Abstract
Objective
To compare cost estimates for hospital stays calculated using diagnosis-related group (DRG) weights to actual Medicare payments.
Data Sources/Study Setting
Medicare MedPAR files and DRG tables linked to participant data from the Study of Osteoporotic Fractures (SOF) from 1992 through 2010. Participants were women age 65 and older recruited in three metropolitan and one rural area of the United States.
Study Design
Costs were estimated using DRG payment weights for 1,397 hospital stays for 795 SOF participants for 1 year following a hip fracture. Medicare cost estimates included Medicare and secondary insurer payments, and copay and deductible amounts.
Principal Findings
The mean (SD) of inpatient DRG-based cost estimates per person-year were $16,268 ($10,058) compared with $19,937 ($15,531) for MedPAR payments. The correlation between DRG-based estimates and MedPAR payments was 0.71, and 51 percent of hospital stays were in different quintiles when costs were calculated based on DRG weights compared with MedPAR payments.
Conclusions
DRG-based cost estimates of hospital stays differ significantly from Medicare payments, which are adjusted by Medicare for facility and local geographic characteristics. DRG-based cost estimates may be preferable for analyses when facility and local geographic variation could bias assessment of associations between patient characteristics and costs.
Keywords: Hospital costs, DRG weights, Medicare claims, Medicare payment, cohort-claims linked studies
Studies of health care costs in the United States commonly use Medicare payment variables in claims files as an indicator for those costs for three reasons; (1) those age 65 and older have the highest per person health care costs; (2) Medicare is the insurance carrier that is the primary payer for 95 percent of this segment of the population, allowing for such studies to be representative to all regions of the United States; and (3) Medicare strives to pay a specific amount needed to care for that condition based on the resource intensity needed for patients with that condition. Medicare inpatient claims files include what Medicare and secondary insurers (if any) paid the hospital provider, deductible and copayments for which the patient is responsible, and any additional outlier payments added by Medicare.
Large epidemiologic cohort studies, such as the Study of Osteoporotic Fractures (SOF), Framingham, and the Women's Health Initiative, have phenotypically characterized individual participants with greater detail and accuracy than claims or medical record data. Therefore, linkages of these cohorts to Medicare claims may improve estimation of the association between individual characteristics and health care costs.
Despite the advantages of Medicare data, calculating resource costs for hospital care using linked cohort Medicare claims datasets presents many challenges. Large cohort studies typically recruit their study populations in a limited number of regions of the United States. The choice of specific study sites is important for two reasons. First, there is significant geographic variation in health care costs across the United States (Fisher et al. 2003a,b; Song et al. 2010; Zuckerman et al. 2010; Kelley et al. 2011) even within small geographic regions (Rosenthal et al. 1997). The degree to which this variation can be explained by beneficiary health status is controversial (Hadley et al. 2011; Hadley and Reschovsky 2012), but if geographic variation in “true” inpatient costs is not the focus of a particular study, the choice of study sites could affect the results in unintended ways.
Second, even if the actual resources used to treat case mix and severity-adjusted patients in two geographic areas are identical, Medicare adjusts payments to most hospital providers for local variation in the unit prices of inputs to care (labor and capital). These geographic differences may not be relevant to the determination of associations between individual characteristics and resource costs required for their health care unless the analysis is focused specifically on variation due to input prices. For example, whether a patient is hospitalized for a condition in a region with high labor costs conceptually would not be relevant to the association of chronic kidney disease with the resources required to care for patients with that condition. Removing geographic adjustment factors is also required to generalize findings of studies with data from only some to all geographic regions of the United States.
Medicare also pays extra to hospitals that employ physicians in training (interns and residents) and to hospitals that care for a disproportionate share (DSH) of indigent clients. As is true of input prices, being in a teaching versus nonteaching hospital or a DSH hospital may not be relevant to the association of individual characteristics with resource costs required for hospital care, unless the focus is explicitly on comparison of Medicare's costs across those types of institutions.
Medicare payment policy also has changed over time, including the diagnosis-related group (DRG) codes assigned to different constellations of ICD-9 diagnoses and procedures, the weights assigned to those DRGs, and the specific methodology for geographic adjustments. Cohort-claims linked studies that have followed participants over many years need to account for these time specific differences and for health care cost inflation, such that hospital utilization in different years is comparable.
Finally, Medicare does not use the prospective payment system (PPS, introduced in 1983) to determine payments to hospitals in the State of Maryland, critical access hospitals, some other rural hospitals, and some comprehensive cancer centers. If a significant proportion of claims linked to cohort data are from hospitals not paid under the PPS, then making payments to all hospitals comparable presents a challenge.
Our purpose is to demonstrate how researchers can overcome these challenges. First, we describe in more detail how Medicare adjusts payments to hospitals. Second, we propose a method of estimating costs based on DRG weights that reflects the acuity of the medical and/or surgical condition of the patient, but it does not include other adjustments based on geographic location and other hospital characteristics. Third, we compare cost estimates produced by the DRG weight method to cost estimates from Medicare Provider Analysis and Review (MedPAR) claims data for hospital claims for 1 year following a hip fracture, using data of the SOF.
How Does CMS Determine Payment for a Hospital Stay?
We begin with a general overview of how Medicare determines payment for hospital stays under the PPS.
