Abstract
Trauma remains the leading cause of morbidity and mortality in the United States among children from the age 1 year to 21 years old. The most common cause of lethality in pediatric trauma is traumatic brain injury (TBI). Early coagulopathy has been commonly observed after severe trauma and is usually associated with severe hemorrhage and/or traumatic brain injury. In contrast to adult patients, massive bleeding is less common after pediatric trauma. The classical drivers of trauma-induced coagulopathy (TIC) include hypothermia, acidosis, hemodilution and consumption of coagulation factors secondary to local activation of the coagulation system following severe traumatic injury. Furthermore, there is also recent evidence for a distinct mechanism of TIC that involves the activation of the anticoagulant protein C pathway. Whether this new mechanism of posttraumatic coagulopathy plays a role in children is still unknown. The goal of this review is to summarize the current knowledge on the incidence and potential mechanisms of coagulopathy after pediatric trauma and the role of rapid diagnostic tests for early identification of coagulopathy. Finally, we discuss different options for treating coagulopathy after severe pediatric trauma.
Keywords: Trauma, coagulopathy, children, mechanisms, stratification, treatment
Introduction
Trauma remains the leading cause of morbidity and mortality in the United States among children from the age of 1 year to 21 years old [1, 2]. Compared to adults, children appear to sustain higher rates of blunt than penetrating trauma [3]. Children may also be victims of non-accidental trauma that is often associated with TBI.
Perturbations in blood coagulation have been commonly observed in trauma, and are associated with adverse outcomes in adults as well as children [3-9]. Attempts to define the perturbations in blood coagulation after trauma have been hindered by inadequate measures of coagulation; also there is no common laboratory parameter that defines coagulopathy appropriately. Acute traumatic coagulopathy (ATC) has been described by Davenport as an early endogenous process, driven by a combination of tissue injury and shock that is associated with increased mortality and worse outcome in the severely injured trauma patient. In adults, endothelial activation of Protein C is a central mechanism of ATC, which produces rapid anticoagulation and fibrinolysis following severe trauma [10]. Trauma-induced coagulopathy (TIC) includes not only ATC, but also other mechanisms of iatrogenic coagulopathy (IC), such as dilution, acidosis and hypothermia. It is a global failure of the coagulation system to sustain adequate hemostasis after major trauma. Derangements in coagulation screens identifying hypo- or hypercoagulation, are detectable in the hyper acute phase following severe trauma [10]. As early as 1982, Miner et al. described the presence of at least one coagulation abnormality in 71% of children with head trauma [11]. However, only a limited number of studies have been performed on the incidence of TIC after pediatric trauma. The incidence of coagulation abnormalities on admission reported in these retrospective pediatric studies range widely from 10% to 77 % (Table 1). Expanded knowledge on coagulation status of severely injured children is critical to further improvement of pediatric trauma care. In adults, damage control resuscitation (DCR) strategies have been developed to achieve early aggressive correction of TIC in conjunction with other interventions designed to achieve early hemostasis [12]. These strategies have been accompanied by improved outcomes [13-15]. In contrast to adults, massive bleeding is less common after pediatric trauma. TBI appears to be the common trigger of TIC and mortality in children [16, 17]. The complex pathophysiological mechanisms of the coagulation abnormalities associated with TBI are not yet fully understood, but might differ from coagulation disturbances associated with massive systemic bleeding.
Table 1.
Overview of published studies on coagulopathy after pediatric trauma.
| Study design | Number of subjects | References | Year | Definition of coagulopathy | Incidence of coagulopathy on admission | Study population | Main Results |
|---|---|---|---|---|---|---|---|
| Retrospective | 87 | [11] | 1982 | Abnormal clotting tests/DIC: organ failure + low fibrinogen, ↑ PT and aPTT, ↑ FDP, thrombocytopenia or rapid declining PC | 71% one abnormal clotting test 32% ‘DIC’ and fibrinolysis | Pediatric TBI patients < 2hr of injury | ‘DIC’ is associated with ↑ mortality |
| Retrospective | 147 | [126] | 1997 | Moderately elevated PT >16s. ↑ PT and aPTT, or an elevated PT in conjunction with a low PC , low fibrinogen, and/or a positive FDP | 37% | Pediatric TBI patients evaluated for child abuse, radiological evidence and coag testing with two days | ↑PT and activated coagulation strongly related to presence of parenchymal brain damage. Non-survivors: coagulation abnormalities more frequent and severe. |
| Prospective | 60 | [127] | 2001 | PT, aPTT, low fibrinogen, PC, FDP | 10% DIC | Pediatric TBI patients admitted to PICU with blood draws within 4 hrs of injury | Patients with longer aPTT, ↑ FDP, ↓ fibrinogen and low PC greater risk of a poor outcome/worse GOS |
| Retrospective | 69 | [18] | 2001 | FDP > 1000 g/mL | NA | Isolated TBI patients <16 years | FDP > 1000 μg/mL predicts poor outcome (GOS 1-3) in children with isolated TBI. FDP's are a strong independent prognosticator of outcome in children with GCS between 7 and 12. |
| Retrospective | 830 | [128] | 2001 | INR ≤ 1.2 or aPTT ≥ 33s | 28% | Blunt head or torso trauma < 15 years | Minor elevations on coag studies independently associated with GCS ≤13, ↓SBP, open/multiple bone fractures and major tissue wounds |
| Retrospective | 53 | [129] | 2001 | PT > 14.5, INR > 1.2, aPTT > 38 | 67% of patient with GCS ≤ 14 and 7% with GCS 15 | Pediatric patients with TBI | Patients with GCS ≤ 14 ↑ risk for intracranial injury and coagulopathy. Risk increases inversely with the GCS. A mean of 1 unit of FFP was required in patients with GCS ≤ 14. |
| Retrospective | 122 | [19] | 2002 | DIC: organ failure + low fibrinogen, ↑ PT and aPTT, ↑ FDP, thrombocytopenia or rapid declining PC | 14.8% DIC | Pediatric patients with severe TBI admitted to PICU | Hemocoagulative disorders are predictors of GOS. |
| Retrospective | 521 | [130] | 2007 | PT INR ≥ 1.2 PTT ≥ 33 s PC < 100 × 103 | 51% | Blunt TBI < 15 years with ≥ 2 CT scans | Coagulopathy was associated with worsening CT findings and prognostic for poor outcome. |
| Retrospective | 16 | [131] | 2007 | ↑PT, aPTT, fibrinogen PC, FDP | 50% | Severe TBI < 12 months | Major coagulative alterations had a high positive correlation with GOS. Lesser hematocoagulative disorders did not correlate with outcome |
| Cross-sectional | 301 | [132] | 2007 | PA < 70 % and/or PT>16 s and/or aPTT >10 s when compared to controls and/or PC < 150 × 103 | 77% | Moderate or severe TBI < 17 years requiring ICU admission | Coagulopathy directly associated with trauma severity, but not with a rise in mortality. |
| Retrospective | 58 | [133] | 2009 | PT test < 50% | 29% | TBI and GCS ≤ 8 less than 6 years | Coagulation disorders independent predictor of mortality |
| Prospective Cohort | 57 | [134] | 2010 | Abnormal clotting tests | NA | Children with suspected TBI requiring a head CT | D-Dimer was an independent predictor of brain injury on head CT and was a stronger predictor than initial GCS |
| Retrospective | 320 | [20] | 2011 | PC of < 100 × 103 μL and/or INR > 1.2 and/or aPTT > 36 s | 42.8% | Isolated TBI < 18 years | Low GCS, increasing age, ISS ≥ 16 and intraparenchymal lesions independently associated with TBI coagulopathy |
| Retrospective | 744 | [8] | 2012 | INR ≥ 1.5 | 38.3% | Trauma patients <18 years in combat facility with ISS, INR, BD and mortality data | Coagulopathy and shock independently associated with mortality |
| Retrospective | 200 | [15] | 2012 | PT test <70%, aPTT > 38 s or PC < 100 × 103 μL | 28% | Blunt isolated TBI <14 years | GCS ≤ 8 at scene in isolated TBI is associated with ↑risk for coagulopathy and mortality |
| Prospective | 102 | [9] | 2012 | PT < 15.9 s aPTT < 42.1 s fibrinogen <180 mg/dL or PC < 185 × 103 μL | 72% | Pediatric trauma patients receiving a MTP | No difference in mortality or improved outcome |
| Retrospective | 803 | [3] | 2013 | INR > 1.2 | 37.9% | Level 1 trauma patients < 18 years requiring ICU admission and received coag studies | Coagulopathy is an independent predictor of mortality after trauma. Significant increase in mortality in TBI patients. |
| Retrospective | 86 | [58] | 2013 | NA | NA | Level 1 trauma patients < 14 years admitted to an ICU. | Admission TEG correlated with conventional coag tests and predicted early Tx, early LSI and outcome. |
DIC= Disseminated Intravascular Coagulation. PT= Prothrombin Time. aPTT = Activated partial thromboplastin time. INR= International normalized ration. FDP=Fibrinogen degrading product. PC =platelet count. BD= Base Deficit. TBI= Traumatic brain injury. PICU= Pediatric Intensive Care Unit. ICU=Intensive Care Unit. GOS= Glasgow Outcome Scale. GCS= Glasgow Coma Scale. SBP= systolic blood pressure. ISS= Injury Severity Score. PA: Prothrombin Activity. Tx = Transfusion. LSI=Lifesaving Intervention. CT= Computed tomography. MTP: Massive Transfusion Protocol. TEG= Thromboelastography. NA=Not available.
The goal of this review is to summarize the current knowledge on the incidence and potential mechanisms of coagulopathy after pediatric trauma as well as the role of rapid diagnostic testing for early identification of TIC. Finally, we discuss different options for treating coagulopathy after severe pediatric trauma.
Coagulopathy after pediatric trauma
Over the past decade, a better understanding of TIC and its mechanistic explanations has led to a new therapeutic approach requiring earlier and more aggressive management in adults. Although TIC has long been associated with trauma in children [11], the pediatric population has been understudied and few investigations have been performed to date (Table 1). Recent data from combat support hospitals in Iraq and Afghanistan where children with traumatic injuries were treated revealed an independent association between TIC and shock on admission and higher in-hospital mortality than patients without shock or TIC [8]. The authors used a trauma registry capturing 744 patients under the age of 18 over a 7-year period. The incidence of early TIC and shock were 27% and 38.3% with an associated mortality of 22% and 16.8%, respectively. Coagulopathy was defined as an International Normalized Ratio (INR) ≥ 1.5 and shock as a base deficit of ≥ 6. Strengths of this study include the use of a comprehensive registry from multiple centers, the size of the study population and the analysis of many covariates. The authors acknowledged that the retrospective nature of the analysis potentially introduced a selection bias, since only patients with full datasets on coagulation studies and shock were included. Furthermore, one could argue that the distribution of mechanisms of injury in this population differ widely from pediatric trauma patients treated in civilian hospitals and are therefore not representative: whereas 43% of children in the studied cohort suffered from injuries resulting from explosion, 26% from gunshot wounds and only 10% of patients sustained a motor vehicle accident. Regardless, this study illustrates an association between TIC and worse outcomes for pediatric patients who sustain severe traumatic injury.
