Abstract
Childhood-onset systemic lupus erythematosus (cSLE) is a severe multisystem autoimmune disease. Renal involvement occurs in the majority of cSLE patients and is often fatal. Renal biopsy is an important investigation in the management of lupus nephritis. Treatment of renal lupus consists of an induction phase and maintenance phase. Treatment of childhood lupus nephritis using steroids is associated with poor outcome and excess side-effects. The addition of cyclophosphamide to the treatment schedule has improved disease control. In view of treatment failure using these drugs and a tendency for non-adherence, many newer agents such as immune-modulators and monoclonal antibodies are being tried in patients with cSLE. Trials of these novel agents in the pediatric population are still lacking making a consensus in the management protocol of pediatric lupus nephritis difficult.
Keywords: Pediatric, Lupus nephritis, Management, Monoclonal antibody, Cyclophosphamide, Mycophenolate mofetil
Core tip: Childhood-onset systemic lupus erythematosus (cSLE) is a rare but severe autoimmune disease with multisystem involvement. Renal disease occurs in 50% to 75% of all cSLE patients and is a major cause of increased morbidity and mortality. Originally SLE nephritis was treated with steroids with a poor outcome which improved markedly with the introduction of cyclophosphamide, but at the cost of increased side effects which resulted in a further search for a less toxic, but equally effective regime. Here we discuss some newer drugs including immune-modulators and monoclonal antibodies in addition to azathioprine and mycophenolate mofetil, however, most of the evidence on these medications is restricted to adult literature and pediatric data are extrapolated from these trials.
INTRODUCTION
Epidemiology
Childhood-onset systemic lupus erythematosus (cSLE) is a rare but severe autoimmune disease with multisystem involvement, the incidence is 0.3/100000-0.9/100000 children-per year with a prevalence of 3.3/100000-8.8/100000 children[1]. A higher frequency of cSLE is reported in Asians, African Americans, Hispanics, and native Americans[2]. Median age of onset of cSLE is between 11 and 12 years (rare below 5 years), and 80% of patients are female[3]. cSLE follows a more severe disease course than adult-onset SLE, with higher morbidity and lower survival rates[4].
Diagnosis of cSLE
Four out of 11 American College of Rheumatology (ACR) criteria have a sensitivity and specificity greater than 95% for the diagnosis of cSLE. These criteria are as follows: malar rash, discoid rash, photosensitivity rash, oral or nasopharyngeal ulceration, nonerosive arthritis, serositis, renal disorder, neurologic disorder, hematologic disorder, immunologic disorder, and antinuclear antibody[5]. Although still not widely used, the newer systemic lupus international collaborating clinics (SLICC) criteria have been introduced for the classification of SLE[6]. According to the SLICC rule for the classification of SLE, the patient must satisfy at least 4 criteria, including at least one clinical criterion and one immunologic criterion OR the patient must have biopsy-proven lupus nephritis in the presence of antinuclear antibodies or anti-double-stranded DNA antibodies.
Renal involvement
Renal disease occurs in 50% to 75% of all cSLE patients, mostly within the first 2 years after diagnosis[7]. Lupus nephritis (LN) is more common in males and in non-White populations[8,9]. Initial manifestations of renal disease range from minimal proteinuria and microscopic hematuria to nephrotic-range proteinuria, urinary casts, severe hypertension, peripheral edema, and renal insufficiency or acute renal failure. SLE most commonly affects the glomerulus (i.e., lupus nephritis), but can also involve the renal interstitium. It can also present with features of thrombotic microangiopathy including both atypical hemolytic uremic syndrome as well as thrombotic thrombocytopenic purpura.
CASE DEFINITION FOR LN
As per the ACR criteria, LN is defined as: persistent proteinuria i.e., 0.5 g per day [a spot urine protein/creatinine ratio of 0.5 can be substituted) or greater than 3+ by dipstick; and/or cellular casts including red blood cells (RBCs), granular, tubular, or mixed][10]. An additional, perhaps optimal, criterion is a renal biopsy sample demonstrating immune complex-mediated glomerulonephritis compatible with LN[11]. As the severity of the nephritis may not correlate with the severity of the clinical signs and symptoms, a renal biopsy should be performed for any suspicion of glomerulonephritis, including persistent mild proteinuria.
INDICATIONS FOR RENAL BIOPSY IN PATIENTS WITH CSLE[12]
Increased serum creatinine without compelling alternative causes, such as sepsis, hypovolemia, or medication.
Confirmed proteinuria of 1.0 g per 24 h (either 24-h urine specimens or spot protein/creatinine ratios are acceptable).
