Abstract
The objective of this study was to compare the outcomes of the modified Nesbit procedure using different techniques for dissecting the neurovascular bundle (NVB) to correct ventral congenital penile curvatures (CPCs). The bundle was mobilized using the medial and lateral dissection technique in 21 (Group 1) and 13 (Group 2) patients, respectively. In the medial technique, Buck's fascia is opened at the dorsal side of the penis, the deep dorsal vein is removed at the most prominent site of the curvature and a diamond-shaped tunica albuginea (TA) is excised from the midline of the penis. In the lateral technique, the bundle is mobilized using a longitudinal lateral incision of the Buck's fascia above the urethra at the 5 and 7 o’clock positions via a bilateral approach. The localization and degree of curvature was evaluated using the combined intracavernous injection stimulation test or from the patients’ photographs. The mean patient age and degree of curvature were similar between groups. The mean operation time was longer for Group 2 (P = 0.01). In Group 1, nine patients (42.8%) required one diamond excision, 10 (47.6%) required two diamond excisions and two (9.5%) required more than two excisions; in Group 2, six patients (46.2%) required two diamond excisions and seven patients (53.8%) required more than two diamond excisions (P = 0.019). The differences in penile shortening, penile straightening and numbness of the glans penis were not statistically significant. Medial dissection of the bundle for the modified Nesbit procedure reduces the number of diamond-shaped removals of TA and thus shortens operation time in comparison with its lateral counterpart.
Keywords: congenital penile curvature, lateral dissection, medial dissection, nesbit, neurovascular bundle, ventral curvature
INTRODUCTION
Congenital penile curvature (CPC) is a rare condition with a prevalence of 0.04%–0.60% in the population.1,2 However the incidence of curvature without hypospadias was reported to be 4%–10% in a recent study.3 In CPC, there is a relative asymmetry between the two sides of the erect penis, which may arise from decreased compliance of one side of the tunica albuginea (TA) or outright foreshortening of one of the erectile bodies; consequently, straightening of the penis can be achieved using various surgical techniques.
One of the most common and the best validated techniques for correcting ventral CPC is the Nesbit procedure, which is performed by excising a pair of ellipsoid portions of TA from the dorsal side of the corpora cavernosa.4,5,6 In this technique, the neurovascular bundle (NVB) is totally mobilized using longitudinal lateral incisions of the Buck fascia above the urethra at the 5 and 7 o’clock positions using a bilateral approach.7 Overtime, various modifications of this technique have been proposed, such as the excision of a diamond of tissue from the TA instead of the originally described ellipsoid portions.8 Giammusso et al.9 and Colpi et al.10 reported a modification of the Nesbit operation consisting of the excisions of a diamond-shaped portion from the intracavernous septum and medial dissection of the NVB. In the present study, we aimed to compare the outcomes of a modified Nesbit procedure using medial or lateral dissection of NVB to correct ventral CPC.
MATERIALS AND METHODS
Patients
Between July 2005 and June 2010, 34 patients who underwent surgical correction for ventral CPC with a modified Nesbit procedure performed by a single surgeon (AK) were evaluated. Seven patients had concomitant lateral deviation. The mean presentation age and degree of curvature were 25.0 ± 7.2 (16–47) years and 54.7 ± 12.9 (30–90) degrees, respectively.
Preoperatively, all patients were evaluated with a comprehensive history and clinical examination. The localization and degree of curvature was evaluated using intracavernous injection of a vasoactive agent (described elsewhere) or patients’ photographs.1 The indications for surgical treatment were difficult penetration during coitus and/or embarrassment about the shape of the erect penis. Both sides of the erect penis had adequate length for shortening operations (length was measured with the penis in an erect state), and none of the patients reported erectile dysfunction.
Of the present study cohort, 21 and 13 patients underwent a modified Nesbit procedure with medial (Group 1) or lateral (Group 2) dissection of NVB. Group 1 underwent the modified Nesbit procedure between June 2007 and June 2010 and Group 2 underwent the procedure between July 2005 and June 2007.
