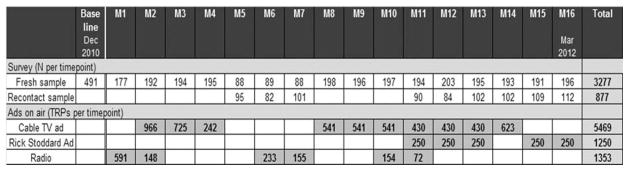
Population-level exposure combined monthly TRPs for the effective ads. TRPs are a standard estimate of how many people were potentially in the target audience (for this campaign, adults aged 25–54 years) for purchased advertising. The percentage of the population exposed (reach) and the average number of exposures (frequency) are multiplied to estimate TRPs. Thus an ad earns 100 TRPs if 100% of the audience was exposed once. Figures 1 and 2 present the monthly combined TRPs for the effective ads (numerically and graphically).
Figure 2.
Population-level effects of ad activity on quitting and using help: Philadelphia antismoking campaign, 2010–2012
Lines depict 3-month moving averages with CIs of ±2 SEs. Note that a moving average cannot be calculated for baseline, the first month, or the last month of the campaign period. Bars indicate the amount of campaign targeted rating points (TRPs) purchased each month (labeled on the right axis).
Confounders
All analyses adjusted for potential confounders: participant demographics (gender, race (white/nonwhite), age, education (years), marital status, children in household, and home ownership), religious attendance, Medicaid insurance, health status, and health orientation. Smoking-specific confounders included number of cigarettes smoked per day, percentage of other smokers in the household, and time to first cigarette (as a measure of nicotine dependence36). A dummy variable for the first 2 months of each phase of the NRT giveaways was also included. Individual-level analyses included a dummy variable for the first month each ad aired. Finally, all lagged analyses adjusted for use of the respective outcome prior to the first interview.
Outcomes
Overall use of help indicated whether a smoker used any of six types of help. It was created from six individual items (Did you [seek advice from your doctor or another health care provider; call the telephone quitline: 1-800-Quit-NOW; go to the website: SmokeFreePhilly.org; go to any programs; use any NRTs; use any prescription pill medications] to help you quit smoking since [3 months prior to interview]? What about in the past 30 days?). Seeking (non-doctor) advice indicated respondents had used any of three sources (quitline, website, or programs). Using medications indicated they had used either NRTs or pills. Parallel measures of intentions to do the six individual behaviors in 3 months were also assessed with four-point scales, where 1=definitely will not and 4=definitely will. Overall intentions to use help, seek (non-doctor) advice, and use medication were assigned based on the most likely rating of the individual intentions included in the respective sets.
Some researchers have raised concerns about advocating help in campaigns, as smokers may underestimate the risks of smoking or believe that they are too addicted to quit.37,38 Although there is little direct evidence for this hypothesis,39 the campaign’s impact on quit attempts regardless of help and reductions in daily cigarettes were also assessed.
Data Analyses
The analysis first considered evidence for population-level change in behaviors and intentions from baseline to during the campaign. Logistic and linear regression analyses compared baseline behaviors in the past month and intentions to the overall average of those outcomes during the campaign. The analysis also considered evidence for an upward trajectory during the campaign, assuming that campaign effects accumulate. Population-level analyses also assessed covariation between monthly campaign activity and outcomes. Following Dunlop and colleagues,40 a series of logistic regressions with increasingly larger accumulations of monthly TRPs tested ad activity’s effects on behaviors in the past month and on intentions.
For the individual-level analyses, cross-sectional and lagged analyses regressed behavior and intentions on campaign recall and potential confounders. The cross-sectional regressions used past-month behaviors and intentions as outcomes. The lagged analyses, using the recontact sample with 3-month follow-up interviews, predicted 3-month behavior and intention outcomes, adjusting for the matching behaviors and intentions at first interview and the other confounders. Although the lagged analyses were conducted on a smaller sample, they provide stronger evidence for causal claims because the temporal order is clear.
All analyses were conducted in 2012 using Stata version 12 (StataCorp, 2011, Cary NC) and were weighted separately for the cross-sectional and recontact samples by age, race, education, gender, homeownership, number of adults in the household, and presence of children to the 2008 Public Health Management Corporation (PHMC) data on Philadelphia smokers (www.chdbdata.org). Missing data ranged from 8%–15% in the individual analyses and were listwise deleted. All demographic results reported in the text are unweighted.
