Abstract
Objectives
To determine the association of neighborhood socioeconomic status (SES) with bystander-initiated cardiopulmonary resuscitation (CPR) and patient outcomes of out of hospital cardiac arrests (OHCAs) in an Asian metropolitan area.
Methods
We performed a retrospective study in a prospectively collected cohort from the Utstein registry of adult non-traumatic OHCAs in Taipei, Taiwan. Average real estate value was assessed as the first proxy of SES. Twelve administrative districts in Taipei City were categorized into low versus high SES areas to test the association. The primary outcome was bystander-initiated CPR, and the secondary outcome was patient survival status. Factors associated with bystander-initiated CPR were adjusted for in multivariate analysis. The mean household income was assessed as the second proxy of SES to validate the association.
Results
From January 1, 2008 to December 30, 2009, 3573 OHCAs received prehospital resuscitation in the community. Among these, 617 (17.3%) cases received bystander CPR. The proportion of bystander CPR in low-SES vs. high-SES areas was 14.5% vs. 19.6% (p < 0.01). Odds ratio of receiving bystander-initiated CPR in low-SES areas was 0.72 (95% confidence interval: [0.60–0.88]) after adjusting for age, gender, witnessed status, public collapse, and OHCA unrecognized by the online dispatcher. Survival to discharge rate was significantly lower in low-SES areas vs. high-SES areas (4.3% vs. 6.8%; p < 0.01). All results above remained consistent in the analyses by mean household income.
Conclusions
Patients who experienced an OHCA in low-SES areas were less likely to receive bystander-initiated CPR, and demonstrated worse survival outcomes.
Keywords: Cardiopulmonary resuscitation (CPR), Emergency medical system (EMS), Education, Socioeconomic status (SES), Neighborhood, First responder
1. Introduction
Bystander-initiated cardiopulmonary resuscitation (CPR) is a vital link in the community chain-of-survival for out-of-hospital cardiac arrest (OHCA).1,2 For every 30 patients receiving bystander CPR, one additional life will be saved.1 However, the bystander CPR rate for OHCA patients remains unsatisfactory worldwide. The rate ranged from 10% to 65% in the United States,3,4 and were even lower among many Asian countries from 1.5% to 36.7%.5–9 Major barriers to laypersons’ willingness to perform bystander CPR include the fear of injuring the patient by incorrect or poor CPR performance, the physical inability of the bystander to perform CPR, legal liability, and the risk of infectious disease transmission.10–12
Previous studies have indicated that there are individual-level factors that influence the rate of bystander CPR, but the neighborhood in which the arrest occurs may also affect the rate of bystander CPR. The neighborhood factors associated with bystander CPR rates include location of collapse (public vs. private), the racial composition or educational level of residents, and socioeconomic status (SES).13–16 Sasson et al. examined the correlations between bystander CPR rates and neighborhood features, and identified higher OHCA rates and lesser provision of bystander CPR in communities with lower income, lower education level, and higher percentage of black residents.14,17,18 Recently, a large cohort study also showed lower bystander-initiated CPR in low-income black neighborhoods than those in high-income white neighborhoods.3 Identifying areas with lower rates of bystander-initiated CPR in a community could facilitate efficient delivery of CPR training courses based on local needs, and increase the overall bystander CPR rate for OHCAs. Therefore, communities are advised to conduct a surveillance to identify areas with lower rates of bystander CPR to evaluate for neighborhood effect.2
Currently the association of SES with bystander-initiated CPR has only been reported in North America. Compared to North America, Asian communities have a lower rate of bystander-initiated CPR, a less complex racial composition, and a lesser disparity between rich and poor. Whether the association between SES and bystander-initiated CPR exists universally has not been examined previously.
Using the Utstein-based registered data from an Asian metropolitan area, we conducted a study to evaluate the association between SES and bystander-initiated CPR, and to examine whether the difference of bystander CPR rate influences patient outcomes.
