Abstract
Objectives
The purpose of this study is to determine the association between personal characteristics, a person’s oral health literacy, and failing to show for dental appointments at a university dental clinic.
Methods
A secondary data analysis was conducted on data collected from 200 adults at a university dental clinic between January, 2005 and December, 2006. In the original study, an oral health literacy instrument, the Rapid Estimate of Adult Literacy in Medicine and Dentistry (REALM-D), was administered, sociodemographic and health information seeking behavior gathered, and electronic records reviewed.
Results
Descriptive and bivariate analyses, and a classification and regression tree (CART) analysis were conducted. Seeking health information through fewer sources versus multiple sources was the strongest predictor of failing to show. The subjects’ oral health literacy, as measured by the REALMD List 3 score was the next most significant variable. CART analyses also selected gender, chief complaint, age, and payment type as predictor variables.
Conclusions
Multiple factors contribute to failing to show for dental appointments. However, individuals who use fewer sources of oral health information, a subset of health literacy skills, are more likely to fail to show for dental appointments.
INTRODUCTION
Failing to show (FTS) rates are the percentage of patients who fail to appear at their appointments with no, or only a few hours, warning. FTS for dental appointments have important potential ramifications for the dental health care system and patients’ oral health. When patients FTS for appointments dental practices generate less revenue/production, staff are less efficiently used, and patients who FTS access less dental care thereby increasing their risk of poor dental health (1, 2).
Published FTS rates for dental appointments in the United States vary from 7.3% at a university-based pediatric dental clinic (3) to 24% FTS of 57 safety-net dental clinics in Illinois (4), to 47.0% at a community pediatric dental clinic (1). Although we focus on the US in this paper, numerous researchers in other countries have also investigated FTS (2, 5-16). Forgetting the appointment and illness are frequently cited as reasons for FTS, however the literature is inconsistent as to other factors (1-5, 7-11, 13-22). Factors related to difficulty canceling appointment (e.g. no telephone, called but could not get through), a long lag time between appointments, and having conflicting time commitments (1, 2, 5, 9, 10, 14); not seeing the dental service as valuable (10, 18); lack of trust in the dental health care system (19); and health issues (e.g. illness, negative emotionality, mental health) (1, 2, 5, 8-11, 14, 16, 17) have been shown to be associated with an increased risk of FTS. Other factors have contradictory findings, with associations between FTS and attendance in some studies but not in others. These include factors related to difficulty in leaving work/school; sociodemographic factors (e.g. age, gender, ethnicity, parental education, and SES); dental fear, satisfaction with previous dental treatment, the nature of the dental treatment needed, and the use of public payment assistance (2-6, 8-10, 12, 13, 15, 16, 18-23). Although studies argue that public insurance (e.g. Medicaid in the U.S.) is an important factor in failing to show (4, 20), Farr (21) describes a wide range of failing to show rates for both Medicaid and non-Medicaid patients suggesting that people with public insurance may have multiple factors unrelated to payment source that contribute to failing to show.
Health literacy describes an individual’s capacity to obtain, process, and understand written or verbal health information to make informed health decisions (24, 25). The U.S. Institute of Medicine defines health literacy as “… a shared function of social and individual factors, which emerges from the interaction of the skills of individuals and the demands of social systems”(26). Seeking health-related information includes being able to identify how to get needed health care, and then being able to understand and interpret that information in order to access dental care (27-36).The purpose of this study is to determine the association between personal characteristics, an individual’s oral health literacy and failing to show for dental appointments.
MATERIALS AND METHODS
Study Sample
A secondary data analysis was conducted on data collected from 200 adults seeking care for the first time from a university adult general clinic between January, 2005 and June, 2006 (37). Subjects in the study were screened by a clinic coordinator based on information from the health forms patients completed. Eligibility criteria included being > 18 years of age; no cognitive, vision or hearing impairment; and the ability to complete an informed consent to participate in the study in English. Eligible subjects were given a letter in English describing the study and inviting them to participate. The letter was read to each participant. It was stressed that participation was voluntary; the subject could withdraw if they so desired; and they would receive $5.00 for completing the survey. Other than requiring subjects to read and pronounce the words in the REALM-D instrument, responses to survey questions were obtained via interviews of subjects. Further details of subject recruitment and administration protocol of the original study are published elsewhere (37).