Surgical technique
After a circumcising incision, the skin was degloved to the base of the penis. An artificial erection was induced by injecting saline through a 21-gauge butterfly cannula inserted into one of the corpora cavernosa to determine the most prominent site of the penile curvature.
During the lateral or medial dissection of the NVB, optical magnification (3.5 ×) was preferred to isolate the NVB from the underlying TA.
For the lateral dissection technique, the NVB was mobilized using longitudinal lateral incisions of the Buck's fascia above the urethra at the 5 and 7 o’clock positions, and the fascia was removed to the 11 and 1 o’clock positions. Afterwards, Allis clamps were applied to the TA of the right and left corpora cavernosa and a pair of diamond-shaped tunica were excised symmetrically (Figure 1). For the medial dissection technique, Buck's fascia was opened at the dorsal side of the penis, and the deep dorsal vein was removed at the most prominent location of the curvature. The NVB was minimally dissected (approximately 0.5 cm from each side) in a medial-to-lateral direction. After the induction of artificial erection, Allis clamps were applied to the TA in the bed of NVB, and one or more diamond-shaped, 4- to 5-mm deep excisions were made from the inter-cavernous septum (Figure 2). Afterwards, the residual defect was closed transversely with nonabsorbable No. 0 polyester sutures, using an inverted stitch technique to bury the knots under the TA. The second layer of the tunica was closed using 2-0 polyglycolic acid sutures. Of note, specific attention was taken to excise diamond-shaped tissues from TA less than 1 cm in a longitudinal direction to prevent “dog-ear” deformity. When needed, more than one diamond-shaped tunica was excised to correct the deformity completely, depending on the degree of residual curvature. After penile straightening was confirmed by intraoperative artificial erection and a curvature degree less than 10, Buck's fascia was closed with 5-0 polyglactin sutures after hemostasis was achieved. The Colles fascia and skin were closed with 3-0 polyglactin sutures.
Figure 1.
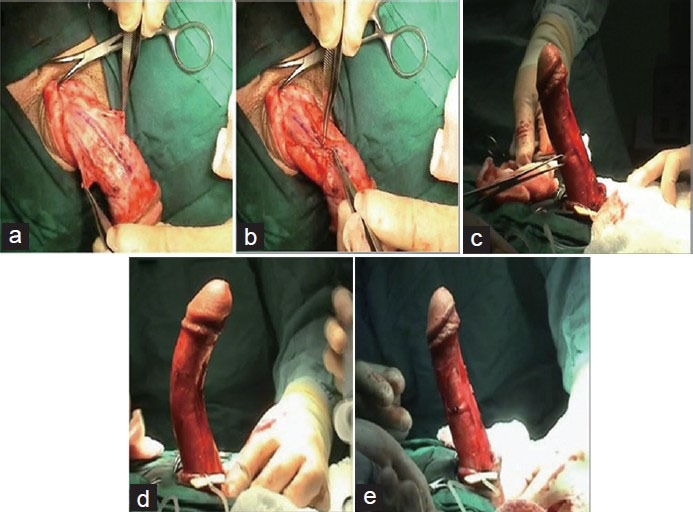
The lateral dissection technique for the modified Nesbit procedure. (a) Neurovascular bundle mobilized using longitudinal lateral incisions of the Buck's fascia above the urethra at the 5 and 7 o’clock positions. (b) Fascia was removed towards to the 11 and 1 o’clock positions. (c) Allis clamps applied to the tunica albuginea of the right and left corpora cavernosa. (d) Initial artificial erection of penis. (e) Straight penis at the final artificial erection confirmation.
Figure 2.