2. Methods
2.1. EMS setting in Taipei and Utstein-based dataset
Taipei City has a population of 2.65 million in the area of 272 km2. The metropolis is covered by fire-based, two-tiered emergency medical service (EMS) system including 39 basic life support (BLS) teams with early defibrillation capability and 4 advanced life support (ALS) teams capable and authorized to perform tracheal intubation and intravenous injections of adrenaline (epinephrine) and atropine.19,20
The Utstein-based data of Taipei EMS has been developed and modified for a quality assurance process for OHCAs since early 2000. The registry data contains the dispatch records, modes and timeliness of pre-hospital care, patients’ demographics (age, sex), arrest characteristics (witnessed status, bystander CPR, initial recorded rhythm), automated external defibrillator records, and patient outcomes from the EMS receiving hospitals, including return of spontaneous circulation (ROSC), survival to hospital admission, survival to hospital discharge, and neurologic functional status by cerebral performance category (CPC) at discharge.
2.2. Study design, study population and data collection
We conducted a retrospective study in a prospective cohort of the Utstein-based registry of Taipei EMS OHCAs. This study was designed as a descriptive analysis between SES of the twelve administrative districts in Taipei and likelihood of receiving bystander-initiated CPR. Because the record of “bystander-initiated CPR” was not required until mid-2007, data for this study was selected thereafter. The study protocol has been approved by the Institutional Review Board of the National Taiwan University Hospital.
Patients with OHCA from January 1, 2008 to December 31, 2009 registered in the Utstein-based system were enrolled. Patients without transport to hospital due to obvious death or an existing do-not-attempt-resuscitate (DNAR) orders, or OHCA with traumatic cause, or pediatric cases (<18 years old) were excluded. Data on each OHCA are collected from a combination of forms of run sheets filled out by EMS personnel who responded to the call, hospital records, and defibrillator downloads.
2.3. Measures of exposure and outcomes
2.3.1. Exposure: surrogate for socioeconomic status
We intended to study how the SES of the area affects the provision of CPR in prehospital setting. In health research, SES is viewed as a composite condition of a person according to educational attainment, mean income, occupation, wealth and so on.21 However, all the information above is not collected as a part of the cardiac arrest registry. Accurate measurement of SES is difficult in EMS research field. Therefore, literature of SES and EMS research employ surrogate measures for neighborhood SES.3,13,14,16,22
In this study, community SES is assessed by the average price of real estate in 2008 and 2009 among the 12 administrative districts in Taipei City, similar in the study by Vaillancourt et al.13 Historically, significant disparity exists between publicly announced land value by government and current assessed residential property value by market in Taiwan. As registry of the real selling price of property was implemented by Department of Land Administration only after 2012 exact price of real estate property in 2008 and 2009 was not available. Therefore, we estimated the price of real estate during the study period by averaging announced property values from two major real estate agencies in Taiwan.
2.3.2. Outcomes rates of bystander-initiated CPR and cardiac arrest survival
We defined two outcomes of interest: the provision of bystander CPR and survival of patients with OHCA. The primary outcome was the rate of bystander CPR as obtained from the web-based Utstein-based registry system in Taipei during the study period. Bystander CPR on EMS arrival was recorded by EMS personnel on ambulance run sheet for every OHCA. Secondary outcomes were the survival status of patients, including sustained ROSC (longer than 2 h), survival to hospital discharge, and favorable neurological outcome of survivors defined by cerebral performance category (CPC) scale 1 and 2.
2.4. Validation by a second proxy of SES: the mean household income
To verify the association of bystander CPR and community SES as defined by average real estate price, the analyses were repeated using a second proxy of SES, the mean household income in 2008 and 2009 among the 12 administrative districts in Taipei City. The values of mean household income, annually reported by Department of Budget, Accounting and Statistics, Taipei City Government through cluster sampling of Taipei citizens, represented the finical status at home-level in the area, and has been commonly used as a proxy of neighborhood effect in previous studies.3,16
2.5. Statistical analysis
Mean and standard deviation (S.D.) were calculated as summaries of the continuous variables. For categorical variables, number and percentage were computed. Unpaired Student’s t-tests were used for comparisons of continuous variables, and binominal variables were analyzed with Chi-square or Fisher’s exact tests, as appropriate. Linear regression was applied to examine the correlation between ranks of SES and rates of bystander-initiated CPR at the district level. Logistic regression and stratification were utilized for multivariate analysis and examination of interactions of variables. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated and two-tailed p-values of <0.05 were considered significant. Data were entered, processed and analyzed using SAS software version 9.2 (SAS Institute, Cary, NC).