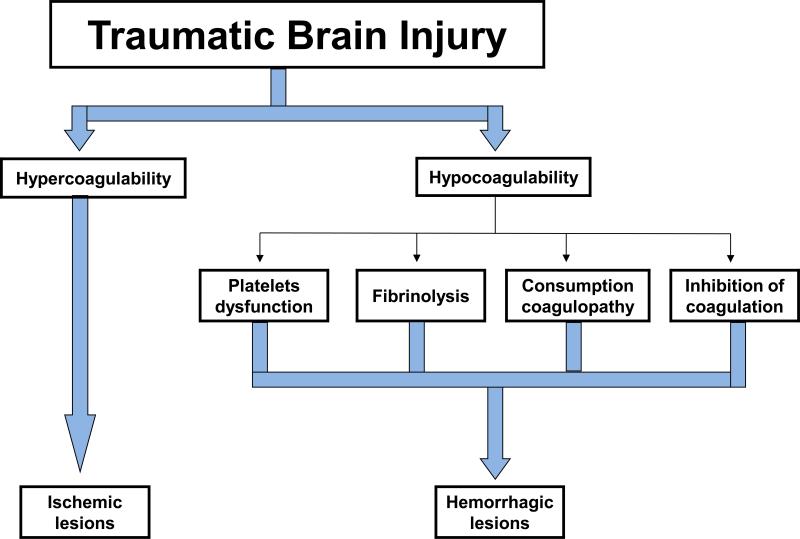
Several studies have evaluated the relationship between TIC and outcome in the civilian pediatric trauma population. A prospective study performed by Hendrickson et al. evaluated TIC in 102 civilian pediatric trauma patients and found a high prevalence of coagulation abnormalities in children requiring a least one blood product in the first 24 hours of admission [9]. The prothrombin time was abnormal in 72%, partial thromboplastin time in 38%, fibrinogen in 52%, hemoglobin in 58%, and platelet count in 23%. Furthermore, abnormal prothrombin time, partial thromboplastin time, and platelet count were strongly associated with mortality and remained significantly associated in the multivariate analysis after adjusting for injury severity score. As TIC is particularly prevalent in pediatric patients with TBI, several studies have examined the relationship between TIC and outcome in this patient population. For example, Vavilala et al. reported that fibrin degradation product levels over 1000 μg/mL on admission predicted a poor outcome in children under the age of 16 with a Glasgow Coma Score (GCS) between 7-12 with isolated head injury [18]. Chiaretti et al. also showed that coagulation abnormalities were associated with poor outcome including both mortality and long-term neurologic deficit [19]. Furthermore, Talving and colleagues reported an incidence of TIC exceeding 40% in a retrospective study of 320 children sustaining isolated TBI [20]. The mortality rate was 17.5% versus 0.5% in coagulopathic versus noncoagulopathic patients, respectively. However, after logistic regression to adjust for confounders, no statistically significant mortality difference in patients with and without TIC was noted. The Talving study concluded that a low GCS, a high Injury Severity Score (ISS) and increasing age were independently associated with TBI coagulopathy. This age related factor suggests that physiological derangements occurring early after TBI and contributing to TIC may be better tolerated in early childhood. These results were not replicated in subsequent studies. Peinigner et al., in a retrospective analysis of 200 datasets from the German trauma registry, found that the GCS was predictive of hemocoagulative disorders after blunt head trauma. Children with an initial GCS ≤ 8 who presented with TIC on admission to the hospital showed an increased risk for mortality [15]. Finally, our research group has recently shown in a retrospective 10-year review of 803 children after severe trauma that early coagulopathy, defined as an INR ≥ 1.2 at presentation, is an independent predictor of mortality [3]. The increase in mortality was particularly significant in patients with TBI, either isolated or combined with other injuries. Although these studies describe an association between severe TIC and increased mortality after severe pediatric trauma, the retrospective nature of these studies precludes statements of causality. Whether TIC is simply a marker of severe trauma (particularly brain trauma), or, in fact, contributes to secondary injury is uncertain. Several mechanisms have been evoked to explain the coagulation abnormalities associated with TBI (Figure 1). TBI causes a combination of both hypo-and hypercoagulable states, caused by the traumatized brain tissue [21]. Additionally, it has been hypothesized that TBI causes a local release of tissue factor from the injured neurons that is associated with activation of the protein C pathway, thus triggering the release of anticoagulant mediators [4]. However none of these hypotheses has yet been proven in prospective clinical studies. In summary, the mechanisms behind the development of TIC in pediatric trauma patients have not been fully elucidated and no study to date has shown evidence for outcome improvement after correction of the TIC in children.
Figure 1. Current hypothesis for the development of coagulation abnormalities after blunt traumatic brain injury.
A combination of hypocoagulable and hypercoagulable states triggered by the extent of brain injury will lead to secondary injury by way of ischemic and hemorrhagic lesions. Figure modified from [123].
Differences between the adult and pediatric hemostatic systems
Determining the extent of TIC requires reliable testing and an understanding of the physiology of hemostasis in pediatric patients. The hemostatic system develops in utero and evolves over the first few months of life, leading up to maturational differences of many levels of coagulation factors. This inevitably also leads to differences in the normal ranges of coagulation screening tests for very young infants as compared to adults. A series of papers by Andrews et al. in the late 1980's describes the differences between the pediatric and adult hemostatic systems, and how age-related changes occur as the hemostatic system matures [22-25].
In healthy children from 1 to 16 years old, the hemostatic system has reached a higher degree of maturation. The screening tests consisting of prothrombin time (PT), activated partial thromboplastin time aPTT, and fibrinogen are almost identical to those of adults. However, mean values of seven coagulant proteins (II, V, VII, IX, X, XI, XII) in children might still be significantly lower than adult values [22, 26, 27] and the PT might be slightly prolonged because plasma prothrombin concentrations during childhood can be 10% to 20% lower than for adults, along with factor VII levels [25, 26]. Plasma concentrations of anti-thrombin (AT), protein C (PC) and protein S (PS), all major inhibitors of the coagulation system show low levels at birth. The mean values for PS and AT are similar to those in adults by 3 and 6 months of age respectively, whereas PC is still markedly lower at 6 months of age [23, 24]. Lower values of tissue factor pathway inhibitor (TFPI) have been observed in newborns [28].
Although all key components of the fibrinolytic system are present at birth, important age-dependent quantitative and qualitative differences can be observed in children. The major age-dependent differences include decreased plasma concentrations of plasminogen, tissue plasminogen activator (t-PA) and α-antiplasmin (α2-AP), increased plasma concentrations of plasminogen activator inhibitor-1 (PAI-1), as well as a decrease in both plasmin generation and overall fibrinolytic activity [29].
Limited studies are available on platelet count and function in children; most have been performed in neonates or young infants. Platelet counts have been studied in young healthy infants of varying ages and it appears that they are significantly higher at 2 months and lower at both 5 and 13 months [30]. Differences in platelets between healthy neonates and adults in regards to their response to platelet agonists have also been described. Initial platelet aggregation using flow cytometry consistently demonstrated that platelets from neonatal cord blood were less responsive than adult platelets to agonists such as adenosine 5’diphosphate, epinephrine, collagen, thrombin and thromboxane analogs [31]. The mechanism(s) underlying these differences are still poorly understood, although it has been suggested that the hyporesponsiveness to epinephrine is probably due to the presence of fewer α2-adrenergic receptors [32]. In addition, the reduced response to collagen likely reflects the impairment of calcium mobilization [33], and the decreased response to thromboxane may result from differences in signaling downstream from the receptor in neonatal platelets [34].
Studies of primary hemostasis revealed significantly shorter bleeding times in healthy neonates compared to adults [22]. Other studies using a platelet function analyzer found shorter closure time in neonates than adults [35]. This apparently paradoxical finding of enhanced primary hemostasis in the face of platelet hypoactivity has been attributed to the higher hematocrit levels, higher mean corpuscular volumes, and higher von Willebrand factor concentrations in the blood of neonates [22]. Whether this in vitro platelet hyporeactivity of neonates translates into poor platelet reactivity under in vivo conditions is not well known.
The thrombin hemostasis system might also differ in children. It has been observed that the capacity to generate thrombin in vitro by a chromogenic assay is decreased by 26% in plasma from children aged 1 to 16 years compared to adults; this would justify the lower prevalence of thromboembolic complications in this period [36]. When compared to adult reference ranges, children ages 1 to 5 might display higher values of soluble thrombomodulin, thrombin-antithrombin complex and D-dimer [37].
Taken together, the results of these studies indicate some variability in the maturation of the different coagulation proteins and of the functional activity of platelets in young children. However, the susceptibility to bleeding is based upon the contextuality of the entire hemostatic system as evaluated by coagulation monitoring devices assessing the viscoelastic properties of whole blood and platelet function testing and not just on coagulation factor and anti-coagulation factor balance changes over time.
Early detection of TIC after pediatric trauma
The basic precondition for adequate management of a coagulation problem in the acute phase after trauma is timely recognition. Scoring systems and algorithms have been developed to evaluate severely injured patients to help guide activation of massive transfusion protocols. These systems are limited by their retrospective design. An alternative for early identification of TIC is through point of care evaluation of coagulation status [38]. A number of tests are available to assess coagulation in the pediatric population; standard coagulation monitoring comprises the early and repeated determination of conventional coagulation tests (CCT) such as PT, aPTT, INR, and fibrinogen. It is frequently assumed that these CCTs monitor coagulation; however, these tests monitor only the initiation phase of blood coagulation and represent only the first 4% of thrombin production [39]. It is, therefore, possible that the conventional coagulation screen appears normal, while the overall state of blood coagulation is abnormal [40-42]. Moreover CCT, originally developed for the guidance of anticoagulation therapy or management of certain disease states, assess only plasma-based components of the coagulation system and do not account for the contribution of the endothelium and cellular components of blood. Also, the detection of hypercoagulability is limited by the use of CCT. As the majority of trauma patients become hypercoagulable it would be important to use coagulation monitoring devices, such as thromboelastography, that have been shown to accurately assess hypercoagulation in other conditions [43].
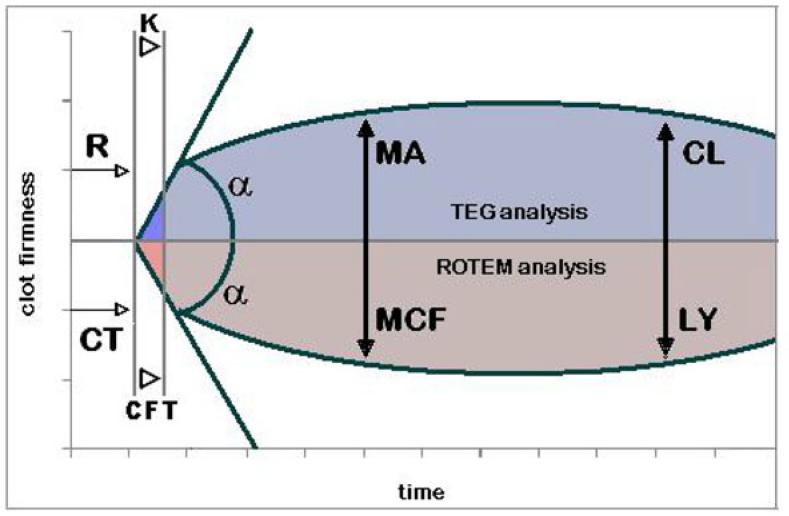
Increasing emphasis focuses on the importance of coagulation monitoring devices assessing the viscoelastic properties of whole blood and platelet function testing, i.e., thromboelastography (TEG®), rotation thrombelastometry (RoTEM®), and impedance aggregometry (Multiplate®; DiaPharma, West Chester, Ohio). (Table 2 and Figure 2). TEG/RoTEM® measure and graphically display the changes in viscoelasticity at all stages of the developing and resolving clot, starting with fibrin formation and continuing on through clot retraction and fibrinolysis with minimal delays. Furthermore, the coagulation status of patients is assessed in whole blood, providing a functional assay that allows the plasma-based coagulation system to interact with platelets, red cells and white blood cells, thereby providing useful information on platelet function [44]. In addition, with the development of the Multiplate® device and FDA clearance for two of its tests, a rapid point of care platelet function testing will soon become available clinically and has successfully been used in research studies to identify platelet dysfunction in adult trauma patients [45]. A major benefit of these assays is their ability to evaluate the coagulation system in whole blood, which may improve the accuracy of monitoring hemostasis.
Table 2.
Viscoelastic tests available for the pediatric trauma population.
| Test | Definition | Hemostatic phase | Cause for abnormalities | Intervention | Studies on the use of viscoelastic tests after pediatric trauma | ||
|---|---|---|---|---|---|---|---|
| TEG® Assay time: 10-15 min | RoTEM® Assay time: 5-10 min | TEG® | RoTEM® | ||||
| R | CT | Time from initiation of test until the beginning of the clot formation | Initiation of coagulation | Prolonged R/CT: -Factor deficiencies -Anticoagulants Short R/CT: -Plasma hypercoagulability |
Plasma | Admission rapid TEG results correlate with conventional coag tests and predict early transfusion, early LSI and outcome. [58] Report on TEG guided hemostatic resuscitation [135] | Age related reference ranges established in children [61] Report on Successful RoTEM-guided Hemostatic therapy after blunt trauma. [80] |
| K | CFT | Time from start of the clot formation to the curves reaches amplitude of 20 mm | Amplification of coagulation | Prolonged K/CFT: -Factor deficiencies -Hypofibrinogenaemia -Thrombocytopenia -Platelet dysfunction |
Cryoprecipitate | ||
| α | α | Angle between baseline and the tangent to the curve through the starting point of coagulation | Propagation of coagulation ‘Thrombin burst’ | Low α -Factor deficiencies -Hypofibrinogenaemia -Thrombocytopenia -Platelet dysfunction |
Cryoprecipitate | ||
| MA | MCF | Amplitude measured at max curve width | Low MA/MCF -Hypofibrinogenaemia -Thrombocytopenia -Platelet dysfunction -FXIII deficiency |
Platelets (consider FXIII concentrate if ongoing bleeding and persistently low MA/MCF) | |||
| LY | ML | Reduction in area under curve (LY) or in amplitude (ML) from the time MA/MCF is achieved until 30 or 60 min after MA/MCF | Fibrinolysis | Increased LY/ML - Hyperfibrinolysis |
Antifibrinolytics | ||
Table modified from [136]
Figure 2. Typical tracings of viscoelastic coagulation devices.