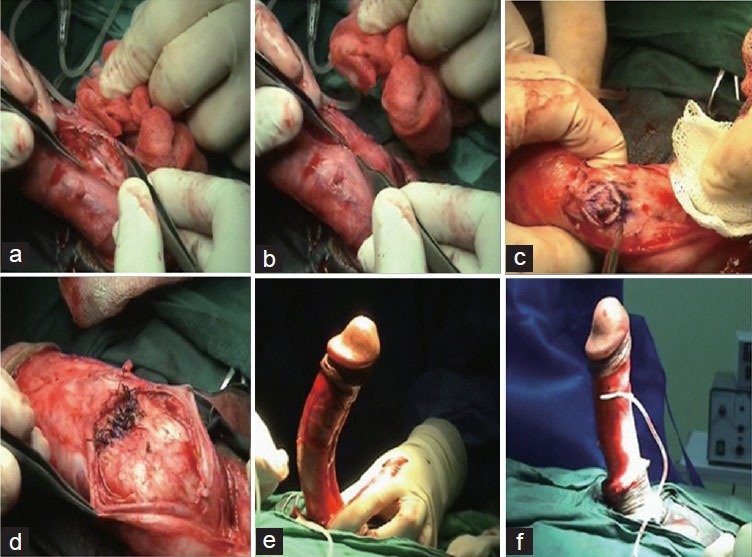
The medial dissection technique for the modified Nesbit procedure. (a) Buck's fascia was opened at the dorsal side of the penis. (b) The deep dorsal vein was removed at the most prominent location of the curvature. (c) One or more diamond-shaped, 4- to 5-mm deep excisions were made from the intercavernous septum. (d) The residual defect closed transversely with nonabsorbable no. 0 polyester sutures, using an inverted stitch technique to bury the knots under the TA. The second layer of the tunica was closed using 2-0 polyglycolic acid sutures. (e) Initial artificial erection of penis. (f) Straight penis at the final artificial erection confirmation.
Postoperative assessment
The patients were evaluated according to clinical criteria, such as penile straightening, penile shortening, recurrence of curvature, suture discomfort, erectile function and operative parameters, such as the mean operation time and the number of diamonds removed. Office consultations were performed at 3 and 12 months postoperatively and every 6 months thereafter.
Statistical analysis
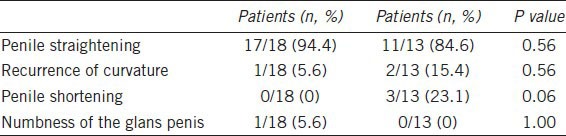
Statistical analysis was performed using Statistical Package for Social Sciences version 16 (SPSS Inc., Chicago, Illinois). Continuous variables were compared with the Mann–Whitney U test. The proportion of categorical variables was analyzed using Chi-squared or Fisher's exact tests, as appropriate (Tables 1 and 2).
Table 1.
Comparison of preoperative and perioperative parameters for both groups
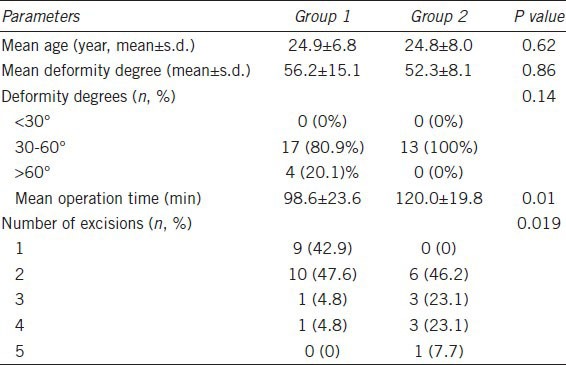
Table 2.
Comparison of the postoperative outcomes for the two groups
RESULTS
The patients’ mean age and mean degree of curvatures were similar between the groups (Table 1). For Group 1, the degree of the curvature was greater than 60° in four patients (19%) and between 30 and 60° in 17 (81%) patients. All the patients in Group 2 had curvatures between 30 and 60°.
The mean operation time was longer for Group 2 (98.6 vs 120.0 min, P = 0.01). In the Group 1, nine patients (42.9%) required one diamond-shaped excision, 10 (47.6%) required two excisions, and 2 (9.5%) required more than 2 excisions; in Group 2, six patients (46.2%) required 2 excisions and seven (53.8% required more than two excisions (P = 0.019; Table 1).