Combinations of the following, assuming the findings are confirmed in at least 2 tests performed within a short period of time and in the absence of alternative causes: (1) Proteinuria: 0.5 g per 24 h plus hematuria, defined as 5 RBCs per hpf; and (2) Proteinuria: 0.5 g per 24 h plus cellular casts.
Renal biopsy should be reported as per the International Society of Nephrology/Renal Pathology classification (Table 1). Recent modifications of the activity and chronicity index not only help in acute management, but also help in prognostication.
Table 1.
International society of nephrology/renal pathology society 2003 classification of lupus nephritis[11,12]
| Class | Name | Light microscopy | Immunofluorescence | ||
| I | Minimal mesangial LN | Normal | Mesangial immune deposits | ||
| II | Mesangial proliferative LN | Mesangial hypercellularity or mesangial matrix expansion | Mesangial immune deposits | ||
| III | Focal LN | A | Active lesions | Segmental, or global glomerulonephritis (< 50% of glomeruli) | Diffuse subendothelial immune deposits |
| A/C | Active and chronic lesions | ||||
| C | Chronic lesions | ||||
| IV | Diffuse LN | A | Active lesions | Segmental, or global glomerulonephritis LN (> 50% glomeruli) | Diffuse subendothelial immune deposits |
| A/C | Active and chronic lesions | ||||
| C | Chronic lesions | ||||
| V | Membranous LN | Global or segmental subepithelial immune deposits | |||
| VI | Advanced sclerosing LN | LN (> 90% globally Sclerosed glomeruli without residual activity) | |||
Class V may occur in combination with class III or IV, in which case both will be diagnosed. LN: Lupus nephritis.
TREATMENT
Originally SLE nephritis was treated by steroids with a poor outcome which improved markedly with the introduction of cyclophosphamide. The first controlled trial reporting the short-term efficacy of cyclophosphamide for lupus nephritis in adults was published in 1971[13]. Initially this combination was advocated for a prolonged period, but unfortunately the improved outcome was found to be associated with long-term side effects, which resulted in a further search for a less toxic, but equally effective regime. Most of the studies have been performed in adults and to a large extent the current recommendations are borrowed heavily from adult studies. The current therapeutic strategy for SLE nephritis distinguishes two distinct phases of treatment. The first phase is INDUCTION therapy which aims to control disease activity by inducing remission of disease flare (which may be the initial presentation or represent a new flare). It is at this point that potential organ-threatening and/or life-threatening disease needs to be aggressively treated. The second phase is MAINTENANCE, wherein the target is to avoid relapses and control the disease by limiting inflammation and damage.
Class I/II LN are milder and generally do not require immunosuppressive treatment, whereas class III /IV needs to be treated aggressively[14]. Research studies over the last decade have shown increasing evidence of the efficacy of mycophenolate mofetil (MMF)/azathioprine (AZA) with a better side effect profile as compared to cyclophosphamide (CyC). Despite this, as shown by the recently conducted consensus meeting of pediatric rheumatologists and nephrologists in North America, the majority still prefer CyC as the induction agent[15]. Most of the studies on the use of MMF in children have only been case series. The largest series included 31 children or young people who were treated with MMF (either initially or switched from AZA) and showed that 73% had a good response without any recorded major side-effects[16]. Among the multiple adult studies, the first comparative study on MMF compared with CyC was published in Hong Kong in 2000[17]. MMF and CyC showed similar rates of improvement and of complete remission, 81% and 76%, respectively. Patients experienced fewer side-effects with MMF treatment. Subsequently Contreras et al[18], studied 59 adults with lupus nephritis who were initially treated with 4-7 mo infusions of CyC and then randomized to quarterly infusions of CyC or oral MMF or AZA. Patients treated with AZA or MMF showed fewer flares than those treated with CyC, six, three, and eight flares, respectively. Patients treated with MMF experienced fewer side-effects than those treated with CyC except for an increased risk of gastrointestinal symptoms and diarrhea with MMF. To date, the biggest study, the aspreva lupus management study (ALMS) attempted to determine the efficacy of MMF as an induction agent for LN. The study included 370 patients with class III through V lupus nephritis[19] and consisted of one 24-wk induction phase and thereafter a 3-year maintenance phase. The results did not show any difference between the percentages of patients responding to treatment (56.2% in the MMF group, and 53.0% in the CyC group). There was also no significant difference in the rate of side-effects and a tendency for more severe adverse events in the MMF group (P = 0.07). In a sub-analysis of the ALMS, Isenberg et al[20] showed that response varied with race, in that Black and Hispanic patients responded better to MMF (60.4%) compared to CyC (38.5%), P = 0.03. In a recently published meta-analysis, Touma et al[21] looked at the cumulative evidence for MMF/CyC as induction treatment. Four trials with 668 patients were included and no difference in clinical efficacy was found between the two drugs. MMF did, however, show significantly less alopecia (RR = 5.77; 95%CI: 1.56-21.38), but other side-effects were not significantly different. Researchers have also studied patients with class V nephritis (i.e., a membranous pattern on kidney biopsy) and found no differences between the MMF and CyC-treated groups[22]. Based on these studies, the ACR has published their recommendation on SLE nephritis, albeit targeted primarily towards the adult population.