A, upper side: Thrombelastograph (TEG®) tracing: r = reaction time; K = kinetics; α = slope between r and k; MA = maximum amplitude; CL = clot lysis. B, lower side: Rotation Thrombelastography (RoTEM®) tracing: CT = clotting time; CFT = clot formation time; α = slope of tangent at 2 mm amplitude; MCF = maximal clot firmness; LY = Lysis. Figure modified from [105].
Early variables of clot firmness assessed by viscoelastic testing, such as thromboelastography have been shown to be good predictors for the need for massive transfusion, the incidence of thrombotic/thromboembolic events and for mortality in adult surgical and trauma patients [42, 46-55]. The delay in detection of TIC can influence outcome and the turn-around time of viscoelastic devices (TEG/RoTEM®) has been shown to be significantly shorter by 30 to 60 minutes compared to conventional laboratory testing in both adult and pediatric patient populations [42, 56, 57]. Data on the measurement of viscoelastic properties of whole blood in children after trauma are limited. An initial study detailing the use of viscoelastic devices has recently been described in 86 children sustaining severe trauma [58]. Interestingly, rapid TEG was used in that study which produced faster results than conventional TEG measurements. Similarly, the use of interim ROTEM® values (A10) have been shown to provide an early and specific assessment of coagulation status after trauma in adult patients in order to guide resuscitation [59]. These investigators described results comparable to adult studies [50, 60] with admission data correlating with CCT and predicting early transfusion and outcome. Thus, although normal values of viscoelastic properties of whole blood have been established in healthy children of all ages for thromboelastography, thromboelastometry and impedance aggregometry [61-64], carefully designed prospective trials on the use of these global measurements of hemostasis are warranted to obtain a more detailed description of the coagulation abnormalities that occur post-trauma in this special population.
Potential mechanisms of TIC after pediatric trauma
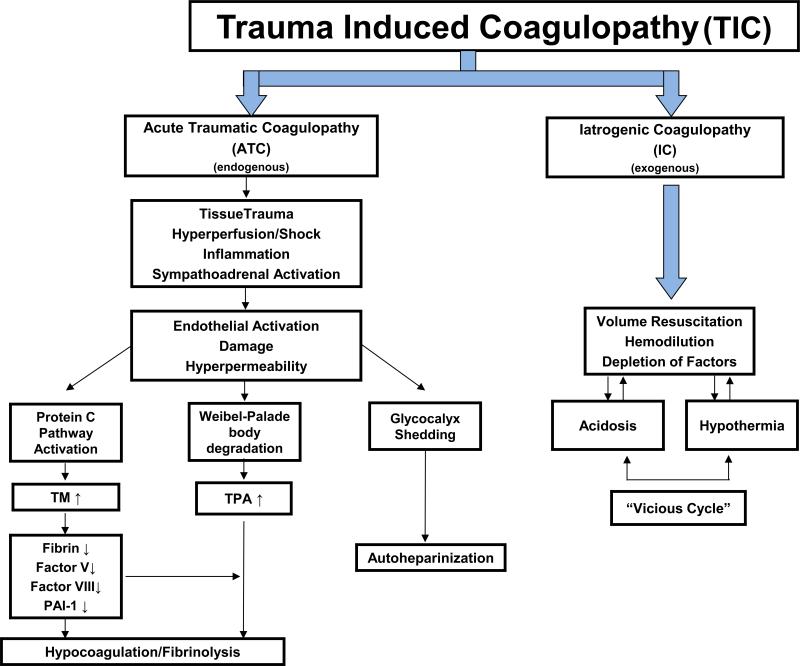
There are several potential mechanisms that contribute to the development of TIC. Much adult trauma literature details mechanisms and drivers of TIC, but there are only limited descriptions characterizing these mechanisms in pediatric trauma. The principal mechanistic drivers are summarized in Figure 3. As the number of aforementioned drivers of TIC mount following injury, the probability of life-threatening coagulopathy increases exponentially. Previous studies have shown that the conditional probability of developing TIC with moderate injury without the presence of additional triggers for coagulopathy is 1%. However, with increased ISS > 25 and hypotension, the probability increases to almost 40%, and in cases with ISS > 25, hypotension, hypothermia, and acidosis, the probability of developing TIC increases to 98% [65].
Figure 3. Potential mechanisms involved in the trauma-induced coagulopathy in children.
There is much adult literature detailing mechanisms and drivers of acute traumatic coagulopathy (ATC) and iatrogenic coagulopathy (IC). The classical physiologic drivers include hypothermia, acidosis, dilution secondary to intravenous administration of crystalloids and consumption of coagulation factors and might be similar between children and adults, although there is a limited description of these mechanisms in pediatric trauma. There is recent evidence for a distinct mechanism for early ATC in patients who have not been exposed to the traditional coagulopathy triggers and that may involve the activation of the anticoagulant protein C pathway, the Weibel-Palade body degradation and glycocalyx shedding. Whether these new mechanisms of ATC play a role in children is still unknown. TM: Thrombomodulin, TPA: tissue plasminogen activator, PAI-1: plasminogen activator inhibitor −1. Figure modified from [76] and [124].
Physiologic and iatrogenic dilution in trauma patients when present can act as an additional mechanistic driver of TIC. In times of hypotension, physiologic or iatrogenic dilution potentiates the osmotic activity of plasma leading to a shift of extravascular water into the intravascular space. Until equilibrium is reestablished, this osmotic activity causes a proportional dilution of plasma proteins and coagulation factors adversely affecting their subsequent interactions. Monroe et al. modeled the action of factor VIIa in dilutional coagulopathy and demonstrated a calculated reduction in single factor concentration of 37% resulting in a 75% reduction in overall factor complex activity [66]. The effects of iatrogenic dilution in trauma were nicely demonstrated in a study of patients from the German Trauma Society Database (TR-DGU). Investigators observed TIC upon emergency room (ER) admission in greater than 40% of patients receiving more than 2000 mL in transport, in greater than 50% of patients with more than 3,000 mL in transport, and in 70% of patients with more than 4,000 mL of fluid administered in the pre-hospital phase of care [67]. This dilution is accompanied by consumption and inactivation of coagulation factor substrates and coagulation enzymes of varying magnitudes depending upon the degree of individual injury [68].
In addition to dilutional mechanisms of TIC, the effects of temperature and pH on coagulation factor and complex activity have also been well described. The pace of coagulation factor reactions is affected by hypothermia and acidosis. Kermode et al. and Jurkovich et al. have demonstrated that coagulation interactions are slowed down by approximately 5% with each degree Celsius drop in temperature. Similarly, the critical interactions between factors and glycoproteins that activate platelets are absent in 75% of individuals at 30 degrees Celsius [69, 70]. A reduction in pH to 7.2 has been shown to reduce coagulation factor complex activities by 50% with activity falling to 20% of normal at a pH of 6.8 [71].
Fibrinolysis is another important mechanism controlled by the coagulation system, which plays a role in TIC. The coagulation system modulates fibrinolysis maintaining stable blood clots for the time necessary to control bleeding. In the normal setting, high concentrations of thrombin inhibit plasmin activation by the activation of thrombin-activated fibrinolysis inhibitor (TAFI) and PAI-1. However hypothetically, in the setting of trauma, if the thrombin burst is not robust, TAFI remains inactivated allowing thrombin to bind to thrombomodulin on endothelial cells leading to protein C activation, subsequent Factor V, VII, and PAI-1 inactivation, and increased fibrinolysis. Hyperfibrinolysis has been identified as a significant risk factor for mortality in bleeding trauma patients [72, 73].
Over a quarter of adult trauma patients demonstrate detectable coagulopathy on arrival to the emergency department before the development of the classic triad of hypothermia, dilution, and acidosis. Brohi and colleagues, in a large prospective study of 209 patients presenting with a severe trauma (ISS equal or more than 16) and meeting the criteria for the highest trauma activation, documented the development of TIC within one hour after injury in approximately 30% of patients. In this study, patients arriving coagulopathic had significantly increased mortality of 40% [5]. Other authors subsequently reported similar findings [6]. In the study by Brohi et al., potential mechanisms for TIC were also evaluated. In this cohort of severely injured adult patients, plasma levels of protein C zymogen were found to be depleted on admission to the hospital [4]. More recent data from the same investigators showed that in a similar group of 200 adult trauma patients, the combination of tissue injury, elevated ISS, and shock was associated with TIC nearly immediately after their injury [74]. They found TIC was strongly correlated with the activation of the protein C pathway. Further evidence for protein C activation is demonstrated by the fact that they also found a strong inverse correlation between plasma levels of activated Protein C (aPC), factor Va and VIIIa inactivation and the derepression of fibrinolysis. Activated protein C directly inhibits PAI-1, which usually serves to limit t-PA activity. Without the limitation of PAI-1, tPA is free to enhance the conversion of plasminogen to plasmin and thereby enhance fibrinolysis. In summary, aPC exerts its profound anticoagulant activity by inhibiting coagulation and through derepression of fibrinolysis [4].
The possible mechanistic role of the protein C pathway in the development of TIC was also demonstrated in a mouse model of trauma-hemorrhage [75]. Mice subjected to a pressure-controlled hemorrhage to a MAP of 40 mmHg for 60 min developed a severe metabolic acidosis (BD > 10), were hypocoagulable (had an increase in their aPTT) and had a significant increase in their plasma levels of aPC. The aPTT returned to normal values 12h later. When mice were pretreated with an antibody that blocks the anticoagulant domain of aPC it reversed the coagulopathy induced by severe trauma, indicating that the activation of the protein C pathway might play a mechanistic role in TIC.
Another potential driver of TIC is the disruption of the vascular endothelium and its glycocalyx following trauma due to hypoperfusion, tissue trauma, inflammation and sympathoadrenal activation. Significant levels of heparin-like compounds exist in the non-circulating plasma of the glycocalyx and may be released with its disruption [76]. Evidence supporting this mechanism was revealed in a prospective study of 77 adult trauma patients with auto-heparinization by TEG, which was likely related to endothelial glycocalyx degradation, as exhibited by increased syndecan-1, thrombomodulin and interleukin-6 levels [77].
One would assume that certain physiologic drivers would be similar between children and adults, including hypothermia, acidosis, dilutional effects and consumption of coagulation factors. However, on a more detailed level, minimal literature exists on a pediatric patient's response to significant traumatic tissue injury and the release of inflammatory markers and anticoagulation factors, like aPC, which may interfere with coagulation and hemostasis. A detailed description of the mechanistic changes in the coagulation system associated with severe trauma has not been performed in the pediatric population and will require further investigation.
Treatment options for TIC in pediatric trauma
Administration of procoagulant concentrates
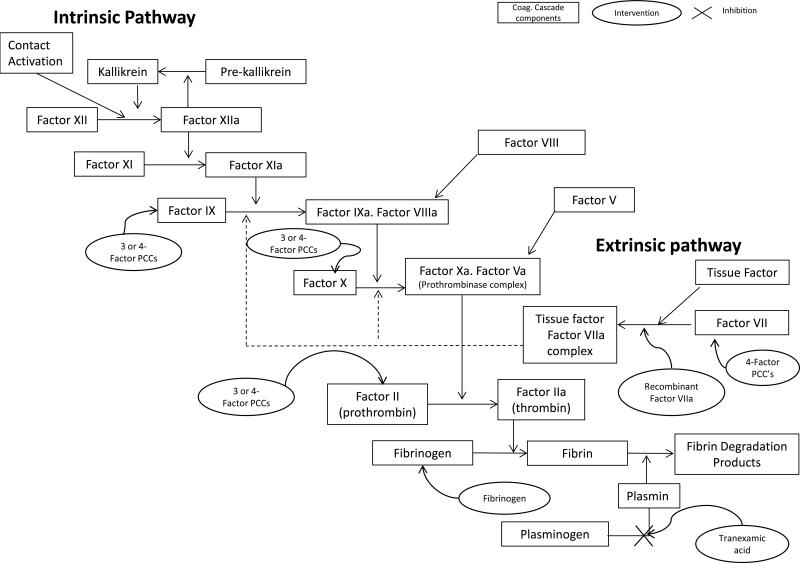
In adults, DCR strategies have been developed to achieve an early aggressive correction of TIC [12, 78]. This strategy has been accompanied by improved outcomes [13-15]. We hypothesize that in pediatric patients with coagulopathy that is rapidly identified and amenable to correction a goal-directed approach to resuscitation may be more appropriate than an empiric blood product approach. The most important procoagulant concentrates include fibrinogen concentrate, prothrombin complex concentrate (PCC), recombinant factor VIIa (rFVIIA) and antifibrinolytics such as the tranexamic acid. The effect of these adjuvant interventions has not been systematically studied in the pediatric population. The use of these hemostatic agents in a goal-directed fashion guided by TEG/RoTEM monitoring to assess effectiveness and avoid potential thromboembolic complications make for a compelling therapeutic strategy (Table 3 and Figure 4).
Table 3.