The mean follow-up time was 16.1 (3–48) months for Group 1 and 31.6 (3–66) months for Group 2. Residual/recurrent curvature was defined as a curvature degree greater than 20° or curvature that prevented coitus. In Group 1, three patients were lost to follow-up and postoperative values of 18 patients were used in the calculations. The initial penile straightening and the recurrence of the curvature rates were reported as 94.4% (n = 17/18) vs 84.6% (n = 11/13, P = 0.56) and 5.6% vs 15.4% (P = 0.56) for these two groups, respectively. The difference between the groups was even more drastic for patient-reported penile shortening rates (0% vs 23.1%, P = 0.06). Patient-reported numbness of the glans penis was observed in one (5.6%) patient who underwent medial dissection and no patients in the lateral dissection group. Although there was no statistically significant difference between the two groups in terms of postoperative outcomes, Group 1 showed substantially better performance for these parameters. The postoperative outcomes for both groups are presented in Table 2.
DISCUSSION
Surgical treatment alternatives for penile curvature have been defined as shortening the convex or lengthening the concave side of the penis and penile disassembly technique. In fact, the penile lengths of patients with CPC are longer than average.11 Therefore, penile shortening procedures have generally been preferred in the treatment of CPC. Several shortening procedures, including penile plication and the Nesbit and Yachia procedures, have been described.7
Simple plication of the TA (penile plication) was popularized by Ebbehoj and Metz.12 Yachia described longitudinal incisional corporoplasty, in which the TA was incised longitudinally and then sutured transversally.13 The advantage of both techniques is that there is no need to dissect the underlying erectile tissue. However, suture granulomas, which may develop as a result of tunical plication, are perceivable during palpation of the penis and also during sexual intercourse. In Yachia's technique, suture discomfort is lower than in the former technique. In a study comparing plication and the lateral Nesbit technique, there was a significant difference in penile hyposensitivity, with rates of 38% and 75%, respectively.14 The rate of recurrence reported for the Nesbit procedure was much lower than the plication rate reported in comparative studies (0%–18% vs 16%–55%).14,15
Nesbit originally described the correction of congenital penile deformities to shorten the longer side of the penis by excising an elliptic portion of TA.4 Depending on the degree of curvature, more than one ellipsoid portions of the tunica may need to be excised to correct the deformity completely. In the largest series, 16 years of experience with using the Nesbit procedure to correct CPC in 106 patients was published and reported a success rate of 96.2%.16 Similarly, in the present study, success was achieved in 94.4% of Group 1 and 84.6% of Group 2. Because of its high success rate, this technique is preferred in some reports.9
In a recent Nesbit modification, smaller (3 × 2 mm) parts of the TA were removed, and the NVB was mobilized only on one side to prevent neural injury.17 The “underlap technique” is another Nesbit modification that has been recently proposed; it is based on the preparation of U-shaped TA flaps without excision.18
Generally, for the correction of ventral deformities, the NVB may be mobilized using medial or lateral dissection techniques. In the lateral dissection technique, the NVB is mobilized by longitudinal lateral incisions of Buck's fascia above the urethra at the 5 and 7 o’clock positions using a bilateral approach, and the NVB was elevated toward the midline. In contrast, in the medial dissection technique, after the removal of the deep dorsal vein, limited dissection of the NVB on the dorsolateral aspect of the corpora cavernosa is needed when applying the Nesbit procedure. Additionally, when medial dissection is chosen, the excision of a single diamond-shaped tunical portion from the midline of the penis may be sufficient to provide penile straightening. In the present study, the curvatures of nine patients in the medial dissection group were straightened by excising a single diamond-shaped section from the midline of the TA. Meanwhile, it is rational to consider that in the medial dissection technique, the excision of a diamond at the midline protects the symmetry of the corpora cavernosa more than the lateral dissection technique does.9 Because of the above-mentioned advantages, we changed our approach from lateral dissection to the medial dissection technique.