Before the start of each fiscal year, Medicare determines a standard base payment amount for all hospital stays (Table1), published each year in the Federal Register.1 Medicare assigns a DRG code to each hospital stay based on the constellation of the diagnoses and procedures associated with that stay. Each DRG is assigned a weight that reflects the intensity of monetary resources required to care for a person with that DRG, and it is calculated by Medicare as the average costs across the United States for all hospital stays assigned to that specific DRG relative to the average cost for all hospitalizations (Edwards et al. 1994; Goldfield 2010). From 1992 through 2004, the standardized base amount varied according to whether the hospital provider was located in a large urban, other urban, or rural area (Table1).
- Medicare then adjusts the standard base payment amount for the relative input prices of labor and capital specific for the geographic location in which the hospitalization occurred, first splitting the standard base payment amount into operating and capital components. Medicare adjusts a portion of the operating amount (ranging from 62 to 71 percent between 1992 and 2010) for labor costs using the hospital wage index (hwi), and the capital amount by the capital wage index (cwi; called the geographic adjustment factor in the CMS Impact Files [Centers for Medicare and Medicaid Services 2013] since 2005). The geographic-adjusted standard base amount is thus calculated as:
where: Standard_Base_AmountUNADJUSTED is the sum of the standard operating and capital amounts before adjustment for local capital and labor input prices; Prop_Operating is the proportion of the total unadjusted standard base amount that is for operating costs; and Prop_Labor is the proportion of the operating costs attributable to labor and therefore subject to adjustment by the hwi.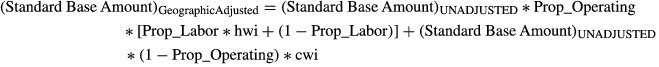
(1) The geographically adjusted standard base amount then is multiplied by the weight for that DRG. The DRG weights for all DRGs for each year 1992 through 2010 inclusive are publicly available on the CMS website (also available from the VA Health Economic Resource Center) (Centers for Medicare and Medicaid Services 2009; Veterans Administration Health Economics Resource Center 2013).
Medicare adds additional payment for stays that are considered outliers for which the DRG codes are thought not to fully capture the true costs of caring for that person, based on procedure and diagnosis codes and/or length of stay.
- However, in instances where the length of stay is particularly short and the person is transferred to another hospital, Medicare believes costs of care are being shifted from the hospital to which the patient was first admitted to the hospital to which the patient is being transferred, and calculates a geographically adjusted daily base payment rate for a particular DRG to be:
. For each DRG, Medicare calculates the geometric mean2 length of stay for each fiscal year from Medicare beneficiary data for the previous year. The total cost for extra short stays accompanied by a transfer to another hospital is then calculated as: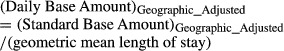
(2)
, where LOS is the length of stay of the hospitalization. Because hospital-based interventions are more intense on the first day of a hospital stay, Medicare pays twice the daily rate for that first day. By this formula, hospital stays that are more than 1 day shorter than the geometric mean length of stay for that DRG would be paid less than longer hospital stays with that DRG. Throughout the 1990s lengths of stay decreased for hospital stays under many DRGs accompanied by increasing transfers to skilled nursing facilities (SNFs). Starting in 1998, Medicare began using Equation 3 for extra short hospital stays associated with certain DRGs accompanied by transfer to an SNF or inpatient rehabilitation facility (IRF) (Cromwell, Donoghue, and Gilman 2002).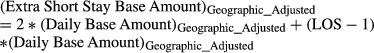
(3) Medicare then adds in payment, if applicable, for Direct Graduate Medical Education and for bad debts (called Passthru payments). Bad debts represent copays and deductibles that the hospital has been unable to collect from beneficiaries.
Medicare makes additional payments for Indirect Medical Education (IME) to hospitals that employ physicians in training for patient care and for treatment of a DSH of patients on Supplemental Security Income or who are eligible for Medicaid, but not Part A Medicare.
- Beyond all of the payments listed above, Medicare has added in additional payments, for the costs of donor organ acquisition, and in some years for use of new technologies that are particularly expensive. Based on these variables, the total allowable payment cost, including the copays and deductibles for which the patient is responsible, is equal to:

(4)
Table 1.