Results
The cross-sectional sample consisted of 3010 adult Philadelphia smokers, of whom 64% were women and 47% were non-Hispanic black (Table 1). Mean age was 52 years (SD=14 years). Most participants (65%) earned less than $40,000 a year, the median income of Philadelphia. Nevertheless, most had a doctor (78%) and some type of health insurance (90%).
Table 1.
Demographics and smoking behaviors
| Cross-sectional (n=3010)a % or M ± SD |
Recontact (n=804)a % or M ± SD |
|||
|---|---|---|---|---|
| Unweighted | Weighted | Unweighted | Weighted | |
| Female | 64 | 52 | 66 | 53 |
| Race/ethnicityb | ||||
| Non-Hispanic white | 43 | 42 | 45 | 42 |
| Non-Hispanic black | 47 | 44 | 48 | 44 |
| Hispanic | 6 | 9 | 4 | 9 |
| Other | 3 | 5 | 3 | 5 |
| Age (years) | 52 ± 14 | 45 ± 15 | 54 ±13 | 46 ± 14 |
| Education (years) | 13 ± 2 | 13 ± 2 | 13 ± 2 | 13 ± 2 |
| Marital status | ||||
| Married/living as married | 36 | 37 | 35 | 34 |
| Divorced/widowed/separated | 33 | 24 | 36 | 26 |
| Never married | 31 | 39 | 29 | 40 |
| Children present | 33 | 37 | 28 | 38 |
| Own (versus rent) | 61 | 49 | 61 | 50 |
| Income (<$40,000) | 65 | 66 | 66 | 68 |
| Employed | 42 | 45 | 41 | 42 |
| Religious attendance (more than monthly) | 43 | 39 | 42 | 36 |
| Insurance | ||||
| Any insurance other than Medicaid | 55 | 50 | 58 | 50 |
| Medicaid | 35 | 38 | 34 | 40 |
| Not covered by insurance | 10 | 12 | 8 | 10 |
| Has a doctor | 78 | 73 | 80 | 76 |
| Health statusb | ||||
| Very good/excellent | 25 | 25 | 26 | 26 |
| Good | 39 | 37 | 38 | 35 |
| Fair/poor | 36 | 38 | 37 | 39 |
| Health orientationb | ||||
| Strongly agree | 70 | 68 | 72 | 71 |
| Somewhat agree | 26 | 27 | 25 | 24 |
| Disagree | 4 | 4 | 3 | 4 |
|
| ||||
| Daily cigarettes | 13 ± 10 | 13 ± 10 | 14 ± 10 | 14 ± 10 |
| <5 minutes to first cigarette | 28 | 30 | 30 | 30 |
| Living situation | ||||
| All smokers | 19 | 29 | 19 | 23 |
| Some smokers | 11 | 17 | 11 | 13 |
| All others non-smokers | 35 | 28 | 34 | 38 |
| Alone | 35 | 26 | 36 | 26 |
Sample size reflects the unweighted analysis sample, which does not include 30-day quitters or those missing on confounders.
Percentage breakdowns within the variable do not always add up to 100% because of rounding.
Participants on average smoked a little over half a pack per day (13 cigarettes). Twenty-eight percent of respondents reported high levels of nicotine dependence. Thirty percent lived with other smokers. Most reported that their health was at least good (64%), and the majority (70%) agreed that they had a healthy orientation (e.g., strongly agreed that their health was important to them). Baseline use of help in the past month was 11.5%, and that of making a quit attempt was 19.0% (Table 2).
Table 2.