Published studies of treatment regimens for coagulopathy following pediatric trauma.
| Intervention | Study design | Number of subjects | References | Year | Study population | Main Results |
|---|---|---|---|---|---|---|
| PCC | Case Report | 1 | [88] | 2011 | 8 kg infant with liver trauma and severe hemorrhage | Patient with acidosis (pH 6.67) and severe anemia (Hb 4 mg/dL). Poorly controlled bleeding despite surgical intervention, FFP and platelets. Vit K and 30 IU/kg PCC administered, with rapid cessation of bleeding and INR ↓ from 2.9 to 1.5. |
| rFVIIa | Case Reports | 3 | [84] | 2003 | 5 wks, 20 mo and 1 yr old with (T)BI | One patient received rFVIIa (bolus of 90 μg/kg) after failing of repeated FFP to correct coagulopathy; two patients received rFVIIa as initial therapy. Two of three children had good neurologic outcomes; third progressed to brain death. No thrombotic complications; intracranial devices placed w/o intracranial hemorrhage. |
| rFVIIa | Retrospective case series | 135 | [83] | 2009 | Pediatric patients receiving rFVIIa | Median transfusion volume decreased in the 24 hours after rFVIIa vs. prior 24 hrs. (11.7 mL/kg vs. 29.7 mL/kg). Mortality lower in surgical/trauma patients (16%) compared to medical patients (58%). Three thrombotic events resulted in two deaths. |
| Fibrinogen | Case Report | 1 | [80] | 2013 | 20 kg, 7 year old with severe abdominal and pelvic trauma | EBL of >70 mL/kg. Goal-directed therapy with ROTEM resulted in administration of 2 g fibrinogen and 3 u of RBC with no FFP or platelets. The ratio of intra-operative fibrinogen concentrate (g) to RBC (U) was 0.7 |
| MT | Prospective | 53 | [110] | 2012 | Pediatric trauma patients | Outcome data compared before and after institution of pediatric MTP. Median FFP: RBC ratio was higher after MTP (1:1.8 vs. 1:3.6). Time to FFP dosing decreased 4-fold with MTP. No difference in mortality. |
| MT | Prospective cohort | 55 | [113] | 2012 | Pediatric patients requiring un–cross-matched blood | Coagulopathy, aPTT >36 s associated with initiation of MTP. ISS for the MTP group was 42 vs 25 for the non–MTP group. More thromboembolic complications in the non–MTP group. No difference in mortality. |
| Therapeutic | ||||||
| Level IV | ||||||
| MT | Retrospective cohort | 105 | [114] | 2013 | Pediatric trauma patients < 18 yo requiring massive transfusion | Higher plasma/RBC and platelet/RBC ratios were not associated with increased survival. |
PCC= Prothrombin Complex Concentrate. FFP=fresh frozen plasma INR= International Normalized Ratio. TBI= traumatic brain injury. rFVIIa= recombinant Factor VII. U=unit. EBL= estimated blood loss. MT= Massive Transfusion. MTP=massive transfusion protocol. RBC=red blood cell.. aPTT = Activated partial thromboplastin time. ISS= Injury Severity Score.
Figure 4. Treatment of acute traumatic coagulopathy in children.
This cartoon represents the coagulation cascade and the effect of potential therapeutic approaches for treating acute traumatic coagulopathy in children. PCC: prothrombin complex concentrate. Figure modified from [125].
Fibrinogen concentrate
Fibrinogen concentrate (HaemocomplettanP/RiaSTAP, CSL Behring, USA) has been marketed for a number of years for the treatment of congenital hypofibrinogenemia, but has been advocated as a fibrinogen replacement therapy for patients requiring massive transfusion [79]. It is produced from pooled human plasma by fractionation and undergoes inactivation steps; it has a fibrinogen concentration of around 20 mg/ml. Despite the evidence supporting maintenance of adequate fibrinogen levels in bleeding patients, little data is available on the administration of fibrinogen concentrate to trauma patients. In pediatric trauma, the use of a fibrinogen concentrate was recently reported in a seven-year-old patient with severe abdominal and pelvic trauma [80]. On arrival to the emergency department, he received 250 mL red blood cells (RBC), 250 mL crystalloid and 0.5 g fibrinogen concentrate, which were given pre-emptively. He then underwent goal-directed hemostatic therapy using RoTEM®. A total of 2 g fibrinogen was administered, while fresh frozen plasma (FFP) and platelets were avoided. Despite an estimated blood loss of >70 mL/kg, the patient received only 3 Units of RBC. The ratio of intra-operative fibrinogen concentrate (g) to RBC (U) was 0.7, which is similar to the ratio of 0.9 described by Schochl when looking at thromboelastometry-guided coagulation factor concentrate based therapy versus FFP in adult trauma [81]. Fibrinogen or cryoprecipitate (for fibrinogen replacement) received a grade 1C recommendation in a recent European guideline for management of traumatic bleeding in adult patients with thromboelastometric signs of fibrinogen deficiency or a fibrinogen level of less than 1.5-2.0 g/L and significant bleeding [82].
Recombinant Factor VIIa
Recombinant Factor VIIa (rFVIIa) was initially developed for treatment of hemophilia and acquired inhibitors, but off-label use of rFVIIa has become increasingly prevalent. rFVIIa has a more developed presence in the pediatric literature than that of the other factor concentrates. Its effectiveness in neonates, infants and children with TIC and clinically significant bleeding, as well as complications following its administration in pediatric patients have been described in several reports. A retrospective case series of 135 pediatric patients receiving rFVIIa for off label use revealed its potential for clinical utility in the setting of surgery and trauma. In this case series, 15 patients received rFVIIa for trauma, 19 patients for surgical bleeding, 16 patients for procedural prophylaxis and 28 patients for bleeding resulting from disseminated intravascular coagulation/sepsis. There was a decrease in 24-hour median transfusion volume after rFVIIa administration. Surgical patients had control of life-threatening bleeding with low associated mortality. Indeed, the mortality rate was significantly lower in the surgical/trauma patients (16%) in comparison to medical patients (58%). Major thrombotic events were seen in 3 patients after rFVIIa, resulting in two deaths and one leg amputation [83]. Another case review study on pediatric patients suffering from severe TIC after cerebral injury reports a rapid correction of hemostatic abnormalities after administration of a bolus of 90 μg/kg rFVIIa in three children aged 5 weeks, 20 months and 11 years [84].
Dosing recommendations in the pediatric-aged patient are extrapolated, in part, from the adult literature, supplemented by the pediatric hemophiliac population. Bolus doses have ranged from 40 - 100 μg/kg in the non-hemophiliac pediatric population. With ongoing bleeding or risk for bleeding, repeat doses at intervals of two to six hours have been administered. In addition to bolus dosing, continuous infusion (20-30 μg/kg/h) following the bolus to maintain hemostatic levels of rFVIIa have been reported. Compared to adults, the pharmacokinetics in pediatric patients demonstrates a shorter half-life and an increased clearance [85]. In addition to its effects on coagulation function, recent data reports enhanced platelet function [84], suggesting a potential role in patients suffering from qualitative platelet disorders, which may include severely injured pediatric trauma patients, more specifically brain-injured children. However, some limitations in the use of rFVIIa have been observed in adults. Data from 21 institutions and 380 patients was collected from the Western Trauma Association web based registry and revealed several indicators of poor response to rFVIIa, including acidosis (pH < 7.2), thrombocytopenia (platelets < 100,000) and hypotension (systolic </= 90). Based on these results, maximal benefit cannot be achieved with administration late in the treatment of a hemorrhaging trauma patient [86].
Prothrombin complex concentrate
Prothrombin complex concentrate (PCC), also referred to as factor IX complex, is derived from pooled human plasma and contains 25-30 times the concentration of clotting factors as FFP. Four-factor PCCs contain factors II, VII, IX and X, while 3-factor PCCs contain little or no factor VII. Depending on the formulation, PCCs may additionally contain protein C, protein S, anti-thrombin and low dose heparin [87]. Most formulations available in the United States are 3-factor PCCs and are approved for prevention and control of bleeding in patients with hemophilia B. However, due to the availability of highly purified and recombinant factor IX products, PCCs are rarely used for this indication. There have been no controlled clinical trials evaluating the use of PCC in massive bleeding; recommendations are generally based on retrospective or observational studies, case reports, and expert opinion [87]. Literature regarding use of PCC in the pediatric trauma patient is scarce. One case report described an 8 kg infant with liver trauma and severe hemorrhage who was acidotic (pH 6.67) and severely anemic with a hemoglobin of 4 mg/dl [88]. The patient underwent two surgical procedures and transfusion of packed RBCs, platelets, and FFP. Following the second operation, the infant continued to bleed despite the administration of FFP, platelets, and red blood cells. Vitamin K and 30 IU/kg PCC were administered due to ongoing hemorrhage, at which point there was a rapid cessation of bleeding and the INR decreased from 2.9 to 1.5.
The variability in factor concentration between formulations creates challenges in standardization of dosing. When using the package information regarding dosing recommendations for hemophilia B, an expected increase in factor IX between 20-50% would occur with a dose of 20-50 units/kg [89]. Similarly, Australasian guidelines recommend a dose of 25-50 units/kg of 3-factor PCC to reverse INR following administration of vitamin K antagonists [90]. Caution must be exercised in administration of these agents due to their activity as potent pro-coagulants [91]. Patanwala recommended a maximum cumulative dosage of <50 units/kg due to the risk of thromboembolism [89]. While some studies have shown benefits of PCC, there is currently only level 2C evidence (GRADE working group) for its usage in patients with massive bleeding in concert with FFP [87]. In the European guidelines for management of traumatic bleeding, it is only recommended for the emergent reversal of vitamin-K dependent anticoagulants (grade 1B recommendation) [92]. In order for stronger recommendations to be developed for use in hemorrhage secondary to trauma, there is a need for randomized studies to evaluate outcomes following administration, especially in children.
Tranexamic acid
Tranexamic acid (TXA), an anti-fibrinolytic agent, is a synthetic lysine analog that functions by competitive inhibition of the enzymatic activation of plasminogen to plasmin, responsible for the degradation of fibrin. The Clinical Randomisation of an Antifibrinolytic in Significant Hemorrhage (CRASH-2) investigators revealed a significant decrease in death secondary to bleeding when TXA was administered early following trauma. Despite this favorable outcome, several gaps in knowledge regarding the use of TXA in trauma were identified in a recent review by a United States Department of Defense Committee. Many issues raised are important in the pediatric population as well, including the need for: (1) a more clear cut identification of which patients might benefit from TXA, (2) development of animal models to establish efficacy and safety, and (3) further evaluation of the safety profile of TXA given the increased risk for thrombotic events and the lack of data regarding safety in children [93]. A 2008 systematic review analyzing the use of TXA in pediatric patients undergoing spine surgery revealed six studies. TXA led to a modest decrease in volume of blood transfused, but not the number of patients requiring transfusion. No deaths or major adverse events were reported, however, the number of patients was too small and follow-up duration too brief to draw conclusions regarding safety [94]. Similar results have been found in pediatric cardiac literature [95].
The Royal College of Paediatrics and Child Health (RCPCH) and the Neonatal and Paediatric Pharmacists Group (NPPG) Medicines Committee published an evidence statement in November 2012 addressing the use of TXA for major trauma in children in response to CRASH-2. This Evidence Statement strongly encouraged the need for on-going research into the use of TXA in the pediatric population, but offered pragmatic dosing guidelines based on extrapolation from adult literature, as published use of TXA in pediatric patients has revealed wide variability in dosing. The recommendation by this group was a 15 mg/kg loading dose (max 1 g) over 10 minutes followed by 2 mg/kg/h for at least 8 h or until bleeding stops. As no indication recommendations were given, the group urged caution with administration of TXA in the pediatric trauma population, as a potential risk of thrombosis exists [96]. This stance was supported Reade and colleagues who encouraged the further evaluation of the safety and efficacy of TXA in trauma patients prior to its universal protocolized use [97].
Transfusion of blood and plasma
Massive blood transfusion
In the adult trauma setting, resuscitation strategies have evolved with a trend toward the early and liberal use of blood products, including RBC, FFP and platelets in patients with hemorrhagic shock. Several studies have supported the use of a 1:1:1 platelet to FPP to RBC ratio when transfusing severely injured patients [13, 14, 98, 99]. However, the results of these studies may have been affected by survival bias [100-103]. Other published studies have not shown any improvement in survival utilizing this approach [104-106]. In contrast, two recent studies have still shown a benefit of using a high FFP-blood ratio after adjusting for survival bias [107, 108]. Regardless of these results, a higher ratio transfusion approach has been adopted at the majority of level 1 adult trauma centers and prospective, randomized controlled trials are currently underway to determine optimal ratios for patients with severe hemorrhagic blood loss [109].