Standardized Base Amounts* for Inpatient Hospital Stay Payment under the Prospective Payment System
| Fiscal Year | Standardized Base Amount | Proportion of Standard Amounts Attributed to Operating Expenses | Proportion of Operating Expenses Due to Labor Costs | Inflation Factor to Standardize to 2010 U.S. $† |
|---|---|---|---|---|
| 1992 | Large urban: $3,893 Other urban: $3,927 Rural: $3,908 |
Large urban: 0.896 Other urban: 0.894 Rural: 0.894 |
Any urban: 0.708 Rural: 0.720 |
Large urban: 1.419 Other urban: 1.440 Rural: 1.447 |
| 1993 | Large urban: $4,072 Other urban: $4,014 Rural: $4,003 |
Large urban: 0.898 Other urban: 0.896 Rural: 0.896 |
Any urban: 0.708 Rural: 0.720 |
Large urban: 1.388 Other urban: 1.408 Rural: 1.412 |
| 1994 | Large urban: $4,115 Other urban: $4,056 Rural: $3,946 |
Large urban: 0.908 Other urban: 0.907 Rural: 0.904 |
Any urban: 0.708 Rural: 0.756 |
Large urban: 1.374 Other urban: 1.394 Rural: 1.433 |
| 1995 | Large urban: $4,171 All other: $4,111 |
Large urban: 0.910 All other: 0.908 |
0.714 | Large urban: 1.355 All other: 1.375 |
| 1996 | Large urban: $4,301 All other: $4,241 |
Large urban: 0.893 All other: 0.891 |
0.714 | Large urban: 1.314 All other: 1.333 |
| 1997 | Large urban: $4,347 All other: $4,286 |
Large urban: 0.899 All other: 0.898 |
0.712 | Large urban: 1.300 All other: 1.319 |
| 1998 | Large urban: $4,276 All other: $4,214 |
Large urban: 0.913 All other: 0.912 |
0.711 | Large urban: 1.322 All other: 1.341 |
| 1999 | Large urban: $4,475 All other: $4,231 |
Large urban: 0.916 All other: 0.911 |
Large urban: 0.679 All other: 0.711 |
Large urban: 1.263 All other: 1.336 |
| 2000 | Large urban: $4,328 All other: $4,265 |
Large urban: 0.913 All other: 0.912 |
0.711 | Large urban: 1.306 All other: 1.325 |
| 2001 | Large urban: $4,410 All other: $4,347 |
Large urban: 0.913 All other: 0.912 |
0.711 | Large urban: 1.282 All other: 1.301 |
| 2002 | Large urban: $4,547 All other: $4,482 |
Large urban: 0.914 All other: 0.913 |
0.711 | Large urban: 1.243 All other: 1.261 |
| 2003 | Large urban: $4,658 All other: $4,591 |
Large urban: 0.913 All other: 0.911 |
0.711 | Large urban: 1.214 All other: 1.231 |
| 2004 | Large urban: $4,839 All other: $4,769 |
Large urban: 0.914 All other: 0.913 |
0.711 | Large urban: 1.168 All other: 1.185 |
| 2005 | $4,972 | 0.916 | HWI >1: 0.711 HWI ≤1: 0.62 |
1.137 |
| 2006 | $5,152 | 0.918 | HWI >1: 0.697 HWI ≤1: 0.62 |
1.097 |
| 2007 | $5,302 | 0.919 | HWI >1: 0.697 HWI ≤1: 0.62 |
1.066 |
| 2008 | $5,387 | 0.921 | HWI >1: 0.697 HWI ≤1: 0.62 |
1.049 |
| 2009 | $5,549 | 0.924 | HWI >1: 0.697 HWI ≤1: 0.62 |
1.019 |
| 2010 | $5,653 | 0.924 | HWI >1: 0.688 HWI ≤1: 0.62 |
1.000 |
Standard amounts per final rule for each fiscal year in Federal Register.
Inflation factors are calculated as the following ratio; Standard_Base_Amount2010/Standard_Base_AmountPRIOR_YEAR.
HWI, hospital wage index.
Method 1: Estimation of Hospital Costs Using MedPAR Variables
Because of their availability in the MedPAR payment files and ease of use, many studies estimating costs of hospital care using Medicare claims have used MedPAR payment variables (Kilgore et al. 2009; Patel et al. 2010; Whellan et al. 2010; Kuo and Goodwin 2011; Skolarus et al. 2013). The payment variable in MedPAR called DRGPRICE is equal to Equation 4 minus Outlier and Passthru payments. Therefore, a cost estimate of a hospital stay that represents amount reimbursed to providers from all sources is:
| (5) |
Method 2: Estimation of Hospital Costs Based on DRG weights and Standard Base Amounts (A Proposed Method)
When the researcher's focus is on the cost of resources required to care for individuals, the relevant concept of cost is likely to be the cost (adjusted for severity of their medical and/or surgical conditions) regardless of whether the hospital stay occurred in rural or urban setting, the relative local input prices, whether the patient was hospitalized in a teaching or nonteaching hospital, or whether the hospital was paid under the PPS. For that type of study, the relevant resource cost for an acute hospital stay (excluding those with an extra short length of stay accompanied by transfer to another hospital, SNF, or IRF) based on DRG weights and standard base amounts (from Table1) to be defined as:
| (6) |
For hospital stays occurring prior to 2005, Equation 5 still reflects a small geographic adjustment, since the standard amounts in those years were typically less for rural compared to urban areas.
For extra short stays accompanied by a transfer to another hospital, IRF, or SNF within 1 day of hospital discharge, we agree with Medicare that costs of care probably have been transferred from the first to the receiving institution regardless of DRG, including hospitalizations occurring before fiscal year 1998. To make that adjustment, the hospital cost per day for a particular DRG and fiscal year should be:
| (7) |
and that the resource cost for an extra short stays accompanied by a transfer to be:
| (8) |
Equations 7 and 8 are the same as Equations 2 and 3 except that standard based amounts without geographic adjustment are used and outlier payment is added.