Campaign exposure and cessation outcomes
| Cross-sectional | Recontact (n=808) | |||
|---|---|---|---|---|
| Baseline (n=473) M (SD) | Campaign (n=2567) M (SD) | Campaign Time 1 M (SD) | Campaign Time 2 M (SD) | |
| Campaign activity (median weekly TRPsa) | 0 TRPs | 125 TRPs | 215 TRPs | – |
| Aided campaign recall (exposures per week) | 0.56 (1.44) | 4.00 (4.27) | 3.82 (4.18) | – |
|
| ||||
| Intentions (1–4-point scale) | ||||
| intend to use help | 2.99 (1.01) | 3.04 (1.01) | 2.96 (1.04) | 2.95 (1.03) |
| intend to seek advice from MDb | 2.63 (1.06) | 2.60 (1.08) | 2.54 (1.09) | 2.50 (1.14) |
| intend to seek advice from non-MDc | 2.57 (0.99) | 2.65 (1.02) | 2.55 (1.03) | 2.56 (1.03) |
| intend to call the quitline | 2.23 (0.96) | 2.28 (1.02) | 2.18 (1.01) | 2.20 (1.00) |
| intend to go to the website | 2.30 (1.01) | 2.30 (1.04) | 2.18 (1.02) | 2.19 (1.05) |
| intend to go to a quit program | 1.97 (0.87) | 1.98 (0.94) | 1.91 (0.94) | 1.89 (0.90) |
| intend to use medications | 2.34 (1.04) | 2.44 (1.08) | 2.38 (1.09) | 2.37 (1.10) |
| intend to use NRTsd | 2.13 (1.00) | 2.22 (1.06) | 2.17 (1.07) | 2.12 (1.10) |
| intend to use pills | 1.85 (0.99) | 1.90 (1.02) | 1.87 (1.01) | 1.84 (1.00) |
| intend to quit | 2.66 (0.94) | 2.63 (0.98) | 2.58 (0.98) | 2.69 (0.99) |
| intend to reduce cigarettes | 3.15 (0.89) | 3.14 (0.90) | 3.18 (0.91) | 3.15 (0.90) |
|
| ||||
| Behaviors (0/1) | Last 1 month (%) | Last 3 months (%) | ||
| used help | 11.5 | 13.0 | 33.6 | 30.5 |
| sought advice from MDb | 7.8 | 9.9 | 25.9 | 23.0 |
| sought advice from non-MDc | 2.4 | 1.4 | 4.9 | 6.9 |
| called the quitline | 1.8 | 0.9 | 2.5 | 3.3 |
| went to the website | 0.4 | 0.2 | 1.3 | 2.6 |
| went to a quit program | 0.6 | 0.6 | 1.8 | 1.9 |
| used medications | 4.2 | 4.4 | 11.0 | 11.1 |
| used NRTsd | 2.5 | 3.1 | 8.3 | 8.2 |
| used pills | 2.0 | 1.5 | 3.8 | 3.2 |
| quit attempt | 19.0 | 19.5 | 36.6 | 37.7 |
| reduced cigarettes | 34.4 | 36.1 | 54.2 | 60.7 |
All data are weighted and limited to the analysis sample, which does not include 30-day quitters at Time 1 or those missing on confounders.
Intentions were not asked of 30-day quitters at Time 2, so the recontact sample size for intentions is 734.
TRPs are a standard estimate of how many people were potentially in the target audience (for this campaign, adults aged 25–54 years) for purchased advertising.
MD refers to the participant’s doctor or another health care provider.
Non-MD refers to the quitline: 1-800-QUIT-NOW, the website: SmokeFreePhilly.org, or a quit smoking program.
NRTs such as the patch.
NRTs, nicotine-replacement therapies; TRPs, targeted rating points
Most respondents reported exposure to at least one of the three ads (74%, monthly range=34%–96%; details by ad are shown in the Appendix), and participants reported exposure to these ads four times per week on average (SD=4.3; range=1.3–6.6). The campaign purchased 8072 total TRPs for these three ads (median weekly TRPs=125, range=0–390, indicating 0–3.9 potential exposures per week assuming 100% reach). Self-reported exposure was higher than suggested by the purchased TRPs. This likely reflects some over-reporting bias.
There was no evidence for population-level change in the expected direction on any of the tested behaviors and intentions. No behavioral outcomes or intentions significantly increased during the campaign from baseline levels (Table 2) or showed an upward trajectory during the campaign (Figure 2). There was also no evidence of a negative effect on quit attempts or cigarette reduction. Additional analyses predicting behaviors and intentions from the sum of campaign activity 1, 2, 3, and 4 months prior to the respondents’ interviews did not show evidence of a positive association (data not shown).