3. Results
3.1. Category of high- versus low-SES areas
The first surrogate for SES to test the association with bystander-initiated CPR is the average price of real estate in year 2008 and 2009 in every administrative district. During the study period, average price of real property was 184,374 NTD m−2 (around 6146 USD m−2) among 12 administrative districts in Taipei City. Districts with price higher than the average were defined as high-SES areas (i.e. 6 districts A, B, C, D, E, F, range of price from 9715 USD m−2 to 6756 USD m−2), while those with the price below the level were viewed as low-SES areas (i.e. 6 districts, G, H, I, J, K, L, range of price from 5163 USD m−2 to 3963 USD m−2).
The second surrogate for SES to validate the association with bystander-initiated CPR is the mean household income in year 2008 and 2009 in every administrative district. Average household income was 1,599,000 NTD (around 53,300 USD) among 12 administrative districts in Taipei City during the period. Districts with the mean household income above the average were categorized into high-SES areas (i.e. 6 districts, A, E, C, H, D, B, ranging from 64,500 USD to 54,333 USD), while the others were categorized into low-SES areas (i.e. 6 districts, L, K, F, I, G, J, ranging from 53,200 USD to 41,500 USD).
3.2. Enrollment and patient characteristics
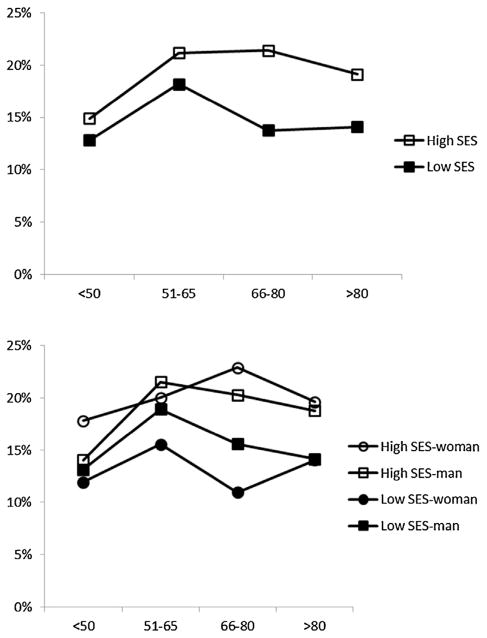
From January 1, 2008 to December 31, 2009, there were total 5525 OHCA cases activating EMS, and 3991 of them with attempted resuscitation by EMS personnel at scene. Excluded traumatic death and pediatric patients, 3573 OHCAs cases were enrolled in final analyses. Mean age was 73.0 ± 16.0 years old and 2226 (62.3%) were male. Only 617 cases (17.3%) received bystander-initiated CPR. The participant flow and SES status defined by average real estate price (high vs. low) included in final analyses were shown in Fig. 1.
Fig. 1.
Patient flow and study. OHCA: out-of-hospital cardiac arrest; N: number; CPR: cardiopulmonary resuscitation; SES: socioeconomic status.