Standardizing Inpatient Resource Costs to One Calendar Year
For hospital costs in early years to be comparable to later years, it is necessary to account for cost inflation over the time period and standardize costs of all hospitalizations to the same year regardless of when they occurred. We recommend using the ratio of the Medicare standard amounts between a current year and prior years as the inflation factor; Standard_Base_AmountCURRENT_YEAR/Standard_Base_AmountPRIOR_YEAR (Table1) rather than the consumer price index for hospital care, because the standard amounts Medicare uses to base their reimbursements are largely based on hospital cost reports that are designed in part to estimate the actual resource costs for hospital care. In contrast, the consumer price index for hospital services specifically is constructed from hospital prices charged uninsured patients and those covered by nongovernment insurers, but not those covered by Medicare (Cardenas 1996).
It should be noted that the same standard amount has been applied to all geographic locations (large urban, other urban, and rural) since 2005. Therefore, when the analysis is standardizing costs to 2005 or a more recent year, the differences between urban and rural hospitals for hospital stays occurring prior to fiscal year 2005 are removed.
Comparison of Estimated Costs for Inpatient Stays Based on DRG Weights versus MedPAR Payment Variables: An Example Study Population
Overview of the Study
We used the SOF, a cohort designed to investigate the epidemiology of fractures in older women. The study recruited 9,704 community-dwelling women age 65 years and older using population-based listings at four geographic locations in the United States (Baltimore, MD; Minneapolis, MN; Portland, OR; and a rural area near Pittsburgh, PA) from 1986 to 1988 (Cummings et al. 1990). Participants had study visits every two to four years with follow-up among active surviving participants over 25 years. Postcards were mailed to participants every 4 months to inquire about incident fractures. For those who reported an incident fracture, medical records were obtained to confirm that the fracture had occurred.
Linkage of Cohort Data to Medicare Claims
Medicare claims for the time period January 1, 1992 through December 31, 2010 were linked successfully to 92 percent of participants still alive and enrolled in the cohort as of January 1, 1992, matching participants to their claims based on Social Security number and date of birth (Schousboe et al. 2013). We identified 1,154 SOF participants who were discharged from a hospital with a primary discharge diagnosis of 820.0x (incident hip fracture) between January 1, 1992 and December 31. We limited our analyses to those who also had (1) no self-reported prior hip fracture at the baseline SOF visit; (2) no incident hip fracture between the baseline visit and January 1, 1992; (3) no evidence from radiographic reports at the time of the fracture showing the fracture to be in the pelvis or distal femur rather than the proximal femur; and (4) enrollment in Medicare Fee for Service (both parts A and B) for the 12-month period following the index hip fracture hospitalization admission date. We used the MedPAR file to identify all hospital stays for the 12 months after hip fracture, and also all IRF and SNF stays over that time period so we could identify those transferred from an acute care hospital to an IRF or SNF. Seven hundred ninety-five (795) women met these criteria.
The number of hospitalizations and mean lengths of stays were characterized for all 795 individuals (Table2). The MedPAR file was used to determine if the hospital stay was paid for under the PPS, and what (if any) IME, DSH, outlier, and passthru payments were made. We estimated costs of 1,397 hospital stays with nonzero Medicare payment that occurred within 1 year of the date of hip fracture for all 795 individuals based on (1) DRG weights and standard base amounts using Equations 6 and 8 and (2) payment variables from the hospital claim using Equation 5. We estimated the correlation (using the Spearman rank statistic) of the estimates based on the two methods for (1) the subset paid under the PPS and (2) all hospital stays with nonzero Medicare payment.
Table 2.
Characteristics of Hospital Stays
| Characteristic | Paid under Prospective Payment System (n = 845)§ | Not Paid under Prospective Payment System (n = 552)§ |
|---|---|---|
| State of hospital stay (%) | ||
| Maryland | 0 (0) | 541 (97.3) |
| Pennsylvania | 456 (53.8) | 6 (1.1) |
| Minnesota | 191 (22.5) | 7 (1.3) |
| Florida | 38 (4.5) | 1 (0.2) |
| Oregon | 30 (3.5) | 0 (0.0) |
| Other* | 133 (15.7) | 1 (0.2) |
| Number (%) with IME payments | 338 (39.9) | 0 (0) |
| Number (%) with DSH payments | 328 (38.7) | 0 (0) |
| Number (%) with outlier payments | 9 (1.1) | 0 (0) |
| Number (%) with passthru payments | 622 (73.3) | 2 (0.4) |
| Mean length of stay, days (SD) | 6.3 (4.5) | 6.4 (4.5) |
| Proportion with extra short stay† and transfer to another facility‡ | 206 (24.3) | 134 (24.1) |
| Estimated cost (SD), MedPAR payment variables | $10,414 (5,674) | $12,623 (8,099) |
| Estimated cost (SD), DRG weight based | $9,403 (4,945) | $8,903 (3,685) |
Twenty-nine other states.
Length of stay ≤ (geometric mean for that DRG and fiscal year) minus one.
Admission to another facility (short stay hospital, SNF, or IRF) within 1 day of discharge from the short stay hospital.
Three stays paid under PPS and three not paid under PPS had zero Medicare Payment.
To visualize the change in rank order of hospital stay costs when using resource costs estimated from DRG weights instead of MedPAR payment variables, we estimated the proportions of hospital stays that would be in a different quintile of cost using one method compared with the other. We did this using (1) each hospital stay as the unit of analysis and (2) the sum of all inpatient costs for the year following the index hip fracture with the individual person as the unit of analysis.