Massive transfusion in children is uncommon, and in non-neonatal pediatric patients, transfusion guidelines are similar to those in adults. In children, because blood volume varies per age, gender and weight [110-112], it is unclear as to what constitutes a massive transfusion. Moreover, the response to massive bleeding in children is thought to differ from the adult response because of their greater physiological reserve and an improved tolerance of blood loss [113]. Data analyzing the effects of a balanced ratio of blood product component administration in massive transfusion is limited in pediatric populations. To date, only three single center studies have been reported on experience with massive transfusion protocol (MTP) in pediatric patients (Table 3). A prospective study on 102 pediatric trauma patients was completed following the institution of a pediatric MTP and outcomes compared with a time period prior to protocol implementation [110]. Following MTP institution, the median FFP:RBC transfusion ratio was 1:1.8 compared with a ratio of 1:3.6 in the pre-MTP patient population. Although this study was not powered to show improvement in outcome, there were two important findings. First, the majority of patients had a least one coagulation value abnormality. Second, implementation of a pediatric MTP with early and aggressive use of plasma transfusion in children with TIC was feasible. In the same year, Chidester et al. performed a prospective cohort study of 55 children, of whom 22 patients received transfusions according to MTP while the other 33 patients received blood at physician discretion [113]. Similar to results reported by Hendrickson et al., mortality was not significantly different between the two groups. However, the MTP group received a greater overall amount of blood products and was more likely to be severely injured. Thromboembolic events were observed exclusively in the non-MTP-group, which the authors attributed to under transfusion in those patients. Importantly, despite utilizing a MTP, neither study was able to reach the protocols’ goal of 1:1 ratio for FFP:RBC transfusion due to the lack of availability of thawed plasma. Recently a retrospective study on 105 pediatric trauma patients receiving massive transfusion found no association between blood product ratios and survival [114]. Interestingly, all casualities suffered from severe TBI (head AIS ≥ 3) and not hemorrhage. Taken together, additional prospective, randomized clinical trials are needed to fully evaluate the effectiveness of varying ratios of blood component therapies in the pediatric trauma population.
Fresh Frozen Plasma
FFP is the most common blood component transfused to treat coagulopathy. FFP is plasma produced from whole blood and frozen to - 40 degree Celsius to preserve labile coagulation factors. FFP typically contains coagulation factors close to normal blood levels as well as other plasma proteins, including immunoglobulins and albumin. Volume is a potential disadvantage of using FFP in the pediatric trauma setting where TIC may be present and rapidly progressing but no volume expansion is needed. Most guidelines suggest that plasma should be only transfused in the case of active bleeding, and not based on abnormal coagulation screens alone [115, 116].
There are inherent risks to the transfusion of FFP. These risks include, but are not limited to, exposure to pathogens, transfusion related acute lung injury (TRALI), transfusion associated circulatory overload (TACO), and adverse immunological reactions. In a retrospective study, Karam et al. found a three-fold increase in risk of new or progressive multiple organ dysfunction syndrome in pediatric patients receiving one or more plasma transfusions [117]. Those patients receiving plasma also had an increase in nosocomial infections and intensive care unit length of stay. Another retrospective study compared trauma patients receiving FFP alone versus coagulation factor concentrates (fibrinogen and PCC) and no FFP. While mortality was similar, patients receiving FFP received more PRBCs and had an increased frequency of multi-organ failure [118]. Recently, a solvent/detergent (SD) treated plasma has been licensed in the U.S.; this product has been shown to dramatically reduce the risk of adverse advents associated with single donor FFP, including reduced TRALI [119]. The application of SD plasma needs to be explored to determine if its use is safer but equally efficacious compared to the use of regular FFP in pediatric trauma patients who are both coagulopathic and hypovolemic.
Advantages of coagulation factor concentrates include immediate availability for administration, lack of excessive volume expansion, standardization of factor concentration and dose, and lack of elevated risk of TRALI [120]. In addition, coagulation factor concentrates have minimal risk of pathogen transmission, as they undergo viral inactivation steps. However, it should be pointed out that plasma may have protective properties that are unrelated to its procoagulant activity, but are related to the restoration of the endothelial glycocalyx layer that is damaged by hypoperfusion and hypoxia [121].
In summary, pediatric data on successful management of TIC are limited and practices are largely extrapolated from the adult trauma experience. Few studies have directly looked at hemostatic interventions in children. It is clear that TIC accompanying pediatric trauma is an area where future prospective randomized trials are needed to define ideal treatment strategies necessary to improve outcomes in this unique patient population.
Conclusion
Coagulation abnormalities after pediatric trauma are more common than previously thought and are associated with increased morbidity and mortality. Essential prerequisites needed to investigate coagulation abnormalities after trauma in the pediatric population are the accurate interpretation of coagulation tests, along with a thorough understanding of the normal postnatal development of the human coagulation system. The laboratory assisted diagnostic approach to several hemostatic disturbances in the newborn and the child is challenging, because collection procedures and coagulation assays must be adapted for very small amounts of blood, and the reference intervals for many assays may differ broadly from those for adults. Measurements of viscoelastic properties of whole blood provides a rapid evaluation of clot dynamics in whole blood and are of greater value than coagulation screens in diagnosing and managing TIC. A number of interventions have been undertaken in trauma patients to minimize TIC and hemorrhage, including balanced MTPs, factor concentrate administration and antifibrinolytic therapy. Despite these interventions, hemorrhage remains the second largest cause of death in adult trauma patients and is responsible for half of the deaths occurring in the first 24 hours [122]. The widespread application of adult traumatic coagulopathy management principles to pediatric traumatic coagulopathy management should not be done blindly and caution needs to be applied in the care of these patients. The mechanisms behind the development of acute traumatic coagulopathy in the pediatric population need to be elucidated and well-designed prospective clinical trials studying the efficacy of early detection and management in TIC after pediatric trauma are urgently needed.
Acknowledgments
Funding Support: NIH RO1 GM086416 (JFP) and the UAB Kirklin Grant (RTR)
References
- 1.Avarello JT, Cantor RM. Pediatric major trauma: an approach to evaluation and management. Emerg Med Clin North Am. 2007;25(3):803–836. doi: 10.1016/j.emc.2007.06.013. [DOI] [PubMed] [Google Scholar]
- 2.Mace SE, Gerardi MJ, Dietrich AM, Knazik SR, Mulligan-Smith D, Sweeney RL, Warden CR. Injury prevention and control in children. Ann Emerg Med. 2001;38(4):405–414. doi: 10.1067/mem.2001.115882. [DOI] [PubMed] [Google Scholar]
- 3.Whittaker B, Christiaans SC, Altice JL, Chen MK, Bartolucci AA, Morgan CJ, Kerby JD, Pittet JF. Early coagulopathy is an independent predictor of mortality in children after severe trauma. Shock. 2013;39(5):421–426. doi: 10.1097/SHK.0b013e31828e08cb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brohi K, Cohen MJ, Ganter MT, Matthay MA, Mackersie RC, Pittet JF. Acute traumatic coagulopathy: initiated by hypoperfusion: modulated through the protein C pathway? Ann Surg. 2007;245(5):812–818. doi: 10.1097/01.sla.0000256862.79374.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brohi K, Singh J, Heron M, Coats T. Acute traumatic coagulopathy. The Journal of trauma. 2003;54(6):1127–1130. doi: 10.1097/01.TA.0000069184.82147.06. [DOI] [PubMed] [Google Scholar]
- 6.MacLeod JB, Lynn M, McKenney MG, Cohn SM, Murtha M. Early coagulopathy predicts mortality in trauma. The Journal of trauma. 2003;55(1):39–44. doi: 10.1097/01.TA.0000075338.21177.EF. [DOI] [PubMed] [Google Scholar]
- 7.Rixen D, Raum M, Bouillon B, Schlosser LE, Neugebauer E. Arbeitsgemeinschaft Polytrauma der Deutschen Gesellschaft fur U: [Predicting the outcome in severe injuries: an analysis of 2069 patients from the trauma register of the German Society of Traumatology (DGU)]. Unfallchirurg. 2001;104(3):230–239. doi: 10.1007/s001130050719. [DOI] [PubMed] [Google Scholar]
- 8.Patregnani JT, Borgman MA, Maegele M, Wade CE, Blackbourne LH, Spinella PC. Coagulopathy and shock on admission is associated with mortality for children with traumatic injuries at combat support hospitals. Pediatr Crit Care Med. 2012;13(3):273–277. doi: 10.1097/PCC.0b013e31822f1727. [DOI] [PubMed] [Google Scholar]
- 9.Hendrickson JE, Shaz BH, Pereira G, Atkins E, Johnson KK, Bao G, Easley KA, Josephson CD. Coagulopathy is prevalent and associated with adverse outcomes in transfused pediatric trauma patients. The Journal of pediatrics. 2012;160(2):204–209. e203. doi: 10.1016/j.jpeds.2011.08.019. [DOI] [PubMed] [Google Scholar]
- 10.Davenport R. Pathogenesis of acute traumatic coagulopathy. Transfusion. 2013;53(Suppl 1):23S–27S. doi: 10.1111/trf.12032. [DOI] [PubMed] [Google Scholar]
- 11.Miner ME, Kaufman HH, Graham SH, Haar FH, Gildenberg PL. Disseminated intravascular coagulation fibrinolytic syndrome following head injury in children: frequency and prognostic implications. The Journal of pediatrics. 1982;100(5):687–691. doi: 10.1016/s0022-3476(82)80565-9. [DOI] [PubMed] [Google Scholar]
- 12.Spinella PC, Holcomb JB. Resuscitation and transfusion principles for traumatic hemorrhagic shock. Blood Rev. 2009;23(6):231–240. doi: 10.1016/j.blre.2009.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Borgman MA, Spinella PC, Perkins JG, Grathwohl KW, Repine T, Beekley AC, Sebesta J, Jenkins D, Wade CE, Holcomb JB. The ratio of blood products transfused affects mortality in patients receiving massive transfusions at a combat support hospital. The Journal of trauma. 2007;63(4):805–813. doi: 10.1097/TA.0b013e3181271ba3. [DOI] [PubMed] [Google Scholar]
- 14.Maegele M, Lefering R, Paffrath T, Tjardes T, Simanski C, Bouillon B. Working Group on Polytrauma of the German Society of Trauma S: Red-blood-cell to plasma ratios transfused during massive transfusion are associated with mortality in severe multiple injury: a retrospective analysis from the Trauma Registry of the Deutsche Gesellschaft fur Unfallchirurgie. Vox Sang. 2008;95(2):112–119. doi: 10.1111/j.1423-0410.2008.01074.x. [DOI] [PubMed] [Google Scholar]