However, at the individual level, lagged logistic regression analyses indicated that campaign recall significantly predicted four behaviors: using help, seeking advice from a doctor, using medication, and making a quit attempt (Table 3). After adjusting for prior use of help (in the past 3 months) and the other confounders, each additional campaign exposure per week was associated with an 8% increase in the likelihood of using help in the next 3 months (OR=1.08, p<0.01). The predicted probability of using help for those reporting average campaign exposure was 30%, and that for those reporting no campaign exposure was 25%. The lagged analyses also showed that quit attempts in the past 3 months significantly increased with campaign exposure (OR=1.06, p<0.05). Follow-up analyses showed that quit attempts with any help increased with campaign exposure (OR=1.11, p<0.01). In contrast, quit attempts without help were not related to campaign exposure (OR=0.99, p=0.65).
Table 3.
Individual-level, cross-sectional and lagged campaign effects
| Cross-sectional (n=2567) | Lagged (n=734) | |||
|---|---|---|---|---|
|
| ||||
| Intentions (1–4-point scale) | b | 95% CI | b | 95% CI |
|
| ||||
| intend to use help | 0.01* | 0.00, 0.02 | 0.01 | −0.01, 0.03 |
| intend to seek advice from MDa | 0.01* | 0.00, 0.03 | 0.01 | −0.01, 0.03 |
| intend to seek advice from non-MDb | 0.02** | 0.01, 0.03 | 0.01 | −0.01, 0.03 |
| intend to call the quitline | 0.02** | 0.01, 0.03 | 0.01 | −0.01, 0.03 |
| intend to go to the website | 0.01 | 0.00, 0.02 | 0.00 | −0.02, 0.03 |
| intend to go to a quit program | 0.02** | 0.01, 0.03 | 0.00 | −0.02, 0.01 |
| intend to use medications | 0.01 | 0.00, 0.02 | 0.02 | 0.00, 0.04 |
| intend to use NRTsc | 0.01 | 0.00, 0.02 | 0.02 | 0.00, 0.04 |
| intend to use pills | 0.01 | 0.00, 0.02 | 0.01 | −0.01, 0.03 |
| intend to quit | 0.01 | 0.00, 0.02 | 0.01 | −0.01, 0.03 |
| intend to reduce cigarettes | 0.00 | −0.01, 0.01 | 0.01 | −0.01, 0.03 |
| Behaviors (0/1) | Cross-sectional (past 1 month) (n=2567) | Lagged (past 3 months) (n=808) | ||
|---|---|---|---|---|
|
| ||||
| OR | 95% CI | OR | 95% CI | |
|
| ||||
| used help | 1.03 | 0.99, 1.06 | 1.08** | 1.03, 1.13 |
| sought advice from MDa | 1.03 | 0.99, 1.06 | 1.08** | 1.02, 1.14 |
| sought advice from non-MDb | 1.10** | 1.04, 1.17 | 1.04 | 0.97, 1.12 |
| called the quitline | 1.09* | 1.00, 1.18 | 1.11 | 0.99, 1.24 |
| went to the website | 1.11 | 0.97, 1.28 | 1.08 | 0.96, 1.21 |
| went to a quit program | 1.14* | 1.02, 1.27 | 0.87 | 0.75, 1.01 |
| used medications | 0.99 | 0.94, 1.05 | 1.09* | 1.01, 1.18 |
| used NRTsc | 1.02 | 0.95, 1.08 | 1.08 | 0.98, 1.19 |
| used pills | 0.92 | 0.84, 1.01 | 1.06 | 0.97, 1.16 |
| quit attempt | 1.02 | 0.99, 1.05 | 1.06* | 1.00, 1.11 |
| reduced cigarettes | 1.03* | 1.00, 1.05 | 1.01 | 0.96, 1.06 |
Note: Boldface and shaded estimates indicate statistical significance (*p<0.05, **p<0.01).
All data are weighted and limited to the analysis sample, which does not include 30-day quitters at Time 1 or those missing on confounders.
Cross-sectional associations adjust for: gender, race (white/nonwhite), age, education (years), marital status, children in household, home ownership, religious attendance, Medicaid insurance, health status, health orientation, number of cigarettes smoked per day in the last week, percentage of other people in the household who smoke, time until first cigarette, first 2 months of NRT giveaways, and first month an ad airs.