Results
Of the 795 SOF participants identified for these analyses, 56 percent did not require additional hospitalization after the initial stay for their hip fracture, 27.4 percent required one additional hospitalization, and 16.3 percent required two or more additional hospitalizations (Figure1). The majority of hospitalizations occurred in the states where the SOF participants were recruited, but 173 (12.3 percent) occurred in states other than the four where the SOF study sites are located, reflecting the mobility of the study population over the 19-year period (Table2). Among 845 hospital stays paid under the PPS, 39.9 percent were given IME payments (representing 6.6 percent of DRGPRICE for those with nonzero reimbursement), and 38.7 percent were given DSH payments (representing 5.7 percent of DRGPRICE among those with nonzero DSH reimbursement). Passthru payments were added for 73.3 percent of all acute hospital stays paid under the PPS (representing 6.4 percent of DRGPRICE for those hospital stays with nonzero passthru reimbursements). For hospital stays that were not reimbursed under the PPS, costs for medical education and burden of indigent clients were already factored into their estimated costs and additional IME, DSH, outlier, or passthru payments do not appear in MedPAR.
Figure 1.
Distribution of Number of Hospital Admissions during Year Following Hip Fracture *Active SOF participants as of January 1, 1992, who had an incident hip fracture enrolled in Medicare Fee for Service on the date of hip fracture through the following 365 days.^Includes initial acute hospital stay to surgically treat hip fracture.
Twenty-four percent of hospital stays had extra short lengths of stay and were associated with a transfer to another facility (Table2). Applying a transfer penalty by using the per diem method of calculating the cost of the hospital stay resulted in a reduction of calculated costs for 95 percent of these stays. The mean decrease was $1,475 (with 5 and 95 percentile values, respectively, of −$3,854 and $0).
The Spearman correlation of length of stay with standardized costs calculated using DRG weights was 0.29. However, the total days spent in acute care hospitals during the year after hip fracture was more strongly correlated with the sum of standardized costs of acute hospital care (Spearman correlation 0.80).
Comparison of Costs Calculated from Standard Base Amounts and DRG Weights to Costs Calculated Solely from MedPAR Payment Variables
Resource costs calculated using DRG weights and standard base amounts were substantially different than the cost estimates from payment variables, especially for hospital stays not paid under the PPS (Table2). When hospital stays with nonzero Medicare payment paid under the PPS were considered (n = 845), the correlation between standardized costs estimated from our method with estimates from Medicare payment variables (without removal of geographic adjustment factors, IME payments, and DSH payments) was 0.85 (Figure2, panel A). When all hospital stays with nonzero Medicare payment were considered, including those not paid under PPS (n = 1,397), the correlation between the estimates from raw MedPAR variables and those from standard base amounts and DRG weights was reduced further to 0.71 (Figure2, panel B). For the subset of hospital stays not paid under the PPS, the correlation was even lower (0.56).
Figure 2.
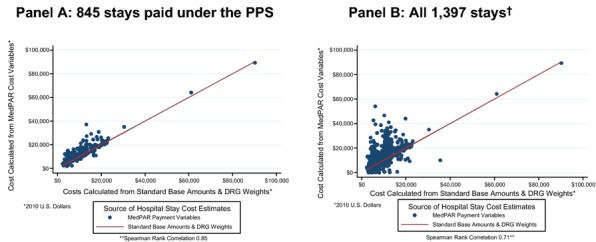
Scatterplots of Cost Estimates from Medicare Payment Variables versus Costs from Standard Base Amounts and DRG Weights†Six hospital stays with zero Medicare payment excluded. DRG, diagnosis-related group; PPS, prospective payment system.
Comparison of Rank Order of Hospital Costs
The rank order of hospital stay costs was considerably altered using cost estimates based on DRG weights and standard base amounts instead of payment variables. Only 49 percent of hospital stays were in the same quintile of costs when calculated with our method of standardization compared with quintile of payment cost estimates (Figure3, panel A). When all hospital costs per person for the year following a hip fracture were summed, the mean and standard deviation of DRG weight-based resource costs in 2010 U.S. dollars ($16,268 and $10,058, respectively) were somewhat lower than the mean and standard deviation of costs derived from MedPAR variables ($19,937 and $15,531, respectively). Only 51 percent had yearly costs based on DRG weights in the same quintile as when estimated from claims-based payment variables (Figure3, panel B).
Figure 3.
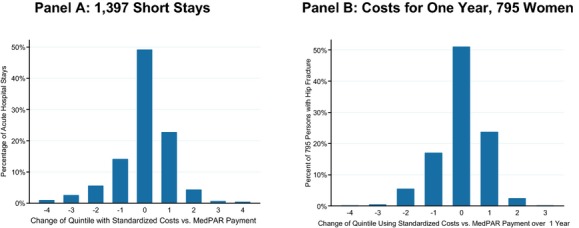
Change of Quintile for DRG Weight-Based Costs versus Costs Estimated from Claim Payment Variables
Discussion
Our results show that resource costs that reflect the acuity of the medical and surgical condition of the patient, calculated from DRG weights and standard base amounts, differ substantially from costs that are calculated from Medicare claims payment variables that include adjustments for the hospital's geographic location and other characteristics, payments for medical education, and care for indigent clients. For research questions for which of these adjustments are not relevant, estimating costs using Medicare payments that include these adjustments at best introduces stochastic noise that would reduce statistical power (in analyses where costs are the dependent variable) and might bias estimated associations of costs with other outcomes toward the null (in analyses where costs are a predictor variable). Reduced power may not be a concern for studies that have used the 5 percent chronic condition warehouse sample of Medicare to assess costs (Kilgore et al. 2009), because of its large size. However, cohort studies that link to Medicare claims generally will have much smaller sample sizes.