- 15.Peiniger S, Nienaber U, Lefering R, Braun M, Wafaisade A, Wutzler S, Borgmann M, Spinella PC, Maegele M. Trauma Registry of the Deutsche Gesellschaft fur U: Balanced massive transfusion ratios in multiple injury patients with traumatic brain injury. Crit Care. 2011;15(1):R68. doi: 10.1186/cc10048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Langlois JA, Rutland-Brown W, Thomas KE. The incidence of traumatic brain injury among children in the United States: differences by race. J Head Trauma Rehabil. 2005;20(3):229–238. doi: 10.1097/00001199-200505000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Kipfmueller F, Wyen H, Borgman MA, Spinella PC, Wirth S, Maegele M. [Epidemiology, risk stratification and outcome of severe pediatric trauma]. Klinische Padiatrie. 2013;225(1):34–40. doi: 10.1055/s-0032-1329945. [DOI] [PubMed] [Google Scholar]
- 18.Vavilala MS, Dunbar PJ, Rivara FP, Lam AM. Coagulopathy predicts poor outcome following head injury in children less than 16 years of age. J Neurosurg Anesthesiol. 2001;13(1):13–18. doi: 10.1097/00008506-200101000-00003. [DOI] [PubMed] [Google Scholar]
- 19.Chiaretti A, Piastra M, Pulitano S, Pietrini D, De Rosa G, Barbaro R, Di Rocco C. Prognostic factors and outcome of children with severe head injury: an 8-year experience. Childs Nerv Syst. 2002;18(3-4):129–136. doi: 10.1007/s00381-002-0558-3. [DOI] [PubMed] [Google Scholar]
- 20.Talving P, Lustenberger T, Lam L, Inaba K, Mohseni S, Plurad D, Green DJ, Demetriades D. Coagulopathy after isolated severe traumatic brain injury in children. The Journal of trauma. 2011;71(5):1205–1210. doi: 10.1097/TA.0b013e31820d151d. [DOI] [PubMed] [Google Scholar]
- 21.Harhangi BS, Kompanje EJ, Leebeek FW, Maas AI. Coagulation disorders after traumatic brain injury. Acta neurochirurgica. 2008;150(2):165–175. doi: 10.1007/s00701-007-1475-8. discussion 175. [DOI] [PubMed] [Google Scholar]
- 22.Andrew M, Paes B, Johnston M. Development of the hemostatic system in the neonate and young infant. Am J Pediatr Hematol Oncol. 1990;12(1):95–104. doi: 10.1097/00043426-199021000-00019. [DOI] [PubMed] [Google Scholar]
- 23.Andrew M, Paes B, Milner R, Johnston M, Mitchell L, Tollefsen DM, Castle V, Powers P. Development of the human coagulation system in the healthy premature infant. Blood. 1988;72(5):1651–1657. [PubMed] [Google Scholar]
- 24.Andrew M, Paes B, Milner R, Johnston M, Mitchell L, Tollefsen DM, Powers P. Development of the human coagulation system in the full-term infant. Blood. 1987;70(1):165–172. [PubMed] [Google Scholar]
- 25.Andrew M, Vegh P, Johnston M, Bowker J, Ofosu F, Mitchell L. Maturation of the hemostatic system during childhood. Blood. 1992;80(8):1998–2005. [PubMed] [Google Scholar]
- 26.Flanders MM, Crist RA, Roberts WL, Rodgers GM. Pediatric reference intervals for seven common coagulation assays. Clin Chem. 2005;51(9):1738–1742. doi: 10.1373/clinchem.2005.050211. [DOI] [PubMed] [Google Scholar]
- 27.Flanders MM, Phansalkar AR, Crist RA, Roberts WL, Rodgers GM. Pediatric reference intervals for uncommon bleeding and thrombotic disorders. The Journal of pediatrics. 2006;149(2):275–277. doi: 10.1016/j.jpeds.2006.04.008. [DOI] [PubMed] [Google Scholar]
- 28.Fritsch P, Cvirn G, Cimenti C, Baier K, Gallistl S, Koestenberger M, Roschitz B, Leschnik B, Muntean W. Thrombin generation in factor VIII-depleted neonatal plasma: nearly normal because of physiologically low antithrombin and tissue factor pathway inhibitor. J Thromb Haemost. 2006;4(5):1071–1077. doi: 10.1111/j.1538-7836.2006.01947.x. [DOI] [PubMed] [Google Scholar]
- 29.Parmar N, Albisetti M, Berry LR, Chan AK. The fibrinolytic system in newborns and children. Clin Lab. 2006;52(3-4):115–124. [PubMed] [Google Scholar]
- 30.Hinchliffe RF, Bellamy GJ, Bell F, Finn A, Vora AJ, Lennard L. Reference intervals for red cell variables and platelet counts in infants at 2, 5 and 13 months of age: a cohort study. Journal of clinical pathology. 2013;66(11):962–966. doi: 10.1136/jclinpath-2013-201742. [DOI] [PubMed] [Google Scholar]
- 31.Sitaru AG, Holzhauer S, Speer CP, Singer D, Obergfell A, Walter U, Grossmann R. Neonatal platelets from cord blood and peripheral blood. Platelets. 2005;16(3-4):203–210. doi: 10.1080/09537100400016862. [DOI] [PubMed] [Google Scholar]
- 32.Corby DG, O'Barr TP. Decreased alpha-adrenergic receptors in newborn platelets: cause of abnormal response to epinephrine. Developmental pharmacology and therapeutics. 1981;2(4):215–225. [PubMed] [Google Scholar]
- 33.Gelman B, Setty BN, Chen D, Amin-Hanjani S, Stuart MJ. Impaired mobilization of intracellular calcium in neonatal platelets. 39. Pediatric research. 1996;(4 Pt 1):692–696. doi: 10.1203/00006450-199604000-00022. [DOI] [PubMed] [Google Scholar]
- 34.Israels SJ, Odaibo FS, Robertson C, McMillan EM, McNicol A. Deficient thromboxane synthesis and response in platelets from premature infants. Pediatric research. 1997;41(2):218–223. doi: 10.1203/00006450-199702000-00011. [DOI] [PubMed] [Google Scholar]
- 35.Israels SJ, Cheang T, McMillan-Ward EM, Cheang M. Evaluation of primary hemostasis in neonates with a new in vitro platelet function analyzer. The Journal of pediatrics. 2001;138(1):116–119. doi: 10.1067/mpd.2001.109794. [DOI] [PubMed] [Google Scholar]
- 36.Andrew M, Mitchell L, Vegh P, Ofosu F. Thrombin regulation in children differs from adults in the absence and presence of heparin. Thromb Haemost. 1994;72(6):836–842. [PubMed] [Google Scholar]
- 37.Sosothikul D, Seksarn P, Lusher JM. Pediatric reference values for molecular markers in hemostasis. J Pediatr Hematol Oncol. 2007;29(1):19–22. doi: 10.1097/MPH.0b013e3180308749. [DOI] [PubMed] [Google Scholar]
- 38.Maegele M, Spinella PC, Schochl H. The acute coagulopathy of trauma: mechanisms and tools for risk stratification. Shock. 2012;38(5):450–458. doi: 10.1097/SHK.0b013e31826dbd23. [DOI] [PubMed] [Google Scholar]
- 39.Mann KG, Butenas S, Brummel K. The dynamics of thrombin formation. Arterioscler Thromb Vasc Biol. 2003;23(1):17–25. doi: 10.1161/01.atv.0000046238.23903.fc. [DOI] [PubMed] [Google Scholar]
- 40.Levrat A, Gros A, Rugeri L, Inaba K, Floccard B, Negrier C, David JS. Evaluation of rotation thrombelastography for the diagnosis of hyperfibrinolysis in trauma patients. Br J Anaesth. 2008;100(6):792–797. doi: 10.1093/bja/aen083. [DOI] [PubMed] [Google Scholar]
- 41.Johansson PI, Stensballe J. Effect of Haemostatic Control Resuscitation on mortality in massively bleeding patients: a before and after study. Vox Sang. 2009;96(2):111–118. doi: 10.1111/j.1423-0410.2008.01130.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Davenport R, Manson J, De'Ath H, Platton S, Coates A, Allard S, Hart D, Pearse R, Pasi KJ, MacCallum P, et al. Functional definition and characterization of acute traumatic coagulopathy. Critical care medicine. 2011;39(12):2652–2658. doi: 10.1097/CCM.0b013e3182281af5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Krzanicki D, Sugavanam A, Mallett S. Intraoperative hypercoagulability during liver transplantation as demonstrated by thromboelastography. Liver transplantation : official publication of the American Association for the Study of Liver Diseases and the International Liver Transplantation Society. 2013;19(8):852–861. doi: 10.1002/lt.23668. [DOI] [PubMed] [Google Scholar]
- 44.Ganter MT, Hofer CK. Coagulation monitoring: current techniques and clinical use of viscoelastic point-of-care coagulation devices. Anesth Analg. 2008;106(5):1366–1375. doi: 10.1213/ane.0b013e318168b367. [DOI] [PubMed] [Google Scholar]
- 45.Kutcher ME, Redick BJ, McCreery RC, Crane IM, Greenberg MD, Cachola LM, Nelson MF, Cohen MJ. Characterization of platelet dysfunction after trauma. The journal of trauma and acute care surgery. 2012;73(1):13–19. doi: 10.1097/TA.0b013e318256deab. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.McCrath DJ, Cerboni E, Frumento RJ, Hirsh AL, Bennett-Guerrero E. Thromboelastography maximum amplitude predicts postoperative thrombotic complications including myocardial infarction. Anesth Analg. 2005;100(6):1576–1583. doi: 10.1213/01.ANE.0000155290.86795.12. [DOI] [PubMed] [Google Scholar]
- 47.Kashuk JL, Moore EE, Sabel A, Barnett C, Haenel J, Le T, Pezold M, Lawrence J, Biffl WL, Cothren CC, et al. Rapid thrombelastography (r-TEG) identifies hypercoagulability and predicts thromboembolic events in surgical patients. Surgery. 2009;146(4):764–772. doi: 10.1016/j.surg.2009.06.054. discussion 772-764. [DOI] [PubMed] [Google Scholar]
- 48.Johansson PI, Stensballe J, Vindelov N, Perner A, Espersen K. Hypocoagulability, as evaluated by thrombelastography, at admission to the ICU is associated with increased 30-day mortality. Blood Coagul Fibrinolysis. 2010;21(2):168–174. doi: 10.1097/MBC.0b013e3283367882. [DOI] [PubMed] [Google Scholar]
- 49.Leemann H, Lustenberger T, Talving P, Kobayashi L, Bukur M, Brenni M, Bruesch M, Spahn DR, Keel MJ. The role of rotation thromboelastometry in early prediction of massive transfusion. The Journal of trauma. 2010;69(6):1403–1408. doi: 10.1097/TA.0b013e3181faaa25. discussion 1408-1409. [DOI] [PubMed] [Google Scholar]
- 50.Cotton BA, Faz G, Hatch QM, Radwan ZA, Podbielski J, Wade C, Kozar RA, Holcomb JB. Rapid thrombelastography delivers real-time results that predict transfusion within 1 hour of admission. The Journal of trauma. 2011;71(2):407–414. doi: 10.1097/TA.0b013e31821e1bf0. discussion 414-407. [DOI] [PubMed] [Google Scholar]
- 51.Schochl H, Cotton B, Inaba K, Nienaber U, Fischer H, Voelckel W, Solomon C. FIBTEM provides early prediction of massive transfusion in trauma. Crit Care. 2011;15(6):R265. doi: 10.1186/cc10539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Windelov NA, Welling KL, Ostrowski SR, Johansson PI. The prognostic value of thrombelastography in identifying neurosurgical patients with worse prognosis. Blood Coagul Fibrinolysis. 2011;22(5):416–419. doi: 10.1097/MBC.0b013e3283464f53. [DOI] [PubMed] [Google Scholar]
- 53.Cotton BA, Minei KM, Radwan ZA, Matijevic N, Pivalizza E, Podbielski J, Wade CE, Kozar RA, Holcomb JB. Admission rapid thrombelastography predicts development of pulmonary embolism in trauma patients. The journal of trauma and acute care surgery. 2012;72(6):1470–1475. doi: 10.1097/TA.0b013e31824d56ad. discussion 1475-1477. [DOI] [PubMed] [Google Scholar]
- 54.Kunio NR, Differding JA, Watson KM, Stucke RS, Schreiber MA. Thrombelastography- identified coagulopathy is associated with increased morbidity and mortality after traumatic brain injury. American journal of surgery. 2012;203(5):584–588. doi: 10.1016/j.amjsurg.2011.12.011. [DOI] [PubMed] [Google Scholar]
- 55.Pezold M, Moore EE, Wohlauer M, Sauaia A, Gonzalez E, Banerjee A, Silliman CC. Viscoelastic clot strength predicts coagulation-related mortality within 15 minutes. Surgery. 2012;151(1):48–54. doi: 10.1016/j.surg.2011.06.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Haas T, Spielmann N, Mauch J, Madjdpour C, Speer O, Schmugge M, Weiss M. Comparison of thromboelastometry (ROTEM(R)) with standard plasmatic coagulation testing in paediatric surgery. Br J Anaesth. 2012;108(1):36–41. doi: 10.1093/bja/aer342. [DOI] [PubMed] [Google Scholar]