Lagged analyses additionally adjust for first interview outcome levels.
MD refers to the participant’s doctor or another health care provider.
Non-MD refers to the quitline: 1-800-QUIT-NOW, the website: SmokeFreePhilly.org, or a quit smoking program.
NRTs such as the patch.
NRTs, nicotine replacement therapy
Recall was significantly associated with five intention measures in cross-sectional linear regression models (Table 3). These associations were small but positive, and the remaining non-significant associations were also in a positive direction. However, recall did not significantly affect intentions in the lagged models. Observed cross-sectional associations between recall and three intentions corresponded to lagged effects of recall on actual behaviors, namely using any help, specifically seeking advice from a doctor, and a trend for using medication (intention p=0.08). Taken together, these results suggest that the campaign impacted the use of help among those exposed.
Discussion
Consistent with prior individual-level findings of the positive impact of cessation product ads on both utilization and quits,22 this study provides individual-level evidence that the campaign increased smokers’ use of any help among those exposed. Although the individual-level effects are small, they are striking, as they were produced primarily through ad taglines. Participants reporting more exposure were more likely to use help, even after adjusting for baseline use of help. Specifically, they were more likely to seek advice from a doctor and use medications. These lagged effects were also supported by cross-sectional associations between recall and intentions, adjusting for confounders. Although lagged analyses relied on a subsample of all participants, it was weighted to represent Philadelphia smokers, which reduces the threat of subsample bias.
At the population-level, however, there was no measurable evidence of change in using help. Considering the small size of the individual-level effect (the predicted probability of using help increased 5% for those with average levels of exposure relative to those with no exposure), the population-level effect is estimated to be only 2.5% (as half of the population did not see the campaign ≥four times a week). Thus, it is not surprising that population-level effects were not detected, as the sample size was only large enough to detect a 5% population increase in the use of help. The individual-level analysis, on the other hand, could detect smaller effects (1.9% change cross-sectionally; 4.6% change lagged). Sacrificing the ability to detect smaller population-level effects (using a larger sample) for the causal power of including a recontact sample was a valuable tradeoff in the study design.
Although small, a 2.5% population-level effect among 384,532 Philadelphia smokers (according to PHMC data, 25.2% of Philadelphians smoked in 2010) suggests that this campaign led to an estimated 9613 additional smokers in Philadelphia using some form of help to quit smoking. Given the evidence that using help to quit leads to more success,1,2,11 these smokers will likely be more successful in their quit attempts.
This campaign was unique in that it encouraged the use of help primarily through a tagline. Thus, we would expect the impact to be small. Additional pretesting of the final ads (rather than only testing to choose between draft ads) may have alerted planners of the small effects. Ads that fully integrated help into the narrative, provided specific information about types of help, or modeled a smoker using help would be expected to have larger effects.16 In addition, current research suggests that negative health effects messages have been the most persuasive, in part because of their emotional tone.26,41–43 Finally, ads with clear narratives (like the three in this campaign) have also been shown to be more effective.44 Integrating negative health effects into a quitting-with-help narrative could be quite powerful.
Some researchers are concerned that help-focused advertising will reduce quits overall.17,45 The evidence from this study, contrarily, showed a positive effect of the tagline promoting help on overall quitting.
Conclusion
The Philadelphia campaign was the first to measure the impact of a tagline on the use of help. The evaluation design provided an understanding of the efficacy of this tagline on the use of help among those who noticed the campaign (small, but reliable) and of the overall effect of the campaign on the average smoker (not detectable). We speculate that the campaign could have had a larger impact if ads had targeted using help to quit more aggressively.
Supplementary Material
Acknowledgments
The authors thank Giridhar Mallya, MD, MHSP for his thoughtful comments on this study, Emily Brennan, PhD for her assistance with interpretation of the data, Joseph N. Cappella, PhD for his useful comments on earlier presentations of this work, and Andy S.L. Tan, PHD, MBBS, MPH, MBA, Mihaela Moldovan-Johnson, PhD, Heather Forquer, MPH, and Danielle Naugle for their assistance with study and survey design.