Variables
Patient reported variables
Oral health literacy was assessed with the 84-item Rapid Estimate of Adult Literacy in Medicine and Dentistry (REALM-D), a validated and reliable (Cronbach’s alpha=0.958) word recognition screening instrument in which dental terms were added to the existing 66 item Rapid Estimate of Adult Literacy in Medicine (REALM) to create an instrument that quantifies both medical and dental health literacy (37). The structure of the REALM-D consists of three lists (List 1, List 2, and List 3) of 28-words each of increasing difficulty, ranging from one syllable words in List 1 to the most difficult words in List 3.Reliability of the three lists were α=0.900, α=0.915, and α=0.893, respectively (37). Subjects are asked to read each word, and one point was given for those pronounced correctly. Zero points are given for those mispronounced or not attempted. Scores for each list (1-3) are computed individually and, used as independent List scores or summed to create a total REALM-D score.
Sociodemographic information asked of each participant included age, race, gender, primary language, and educational attainment. Subjects were also asked to indicate all health information resources (magazines, television, newspapers and/or the internet) that they used. The number of resources was summed 0-4.
Electronic health record variables
The electronic chart provided information on the subject’s chief complaint, insurance status, and failing to show during the first six months after initial screening/acceptance to the dental clinic. The subject’s chief complaint was recorded as either no chief complaint at their initial screening or recorded verbatim and then categorized as urgent (pain or presence of infection) or non-urgent (all other reasons). Payment type refers to how the patient’s dental treatment was paid. The university dental clinic requires upfront payment for all patients except those on Medicaid (Public Insurance) and those having Delta Dental insurance (Private Insurance) which assigns the university benefits. All other patients are combined into one payment type (Cash). The subjects’ attendance was categorized into 1 of 3 mutually exclusive groups: 1) no follow-up appointment within 6 months after the individual’s initial screening appointment (No Follow-up), 2) subject attendance or prior cancellation for all scheduled appointments (Completed), and 3) failure to show to at least one scheduled appointment (Failed). Though it is school policy for student dentists to confirm appointments the electronic record does not collect information on how or when the patient was reminded of the appointment by the care provider.
Statistical Analysis
Descriptive, bivariate and multivariate analyses were conducted, evaluating the associations between subject factors (age, race, gender, primary language, education, payment type, chief complaint, the number of health information resources used, and oral health literacy as measured by the REALM-D) and dental attendance behavior. Proportions were compared across the three dental attendance categories (No Follow-up, Completed, Failure To Show) using Fishers exact test. Mean scores for age, number of health information sources used and REALM-D and REALM-D List 3 scores across the 3 dental attendance categories were compared using Analysis of Variance (ANOVA) or the non parametric Kruskal-Wallis test.
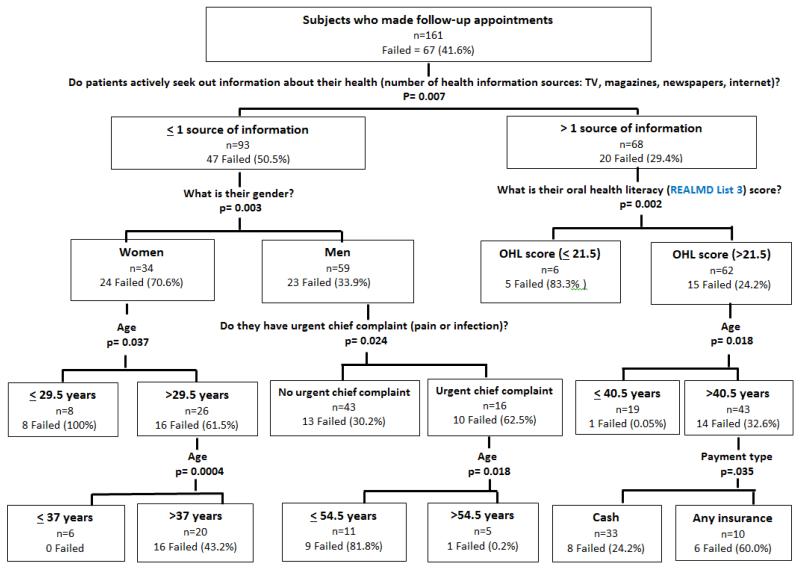
The simultaneous ability of all 10 potential predictors including each of the three component lists of the REALM-D instrument to predict completers versus those failing to show was evaluated using a multivariate classification tree model (CART – Classification and regression tree) (38)(Figure 1). Subjects who did not follow up with any appointment after the initial screening were excluded. The CART, a computer based predictive modeling algorthim, is a sensitive, non-parametric technique that can identify subgroups that mostly fail to show or mostly complete. The CART tree is formed by looking at all possible variable values and finding those variable values that best separate those who fail to show from those who complete. Initially, the best variable value overall is chosen, splitting the data into two subsets (child nodes). The process is repeated in each child node, further splitting the data until no further splits are statistically significant (node homogeneity). In the CART analysis, the most important variable is the variable chosen to make the first (overall) split. Variables chosen in subsequent splits in the subset nodes are sequentially less important. A cross tabulation of the tree compared predicted categories versus the actual categories to determine the tree model accuracy. Overall CART accuracy is defined as the unweighted average of the percent correctly classified in each category.