Because of the surgical method used, penile shortening should be accepted as a normal outcome. In one of the two studies in which the lateral dissection technique was preferred, Savoca et al.19 reported significant penile shortening (from 1.5 to 3 cm) in 36 of 279 patients with the Nesbit procedure after a mean follow-up of 89 months. Of these patients, only five (1.79%) reported difficulty during sexual intercourse that was attributable to penile shortening.19 Similarly, in the study by Andrews et al.16 penile shortening was detected in 3.7% of the patients. In that study, no patients complained of sexual dysfunction that was attributable to postoperative penile shortening.16 All the patients in the present study reported penile shortening after the procedure. However, in the lateral dissection group, 23.1% of the patients attached importance to that finding, which was not statistically significant. Studies claiming that potentially greater penile shortening might ensue after lateral dissection associated this finding with the use of the diamond-shaped excisions of the TA and the disruption of intercavernosal symmetry.10 However, the penile length in patients with CPC is more than two standard deviations greater than the mean normal length for their age.20 Therefore, we believe that penile shortening after straightening procedures is not a serious concern for patients with CPC when compared with patients with Peyronie's disease.
Suture discomfort during sexual intercourse has been reported in 35% of patients who underwent penile plication using nonabsorbable sutures and 12% of those who underwent multiple parallel plication techniques.16,19,20,21 In one study, palpable suture induration was as high as 51% in patients who underwent plication.22 However, in our study, which used a modified Nesbit technique, none of the patients in either group complained of discomfort from sutures. Similarly, Colpi et al.10 also did not report any incidence of discomfort related to sutures in 51 CPC patients who underwent the modified Nesbit procedure. Those authors used a penile septoplasty technique to mobilize the NVB. In this technique, following a limited NVB dissection, a diamond-shaped midportion of the TA is excised to close the defect. The authors reported a 96% success rate without any significant complications.10 In our series, after medial dissection of the NVB and the removal of a diamond-shaped portion from the midline of the TA, the defect was closed in two layers using nonabsorbable-0-polyester intratunically and absorbable 2–0 polyglycolic sutures. The preference of the intratunical nonabsorbable suturing technique is thought to decrease recurrence rates and to minimize discomfort that might arise from suturing. One of the important points associated with recurrences is the tension of the suture. In this technique, in which a diamond-shaped portion is excised from the midline, the tensile load of the septal sutures during full penile erection is reduced in comparison with the extraction of ellipsoid tissue from both corpora cavernosa and double plication performed following a lateral dissection technique.23
Histological and neuroanatomical studies conducted by Baskin et al.24 detected an absence of nerve fibers at the 12 o’clock position. Because of the minimal mobilization of NVB is required in the medial dissection technique, it might be postulated that the risk of sensory nerve damage is lower than that associated with the lateral dissection technique. However, in the present study, no statistically significant difference between groups was detected for glandular partial sensory loss. In a study in which medial dissection was preferred, partial glandular sensory loss was not reported in patients who had undergone the modified Nesbit procedure.11 Similarly, in only two (1.9%) of 106 patients with CPC who had undergone the modified Nesbit procedure with lateral dissection, partial glandular sensory loss was reported; thus, it might be concluded that the probability of sensorial nerve damage is not affected by the NVB dissection technique.16
In the medial dissection technique, only a diamond-shaped portion of TA overlying intercavernosal septum was excised, which meant fewer of excisions relative to the lateral dissection technique. In the present study, a significant difference in the number of diamond-shaped portions dissected was noted (P = 0.019). A narrower excision area and fewer numbers of excisions in the medial dissection technique lead to relatively shorter operative times.
The present study is the first comparative study of the modified Nesbit procedure for comparing NVB dissection techniques. However, this study has some limitations because of its retrospective, nonrandomized design and small number of patients. It should be noted that the patient variation between the two groups is caused by the time-based patient selection method of the study (Lateral dissection: 2005–2007 and medial dissection: 2007–2010). Consequently, long-term prospective and randomized studies with larger patient series are necessary to standardize the role of medial dissection NVB in the modified Nesbit procedure.