Using DRG weights to calculate payments is simple and applicable to stays in any acute care hospital in the United States for which Medicare is the primary payer. The only data required from Medicare files to apply this method are the DRG associated with the hospital stay, the length of stay, information about whether the person was transferred to (or from) another facility, and any outlier payments for the hospital stay. The weights for each DRG, the geometric mean length of stay for that DRG, and the standard base amounts on which Medicare bases payment are needed for the fiscal year in which the person was hospitalized. Inflation factors to standardize all costs to the same year are needed when the dataset being used spans several years. Tables with these additional data are in the public domain and are available from the corresponding author by request.
Our method has advantages over other methods to estimate costs of hospital care. One can algebraically rearrange Equations 4–4 to obtain a cost estimate for hospital stays based on the DRGPRICE payment variable with the geographic adjustments and IME and DSH payments removed. This approach requires using CMS Impact files to identify hospital and capital wage indices for the hospitals in which stays occurred (Centers for Medicare and Medicaid Services 2013) and is not applicable to hospital stays that are not paid under the PPS. Others have also estimated costs by using regression models to adjust Medicare payments for hospital characteristics (including its geographic location, the local hwi, and local area poverty rate) (Jha et al. 2009; Joynt, Orav, and Jha 2011), but the parameter coefficients produced from such a regression model are likely to be applicable to only the specific hospitals included in that study. However, this approach has the advantage that it captures the relative importance of predictors such as hospital characteristics and individual-level characteristics, adjusted for each other. Cost to charge ratios, which can be gleaned for each fiscal year for any hospital provider from Medicare Cost Reports, have been used to estimate the true cost of care for a stay in any acute care hospital from hospital charges (Taira et al. 2003; Groeneveld et al. 2008; Brinjikji et al. 2011; Roy et al. 2012; Jain et al. 2013). However, this method is tedious, and it may be accurate only if the patient's utilization within each cost center in the hospital is adjusted by the unique cost to charge ratio of that center before the aggregate cost for the entire stay is calculated (Taira et al. 2003). Moreover, cost variation attributable to hospital characteristics and local input prices is retained by this method. For research questions where it is important to capture these sources of cost variation, use of cost to charge ratios at the hospital department level may be the gold standard for estimating the true resource utilization for hospital care. Finally, one could use institutional lengths of stay as a surrogate measure of resource utilization, but this does not capture outpatient utilization. In contrast, estimated inpatient costs can be summed with outpatient costs to yield estimates of total costs of care.
Additional studies comparing all of these methods of hospital cost estimation are needed. Our method is most suited to research questions regarding the associations of individual patient characteristics and hospital costs. In addition, our method would be appropriate for investigations of hospital costs attributable to the medical and surgical acuity of populations that include individuals insured by two or more insurers with different payment policies for hospital stays. For example, if one wanted to estimate resource costs for inpatient stays for veterans who use the VA system and/or non-VA hospitals, our method makes hospital stay cost estimation across the two payment systems comparable. Similarly, our method is applicable to investigations comparing the degrees to which two or more insurers with different payment policies may be selecting insurees who are less likely to generate inpatient costs. Our method could also be used in studies comparing the relative true inpatient resource costs, attributable to their patients' medical and surgical acuity, of different types of hospitals (e.g., teaching and community hospitals).
However, there are many other types of research questions where geographic adjustment or extra payments for medical education or DSH hospitals are important to retain. For example, studies done to examine determinants of what Medicare actually pays hospitals (such as characteristics of hospitals and the geographic regions in which they are located) need to use the actual payment variables in the MedPAR file.
Our study has several limitations. Our method depends on DRG weights and outlier payments to fully capture the differences in resource intensity needed to care for the individual during a particular hospital stay. The DRG system was revised considerably in 2007 (and renamed the MS-DRG system) to better capture variations in individual illness acuity, health status, and diagnoses that would influence the resources needed to care for that individual (Rosenstein et al. 2009). Hence, our method does not capture the full variation in resource costs for hospital stays that occurred prior to fiscal year 2008. Additionally, our data are not directly applicable to Medicare Advantage enrollees, but our method could be used to estimate national resource costs for hospital stays of Medicare Advantage enrollees if claims data with the variables needed to apply the method were available from Medicare Advantage carriers.
Our dataset is also limited to individuals recruited at only four geographic areas of the United States. Our analyses address estimation of the relative resource cost of hospital stays and do not address whether the absolute true resource costs are fully captured with the standardized method based on DRG weights. The analyses presented in this article are not applicable to other sources of health care costs, specifically outpatient services and postacute care. We limited our analyses to hospitalizations for the year following a hip fracture, but these included one or more hospital stays for 182 separate DRGs. We believe our method is applicable to all hospital stays regardless of the DRG assigned to that stay, but additional studies comparing these costing methods across the entire breadth of DRGs are needed to confirm this. Finally, additional studies are needed to establish the validity of estimating hospital costs using this method for those younger than age 65 covered by private health insurers.