Figure 1.
Classification and Regression Tree Model which Describes Dental Attendance Behavior of Study Subjects
RESULTS
Sample description
Table 1 describes the characteristics of the subjects by the three dental attendance categories. Sixty-seven of the 200 subjects failed to show for one or more dental appointment(s) (Range 1-8, mean 1.85) during the first six months after their initial acceptance into the adult dental clinic. The majority of these subjects (56.7%) failed only one appointment, 23.9 % failed two appointments, and 19.4 % failed more than two appointments. The sample was 54.5% male, 72.5% with college/post college education, a mean age 48.6 years, and ethnically diverse (42.5% Non-white and 57.5% White). Subjects primarily paid via Cash (72.0%); 9.5% were on Public Insurance (Medicaid), and 18.5% had Private Insurance. Thirty-three (16.5%) subjects did not report any chief complaint at their initial screening, 115 (57.5%) reported a non-urgent chief complaint, and 52 (26.0%) reported an urgent chief complaint. Subjects reported a mean of 1.7 (s.d. of 1.4) of the four types of health information resources. The mean oral health literacy as measured by the REALMD, List 3 score was 24.6 (s.d. of 4.2) of a total of 28. There were no significant patient characteristics differences between the three dental attendance groups, although a trend was observed for number of health information sources used and health literacy as measured by the REALMD List 3.Table 2 describes the association between health literacy scores and the type of health information source used (television, magazines, newspapers, internet). The source most commonly sought for health information was the internet (n= 100). However, subjects with low oral health literacy scores (≤21.5 REALMD, List 3) were significantly less likely to use the internet than those with high health literacy scores (>21.5 REALMD, List 3) (p=0.007). A similar trend was observed for those with high oral health literacy and the use of magazines for health information (p=0.056).
Table 1.
Subject attendance behavior by gender, education, chief complaint, payment type, number of health information resources used, age, and oral health literacy score
| Entire Sample (N=200) |
Dental Attendance |
p-value | |||
|---|---|---|---|---|---|
| Failed (N=67) |
Completed (N=94) |
No Follow-up (N=39) |
|||
|
| |||||
| Freq (%) | Freq (%) | Freq (%) | Freq (%) | ||
| Gender | 0.2444 | ||||
| Female | 91 (45.5%) | 35 (52.2%) | 37 (39.4%) | 19 (48.7) | |
| Male | 109 (54.5%) | 32 (47.8%) | 57 (60.6%) | 20 (51.2%) | |
| Race | 0.5674 | ||||
| Non-white | 85 (42,5%) | 25 (37.3%) | 42 (44.7%) | 18 (46.2%) | |
| White | 115 (57.5%) | 42 (62.7%) | 52 (55.3%) | 21 (53.8%) | |
|
English primary
language |
0.5141 | ||||