- 57.Haas T, Spielmann N, Mauch J, Speer O, Schmugge M, Weiss M. Reproducibility of thrombelastometry (ROTEM(R)): point-of-care versus hospital laboratory performance. Scand J Clin Lab Invest. 2012;72(4):313–317. doi: 10.3109/00365513.2012.665474. [DOI] [PubMed] [Google Scholar]
- 58.Vogel AM, Radwan ZA, Cox CS, Jr., Cotton BA. Admission rapid thrombelastography delivers real-time “actionable” data in pediatric trauma. J Pediatr Surg. 2013;48(6):1371–1376. doi: 10.1016/j.jpedsurg.2013.03.036. [DOI] [PubMed] [Google Scholar]
- 59.Woolley T, Midwinter M, Spencer P, Watts S, Doran C, Kirkman E. Utility of interim ROTEM((R)) values of clot strength, A5 and A10, in predicting final assessment of coagulation status in severely injured battle patients. Injury. 2013;44(5):593–599. doi: 10.1016/j.injury.2012.03.018. [DOI] [PubMed] [Google Scholar]
- 60.Ives C, Inaba K, Branco BC, Okoye O, Schochl H, Talving P, Lam L, Shulman I, Nelson J, Demetriades D. Hyperfibrinolysis elicited via thromboelastography predicts mortality in trauma. J Am Coll Surg. 2012;215(4):496–502. doi: 10.1016/j.jamcollsurg.2012.06.005. [DOI] [PubMed] [Google Scholar]
- 61.Oswald E, Stalzer B, Heitz E, Weiss M, Schmugge M, Strasak A, Innerhofer P, Haas T. Thromboelastometry (ROTEM) in children: age-related reference ranges and correlations with standard coagulation tests. Br J Anaesth. 2010;105(6):827–835. doi: 10.1093/bja/aeq258. [DOI] [PubMed] [Google Scholar]
- 62.Chan KL, Summerhayes RG, Ignjatovic V, Horton SB, Monagle PT. Reference values for kaolin-activated thromboelastography in healthy children. Anesth Analg. 2007;105(6):1610–1613. doi: 10.1213/01.ane.0000287645.26763.be. [DOI] [PubMed] [Google Scholar]
- 63.Miller BE, Bailey JM, Mancuso TJ, Weinstein MS, Holbrook GW, Silvey EM, Tosone SR, Levy JH. Functional maturity of the coagulation system in children: an evaluation using thrombelastography. Anesth Analg. 1997;84(4):745–748. doi: 10.1097/00000539-199704000-00008. [DOI] [PubMed] [Google Scholar]
- 64.Halimeh S, Angelis G, Sander A, Edelbusch C, Rott H, Thedieck S, Mesters R, Schlegel N, Nowak-Gottl U. Multiplate whole blood impedance point of care aggregometry: preliminary reference values in healthy infants, children and adolescents. Klinische Padiatrie. 2010;222(3):158–163. doi: 10.1055/s-0030-1249081. [DOI] [PubMed] [Google Scholar]
- 65.Cosgriff N, Moore EE, Sauaia A, Kenny-Moynihan M, Burch JM, Galloway B. Predicting life-threatening coagulopathy in the massively transfused trauma patient: hypothermia and acidoses revisited. The Journal of trauma. 1997;42(5):857–861. doi: 10.1097/00005373-199705000-00016. discussion 861-852. [DOI] [PubMed] [Google Scholar]
- 66.Monroe DM. Modeling the action of factor VIIa in dilutional coagulopathy. Thromb Res. 2008;122(Suppl 1):S7–S10. doi: 10.1016/S0049-3848(08)70010-0. [DOI] [PubMed] [Google Scholar]
- 67.Maegele M, Lefering R, Yucel N, Tjardes T, Rixen D, Paffrath T, Simanski C, Neugebauer E, Bouillon B, Society AGPotGT Early coagulopathy in multiple injury: an analysis from the German Trauma Registry on 8724 patients. Injury. 2007;38(3):298–304. doi: 10.1016/j.injury.2006.10.003. [DOI] [PubMed] [Google Scholar]
- 68.Mann KG, Brummel-Ziedins K, Orfeo T, Butenas S. Models of blood coagulation. Blood Cells Mol Dis. 2006;36(2):108–117. doi: 10.1016/j.bcmd.2005.12.034. [DOI] [PubMed] [Google Scholar]
- 69.Kermode JC, Zheng Q, Milner EP. Marked temperature dependence of the platelet calcium signal induced by human von Willebrand factor. Blood. 1999;94(1):199–207. [PubMed] [Google Scholar]
- 70.Jurkovich GJ, Greiser WB, Luterman A, Curreri PW. Hypothermia in trauma victims: an ominous predictor of survival. The Journal of trauma. 1987;27(9):1019–1024. [PubMed] [Google Scholar]
- 71.Meng ZH, Wolberg AS, Monroe DM, 3rd, Hoffman M. The effect of temperature and pH on the activity of factor VIIa: implications for the efficacy of high-dose factor VIIa in hypothermic and acidotic patients. The Journal of trauma. 2003;55(5):886–891. doi: 10.1097/01.TA.0000066184.20808.A5. [DOI] [PubMed] [Google Scholar]
- 72.Schochl H, Frietsch T, Pavelka M, Jambor C. Hyperfibrinolysis after major trauma: differential diagnosis of lysis patterns and prognostic value of thrombelastometry. The Journal of trauma. 2009;67(1):125–131. doi: 10.1097/TA.0b013e31818b2483. [DOI] [PubMed] [Google Scholar]
- 73.Kashuk JL, Moore EE, Sawyer M, Wohlauer M, Pezold M, Barnett C, Biffl WL, Burlew CC, Johnson JL, Sauaia A. Primary fibrinolysis is integral in the pathogenesis of the acute coagulopathy of trauma. Ann Surg. 2010;252(3):434–442. doi: 10.1097/SLA.0b013e3181f09191. discussion 443-434. [DOI] [PubMed] [Google Scholar]
- 74.Cohen MJ, Call M, Nelson M, Calfee CS, Esmon CT, Brohi K, Pittet JF. Critical role of activated protein C in early coagulopathy and later organ failure, infection and death in trauma patients. Ann Surg. 2012;255(2):379–385. doi: 10.1097/SLA.0b013e318235d9e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Chesebro BB, Rahn P, Carles M, Esmon CT, Xu J, Brohi K, Frith D, Pittet JF, Cohen MJ. Increase in activated protein C mediates acute traumatic coagulopathy in mice. Shock. 2009;32(6):659–665. doi: 10.1097/SHK.0b013e3181a5a632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Maegele M, Schochl H, Cohen MJ. An Up-date on the Coagulopathy of Trauma. Shock in press. 2013 doi: 10.1097/SHK.0000000000000088. [DOI] [PubMed] [Google Scholar]
- 77.Ostrowski SR, Johansson PI. Endothelial glycocalyx degradation induces endogenous heparinization in patients with severe injury and early traumatic coagulopathy. The journal of trauma and acute care surgery. 2012;73(1):60–66. doi: 10.1097/TA.0b013e31825b5c10. [DOI] [PubMed] [Google Scholar]
- 78.Duchesne JC, Holcomb JB. Damage control resuscitation: addressing trauma-induced coagulopathy. Br J Hosp Med (Lond) 2009;70(1):22–25. doi: 10.12968/hmed.2009.70.1.37690. [DOI] [PubMed] [Google Scholar]
- 79.Fenger-Eriksen C, Lindberg-Larsen M, Christensen AQ, Ingerslev J, Sorensen B. Fibrinogen concentrate substitution therapy in patients with massive haemorrhage and low plasma fibrinogen concentrations. Br J Anaesth. 2008;101(6):769–773. doi: 10.1093/bja/aen270. [DOI] [PubMed] [Google Scholar]
- 80.Ziegler B, Schimke C, Marchet P, Stogermuller B, Schochl H, Solomon C. Severe Pediatric Blunt Trauma--Successful ROTEM-Guided Hemostatic Therapy With Fibrinogen Concentrate and No Administration of Fresh Frozen Plasma or Platelets. Clinical and applied thrombosis/hemostasis : official journal of the International Academy of Clinical and Applied Thrombosis/Hemostasis. 2013;19(4):453–459. doi: 10.1177/1076029612458149. [DOI] [PubMed] [Google Scholar]
- 81.Schochl H, Nienaber U, Hofer G, Voelckel W, Jambor C, Scharbert G, Kozek-Langenecker S, Solomon C. Goal-directed coagulation management of major trauma patients using thromboelastometry (ROTEM)-guided administration of fibrinogen concentrate and prothrombin complex concentrate. Critical Care (London, England) 2010;14(2):R55. doi: 10.1186/cc8948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kozek-Langenecker S, Sorensen B, Hess JR, Spahn DR. Clinical effectiveness of fresh frozen plasma compared with fibrinogen concentrate: a systematic review. Critical Care (London, England) 2011;15(5):R239. doi: 10.1186/cc10488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Alten JA, Benner K, Green K, Toole B, Tofil NM, Winkler MK. Pediatric off-label use of recombinant factor VIIa. Pediatrics. 123(3):1066–1072. 200. doi: 10.1542/peds.2008-1685. [DOI] [PubMed] [Google Scholar]
- 84.Morenski JD, Tobias JD, Jimenez DF. Recombinant activated factor VII for cerebral injury-induced coagulopathy in pediatric patients. Report of three cases and review of the literature. J Neurosurg. 2003;98(3):611–616. doi: 10.3171/jns.2003.98.3.0611. [DOI] [PubMed] [Google Scholar]
- 85.Schulman S, Bech Jensen M, Varon D, Keller N, Gitel S, Horoszowski H, Heim M, Martinowitz U. Feasibility of using recombinant factor VIIa in continuous infusion. Thromb Haemost. 1996;75(3):432–436. [PubMed] [Google Scholar]
- 86.Knudson MM, Cohen MJ, Reidy R, Jaeger S, Bacchetti P, Jin C, Wade CE, Holcomb JB. Trauma, transfusions, and use of recombinant factor VIIa: A multicenter case registry report of 380 patients from the Western Trauma Association. J Am Coll Surg. 2011;212(1):87–95. doi: 10.1016/j.jamcollsurg.2010.08.020. [DOI] [PubMed] [Google Scholar]
- 87.Colomina MJ, Diez Lobo A, Garutti I, Gomez-Luque A, Llau JV, Pita E. Perioperative use of prothrombin complex concentrates. Minerva anestesiologica. 2012;78(3):358–368. [PubMed] [Google Scholar]
- 88.Fuentes-Garcia D, Hernandez-Palazon J, Sansano-Sanchez T, Acosta-Villegas F. Prothrombin complex concentrate in the treatment of multitransfusion dilutional coagulopathy in a paediatric patient. Br J Anaesth. 2011;106(6):912–913. doi: 10.1093/bja/aer140. [DOI] [PubMed] [Google Scholar]
- 89.Patanwala AE, Acquisto NM, Erstad BL. Prothrombin complex concentrate for critical bleeding. The Annals of Pharmacotherapy. 2011;45(7-8):990–999. doi: 10.1345/aph.1Q096. [DOI] [PubMed] [Google Scholar]
- 90.Baker RI, Coughlin PB, Gallus AS, Harper PL, Salem HH, Wood EM, Warfarin Reversal Consensus G Warfarin reversal: consensus guidelines, on behalf of the Australasian Society of Thrombosis and Haemostasis. The Medical journal of Australia. 2004;181(9):492–497. doi: 10.5694/j.1326-5377.2004.tb06407.x. [DOI] [PubMed] [Google Scholar]
- 91.Schochl H, Schlimp C, Maegele M. Tranexamic acid, Fibrinogen Concentrate and Prothrombin Complex Concentrate: Data to Support Prehospital Use? Shock in press. 2013 doi: 10.1097/SHK.0000000000000093. [DOI] [PubMed] [Google Scholar]
- 92.Rossaint R, Bouillon B, Cerny V, Coats TJ, Duranteau J, Fernandez-Mondejar E, Hunt BJ, Komadina R, Nardi G, Neugebauer E, et al. Management of bleeding following major trauma: an updated European guideline. Critical Care (London, England) 2010;14(2):R52. doi: 10.1186/cc8943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Pusateri AE, Weiskopf RB, Bebarta V, Butler F, Cestero RF, Chaudry IH, Deal V, Dorlac WC, Gerhardt RT, Given MB, et al. Tranexamic acid and trauma: current status and knowledge gaps with recommended research priorities. Shock. 2013;39(2):121–126. doi: 10.1097/SHK.0b013e318280409a. [DOI] [PubMed] [Google Scholar]
- 94.Tzortzopoulou A, Cepeda MS, Schumann R, Carr DB. Antifibrinolytic agents for reducing blood loss in scoliosis surgery in children. The Cochrane database of systematic reviews. 2008;(3):CD006883. doi: 10.1002/14651858.CD006883.pub2. doi(3):CD006883. [DOI] [PubMed] [Google Scholar]
- 95.Giordano R, Palma G, Poli V, Palumbo S, Russolillo V, Cioffi S, Mucerino M, Mannacio VA, Vosa C. Tranexamic acid therapy in pediatric cardiac surgery: a single-center study. Ann Thorac Surg. 2012;94(4):1302–1306. doi: 10.1016/j.athoracsur.2012.04.078. [DOI] [PubMed] [Google Scholar]
- 96.Royal College of Paediatrics and Child Health Evidence Statement Major trauma and the use of transexamic acid in children. 2012 Available from: http://www.rcpch.ac.uk/system/files/protected/page/121112_TXA%20evidence%20statement_final%20v2.pdf.