ACR recommendation
As per the ACR recent recommendation for class III/IV LN, MMF and glucocorticoids (GC) can be used as induction agents for African-American and Hispanic patients, whereas Cyc and GC remain the first choice for White populations. MMF and GC are agents of choice in isolated class V LN[10]. In mixed cases such as class V with III or IV LN, the treatment should be similar to that for class III/IV LN. Other induction modalities that can be tried in refractory cases include intravenous immunoglobulin, plasma exchange and B-lymphocyte depletion agents such as Rituximab[23,24] (Figures 1 and 2).
Figure 1.
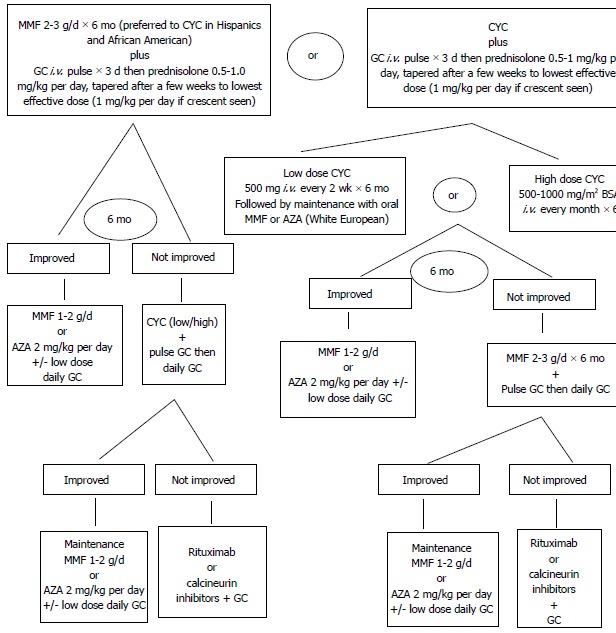
Class III/IV lupus nephritis induction therapy. MMF: Mycophenolate mofetil; CYC: Cyclophosphamide; GC: Glucocorticoids; iv: Intravenous; AZA: Azathioprine; BSA: Body surface area.
Figure 2.
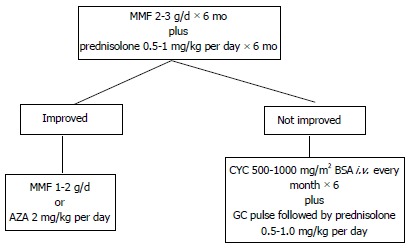
Treatment of class V without proliferative changes and with nephrotic range proteinuria (> 3 g/24 h). MMF: Mycophenolate mofetil; AZA: Azathioprine; CYC: Cyclophosphamide; GC: Glucocorticoids.
The ACR recommends either MMF or AZA and low dose steroid for the maintenance phase. MMF has been shown to be statistically better than AZA in terms of time to treatment failure (a composite including death, end stage renal disease, doubling of serum creatinine, and renal flare)[25].
In patients who fail to respond after 6 mo of treatment with GC plus MMF or CyC, the ACR recommend a switch of immunosuppressive agent from either CyC to MMF or from MMF to CyC, and these changes are accompanied by IV pulses of GCs.
Adherence
Non-adherence to immunosuppressive agents can be common in the adolescent age group[14], resulting in relapse of symptoms and sometimes an acute presentation with renal failure after initial successful treatment. Intravenous agents, such as CyC or rituximab can be considered in this situation, to ensure adherence and disease control.
RECENT ADVANCES IN SLE MEDICATIONS
Despite advances in treatment, mortality related to SLE nephritis has been static over the last decade and morbidity continues to be a major factor. Hence, there is a strong need for more effective drugs with, if possible, fewer side-effects. Studies are particularly required in children, as due to a lack of pediatric studies drugs trialed on adults are still been tried in children with severe lupus nephritis. We will discuss some of the newer medicines, however, most of the evidence on these medications is restricted to adult literature.