| No | 40 (20.0%) | 14 (20.9%) | 16 (17.0%) | 10 (25.6%) | |
| Yes | 160 (80.0%) | 53 (79.1%) | 78 (83.0%) | 29 (74.4%) | |
| Education | 0.4732 | ||||
| ≤High School | 55 (27.5%) | 21 (31.3%) | 22 (23.4%) | 12 (30.8%) | |
| ≥College/post college |
145 (72.5%) | 46 (68.7%) | 72 (76.6%) | 27 (69.2%) | |
| Chief complaint | 0.1394 | ||||
| Not urgent | 115 (57.5%) | 36 (53.7%) | 55 (58.5%) | 24 (61.5%) | |
| Urgent | 52 (26.0%) | 24(35.8%) | 19 (20.2%) | 9 (23.1%) | |
| Unknown (missing in patient record) |
33 (16.5%) | 7(10.4%) | 20 (21.3%) | 6 (15.4%) | |
| Payment Type | 0.5153 | ||||
| Cash | 144 (72.0%) | 44 (65.7%) | 69 (73.4%) | 31 (79.5%) | |
| Public Insurance (Medicaid) |
19 (9.5%) | 7 (10.4%) | 10 (10.6%) | 2 (5.1%) | |
| Private Insur. (Delta Dental) |
37 (18.5%) | 16 (23.9%) | 15 (16.0%) | 6 (15.4%) | |
|
| |||||
| mean (sd) | mean (sd) | mean (sd) | mean (sd) | ||
|
| |||||
|
Number of health
information resources used |
1.8 (1.4) | 1.4 (1.3) | 1.9 (1.4) | 1.9 (1.3) | 0.1515 |
| Age (years) | 48.6 (17.0) | 50.6 (17.5) | 47.5 (16.4) | 47.7 (17.4) | 0.4836 |
|
Health literacy score, REALMD (List 3) |
24.6 (4.2) | 24.1 (4.0) | 24.8 (3.9) | 25.0 (5.0) | 0.082* |
Non-parametric
Table 2.
Comparison of sources of health information for subjects with low and high health literacy scores
| Gets health information from … |
Low health literacy (REALMD list 3≤ 21.5) (N=32) |
High health literacy (REALMD list 3≥21.5) (N=168) |
Pearson Chi-Square, (df=1) |
|---|---|---|---|
|
| |||
| N (%) | N (%) | ||
| TV | 0.630 | ||
| No | 19 (59.4%) | 92 (54.8%) | |
| Yes | 13 (40.6%) | 76 (45.2%) | |
| Magazines | 0.056 | ||
| No | 23 (71.9%) | 90 (53.6%) | |
| Yes | 9 (28.1%) | 78 (46.4%) | |
| Newspapers | 0.140 | ||
| No | 24 (75.0%) | 103 (61.3%) | |
| Yes | 8 (25.0%) | 65 (38.7%) | |
| The internet | 0.007 | ||
| No | 23 (71.9%) | 77 (45.8%) | |
| Yes | 9 (28.1%) | 91 (54.2%) | |
|
Total Number of
Sources of Info |
0.0071 | ||
| ≤1 | 25 (78.1%) | 88 (52.4%) | |
| >1 | 7 (21.9%) | 80 (47.6%) | |
|
Median Sources of
Info |
1 | 1 | |
Classification and Regression Tree (CART) model
CART analysis was conducted on the 161 Failed and Completed subjects. Of the 10 potential predictors considered, the CART model selected six predictor variables: health information used, gender, oral health literacy as measured by the REALM-D List 3 score, chief complaint, age and payment type (Figure 1). Using the six predictor variables, the model found 10 subgroups (terminal nodes), five of which predict FTS and five that predict Completed subjects. Of the 94 subjects who Completed their appointments, 83 (88%) were correctly classified by the CART model. Of the 67 FTS, 44 (66%) were correctly classified. The overall accuracy of the CART model is therefore (88%+66%)/2 = 77% (Table 3).
Table 3.