3.3. Disparity of bystander-initiated CPR among various SES areas defined by average real estate price in Taipei City
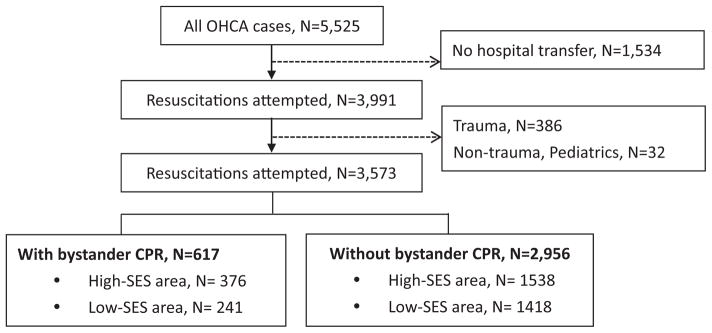
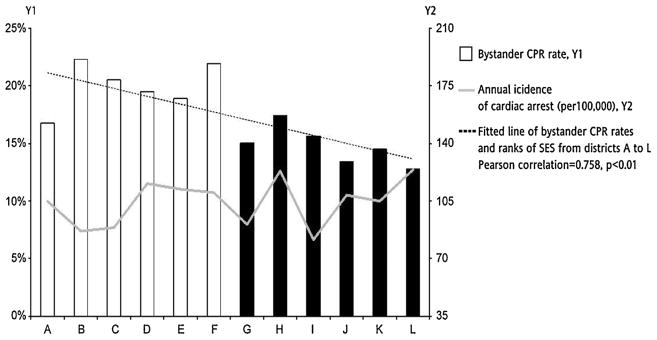
The incidence of patients with adult non-traumatic OHCA and the rates of receiving bystander-initiated CPR among the 12 districts in Taipei were illustrated in Fig. 2. Districts were ranked from the highest (District A) to the lowest (District L) according to the average residential property price. Bystander-initiated CPR rates among high-SES areas (white bars; average 19.6%) were significantly higher than those in low-SES areas (black bars; average 14.5%). At the district level, there was a significant linear correlation between bystander CPR and SES ranking, with Pearson correlation 0.76. However, district SES did not correlate with incidence of OHCAs. Furthermore, stratified analyses of bystander-initiated CPR rates according to age and gender in high-SES areas versus low-SES areas demonstrated consistent disparity, as shown in Fig. 3.
Fig. 2.
Annual incidence of cardiac arrest (per 100,000) and rate of bystander-initiated CPR among 12 districts in Taipei City.
Fig. 3.
Stratified bystander-initiated CPR rate according to SES, age, and gender. Note: “High SES-woman” represents the percentage of arrest women victims who had received bystander CPR in areas defined as high socioeconomic status.
3.4. Primary and secondary outcomes
Baseline characteristics of OHCAs with and without bystander-CPR were listed in Table 1. In univariate analyses, primary outcome (i.e. receiving bystander-initiated CPR) was significantly associated with witnessed status, collapse in public locations, collapse in high-SES areas, OHCA recognized by online dispatcher, and response time of EMS. All secondary outcomes (i.e. patient survival status) were significantly better in OHCAs with bystander CPR.
Table 1.
OHCAs with versus without bystander-initiated CPR.
| Characteristics | Case numbers | With bystander CPR | Without bystander CPR | p-Value |
|---|---|---|---|---|
| OHCA patients – N (%) | 3573 | 617 | 2956 | |
| Age (years) (Mean ± SD) | 73.0 ± 16.0 | 72.9 ± 15.6 | 73.0 ± 16.1 | 0.96 |
| Male | 2226 (62.3%) | 387 (62.7%) | 1839 (62.2%) | 0.82 |
| Witnessed collapse | 1012 (28.3%) | 352 (57.1%) | 660 (22.3%) | <0.01 |
| Collapse in public | 684 (19.1%) | 210 (34.0%) | 474 (16.0%) | <0.01 |
| Lower SES | 1659 (46.4%) | 241 (14.5%) | 1418 (47.8%) | <0.01 |
| OHCA unrecognized by online dispatcher – N (%) | 1779 (49.8%) | 206 (33.4%) | 1573 (53.2%) | <0.01 |
| EMS intervals (min) (mean ± SD) | ||||
| Response time | 6.4 ± 3.3 | 7.0 ± 3.8 | 6.3 ± 3.2 | <0.01 |
| Scene time | 13.0 ± 5.6 | 13.2 ± 5.7 | 13.0 ± 5.6 | 0.54 |
| Transport time | 4.5 ± 2.8 | 4.3 ± 2.7 | 4.5 ± 2.8 | 0.08 |
| Survival status – N (%) | ||||
| Sustained ROSC | 933 (26.1%) | 192 (31.1%) | 741 (25.1%) | <0.01 |
| Survival to discharge | 197 (5.5%) | 55 (8.9%) | 142 (4.8%) | <0.01 |
| CPC1 and 2 | 124 (3.5%) | 35 (5.7%) | 89 (3.0%) | <0.01 |
N, number; CPR, cardiopulmonary resuscitation; OHCA, out-of-hospital cardiac arrest; SD, standard deviation; EMS, emergency medical service; ROSC, return of spontaneous circulation; CPC, cerebral performance category.