Rituximab
Rituximab, a chimeric antibody targeting CD20-positive cells, was first used by Tullus[26] in 2000 in a girl with class V lupus nephritis and therapy-resistant nephrotic syndrome. The therapeutic response was remarkable and her proteinuria improved so much that her serum albumin normalized. Many other clinicians have had similar clinical experiences and several case series have published positive results[14,27]. Unfortunately the first randomized controlled trial, EXPLORER, which included 237 patients with moderate to severe extra-renal lupus did not find any difference between rituximab and placebo[28]. Another large randomized placebo-controlled study on rituximab, the LUNAR trial[29], which included 144 patients with class III or IV lupus nephritis showed that only 30.6% of the patients in the placebo group and 25.4% of the rituximab-treated patient fulfilled the criteria for a complete response. Greater improvements in complement levels (P = 0.025) and antibodies to dsDNA (P = 0.007) were recorded in the rituximab group compared to the placebo group[30].
Belimumab
Belimumab is a fully humanized monoclonal antibody that binds to soluble B-lymphocyte stimulator (BLyS) and acts as a specific inhibitor of its biological activity. BLyS, also known as B-cell activating factor (BAFF) is an immunomodulatory cytokine that promotes B-cell survival, B-cell differentiation, and immunoglobulin class switching. A phase III randomized double-blind placebo controlled study showed significant benefit, but to date, there is not enough data to recommend its use in children with lupus nephritis[31].
Ocrelizumab
Ocrelizumab is a fully humanized antibody that targets CD20-positive B cells. It is a “next-generation rituximab” and the potential problem of human anti-chimeric antibody development is hopefully ameliorated. The BELONG study, 2010 was set up to study the efficacy of ocrelizumab in 381 patients with lupus nephritis[32] and the results are awaited.
Epratuzumab
Epratuzumab is a monoclonal antibody against CD22, another B-cell-specific surface antigen. Early open data in a few patients have shown positive results[33]. A study involving 227 patients found that a dose of 600 mg weekly was associated with greater british isles lupus activity grading improvement[34].
Tocilizumab
Tocilizumab is a humanized monoclonal antibody against the interleukin-6 receptor. In a phase I study of 16 patients with mild to moderate lupus, tocilizumab was found to be well tolerated, significantly reducing plasma cells and dsDNA suggesting a good clinical response[35]. Further studies seem warranted.
Abetimus
Abetimus is an immunomodulating agent designed to induce tolerance in B cells directed against dsDNA and to reduce anti-dsDNA levels. It is a synthetic molecule consisting of four double-stranded oligodeoxyribonucleotides attached to non-immunogenic polyethylene glycol. Abetimus works through the formation and clearance of drug antibody complexes and by tolerating anti-dsDNA specific B cells. Cardiel et al[36], 2008 in a 22-mo study of 317 patients showed that abetimus failed to prolong time to flare compared to the placebo.
Atacicept
Atacicept is a receptor analogue that binds both BAFF and a proliferation-inducing ligand to related members of the tumor necrosis factor superfamily. A phase II study of atacicept showed a marked reduction in B cells and immunoglobulin levels and a short term side-effect profile similar to placebo[37].
Rigeromid
Rigerimod is a spliceosomal peptide that is recognized by CD4+ T cells from patients with lupus, but not from those with other autoimmune diseases. In a 12-wk study, 150 patients with lupus and high SLE Disease Activity Index scores (Safety of estrogens in lupus erythematosus national assessment) were given three infusions of two different doses of rigerimod or placebo followed by 12 wk of observation. The treatment seemed to be well tolerated and a statistically significant reduction in disease activity was recorded[38]. Longer-term studies are needed.
Abatacept
Abatacept is a fusion protein composed of an immunoglobulin fused to the extracellular domain of CTLA-4, a molecule capable of binding B7 which selectively modulates the CD80/CD86:CD28 co-stimulatory signal. A recent 12-mo double-blind placebo-controlled study in 118 lupus patients failed to meet the primary end point of a reduction in new flares[39]. Serious adverse events were higher in the abatacept group compared with the placebo group (20% vs 7%).
Infliximab
The use of infliximab in lupus has been surrounded with major worries. Long-term use of infliximab in lupus patients can cause severe side-effects, including severe infections and even cerebral lymphoma[40].