Prediction of attendance, based on multivariate classification and regression tree (CART) model
| Group | Actual Category |
|||
|---|---|---|---|---|
| Completed | Failed | Total | ||
|
| ||||
| Predicted Category |
Completed | 83 (88%) | 23 | 106 |
| Failed | 11 | 44 (66%) | 55 | |
|
| ||||
| Total | 94 | 67 | 161 | |
Bold values indicate the correct category on which the statistical analysis is based
The most important predictor in the CART analysis was the number of health information sources used (first split, p=0.007), which split the sample into those who used more than 1 source of information (n=68) and those who used one or fewer sources of health information (n=93)(Figure 1). Among the 93 people reporting 1 or fewer health information seeking sources, 47 Failed (50.5%) compared to 20 Failed (29%) for those using more than 1 health resources. Thus, Failed individuals tend to seek health information from fewer sources than people who show up for appointments or reschedule their appointments when required. Conditional on using 1 or fewer sources, gender was the next most significant variable (p=0.003) as 71% of females Failed versus 39% of males (sources × gender interaction). In contrast, for those using more than one source, oral health literacy was the next most important predictor with 83.3% failure for low OHL scores compared to 24.2% failure for higher OHL scores (sources × OHL interaction). Given knowledge of resources, OHL and gender, age and chief complaint were less important, but significant predictors. Considering the 93 subjects with 1 or fewer sources of information, among the 59 male subjects with an urgent chief complaint, 10 of 16 men Failed (62.5%) compared to 13 (30.2%) of the 43 with no urgent chief complaint. Among the 16 males with an urgent chief complaint, age was the final significant (terminal) node, with 81.8% failure in men 54.5 years of age or younger compared to 20% for those older than 54.5 years of age. For women with 1 or fewer sources of information, CART made two splits in the sample of 34 subjects using age, first splitting women at age 29.5 years, and then splitting women older than 29.5 years at 37 years.
Of the 68 subjects who reported using more than 1 sources of health information, the most significant variable chosen was the subject’s oral health literacy, as measured by the REALMD List 3 score (p=.002). Five of six subjects (83%) Failed with a low REALM-D List 3 (equal to or below 21.5) compared to 15 of 62 (24%) with a high REALM-D List 3 score. Age and payment type were less important, but significant predictors conditional on more than one source and REALM-D List 3. Among the 62 subjects with high REALM-D List 3 scores, the next significant predictors were age (p=0.018) with subjects less than or equal to 40.5 years with a 0.05% Failed rate compared to 14 of 62 Failed (32.6%) among those older than 40.5 years. Considering those older than 40.5 years, Payment type (p= 0.035) split the sample with 8 Fails among the 33 subjects paying Cash (24.2%) compared to 6 of 10 (60%) among those subjects having either Private or Public Insurance.
DISCUSSION
Using a tree analysis, our findings show that the number of sources a subject uses to seek health information, the subject’s oral health literacy, gender, age, insurance status, and chief complaint were associated significantly with whether or not the subject followed through (Completed) or failed to attend (Failed) their dental appointments. Seeking health information, a component of health literacy, through fewer sources versus multiple sources was the strongest predictor of FTS. For individuals using multiple sources of health information, low oral health literacy score was the next strongest predictor of FTS. In this decision tree, other factors, such as gender, age, urgent need, and payment type also showed some association, but it was seeking health information that split the group and placed 70% of all people who FTS into one group. Similar to other investigators, we found that public insurance (Medicaid) was not a strong predictor of FTS for dental visits (17,20,23).
These findings emphasize the importance of oral health literacy for successful utilization of health care (25, 39). People who have poor health literacy may have fewer health information sources for a variety of reasons including financial and time constraints or difficulty understanding written materials that discourages reading and internet searches, and cultural biases which may encourage reliance on family members or health care professionals. These same limitations (financial, time, difficulty with written materials, cultural biases) may contribute to difficulty attending or rescheduling dental appointments. In this sample significantly fewer low health literacy subjects (28.1%) reported using the internet than those with high health literacy (54.2%). American adults who do not use the internet report they do not find it’s information valuable (42%); that computers are too difficult to use (21%); or lack access to a computer(18%) (40). Specific interventions to reduce FTS may not be universally effective given the great variability in the factors which influence FTS (3, 23). However, efforts to improve written and verbal communications within health care organizations may be helpful. Studies have demonstrated reminding patients of their appointment with calls or mailed reminders (1, 6, 13, 41); requiring the patient call and confirm their appointment 2 days prior (42), and reducing the gap between scheduling appointments and the appointment date by scheduling only 2 to 5 weeks in advance(8) to all be effective. Schmalzried (43) describes a holistic program that instructs patients who frequently FTS how and when to cancel an appointment, how to obtain help with medication and transportation barriers, and about the effect of FTS on their health costs. This approach reduced the FTS rate from a high of 54% in 2003 to 15% in 2010, reduced staffing costs and improved clinic services.
We observed a trend in our sample among male participants to FTS despite having an urgent chief complaint as seen by other investigators (12). Though the reason for this association is not known, it may reflect the finding by other studies that dental treatment is a low priority or that oral diseases are viewed as not serious problems or are deferrable (8, 11, 13). Improved written and verbal communications may improve patients’ understanding of the risks of deferring care and benefits of timely and preventive dental care and be particularly helpful for patients who have difficulty understanding risks and benefits of health decisions, a characteristic of low health literacy (44).