In conclusion, the present study revealed that fewer diamond-shaped portions of the TA needed to be excised in ventral CPC patients undergoing the Nesbit procedure with a medial dissection technique; hence, this technique shortens operation time. This technique also provides less mobilization of NVB, but neither injury of the sensorial nerve structure nor increase in numbness of the glans penis have been revealed. Despite the statistical nonsignificance, it should be noted that higher rates of curvature recurrence and penile shortening complications were observed in the lateral dissection group. The modified Nesbit procedure with medial dissection technique may provide excellent penile straightening with shorter operation times for patients with ventral CPC.
AUTHOR CONTRIBUTIONS
FA collected data retrospectively and composed the manuscript. TA performed the statistical analysis. ES performed linguistic and overall editing, and drafted and revised the manuscript. MD executed the data interpretation and made intellectual contributions. MO was involved in data collection and patient follow-up. AK performed the surgical procedures, coordinated the overall design and structure of the article, and supervised the writing and drafting process. All authors participated in the design and coordination of the study and sequence alignment and drafted the manuscript. All authors read and approved the final manuscript.
COMPETING INTERESTS
All authors declare no competing interests.
REFERENCES
- 1.Yachia D, Beyar M, Aridogan IA, Dascalu S. The incidence of congenital penile curvature. J Urol. 1993;150:1478–9. doi: 10.1016/s0022-5347(17)35816-0. [DOI] [PubMed] [Google Scholar]
- 2.Ebbehoj J, Metz P. Congenital penile angulation. Br J Urol. 1987;60:264–6. doi: 10.1111/j.1464-410x.1987.tb05497.x. [DOI] [PubMed] [Google Scholar]
- 3.Montag S, Palmer LS. Abnormalities of penile curvature: chordee and penile torsion. ScientificWorldJournal. 2011;11:1470–8. doi: 10.1100/tsw.2011.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nesbit RM. Congenital curvature of the phallus: report of three cases with description of corrective operation. 1965. J Urol. 2002;167:1187–8. doi: 10.1016/s0022-5347(02)80380-9. [DOI] [PubMed] [Google Scholar]
- 5.Frank JD, Mor SB, Pryor JP. The surgical correction of erectile deformities of the penis of 100 men. Br J Urol. 1981;53:645–7. doi: 10.1111/j.1464-410x.1981.tb03282.x. [DOI] [PubMed] [Google Scholar]
- 6.Rodriguez Tolra J, Franco Miranda E, Prats Puig JM, Cuadrado Campana J, Serrallach Mila N. Surgical treatment of the congenital curvature of the penis by the Nesbit technique. Arch Esp Urol. 2004;57:141–5. [PubMed] [Google Scholar]
- 7.Kadioglu A, Kucukdurmaz F, Sanli O. Current status of the surgical management of Peyronie's disease. Nat Rev Urol. 2011;8:95–106. doi: 10.1038/nrurol.2010.233. [DOI] [PubMed] [Google Scholar]
- 8.Kelami A. Congenital penile deviation and its treatment with the Nesbit-Kelami technique. Br J Urol. 1987;60:261–3. doi: 10.1111/j.1464-410x.1987.tb05496.x. [DOI] [PubMed] [Google Scholar]
- 9.Giammusso B, Burrello M, Branchina A, Nicolosi F, Motta M. Modified corporoplasty for ventral penile curvature: description of the technique and initial results. J Urol. 2004;171:1209–11. doi: 10.1097/01.ju.0000110297.98725.25. [DOI] [PubMed] [Google Scholar]