ADJUNCTIVE TREATMENTS
The ACR recommended that all SLE patients with nephritis be treated with a background of hydroxychloroquine (HCQ), unless there is a contraindication[11]. HCQ treatment may reduce the risk of renal damage and clotting events in SLE[41-43]. Medications to control high blood pressure (anti-hypertensive), fluid overload (diuretics), proteinuria (angiotensin converting enzyme inhibitors), hypercoagulability (aspirin or other anticoagulants) and lipid control (statins)[22,44,45] are mainstays of adjunctive treatment. Dietary restriction may be necessary in terms of sodium, protein and calories. Unlike adults, these recommendations must be adjusted to take into account the growth and developmental status of the child. Infection is the most common cause of death in cSLE due to immune suppression[46]. Infections can be difficult to differentiate from a flare of SLE disease activity. C-reactive protein monitoring can be useful as most SLE patients have normal levels, except during inter-current infections.
RECOMMENDED MONITORING OF LUPUS NEPHRITIS
SLE is a chronic disease with the possibility of frequent flare-ups. Hence, these children need to be followed up regularly (Table 2). Compliance can be a major issue and needs to be addressed during each clinic visit[47].
Table 2.
Monitoring schedule for systemic lupus erythematosus nephritis[10]
| Stage of disease | Blood pressure | Urinalysis | Protein/creatinine ratio | Serum creatinine | C3/C4 level | Anti-DNA |
| Active nephritis at onset of treatment | 1 | 1 | 1 | 1 | 2 | 3 |
| Previous active nephritis, none currently | 3 | 3 | 3 | 3 | 3 | 6 |
| No prior or current nephritis | 3 | 6 | 6 | 6 | 6 | 6 |
CONCLUSION
In conclusion, the outcome of lupus nephritis is primarily dependent on histological classification at presentation. Early renal biopsy in all children with features of lupus nephritis to decide on induction therapy, aggressive treatment of hypertension and other adjunct therapy is recommended to improve mortality and morbidity of such patients.
Footnotes
P- Reviewers: Martins LSS, Pedersen EB, Sheashaa HA, Tanaka H S- Editor: Gou SX L- Editor: Webster JR E- Editor: Wu HL
References
- 1.Kamphuis S, Silverman ED. Prevalence and burden of pediatric-onset systemic lupus erythematosus. Nat Rev Rheumatol. 2010;6:538–546. doi: 10.1038/nrrheum.2010.121. [DOI] [PubMed] [Google Scholar]
- 2.Malleson PN, Fung MY, Rosenberg AM. The incidence of pediatric rheumatic diseases: results from the Canadian Pediatric Rheumatology Association Disease Registry. J Rheumatol. 1996;23:1981–1987. [PubMed] [Google Scholar]
- 3.Huang JL, Yao TC, See LC. Prevalence of pediatric systemic lupus erythematosus and juvenile chronic arthritis in a Chinese population: a nation-wide prospective population-based study in Taiwan. Clin Exp Rheumatol. 2004;22:776–780. [PubMed] [Google Scholar]
- 4.Baqi N, Moazami S, Singh A, Ahmad H, Balachandra S, Tejani A. Lupus nephritis in children: a longitudinal study of prognostic factors and therapy. J Am Soc Nephrol. 1996;7:924–929. doi: 10.1681/ASN.V76924. [DOI] [PubMed] [Google Scholar]
- 5.Hochberg MC. Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 1997;40:1725. doi: 10.1002/art.1780400928. [DOI] [PubMed] [Google Scholar]
- 6.Petri M, Orbai AM, Alarcón GS, Gordon C, Merrill JT, Fortin PR, Bruce IN, Isenberg D, Wallace DJ, Nived O, et al. Derivation and validation of the Systemic Lupus International Collaborating Clinics classification criteria for systemic lupus erythematosus. Arthritis Rheum. 2012;64:2677–2686. doi: 10.1002/art.34473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Levy DM, Kamphuis S. Systemic lupus erythematosus in children and adolescents. Pediatr Clin North Am. 2012;59:345–364. doi: 10.1016/j.pcl.2012.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bernatsky S, Boivin JF, Joseph L, Manzi S, Ginzler E, Gladman DD, Urowitz M, Fortin PR, Petri M, Barr S, et al. Mortality in systemic lupus erythematosus. Arthritis Rheum. 2006;54:2550–2557. doi: 10.1002/art.21955. [DOI] [PubMed] [Google Scholar]