We tabulated the baseline data of OHCAs that occurred in high-SES versus low-SES districts in Table 2 to explore the factors affecting bystander-initiated CPR and patient outcomes. Patients with OHCA in high-SES areas were more likely to receive bystander-initiated CPR, to have the OHCA recognized by the online dispatcher, as well as shorter EMS response time and transport time. Although the difference in EMS time intervals might have influenced the secondary outcomes, it was apparently not related to the primary outcomes.
Table 2.
OHCAs occurring in high-SES versus low-SES districts.
| Characteristics | ALL | High SES | Low SES | p-Value |
|---|---|---|---|---|
| OHCA patients – N (%) | 3573 | 1914 | 1659 | |
| Age (years) (mean ± SD) | 73.0 ± 16.0 | 72.9 ± 16.3 | 73.0 ± 15.7 | 0.93 |
| Male | 2226 (62.3%) | 1188 (62.1%) | 1038 (62.6%) | 0.76 |
| Witnessed collapse | 1012 (28.3%) | 558 (29.2%) | 454 (27.4%) | 0.24 |
| EMS intervals (min) (mean ± SD) | ||||
| Response time | 6.4 ± 3.3 | 6.3 ± 3.2 | 6.5 ± 3.4 | 0.049 |
| Scene time | 13.0 ± 5.6 | 13.7 ± 5.6 | 12.3 ± 5.5 | <0.01 |
| Transportation time | 4.5 ± 2.8 | 4.1 ± 2.6 | 5.0 ± 2.9 | <0.01 |
| Total pre-hospital time | 23.9 ± 6.4 | 24.0 ± 6.3 | 23.8 ± 6.6 | 0.23 |
| OHCA unrecognized by online dispatcher – N (%) | 1779 (49.8%) | 869 (45.4%) | 910 (54.9%) | <0.01 |
| Outcomes – N (%) | ||||
| Bystander CPR | 617 (17.3%) | 376 (19.6%) | 241 (14.5%) | <0.01 |
| Sustained ROSC | 933 (26.1%) | 542 (28.4%) | 391 (23.6%) | <0.01 |
| Survival to discharge | 197 (5.5%) | 128 (6.8%) | 69 (4.3%) | <0.01 |
| CPC1 and 2 | 124 (3.5%) | 74 (3.9%) | 50 (3.1%) | 0.18 |
N, number; CPR, cardiopulmonary resuscitation; OHCA, out-of-hospital cardiac arrest; SD, standard deviation; EMS, emergency medical service; ROSC, return of spontaneous circulation; CPC, cerebral performance category.
Multivariate analysis of factors affecting bystander CPR, including age, gender, SES, recognized by online dispatcher, witnessed status, and location of collapse (public vs. private) were illustrated in Fig. 4. The association between SES and bystander-initiated CPR remained significant, with OR: 0.72; 95% CI [0.60–0.88].
Fig. 4.

Adjusted odds ratios of receiving bystander-initiated CPR.
3.5. Validation by mean household income as the second proxy of SES
Primary and secondary analyses using mean household income as the second proxy of SES yielded similar results. There was fewer bystander-initiated CPR in low (274/1738, 15.8%) vs. high-SES districts (343/1835, 18.7%) (p < 0.05). The Pearson correlation between district bystander CPR and SES ranking was 0.43. In multivariate analysis adjusted by the same variables in primary analysis, low SES still significantly associated with low bystander-initiated CPR rate, with OR 0.82 (95% CI 0.68–0.99). Survival to discharge of patients with OHCA was also lower in low-SES areas versus high-SES areas (4.7% vs. 6.6%; p < 0.05).
4. Discussion
In this study, we found that areas with low SES in Taipei City were strongly associated with lower rates of bystander-initiated CPR and worse patient outcomes following OHCAs as compared to those occurring in high-SES areas. This association remained consistent after multivariate analyses and by a second proxy of SES. To our best knowledge, the association between SES and bystander CPR has not been investigated outside the North American communities before. Our study suggests that the association may be a universal phenomenon.