Funding for this evaluation was made possible in part by Cooperative Agreement #1U58DP002633-01 from the CDC, USDHHS and Get Healthy Philly, an initiative of the Philadelphia Department of Public Health, as well as from the National Cancer Institute (grant # P50CA095856).
Footnotes
The views expressed in this manuscript do not necessarily reflect the official policies of the USDHHS, nor does mention of trade names, commercial practices, or organizations imply endorsement by the U.S. Government.
No financial disclosures were reported by the authors of this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Fiore MC, Jaen CR, Baker TB, Bailey WC, Benowitz NL, Curry SJ. Treating tobacco use and dependence: 2008 update. Rockville MD: USDHHS, U.S. Public Health Service; 2008. www.ahrq.gov/clinic/tobacco/treating_tobacco_use08.pdf. [Google Scholar]
- 2.Lemmens V, Oenema A, Knut IK, Brug J. Effectiveness of smoking cessation interventions among adults: a systematic review of reviews. Eur J Cancer Prev. 2008;17(6):535–44. doi: 10.1097/CEJ.0b013e3282f75e48. [DOI] [PubMed] [Google Scholar]
- 3.Stead LF, Buitrago D, Preciado N, Sanchez G, Hartmann-Boyce J, Lancaster T. Physician advice for smoking cessation. Cochrane Database Syst Rev. 2013;5:CD000165. doi: 10.1002/14651858.CD000165.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Stead LF, Perera R, Bullen C, et al. Nicotine replacement therapy for smoking cessation. Cochrane Database Syst Rev. 2012;11:CD000146. doi: 10.1002/14651858.CD000146.pub4. [DOI] [PubMed] [Google Scholar]
- 5.Hughes JR, Shiffman S, Callas P, Zhang J. A meta-analysis of the efficacy of over-the-counter nicotine replacement. Tob Control. 2003;12(1):21–7. doi: 10.1136/tc.12.1.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hughes JR, Stead LF, Lancaster T. Antidepressants for smoking cessation. Cochrane Database Syst Rev. 2007;1:CD000031. doi: 10.1002/14651858.CD000031.pub3. [DOI] [PubMed] [Google Scholar]
- 7.Stead LF, Perera R, Lancaster T. Telephone counselling for smoking cessation. Cochrane Database Syst Rev. 2006;3:CD002850. doi: 10.1002/14651858.CD002850.pub2. [DOI] [PubMed] [Google Scholar]
- 8.Civljak M, Sheikh A, Stead LF, Car J. Internet-based interventions for smoking cessation. Cochrane Database Syst Rev. 2010;9:CD007078. doi: 10.1002/14651858.CD007078.pub3. [DOI] [PubMed] [Google Scholar]
- 9.Lancaster T, Stead LF. Individual behavioural counselling for smoking cessation. Cochrane Database Syst Rev. 2005;2:CD001292. doi: 10.1002/14651858.CD001292.pub2. [DOI] [PubMed] [Google Scholar]
- 10.Stead LF, Lancaster T. Group behaviour therapy programmes for smoking cessation. Cochrane Database Syst Rev. 2005;2:CD001007. doi: 10.1002/14651858.CD001007.pub2. [DOI] [PubMed] [Google Scholar]
- 11.Pierce JP, Gilpin EA, Farkas AJ. Can strategies used by statewide tobacco control programs help smokers make progress in quitting? Cancer Epidemiol Biomarkers Prev. 1998;7(6):459–64. [PubMed] [Google Scholar]
- 12.Cokkinides VE, Ward E, Jemal A, Thun MJ. Under-use of smoking-cessation treatments: results from the National Health Interview Survey, 2000. Am J Prev Med. 2005;28(1):119–22. doi: 10.1016/j.amepre.2004.09.007. [DOI] [PubMed] [Google Scholar]
- 13.Hung WT, Dunlop SM, Perez D, Cotter T. Use and perceived helpfulness of smoking cessation methods: results from a population survey of recent quitters. BMC Public Health. 2011;11(1):592. doi: 10.1186/1471-2458-11-592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shiffman S, Brockwell SE, Pillitteri JL, Gitchell JG. Individual differences in adoption of treatment for smoking cessation: demographic and smoking history characteristics. Drug Alcohol Depend. 2008;93(1–2):121–31. doi: 10.1016/j.drugalcdep.2007.09.005. [DOI] [PubMed] [Google Scholar]