- 9.Alarcón GS, McGwin G, Petri M, Reveille JD, Ramsey-Goldman R, Kimberly RP. Baseline characteristics of a multiethnic lupus cohort: PROFILE. Lupus. 2002;11:95–101. doi: 10.1191/0961203302lu155oa. [DOI] [PubMed] [Google Scholar]
- 10.Dooley MA, Aranow C, Ginzler EM. Review of ACR renal criteria in systemic lupus erythematosus. Lupus. 2004;13:857–860. doi: 10.1191/0961203304lu2023oa. [DOI] [PubMed] [Google Scholar]
- 11.Hahn BH, McMahon MA, Wilkinson A, Wallace WD, Daikh DI, Fitzgerald JD, Karpouzas GA, Merrill JT, Wallace DJ, Yazdany J, et al. American College of Rheumatology guidelines for screening, treatment, and management of lupus nephritis. Arthritis Care Res (Hoboken) 2012;64:797–808. doi: 10.1002/acr.21664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weening JJ, D’Agati VD, Schwartz MM, Seshan SV, Alpers CE, Appel GB, Balow JE, Bruijn JA, Cook T, Ferrario F, et al. The classification of glomerulonephritis in systemic lupus erythematosus revisited. J Am Soc Nephrol. 2004;15:241–250. doi: 10.1097/01.asn.0000108969.21691.5d. [DOI] [PubMed] [Google Scholar]
- 13.Steinberg AD, Kaltreider HB, Staples PJ, Goetzl EJ, Talal N, Decker JL. Cyclophosphamide in lupus nephritis: a controlled trial. Ann Intern Med. 1971;75:165–171. doi: 10.7326/0003-4819-75-2-165. [DOI] [PubMed] [Google Scholar]
- 14.Marks SD, Tullus K. Modern therapeutic strategies for paediatric systemic lupus erythematosus and lupus nephritis. Acta Paediatr. 2010;99:967–974. doi: 10.1111/j.1651-2227.2010.01771.x. [DOI] [PubMed] [Google Scholar]
- 15.Mina R, von Scheven E, Ardoin SP, Eberhard BA, Punaro M, Ilowite N, Hsu J, Klein-Gitelman M, Moorthy LN, Muscal E, et al. Consensus treatment plans for induction therapy of newly diagnosed proliferative lupus nephritis in juvenile systemic lupus erythematosus. Arthritis Care Res (Hoboken) 2012;64:375–383. doi: 10.1002/acr.21558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kazyra I, Pilkington C, Marks SD, Tullus K. Mycophenolate mofetil treatment in children and adolescents with lupus. Arch Dis Child. 2010;95:1059–1061. doi: 10.1136/adc.2009.178608. [DOI] [PubMed] [Google Scholar]
- 17.Chan TM, Li FK, Tang CS, Wong RW, Fang GX, Ji YL, Lau CS, Wong AK, Tong MK, Chan KW, et al. Efficacy of mycophenolate mofetil in patients with diffuse proliferative lupus nephritis. Hong Kong-Guangzhou Nephrology Study Group. N Engl J Med. 2000;343:1156–1162. doi: 10.1056/NEJM200010193431604. [DOI] [PubMed] [Google Scholar]
- 18.Contreras G, Pardo V, Leclercq B, Lenz O, Tozman E, O’Nan P, Roth D. Sequential therapies for proliferative lupus nephritis. N Engl J Med. 2004;350:971–980. doi: 10.1056/NEJMoa031855. [DOI] [PubMed] [Google Scholar]
- 19.Appel GB, Contreras G, Dooley MA, Ginzler EM, Isenberg D, Jayne D, Li LS, Mysler E, Sánchez-Guerrero J, Solomons N, et al. Mycophenolate mofetil versus cyclophosphamide for induction treatment of lupus nephritis. J Am Soc Nephrol. 2009;20:1103–1112. doi: 10.1681/ASN.2008101028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Isenberg D, Appel GB, Contreras G, Dooley MA, Ginzler EM, Jayne D, Sánchez-Guerrero J, Wofsy D, Yu X, Solomons N. Influence of race/ethnicity on response to lupus nephritis treatment: the ALMS study. Rheumatology (Oxford) 2010;49:128–140. doi: 10.1093/rheumatology/kep346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Touma Z, Gladman DD, Urowitz MB, Beyene J, Uleryk EM, Shah PS. Mycophenolate mofetil for induction treatment of lupus nephritis: a systematic review and metaanalysis. J Rheumatol. 2011;38:69–78. doi: 10.3899/jrheum.100130. [DOI] [PubMed] [Google Scholar]