In conclusion, resource costs for required inpatient acute hospital care for Medicare beneficiaries can be estimated using Medicare standard base payment amounts, discharge DRG codes, weights assigned to and the geometric mean length of stay for those DRGs, the actual lengths of stay of the inpatient episodes, and inflation factors to standardize costs to the same year. This method can be used for hospital stays that occurred in 1992 onward regardless of whether the hospital stay occurred in a teaching hospital, in a hospital caring for a DSH of indigent clients, or was paid for by Medicare under the PPS.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: The “Predictors of Health Care Utilization and Costs Attributable to Hip Fractures” is supported by National Institutes of Health funding. The National Institute on Aging (NIA) provides support under the following grant number: 1 R01 AG38415-01A1. The Study of Osteoporotic Fractures (SOF) is supported by National Institutes of Health funding. The National Institute on Aging (NIA) provides support under the following grant numbers: R01 AG005407, R01 AR35582, R01 AR35583, R01 AR35584, R01 AG005394, R01 AG027574, and R01 AG027576.
Disclosures: None.
Disclaimers: None.
Notes
Example: for standard base amounts used for fiscal year 2010, see Federal Register Vol 74, No. 165, Thursday, August 27, 2009, p. 43754.
The geometric mean is defined as the nth root of the product of n numbers. For example, the geometric mean of 2, 8, and 16 is:  .
.
Supporting Information
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
References
- Brinjikji W, Kallmes DF, Rabinstein AA, Lanzino G, Cloft HJ. Hospitalization Costs for Patients with Acute Ischemic Stroke Treated with Endovascular Embolectomy in the United States. Stroke. 2011;42(11):3271–3. doi: 10.1161/STROKEAHA.111.618405. [DOI] [PubMed] [Google Scholar]
- Cardenas E. The CPI (Consumer Price Index) for Hospital Services: Concepts and Procedures. Monthly Labor Review. 1996;119(7):32–42. [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid Services. 2009. . “ Historical DRG Weight File ” [accessed on June 20, 2013]. Available at http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Acute-Inpatient-Files-for-Download-Items/CMS1247872.html. [PubMed]
- Centers for Medicare and Medicaid Services. 2013. . “ Historical Impact Files for FY 1994 through Present ” [accessed on June 20, 2013]. Available at http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Historical-Impact-Files-for-FY-1994-through-Present.html.
- Cromwell J, Donoghue S, Gilman BH. Expansion of Medicare's Definition of Post-Acute Care Transfers. Health Care Financing Review. 2002;24(2):95–113. [PMC free article] [PubMed] [Google Scholar]
- Cummings SR, Black DM, Nevitt MC, Browner WS, Cauley JA, Genant HK, Mascioli SR, Scott JC, Seeley DG, Steiger P, Vogt TM. Appendicular Bone Density and Age Predict Hip Fracture in Women: The Study of Osteoporotic Fractures Research Group. Journal of the American Medical Association. 1990;263(5):665–8. [PubMed] [Google Scholar]
- Edwards N, Honemann D, Burley D, Navarro M. Refinement of the Medicare Diagnosis-Related Groups to Incorporate a Measure of Severity. Health Care Financing Review. 1994;16(2):45–64. [PMC free article] [PubMed] [Google Scholar]
- Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The Implications of Regional Variations in Medicare Spending. Part 1: The Content, Quality, and Accessibility of Care. Annals of Internal Medicine. 2003a;138(4):273–87. doi: 10.7326/0003-4819-138-4-200302180-00006. [DOI] [PubMed] [Google Scholar]
- Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The Implications of Regional Variations in Medicare Spending. Part 2: Health Outcomes and Satisfaction with Care. Annals of Internal Medicine. 2003b;138(4):288–98. doi: 10.7326/0003-4819-138-4-200302180-00007. [DOI] [PubMed] [Google Scholar]
- Goldfield N. The Evolution of Diagnosis-Related Groups (DRGs): From Its Beginnings in Case-Mix and Resource Use Theory, to Its Implementation for Payment and Now for Its Current Utilization for Quality within and outside the Hospital. Quality Management in Health care. 2010;19(1):3–16. doi: 10.1097/QMH.0b013e3181ccbcc3. [DOI] [PubMed] [Google Scholar]
- Groeneveld PW, Matta MA, Greenhut AP, Yang F. The Costs of Drug-Eluting Coronary Stents among Medicare Beneficiaries. American Heart Journal. 2008;155(6):1097–105. doi: 10.1016/j.ahj.2008.01.012. [DOI] [PubMed] [Google Scholar]
- Hadley J, Reschovsky JD. Medicare Spending, Mortality Rates, and Quality of Care. International Journal of Health Care Finance and Economics. 2012;12(1):87–105. doi: 10.1007/s10754-012-9107-0. [DOI] [PubMed] [Google Scholar]