- 15.Levy DT, Mabry PL, Graham AL, Orleans CT, Abrams DB. Reaching Healthy People 2010 by 2013: a SimSmoke simulation. Am J Prev Med. 2010;38(3S):S373–S381. doi: 10.1016/j.amepre.2009.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Orleans CT. Increasing the demand for and use of effective smoking-cessation treatments reaping the full health benefits of tobacco-control science and policy gains--in our lifetime. Am J Prev Med. 2007;33(6S):S340–S348. doi: 10.1016/j.amepre.2007.09.003. [DOI] [PubMed] [Google Scholar]
- 17.Zhu S-H, Lee M, Zhuang Y-L, Gamst A, Wolfson T. Interventions to increase smoking cessation at the population level: how much progress has been made in the last two decades? Tob Control. 2012;21(2):110–8. doi: 10.1136/tobaccocontrol-2011-050371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bui QM, Huggins RM, Hwang W-H, White VM, Erbas B. A varying coefficient model to measure the effectiveness of mass media anti-smoking campaigns in generating calls to a Quitline. J Epidemiol. 2010;20(6):473–9. doi: 10.2188/jea.JE20090105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Langley TE, McNeill A, Lewis S, Szatkowski L, Quinn C. The impact of media campaigns on smoking cessation activity: a structural vector autoregression analysis. Addiction. 2012;107(11):2043–50. doi: 10.1111/j.1360-0443.2012.03958.x. [DOI] [PubMed] [Google Scholar]
- 20.Miller CL, Wakefield MA, Roberts L. Uptake and effectiveness of the Australian telephone Quitline service in the context of a mass media campaign. Tob Control. 2003;12(2S):ii53–ii58. doi: 10.1136/tc.12.suppl_2.ii53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schillo BA, Mowery A, Greenseid LO, et al. The relation between media promotions and service volume for a statewide tobacco quitline and a web-based cessation program. BMC Public Health. 2011;11(1):939. doi: 10.1186/1471-2458-11-939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Avery R, Kenkel D, Lillard DR, Mathios A. Private profits and public health: does advertising of smoking cessation products encourage smokers to quit? J Polit Econ. 2007;115(3):447–81. [Google Scholar]
- 23.Tauras JA, Chaloupka FJ, Emery S. The impact of advertising on nicotine replacement therapy demand. Soc Sci Med. 2005;60(10):2351–8. doi: 10.1016/j.socscimed.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 24.Wakefield MA, Spittal MJ, Yong H-H, Durkin SJ, Borland R. Effects of mass media campaign exposure intensity and durability on quit attempts in a population-based cohort study. Health Educ Res. 2011;26(6):988–97. doi: 10.1093/her/cyr054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wakefield MA, Durkin S, Spittal MJ, et al. Impact of tobacco control policies and mass media campaigns on monthly adult smoking prevalence. Am J Public Health. 2008;98(8):1443–50. doi: 10.2105/AJPH.2007.128991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Durkin SJ, Brennan E, Wakefield MA. Mass media campaigns to promote smoking cessation among adults: an integrative review. Tob Control. 2012;21(2):127–38. doi: 10.1136/tobaccocontrol-2011-050345. [DOI] [PubMed] [Google Scholar]
- 27.Emery S, Kim Y, Choi YK, Szczypka G, Wakefield MA, Chaloupka FJ. The effects of smoking-related television advertising on smoking and intentions to quit among adults in the U.S. : 1999–2007. Am J Public Health. 2012;102(4):751–7. doi: 10.2105/AJPH.2011.300443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.National Cancer Institute. The role of the media in promoting and reducing tobacco use. Bethesda MD: USDHHS, NIH, National Cancer Institute; 2008. NIH Pub. No. 07–6242. Report No.: 19. cancercontrol.cancer.gov/tcrb/monographs/19/m19_complete.pdf. [Google Scholar]
- 29.McAfee T, Davis KC, Alexander RL, Pechacek TF, Bunnell R. Effect of the first federally funded U.S. antismoking national media campaign. Lancet. 2013;382(9909):2003–11. doi: 10.1016/S0140-6736(13)61686-4. [DOI] [PubMed] [Google Scholar]