- 22.Radhakrishnan J, Moutzouris DA, Ginzler EM, Solomons N, Siempos II, Appel GB. Mycophenolate mofetil and intravenous cyclophosphamide are similar as induction therapy for class V lupus nephritis. Kidney Int. 2010;77:152–160. doi: 10.1038/ki.2009.412. [DOI] [PubMed] [Google Scholar]
- 23.Terrier B, Amoura Z, Ravaud P, Hachulla E, Jouenne R, Combe B, Bonnet C, Cacoub P, Cantagrel A, de Bandt M, et al. Safety and efficacy of rituximab in systemic lupus erythematosus: results from 136 patients from the French AutoImmunity and Rituximab registry. Arthritis Rheum. 2010;62:2458–2466. doi: 10.1002/art.27541. [DOI] [PubMed] [Google Scholar]
- 24.Wright EC, Tullus K, Dillon MJ. Retrospective study of plasma exchange in children with systemic lupus erythematosus. Pediatr Nephrol. 2004;19:1108–1114. doi: 10.1007/s00467-004-1552-7. [DOI] [PubMed] [Google Scholar]
- 25.Dooley MA, Jayne D, Ginzler EM, Isenberg D, Olsen NJ, Wofsy D, Eitner F, Appel GB, Contreras G, Lisk L, et al. Mycophenolate versus azathioprine as maintenance therapy for lupus nephritis. N Engl J Med. 2011;365:1886–1895. doi: 10.1056/NEJMoa1014460. [DOI] [PubMed] [Google Scholar]
- 26.Tullus K. New developments in the treatment of systemic lupus erythematosus. Pediatr Nephrol. 2012;27:727–732. doi: 10.1007/s00467-011-1859-0. [DOI] [PubMed] [Google Scholar]
- 27.Marks SD, Tullus K. Targeted B-cell depletion therapy in childhood-onset systemic lupus erythematosus: progress to date. Paediatr Drugs. 2007;9:371–378. doi: 10.2165/00148581-200709060-00004. [DOI] [PubMed] [Google Scholar]
- 28.Merrill JT, Neuwelt CM, Wallace DJ, Shanahan JC, Latinis KM, Oates JC, Utset TO, Gordon C, Isenberg DA, Hsieh HJ, et al. Efficacy and safety of rituximab in moderately-to-severely active systemic lupus erythematosus: the randomized, double-blind, phase II/III systemic lupus erythematosus evaluation of rituximab trial. Arthritis Rheum. 2010;62:222–233. doi: 10.1002/art.27233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Efficacy and safety of rituximab in patients with proliferative lupus nephritis: results from the randomized, double-blind phase III LUNAR study 2010. 9th International Congress on Systemic Lupus Erythematosus, Vancouver, Canada, June 24–27, Poster PO2 E 6 [Google Scholar]
- 30.Effect of rituximab on anti-double-stranded DNA antibody and C3 levels and relationship to response: results from the LUNAR trial 2010. 9th International Congress on Systemic Lupus Erythematosus, Vancouver, Canada, June 24–27, Poster PO2 E 22 [Google Scholar]
- 31.Manzi S, Sánchez-Guerrero J, Merrill JT, Furie R, Gladman D, Navarra SV, Ginzler EM, D’Cruz DP, Doria A, Cooper S, et al. Effects of belimumab, a B lymphocyte stimulator-specific inhibitor, on disease activity across multiple organ domains in patients with systemic lupus erythematosus: combined results from two phase III trials. Ann Rheum Dis. 2012;71:1833–1838. doi: 10.1136/annrheumdis-2011-200831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mysler E, Spindler A, Guzman R, Bijl M, Jayne D, Furie R, Maciuca R, Drappa J, Shahdad S, Close D Study design and baseline patient characteristics of BELONG, the randomized double-blind, placebo-controlled phase III trial of ocrelizumab, a humanized anti-CD20 antibody, in lupus nephritis 2010. 9th International Congress on Systemic Lupus Erythematosus, Vancouver, Canada, June 24–27, Poster PO2 E 20 [Google Scholar]
- 33.Dörner T, Kaufmann J, Wegener WA, Teoh N, Goldenberg DM, Burmester GR. Initial clinical trial of epratuzumab (humanized anti-CD22 antibody) for immunotherapy of systemic lupus erythematosus. Arthritis Res Ther. 2006;8:R74. doi: 10.1186/ar1942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Available from: http://www.ucb.com/_up/ucb_com_news/document. Accessed 10 Nov 2012.