- Hadley J, Waidmann T, Zuckerman S, Berenson RA. Medical Spending and the Health of the Elderly. Health Services Research. 2011;46(5):1333–61. doi: 10.1111/j.1475-6773.2011.01276.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jain NB, Kuye I, Higgins LD, Warner JJ. Surgeon Volume Is Associated with Cost and Variation in Surgical Treatment of Proximal Humeral Fractures. Clinical Orthopaedics and Related Research. 2013;471(2):655–64. doi: 10.1007/s11999-012-2481-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jha AK, Orav EJ, Dobson A, Book RA, Epstein AM. Measuring Efficiency: The Association of Hospital Costs and Quality of Care. Health Affairs. 2009;28(3):897–906. doi: 10.1377/hlthaff.28.3.897. [DOI] [PubMed] [Google Scholar]
- Joynt KE, Orav EJ, Jha AK. The Association between Hospital Volume and Processes, Outcomes, and Costs of Care for Congestive Heart Failure. Annals of Internal Medicine. 2011;154(2):94–102. doi: 10.1059/0003-4819-154-2-201101180-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelley AS, Ettner SL, Morrison RS, Du Q, Wenger NS, Sarkisian CA. Determinants of Medical Expenditures in the Last 6 Months of Life. Annals of Internal Medicine. 2011;154(4):235–42. doi: 10.7326/0003-4819-154-4-201102150-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kilgore ML, Morrisey MA, Becker DJ, Gary LC, Curtis JR, Saag KG, Yun H, Matthews R, Smith W, Taylor A, Arora T, Delzell E. Health Care Expenditures Associated with Skeletal Fractures among Medicare Beneficiaries, 1999-2005. Journal of Bone and Mineral Research. 2009;24(12):2050–5. doi: 10.1359/jbmr.090523. [DOI] [PubMed] [Google Scholar]
- Kuo YF, Goodwin JS. Association of Hospitalist Care with Medical Utilization after Discharge: Evidence of Cost Shift from a Cohort Study. Annals of Internal Medicine. 2011;155(3):152–9. doi: 10.1059/0003-4819-155-3-201108020-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel UD, Greiner MA, Fonarow GC, Phatak H, Hernandez AF, Curtis LH. Associations between Worsening Renal Function and 30-day Outcomes among Medicare Beneficiaries Hospitalized with Heart Failure. American Heart Journal. 2010;160(1):132–8. doi: 10.1016/j.ahj.2010.03.033. , and . “ .” e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenstein AH, O'Daniel M, White S, Taylor K. Medicare's Value-Based Payment Initiatives: Impact on and Implications for Improving Physician Documentation and Coding. American Journal of Medical Quality. 2009;24(3):250–8. doi: 10.1177/1062860609332511. [DOI] [PubMed] [Google Scholar]
- Rosenthal GE, Harper DL, Shah A, Covinsky KE. A Regional Evaluation of Variation in Low-Severity Hospital Admissions. Journal of General Internal Medicine. 1997;12(7):416–22. doi: 10.1046/j.1525-1497.1997.00073.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy A, Kim M, Christein J, Varadarajulu S. Stenting versus Gastrojejunostomy for Management of Malignant Gastric Outlet Obstruction: Comparison of Clinical Outcomes and Costs. Surgical Endoscopy. 2012;26(11):3114–9. doi: 10.1007/s00464-012-2301-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schousboe JT, Paudel ML, Taylor BC, Virnig BA, Cauley JA, Curtis JR, Ensrud KE. Magnitude and Consequences of Misclassification of Incident Hip Fractures in Large Cohort Studies: The Study of Osteoporotic Fractures and Medicare Claims Data. Osteoporosis International. 2013;24(3):801–10. doi: 10.1007/s00198-012-2210-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skolarus LE, Morgenstern LB, Zahuranec DB, Burke JF, Langa KM, Iwashyna TJ. Acute Care and Long-Term Mortality among Elderly Patients with Intracerebral Hemorrhage Who Undergo Chronic Life-Sustaining Procedures. Journal of Stroke and Cerebrovascular Diseases. 2013;22(1):15–21. doi: 10.1016/j.jstrokecerebrovasdis.2011.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song Y, Skinner J, Bynum J, Sutherland J, Wennberg JE, Fisher ES. Regional Variations in Diagnostic Practices. New England Journal of Medicine. 2010;363(1):45–53. doi: 10.1056/NEJMsa0910881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taira DA, Seto TB, Siegrist R, Cosgrove R, Berezin R, Cohen DJ. Comparison of Analytic Approaches for the Economic Evaluation of New Technologies Alongside Multicenter Clinical Trials. American Heart Journal. 2003;145(3):452–8. doi: 10.1067/mhj.2003.3. [DOI] [PubMed] [Google Scholar]
- Veterans Administration Health Economics Resource Center. 2013. . “ Diagnosis-Related Group (DRG) Weights (1983-2007) ” [accessed on June 20, 2013]. Available at http://www.herc.research.va.gov/resources/faq_f03.asp.
- Whellan DJ, Greiner MA, Schulman KA, Curtis LH. Costs of Inpatient Care among Medicare Beneficiaries with Heart Failure, 2001 to 2004. Circulation: Cardiovascular Quality and Outcomes. 2010;3(1):33–40. doi: 10.1161/CIRCOUTCOMES.109.854760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuckerman S, Waidmann T, Berenson R, Hadley J. Clarifying Sources of Geographic Differences in Medicare Spending. New England Journal of Medicine. 2010;363(1):54–62. doi: 10.1056/NEJMsa0909253. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.