- 10.Colpi G, Piediferro G, Castiglioni F, Contalbi G, Carmignani L. Penile septoplasty for congenital ventral penile curvature: results in 51 patients. J Urol. 2009;182:1489–94. doi: 10.1016/j.juro.2009.06.059. [DOI] [PubMed] [Google Scholar]
- 11.Jordan GH, McCammon Kurt A. Surgery of the penis and urethra: curvatures of the penis. In: Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Campbell-Walsh Urology. 10th ed. Saunders; 2011. pp. 992–5. [Google Scholar]
- 12.Ebbehoj J, Metz P. New operation for “krummerik” (penile curvature) Urology. 1985;26:76–8. doi: 10.1016/0090-4295(85)90264-x. [DOI] [PubMed] [Google Scholar]
- 13.Yachia D. Modified corporoplasty for the treatment of penile curvature. J Urol. 1990;143:80–2. doi: 10.1016/s0022-5347(17)39871-3. [DOI] [PubMed] [Google Scholar]
- 14.Leonardo C, De Nunzio C, Michetti P, Tartaglia N, Tubaro A. Plication corporoplasty versus Nesbit operation for the correction of congenital penile curvature. A long-term follow-up. Int Urol Nephrol. 2012;44:55–60. doi: 10.1007/s11255-011-9976-z. [DOI] [PubMed] [Google Scholar]
- 15.Brake M, Keller H, Lamadé F, Groh R, Horsch R. Surgical correction of penile deviation. Nesbit vs. Schroeder-Essed method. Urologe A. 1999;38:264–9. doi: 10.1007/s001200050279. [DOI] [PubMed] [Google Scholar]
- 16.Andrews HO, al-Akraa M, Pryor JP, Ralph DJ. The Nesbit operation for congenital curvature of the penis. Int J Impot Res. 1999;11:119–22. doi: 10.1038/sj.ijir.3900390. [DOI] [PubMed] [Google Scholar]
- 17.Kuehhas FE, Egydio PH. Superficial tunica albuginea excision, using geometric principles, for the correction of congenital penile curvature. BJU Int. 2012;110:E949–53. doi: 10.1111/j.1464-410X.2012.11350.x. [DOI] [PubMed] [Google Scholar]
- 18.Schwarzer JU, Steinfatt H. Tunica albuginea underlap-a new modification of the Nesbit procedure: description of the technique and preliminary results. J Sex Med. 2012;9:2970–4. doi: 10.1111/j.1743-6109.2012.02887.x. [DOI] [PubMed] [Google Scholar]
- 19.Savoca G, Scieri F, Pietropaolo F, Garaffa G, Belgrano E. Straightening corporoplasty for Peyronie's disease: a review of 218 patients with median follow-up of 89 months. Eur Urol. 2004;46:610–4. doi: 10.1016/j.eururo.2004.04.027. [DOI] [PubMed] [Google Scholar]
- 20.Adams MC, Chalian VS, Rink RC. Congenital dorsal penile curvature: a potential problem of the long phallus. J Urol. 1999;161:1304–7. doi: 10.1016/s0022-5347(01)61675-6. [DOI] [PubMed] [Google Scholar]
- 21.Gholami SS, Lue TF. Correction of penile curvature using the 16-dot plication technique: a review of 132 patients. J Urol. 2002;167:2066–9. [PubMed] [Google Scholar]
- 22.Lee SS, Meng E, Chuang FP, Yen CY, Chang SY, et al. Congenital penile curvature: long-term results of operative treatment using the plication procedure. Asian J Androl. 2004;6:273–6. [PubMed] [Google Scholar]
- 23.Kadioglu A, Sanli O, Akman T, Cakan M, Erol B, et al. Surgical treatment of Peyronie's disease: a single center experience with 145 patients. Eur Urol. 2008;53:432–9. doi: 10.1016/j.eururo.2007.04.045. [DOI] [PubMed] [Google Scholar]
- 24.Baskin LS, Erol A, Li YW, Liu WH. Anatomy of the neurovascular bundle: is safe mobilisation possible? J Urol. 2000;164:977–80. doi: 10.1097/00005392-200009020-00014. [DOI] [PubMed] [Google Scholar]