- 97.Reade MC, Pitt V, Gruen RL. Tranexamic acid and trauma: current status and knowledge gaps with recommended research priorities. Shock. 2013;40(2):160–161. doi: 10.1097/SHK.0b013e31829ab240. [DOI] [PubMed] [Google Scholar]
- 98.Perkins JG, Cap AP, Spinella PC, Blackbourne LH, Grathwohl KW, Repine TB, Ketchum L, Waterman P, Lee RE, Beekley AC, et al. An evaluation of the impact of apheresis platelets used in the setting of massively transfused trauma patients. The Journal of trauma. 2009;66(4 Suppl):S77–84. doi: 10.1097/TA.0b013e31819d8936. discussion S84-75. [DOI] [PubMed] [Google Scholar]
- 99.Holcomb JB, Wade CE, Trauma Outcomes G, Brasel KJ, Vercruysse G, MacLeod J, Dutton RP, Hess JR, Duchesne JC, McSwain NE, et al. Defining present blood component transfusion practices in trauma patients: papers from the Trauma Outcomes Group. The Journal of trauma. 2011;71(2 Suppl 3):S315–317. doi: 10.1097/TA.0b013e318227ed13. [DOI] [PubMed] [Google Scholar]
- 100.Snyder CW, Weinberg JA, McGwin G, Jr., Melton SM, George RL, Reiff DA, Cross JM, Hubbard-Brown J, Rue LW, 3rd, Kerby JD. The relationship of blood product ratio to mortality: survival benefit or survival bias? The Journal of trauma. 2009;66(2):358–362. doi: 10.1097/TA.0b013e318196c3ac. discussion 362-354. [DOI] [PubMed] [Google Scholar]
- 101.Halmin M, Bostrom F, Brattstrom O, Lundahl J, Wikman A, Ostlund A, Edgren G. Effect of plasma-to-RBC ratios in trauma patients: a cohort study with time-dependent data*. Critical care medicine. 2013;41(8):1905–1914. doi: 10.1097/CCM.0b013e31828a3214. [DOI] [PubMed] [Google Scholar]
- 102.Ho AM, Dion PW, Yeung JH, Joynt GM, Lee A, Ng CS, Chang A, So FL, Cheung CW. Simulation of survivorship bias in observational studies on plasma to red blood cell ratios in massive transfusion for trauma. The British journal of surgery. 2012;99(Suppl 1):132–139. doi: 10.1002/bjs.7732. [DOI] [PubMed] [Google Scholar]
- 103.Magnotti LJ, Zarzaur BL, Fischer PE, Williams FR, Myers AL, Bradburn EH, Fabian TC, Croce MA. Improved Survival After Hemostatic Resuscitation: Does the Emperor Have No Clothes? The Journal of trauma. 2011;70:97–102. doi: 10.1097/TA.0b013e3182051691. [DOI] [PubMed] [Google Scholar]
- 104.Scalea TM, Bochicchio KM, Lumpkins K, Hess JR, Dutton R, Pyle A, Bochicchio GV. Early aggressive use of fresh frozen plasma does not improve outcome in critically injured trauma patients. Ann Surg. 2008;248(4):578–584. doi: 10.1097/SLA.0b013e31818990ed. [DOI] [PubMed] [Google Scholar]
- 105.Sankarankutty A, Nascimento B, Teodoro da Luz L, Rizoli S. TEG(R) and ROTEM(R) in trauma: similar test but different results? World J Emerg Surg. 2012;7(Suppl 1):S3. doi: 10.1186/1749-7922-7-S1-S3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Hallet J, Lauzier F, Mailloux O, Trottier V, Archamblault P, Zarychanski R, Turgeon AF. The Use of Higher Platelet: RBC Transfusion Ratio in the Acute Phase of Trauma Resuscitation: A Systematic Review. Critical care medicine. 2013;41(12):2800–11. doi: 10.1097/CCM.0b013e31829a6ecb. [DOI] [PubMed] [Google Scholar]
- 107.Lustenberger T, Frischknecht A, Bruesch M, Keel MJ. Blood component ratios in massively transfused, blunt trauma patients--a time-dependent covariate analysis. The Journal of trauma. 2011;71(5):1144–1150. doi: 10.1097/TA.0b013e318230e89b. discussion 1150-1141. [DOI] [PubMed] [Google Scholar]
- 108.Wade CE, del Junco DJ, Fox EE, Cotton BA, Cohen MJ, Muskat P, Schreiber MA, Rahbar MH, Sauer RM, Brasel KJ, et al. Do-not-resuscitate orders in trauma patients may bias mortality-based effect estimates: an evaluation using the PROMMTT study. The journal of trauma and acute care surgery. 2013;75(1 Suppl 1):S89–96. doi: 10.1097/TA.0b013e31828fa422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.The University of Texas Health Science Center . ClinicalTrials.gov [Internet] National Library of Medicine (US); Bethesda (MD): [2013 Oct 4]. Houston. Pragmatic, Randomized Optimal Platelets and Plasma Ratios (PROPPR). 2000. Available from: http://clinicaltrials.gov/show/NCT01545232 NLM Identifier: NCT01545232. [Google Scholar]
- 110.Hendrickson JE, Shaz BH, Pereira G, Parker PM, Jessup P, Atwell F, Polstra B, Atkins E, Johnson KK, Bao G, et al. Implementation of a pediatric trauma massive transfusion protocol: one institution's experience. Transfusion. 2012;52(6):1228–1236. doi: 10.1111/j.1537-2995.2011.03458.x. [DOI] [PubMed] [Google Scholar]
- 111.Dehmer JJ, Adamson WT. Massive transfusion and blood product use in the pediatric trauma patient. Seminars in pediatric surgery. 2010;19(4):286–291. doi: 10.1053/j.sempedsurg.2010.07.002. [DOI] [PubMed] [Google Scholar]
- 112.Barcelona SL, Thompson AA, Cote CJ. Intraoperative pediatric blood transfusion therapy: a review of common issues. Part II: transfusion therapy, special considerations, and reduction of allogenic blood transfusions. Paediatric anaesthesia. 2005;15(10):814–830. doi: 10.1111/j.1460-9592.2004.01549.x. [DOI] [PubMed] [Google Scholar]
- 113.Chidester SJ, Williams N, Wang W, Groner JI. A pediatric massive transfusion protocol. The journal of trauma and acute care surgery. 2012;73(5):1273–1277. doi: 10.1097/TA.0b013e318265d267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Nosanov L, Inaba K, Okoye O, Resnick S, Upperman J, Shulman I, Rhee P, Demetriades D. The impact of blood product ratios in massively transfused pediatric trauma patients. American journal of surgery. 2013;206(5):655–60. doi: 10.1016/j.amjsurg.2013.07.009. [DOI] [PubMed] [Google Scholar]
- 115.Levi M, Toh CH, Thachil J, Watson HG. Guidelines for the diagnosis and management of disseminated intravascular coagulation. British Committee for Standards in Haematology. Br J Haematol. 2009;145(1):24–33. doi: 10.1111/j.1365-2141.2009.07600.x. [DOI] [PubMed] [Google Scholar]
- 116.O'Shaughnessy DF, Atterbury C, Bolton Maggs P, Murphy M, Thomas D, Yates S, Williamson LM. British Committee for Standards in Haematology BTTF: Guidelines for the use of fresh-frozen plasma, cryoprecipitate and cryosupernatant. Br J Haematol. 2004;126(1):11–28. doi: 10.1111/j.1365-2141.2004.04972.x. [DOI] [PubMed] [Google Scholar]
- 117.Karam O, Lacroix J, Robitaille N, Rimensberger PC, Tucci M. Association between plasma transfusions and clinical outcome in critically ill children: a prospective observational study. Vox Sang. 2013;104(4):342–349. doi: 10.1111/vox.12009. [DOI] [PubMed] [Google Scholar]
- 118.Nienaber U, Innerhofer P, Westermann I, Schochl H, Attal R, Breitkopf R, Maegele M. The impact of fresh frozen plasma vs coagulation factor concentrates on morbidity and mortality in trauma-associated haemorrhage and massive transfusion. Injury. 2011;42(7):697–701. doi: 10.1016/j.injury.2010.12.015. [DOI] [PubMed] [Google Scholar]
- 119.Ozier Y, Muller JY, Mertes PM, Renaudier P, Aguilon P, Canivet N, Fabrigli P, Rebibo D, Tazerout M, Trophilme C, et al. Transfusion-related acute lung injury: reports to the French Hemovigilance Network 2007 through 2008. Transfusion. 2011;51(10):2102–2110. doi: 10.1111/j.1537-2995.2011.03073.x. [DOI] [PubMed] [Google Scholar]
- 120.Fries D. The early use of fibrinogen, prothrombin complex concentrate, and recombinant- activated factor VIIa in massive bleeding. Transfusion. 2013;53(Suppl 1):91S–95S. doi: 10.1111/trf.12041. [DOI] [PubMed] [Google Scholar]
- 121.Kozar RA, Peng Z, Zhang R, Holcomb JB, Pati S, Park P, Ko TC, Paredes A. Plasma restoration of endothelial glycocalyx in a rodent model of hemorrhagic shock. Anesth Analg. 2011;112(6):1289–1295. doi: 10.1213/ANE.0b013e318210385c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Kauvar DS, Lefering R, Wade CE. Impact of hemorrhage on trauma outcome: an overview of epidemiology, clinical presentations, and therapeutic considerations. The Journal of trauma. 2006;60(6 Suppl):S3–11. doi: 10.1097/01.ta.0000199961.02677.19. [DOI] [PubMed] [Google Scholar]
- 123.Laroche M, Kutcher ME, Huang MC, Cohen MJ, Manley GT. Coagulopathy after traumatic brain injury. Neurosurgery. 2012;70(6):1334–1345. doi: 10.1227/NEU.0b013e31824d179b. [DOI] [PubMed] [Google Scholar]
- 124.Hess JR, Brohi K, Dutton RP, Hauser CJ, Holcomb JB, Kluger Y, Mackway-Jones K, Parr MJ, Rizoli SB, Yukioka T, et al. The coagulopathy of trauma: a review of mechanisms. The Journal of trauma. 2008;65(4):748–754. doi: 10.1097/TA.0b013e3181877a9c. [DOI] [PubMed] [Google Scholar]
- 125.Bowen DJ. Haemophilia A and haemophilia B: molecular insights. Mol Pathol. 2002;55(2):127–144. doi: 10.1136/mp.55.2.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Hymel KP, Abshire TC, Luckey DW, Jenny C. Coagulopathy in pediatric abusive head trauma. Pediatrics. 1997;99(3):371–375. doi: 10.1542/peds.99.3.371. [DOI] [PubMed] [Google Scholar]
- 127.Chiaretti A, Pezzotti P, Mestrovic J, Piastra M, Polidori G, Storti S, Velardi F, Di Rocco C. The influence of hemocoagulative disorders on the outcome of children with head injury. Pediatr Neurosurg. 2001;34(3):131–137. doi: 10.1159/000056008. [DOI] [PubMed] [Google Scholar]
- 128.Holmes JF, Goodwin HC, Land C, Kuppermann N. Coagulation testing in pediatric blunt trauma patients. Pediatr Emerg Care. 2001;17(5):324–328. doi: 10.1097/00006565-200110000-00002. [DOI] [PubMed] [Google Scholar]
- 129.Keller MS, Fendya DG, Weber TR. Glasgow Coma Scale predicts coagulopathy in pediatric trauma patients. Seminars in pediatric surgery. 2001;10(1):12–16. doi: 10.1053/spsu.2001.19381. [DOI] [PubMed] [Google Scholar]
- 130.Hollingworth W, Vavilala MS, Jarvik JG, Chaudhry S, Johnston BD, Layman S, Tontisirin N, Muangman SL, Wang MC. The use of repeated head computed tomography in pediatric blunt head trauma: factors predicting new and worsening brain injury. Pediatr Crit Care Med. 2007;8(4):348–356. doi: 10.1097/01.PCC.0000270837.66217.3B. [DOI] [PubMed] [Google Scholar]
- 131.Marton E, Mazzucco M, Nascimben E, Martinuzzi A, Longatti P. Severe head injury in early infancy: analysis of causes and possible predictive factors for outcome. Childs Nerv Syst. 23(8):873–880. 200. doi: 10.1007/s00381-007-0314-9. [DOI] [PubMed] [Google Scholar]
- 132.Affonseca CA, Carvalho LF, Guerra SD, Ferreira AR, Goulart EM. Coagulation disorder in children and adolescents with moderate to severe traumatic brain injury. J Pediatr (Rio J) 2007;83(3):274–282. doi: 10.2223/JPED.1639. [DOI] [PubMed] [Google Scholar]
- 133.Melo JR, Di Rocco F, Lemos-Junior LP, Roujeau T, Thelot B, Sainte-Rose C, Meyer P, Zerah M. Defenestration in children younger than 6 years old: mortality predictors in severe head trauma. Childs Nerv Syst. 2009;25(9):1077–1083. doi: 10.1007/s00381-009-0924-5. [DOI] [PubMed] [Google Scholar]
- 134.Swanson CA, Burns JC, Peterson BM. Low plasma D-dimer concentration predicts the absence of traumatic brain injury in children. The Journal of trauma. 2010;68(5):1072–1077. doi: 10.1097/TA.0b013e3181d7a6f2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Nylund CM, Borgman MA, Holcomb JB, Jenkins D, Spinella PC. Thromboelastography to direct the administration of recombinant activated factor VII in a child with traumatic injury requiring massive transfusion. Pediatr Crit Care Med. 2009;10(2):e22–26. doi: 10.1097/PCC.0b013e31819bb939. [DOI] [PubMed] [Google Scholar]
- 136.Diab YA, Wong EC, Luban NL. Massive transfusion in children and neonates. Br J Haematol. 2013;161(1):15–26. doi: 10.1111/bjh.12247. [DOI] [PubMed] [Google Scholar]