Identifying the disparities in the rate of bystander CPR rates in a given community is important for EMS system design. Several studies conducted in the North American communities have attempted to measure the effects of SES on the provision of bystander CPR. One Canadian by Vaillancourt et al. found that when cardiac arrests occurred at a private site, probability of receiving bystander CPR was lower in a low-SES area.13 A report from the Cardiac Arrest Registry to Enhance Survival (CARES) by Sasson et al. declared that OHCAs in low-income black neighborhoods were less likely to receive bystander-initiated CPR than those in high-income neighborhoods.3 In North America, the disparity in bystander CPR and patient outcomes between high- and low-SES communities could be explained by two reasons. First, the educational messages about bystander CPR are not getting across in these areas due to the complexity of racial composition or language barrier.10 Second, the lower bystander CPR rate in low-SES areas may be a product of distrust of local government authority, especially if the bystanders fear contacting the police or wish to avoid involvement in the situation.23
Conducted in an Asian metropolitan area, our study demonstrated the consistent results with previous studies from North America. The study population has less complex racial composition and fewer foreign immigrants. The disparity of accessibility of bystander-initiated CPR and outcomes for patients with OHCA in high-SES versus low-SES neighborhood in this study may arise from three possible causes. First, more patients with OHCA in low-SES neighborhood might have been initially viewed as drunkard or vagrants resting at roadside, rendering less bystander-initiated CPR. Second, responses of dispatchers toward calls from low-versus high-SES neighborhoods were inconsistent, leading to more OHCAs unrecognized by dispatchers (i.e. low- vs. high-SES: 54.9% vs. 45.4%; p < 0.01), and lesser chance of subsequent dispatcher-assisted bystander-initiated CPR. Therefore, it is possible that optimizing dispatcher responses for detecting possible OHCAs by interview with callers from low-SES areas could increase the rate of bystander CPR with dispatcher assistance. Third, the destination hospitals might also influence patient outcomes. In Taipei, there are less tertiary hospitals in the districts categorized as low SES (i.e. high SES vs. low SES: 8 vs. 3), and this may in tern affect the degree of ED and post-resuscitation care after ROSC.
This study provided insights to promote bystander-initiated CPR in the future. Although general large-scale CPR training remains a popular strategy worldwide, training directed to targeted communities with lower bystander CPR rate might improve the likelihood of survival efficiently.2,10 A longitudinal study from Sweden found that trained rescuers doubled the provision of bystander CPR, from 31% to 55%, over the course of two decades.24 A report from Japan supported these findings, reporting that bystanders who had received previous CPR training were 3.40 times (95% CI = [1.31–8.85]) more likely to perform CPR compared to those without previous CPR training.25 However, a prospective study with individual data found that only a minority of CPR-trained bystanders actually performed CPR at scene.11 Furthermore, training unselected laypersons in CPR/defibrillation is costly compared with other public health initiatives.26 CPR/defibrillation training yielded 2.7 quality-adjusted hours of life at the cost of $62 per trainee ($202,400 per quality-adjusted life-year [QALY] gained). Training laypersons in CPR/defibrillation with subsequent defibrillator purchase cost $2,489,700 per QALY.26 Therefore, EMS providers should consider CPR training for laypersons in selected communities, especially in low-SES areas as suggested in our study, for the most efficient training.
5. Limitations of this study
There are three limitations in our study. First, the study was an analysis of OHCA registry without individual bystander data. Robust causal inference between circumstantial factors and the willingness to perform CPR was impossible under this study design. However, the associations found in this study were strong and persistent even after multivariate adjustment and by using the second maker of SES. Findings in this pilot study indicated further intensive epidemiologic research to clarify the plausibility. Second, using price of real estate as a surrogate for SES might not be adequate to capture the many facets of SES. As a predictor of health outcomes, SES is often conceptualized as a complex composite of education, employment, income, and wealth.21 However, it is extremely difficult to employ multi-measures of SES due to availability of relevant data. The use of real-estate value, as adopted in previous literature,13 was an acceptable surrogate in analysis, and the results remained consistent even by using another surrogate (mean household income). Of course, the effect of SES could be estimated more accurately if more individual data were available. Finally, the data was community-based obtained in a single city for 2 years. Novel findings in this study needs to be validated in a more long-term and large-scale research.
6. Conclusion
Our analysis of data from an Utstein-based registry in an Asian metropolitan area revealed that patients who experienced an OHCA in low-SES areas of the city were less likely to receive bystander CPR, and demonstrated worse survival outcomes. The information could guide targeted community training to promote bystander CPR.