- 35.Illei GG, Shirota Y, Yarboro CH, Daruwalla J, Tackey E, Takada K, Fleisher T, Balow JE, Lipsky PE. Tocilizumab in systemic lupus erythematosus: data on safety, preliminary efficacy, and impact on circulating plasma cells from an open-label phase I dosage-escalation study. Arthritis Rheum. 2010;62:542–552. doi: 10.1002/art.27221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cardiel MH, Tumlin JA, Furie RA, Wallace DJ, Joh T, Linnik MD. Abetimus sodium for renal flare in systemic lupus erythematosus: results of a randomized, controlled phase III trial. Arthritis Rheum. 2008;58:2470–2480. doi: 10.1002/art.23673. [DOI] [PubMed] [Google Scholar]
- 37.Pena-Rossi C, Nasonov E, Stanislav M, Yakusevich V, Ershova O, Lomareva N, Saunders H, Hill J, Nestorov I. An exploratory dose-escalating study investigating the safety, tolerability, pharmacokinetics and pharmacodynamics of intravenous atacicept in patients with systemic lupus erythematosus. Lupus. 2009;18:547–555. doi: 10.1177/0961203309102803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.D’Andrea D, Xie F, Zimmer R A randomized, doubleblind, placebo-controlled study of spliceosomal peptide rigerimod in patients with systemic lupus erythematosus (SLE), 2010. 9th [Google Scholar]
- 39.Merrill JT, Burgos-Vargas R, Westhovens R, Chalmers A, D’Cruz D, Wallace DJ, Bae SC, Sigal L, Becker JC, Kelly S, et al. The efficacy and safety of abatacept in patients with non-life-threatening manifestations of systemic lupus erythematosus: results of a twelve-month, multicenter, exploratory, phase IIb, randomized, double-blind, placebo-controlled trial. Arthritis Rheum. 2010;62:3077–3087. doi: 10.1002/art.27601. [DOI] [PubMed] [Google Scholar]
- 40.Aringer M, Houssiau F, Gordon C, Graninger WB, Voll RE, Rath E, Steiner G, Smolen JS. Adverse events and efficacy of TNF-alpha blockade with infliximab in patients with systemic lupus erythematosus: long-term follow-up of 13 patients. Rheumatology (Oxford) 2009;48:1451–1454. doi: 10.1093/rheumatology/kep270. [DOI] [PubMed] [Google Scholar]
- 41.A randomized study of the effect of withdrawing hydroxychloroquine sulfate in systemic lupus erythematosus. The Canadian Hydroxychloroquine Study Group. N Engl J Med. 1991;324:150–154. doi: 10.1056/NEJM199101173240303. [DOI] [PubMed] [Google Scholar]
- 42.Fessler BJ, Alarcón GS, McGwin G, Roseman J, Bastian HM, Friedman AW, Baethge BA, Vilá L, Reveille JD. Systemic lupus erythematosus in three ethnic groups: XVI. Association of hydroxychloroquine use with reduced risk of damage accrual. Arthritis Rheum. 2005;52:1473–1480. doi: 10.1002/art.21039. [DOI] [PubMed] [Google Scholar]
- 43.Jung H, Bobba R, Su J, Shariati-Sarabi Z, Gladman DD, Urowitz M, Lou W, Fortin PR. The protective effect of antimalarial drugs on thrombovascular events in systemic lupus erythematosus. Arthritis Rheum. 2010;62:863–868. doi: 10.1002/art.27289. [DOI] [PubMed] [Google Scholar]
- 44.Kunz R, Friedrich C, Wolbers M, Mann JF. Meta-analysis: effect of monotherapy and combination therapy with inhibitors of the renin angiotensin system on proteinuria in renal disease. Ann Intern Med. 2008;148:30–48. doi: 10.7326/0003-4819-148-1-200801010-00190. [DOI] [PubMed] [Google Scholar]
- 45.Li X, Ren H, Zhang Q, Zhang W, Wu X, Xu Y, Shen P, Chen N. Mycophenolate mofetil or tacrolimus compared with intravenous cyclophosphamide in the induction treatment for active lupus nephritis. Nephrol Dial Transplant. 2012;27:1467–1472. doi: 10.1093/ndt/gfr484. [DOI] [PubMed] [Google Scholar]
- 46.Ruiz-Irastorza G, Olivares N, Ruiz-Arruza I, Martinez-Berriotxoa A, Egurbide MV, Aguirre C. Predictors of major infections in systemic lupus erythematosus. Arthritis Res Ther. 2009;11:R109. doi: 10.1186/ar2764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schmajuk G, Yazdany J. Drug monitoring in systemic lupus erythematosus: a systematic review. Semin Arthritis Rheum. 2011;40:559–575. doi: 10.1016/j.semarthrit.2010.07.010. [DOI] [PubMed] [Google Scholar]