- 30.Farrelly MC, Duke JC, Davis KC, et al. Promotion of smoking cessation with emotional and/or graphic antismoking advertising. Am J Prev Med. 2012;43(5):475–82. doi: 10.1016/j.amepre.2012.07.023. [DOI] [PubMed] [Google Scholar]
- 31.Parvanta S, Gibson L, Forquer H, et al. Applying quantitative approaches to the formative evaluation of antismoking campaign messages. Soc Marketing Q. 2013;19(4):242–64. doi: 10.1177/1524500413506004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fishbein M, Ajzen I. Predicting and changing behavior: the reasoned action approach. New York: Psychology Press; 2010. [Google Scholar]
- 33.Hornik R, Woolf KD. Using cross-sectional surveys to plan message strategies. Soc Marketing Q. 1999;5(2):34–41. [Google Scholar]
- 34.Philadelphia Department of Public Health. Tobacco policy and control program: making the healthy choice the easy choice. Philadelphia PA: Philadelphia Department of Public Health; 2012. www.phila.gov/health/pdfs/TobaccoAnnualReport.pdf. [Google Scholar]
- 35.Niederdeppe J. Assessing the validity of confirmed ad recall measures for public health communication campaign evaluation. J Health Commun. 2005;10(7):635–50. doi: 10.1080/10810730500267662. [DOI] [PubMed] [Google Scholar]
- 36.Baker TB, Piper ME, et al. Transdisciplinary Tobacco Use Research Center (TTURC) Tobacco Dependence. Time to first cigarette in the morning as an index of ability to quit smoking: implications for nicotine dependence. Nicotine Tobacco Res. 2007;9(4S):S555–S570. doi: 10.1080/14622200701673480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pierce JP, Cummins SE, White MM, Humphrey A, Messer K. Quitlines and nicotine replacement for smoking cessation: do we need to change policy? Annu Rev Public Health. 2012;33:341–56. doi: 10.1146/annurev-publhealth-031811-124624. [DOI] [PubMed] [Google Scholar]
- 38.West R, McNeill A, Britton J, et al. Should smokers be offered assistance with stopping? Addiction. 2010;105(11):1867–9. doi: 10.1111/j.1360-0443.2010.03111.x. [DOI] [PubMed] [Google Scholar]
- 39.Durkin SJ, Wakefield MA, Spittal MJ. Looking for boomerang effects: a pre–post experimental study of the effects of exposure of youth to television advertising for nicotine replacement therapy and Zyban. Addict Behav. 2006;31(12):2158–68. doi: 10.1016/j.addbeh.2006.02.020. [DOI] [PubMed] [Google Scholar]
- 40.Dunlop S, Cotter T, Perez D, Wakefield M. Televised antismoking advertising: effects of level and duration of exposure. Am J Public Health. 2013;103(8):e1–8. doi: 10.2105/AJPH.2012.301079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Dunlop SM, Perez D, Cotter T. The natural history of antismoking advertising recall: the influence of broadcasting parameters, emotional intensity and executional features. Tob Control Published Online First. 2012 Nov 10; doi: 10.1136/tobaccocontrol-2011-050256. [DOI] [PubMed] [Google Scholar]
- 42.Biener L, Ji M, Gilpin EA, Albers AB. The impact of emotional tone, message, and broadcast parameters in youth anti-smoking advertisements. J Health Commun. 2004;9(3):259–74. doi: 10.1080/10810730490447084. [DOI] [PubMed] [Google Scholar]
- 43.Davis KC, Nonnemaker JM, Farrelly MC, Niederdeppe J. Exploring differences in smokers’ perceptions of the effectiveness of cessation media messages. Tob Control. 2011;20(1):26–33. doi: 10.1136/tc.2009.035568. [DOI] [PubMed] [Google Scholar]
- 44.Durkin SJ, Biener L, Wakefield MA. Effects of different types of antismoking ads on reducing disparities in smoking cessation among socioeconomic subgroups. Am J Public Health. 2009;99(12):2217–23. doi: 10.2105/AJPH.2009.161638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chapman S, MacKenzie R. The global research neglect of unassisted smoking cessation: causes and consequences. PLoS Med. 2010;7(2):e1000216. doi: 10.1371/journal.pmed.1000216. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.