Acknowledgments
Funding
This research was funded by the National Science Council of Taiwan, grant number NSC 99-2314-B-002-135-MY3 and NSC 101-2314-B-002-120-MY3. Anna Marie Chang was supported by Award Number 1K12HL108974-01 from the National Heart, Lung, and Blood Institute of the United States.
We thank the Taipei City Fire Department and the Taipei City Health Department for their administrative support and the development and implementation of the web-based Utstein-styled quality assurance system for the out-of-hospital cardiac arrests in Taipei City.
Footnotes
A Spanish translated version of the summary of this article appears as Appendix in the final online version at http://dx.doi.org/10.1016/j.resuscitation.2013.07.033.
Conflicts of interest statement
All authors in this study declare no conflicts of interest.
References
- 1.Sasson C, Rogers MA, Dahl J, Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010;3:63–81. doi: 10.1161/CIRCOUTCOMES.109.889576. [DOI] [PubMed] [Google Scholar]
- 2.Sasson C, Meischke H, Abella BS, et al. Increasing cardiopulmonary resuscitation provision in communities with low bystander cardiopulmonary resuscitation rates: a science advisory from the American Heart Association for healthcare providers, policymakers, public health departments, and community leaders. Circulation. 2013;127:1342–50. doi: 10.1161/CIR.0b013e318288b4dd. [DOI] [PubMed] [Google Scholar]
- 3.Sasson C, Magid DJ, Chan P, et al. Association of neighborhood characteristics with bystander-initiated CPR. N Engl J Med. 2012;367:1607–15. doi: 10.1056/NEJMoa1110700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McNally B, Robb R, Mehta M, et al. Out-of-hospital cardiac arrest surveillance –Cardiac Arrest Registry to Enhance Survival (CARES), United States, October 1, 2005–December 31, 2010. MMWR Surveill Summ. 2011;60:1–19. [PubMed] [Google Scholar]
- 5.Ong ME, Shin SD, Tanaka H, et al. Pan-Asian Resuscitation Outcomes Study (PAROS): rationale, methodology, and implementation. Acad Emerg Med. 2011;18:890–7. doi: 10.1111/j.1553-2712.2011.01132.x. [DOI] [PubMed] [Google Scholar]
- 6.Ahn KO, Shin SD, Suh GJ, et al. Epidemiology and outcomes from non-traumatic out-of-hospital cardiac arrest in Korea: a nationwide observational study. Resuscitation. 2010;81:974–81. doi: 10.1016/j.resuscitation.2010.02.029. [DOI] [PubMed] [Google Scholar]
- 7.Ko PC, Ma MH, Yen ZS, Shih CL, Chen WJ, Lin FY. Impact of community-wide deployment of biphasic waveform automated external defibrillators on out-of-hospital cardiac arrest in Taipei. Resuscitation. 2004;63:167–74. doi: 10.1016/j.resuscitation.2004.04.002. [DOI] [PubMed] [Google Scholar]
- 8.Lim HC, Tham KY. Out of hospital cardiac arrests – the experience of one hospital in Singapore. Resuscitation. 2001;51:123–7. doi: 10.1016/s0300-9572(01)00399-9. [DOI] [PubMed] [Google Scholar]
- 9.Nishiuchi T, Hayashino Y, Fukuhara S, et al. Survival rate and factors associated with 1-month survival of witnessed out-of-hospital cardiac arrest of cardiac origin with ventricular fibrillation and pulseless ventricular tachycardia: the Utstein Osaka project. Resuscitation. 2008;78:307–13. doi: 10.1016/j.resuscitation.2008.04.001. [DOI] [PubMed] [Google Scholar]
- 10.Bradley SM, Rea TD. Improving bystander cardiopulmonary resuscitation. Curr Opin Crit Care. 2011;17:219–24. doi: 10.1097/MCC.0b013e32834697d8. [DOI] [PubMed] [Google Scholar]
- 11.Swor R, Khan I, Domeier R, Honeycutt L, Chu K, Compton S. CPR training and CPR performance: do CPR-trained bystanders perform CPR. Acad Emerg Med. 2006;13:596–601. doi: 10.1197/j.aem.2005.12.021. [DOI] [PubMed] [Google Scholar]
- 12.Kanstad BK, Nilsen SA, Fredriksen K. CPR knowledge and attitude to performing bystander CPR among secondary school students in Norway. Resuscitation. 2011;82:1053–9. doi: 10.1016/j.resuscitation.2011.03.033. [DOI] [PubMed] [Google Scholar]
- 13.Vaillancourt C, Lui A, De Maio VJ, Wells GA, Stiell IG. Socioeconomic status influences bystander CPR and survival rates for out-of-hospital cardiac arrest victims. Resuscitation. 2008;79:417–23. doi: 10.1016/j.resuscitation.2008.07.012. [DOI] [PubMed] [Google Scholar]
- 14.Becker LB, Han BH, Meyer PM, et al. Racial differences in the incidence of cardiac arrest and subsequent survival. The CPR Chicago Project. N Engl J Med. 1993;329:600–6. doi: 10.1056/NEJM199308263290902. [DOI] [PubMed] [Google Scholar]
- 15.Galea S, Blaney S, Nandi A, et al. Explaining racial disparities in incidence of and survival from out-of-hospital cardiac arrest. Am J Epidemiol. 2007;166:534–43. doi: 10.1093/aje/kwm102. [DOI] [PubMed] [Google Scholar]
- 16.Mitchell MJ, Stubbs BA, Eisenberg MS. Socioeconomic status is associated with provision of bystander cardiopulmonary resuscitation. Prehosp Emerg Care. 2009;13:478–86. doi: 10.1080/10903120903144833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sasson C, Keirns CC, Smith D, et al. Small area variations in out-of-hospital cardiac arrest: does the neighborhood matter. Ann Intern Med. 2010;153:19–22. doi: 10.1059/0003-4819-153-1-201007060-00255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sasson C, Keirns CC, Smith DM, et al. Examining the contextual effects of neighborhood on out-of-hospital cardiac arrest and the provision of bystander cardiopulmonary resuscitation. Resuscitation. 2011;82:674–9. doi: 10.1016/j.resuscitation.2011.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chiang WC, Ko PC, Wang HC, et al. EMS in Taiwan: past, present, and future. Resuscitation. 2009;80:9–13. doi: 10.1016/j.resuscitation.2008.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ma MH, Chiang WC, Ko PC, et al. A randomized trial of compression first or analyze first strategies in patients with out-of-hospital cardiac arrest: results from an Asian community. Resuscitation. 2012;83:806–12. doi: 10.1016/j.resuscitation.2012.01.009. [DOI] [PubMed] [Google Scholar]
- 21.Daly MC, Duncan GJ, McDonough P, Williams DR. Optimal indicators of socioeconomic status for health research. Am J Public Health. 2002;92:1151–7. doi: 10.2105/ajph.92.7.1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Iwashyna TJ, Christakis NA, Becker LB. Neighborhoods matter: a population-based study of provision of cardiopulmonary resuscitation. Ann Emerg Med. 1999;34:459–68. doi: 10.1016/s0196-0644(99)80047-x. [DOI] [PubMed] [Google Scholar]
- 23.RA, King EM, Sayre M, Colbert S, Bond-Zielinski C, Sasson C. How to design a targeted, community-based cardiopulmonary resuscitation intervention for high-risk neighborhood residents. Ann Emerg Med. 2011;58:S281. [Google Scholar]
- 24.Stromsoe A, Andersson B, Ekstrom L, et al. Education in cardiopulmonary resuscitation in Sweden and its clinical consequences. Resuscitation. 2010;81:211–6. doi: 10.1016/j.resuscitation.2009.10.014. [DOI] [PubMed] [Google Scholar]
- 25.Tanigawa K, Iwami T, Nishiyama C, Nonogi H, Kawamura T. Are trained individuals more likely to perform bystander CPR. An observational study. Resuscitation. 2011;82:523–8. doi: 10.1016/j.resuscitation.2011.01.027. [DOI] [PubMed] [Google Scholar]
- 26.Groeneveld PW, Owens DK. Cost-effectiveness of training unselected laypersons in cardiopulmonary resuscitation and defibrillation. Am J Med. 2005;118:58–67. doi: 10.1016/j.amjmed.2004.08.014. [DOI] [PubMed] [Google Scholar]