Limitations
This secondary data analysis was constrained by the availability of variables already collected and did not allow for the inclusion of all potential factors that have been shown to contribute to FTS. It would be useful for future studies to include a broad range of psychosocial, environmental and enabling factors as well as sociodemographic characteristics. In addition, the generalizability of the study findings are limited by having a subject pool that reflects the dental school clinic population and not necessarily the community of people with lower education and multiple payment sources. Finally, our sample size only allows confirmation of the major predictors, not weaker potential predictors.
Conclusion
This report confirms the association between oral health literacy and failing to show for dental appointments. Specifically, our finding that individuals who use fewer sources of health information are more likely to FTS suggests a complexity of factors consistent with the conceptual framework of oral health literacy contribute to failing to show (FTS) for dental appointments.
Acknowledgement
The study was supported by NIDCR research grant # R03-04-177, PI: Kathryn A. Atchison, University of California-Los Angeles School of Dentistry.
Contributor Information
Dr. Jennifer S. Holtzman, Division of Public Health and Community Dentistry at the University of California, Los Angeles School of Dentistry.
Dr. Kathryn A. Atchison, Division of Public Health and Community Dentistry at the University of California, Los Angeles School of Dentistry.
Dr. Melanie W. Gironda, Division of Public Health and Community Dentistry at the University of California, Los Angeles School of Dentistry.
Ms. Rebecca Radbod, SBCC/Department of Biomathematics at the University of California, Los Angeles.
Dr. Jeffrey Gornbein, Statistical/Biomathematical Consulting Clinic; University of California David Geffen School of Medicine, Department of Biomathematics.
REFERENCES
- 1.Casaverde NB, Douglass JM. The effect of care coordination on pediatric dental patient attendance. J Dent Child (Chic) 2007;74:124–9. [PubMed] [Google Scholar]
- 2.Skaret E, Raadal M, Kvale G, Berg E. Missed and cancelled appointments among 12-18-year-olds in the norwegian public dental service. European journal of oral sciences. 1998;106:1006–12. doi: 10.1046/j.0909-8836.1998.eos106605.x. [DOI] [PubMed] [Google Scholar]
- 3.Iben P, Kanellis MJ, Warren J. Appointment-keeping behavior of medicaid-enrolled pediatric dental patients in eastern iowa. Pediatric dentistry. 2000;22:325–9. [PubMed] [Google Scholar]
- 4.Byck GR, Cooksey JA, Russinof H. Safety-net dental clinics. J Am Dent Assoc. 2005;136:1013–21. doi: 10.14219/jada.archive.2005.0296. [DOI] [PubMed] [Google Scholar]
- 5.Albarakati SF. Appointments failure among female patients at a dental school clinic in saudi arabia. J Dent Educ. 2009;73:1118–24. [PubMed] [Google Scholar]
- 6.Almog DM, Devries JA, Borrelli JA, Kopycka-Kedzierawski DT. The reduction of broken appointment rates through an automated appointment confirmation system. J Dent Educ. 2003;67:1016–22. [PubMed] [Google Scholar]
- 7.Bos A, Hoogstraten J, Prahl-Andersen B. Failed appointments in an orthodontic clinic. American journal of orthodontics and dentofacial orthopedics: official publication of the American Association of Orthodontists, its constituent societies, and the American Board of Orthodontics. 2005;127:355–7. doi: 10.1016/j.ajodo.2004.11.014. [DOI] [PubMed] [Google Scholar]
- 8.Gustafsson A, Broberg AG, Bodin L, Berggren U, Arnrup K. Possible predictors of discontinuation of specialized dental treatment among children and adolescents with dental behaviour management problems. European journal of oral sciences. 2010;118:270–7. doi: 10.1111/j.1600-0722.2010.00734.x. [DOI] [PubMed] [Google Scholar]
- 9.Heidmann J, Christensen LB. Immigrants and a public oral health care service for children in denmark. Community Dent Oral Epidemiol. 1985;13:125–7. doi: 10.1111/j.1600-0528.1985.tb00425.x. [DOI] [PubMed] [Google Scholar]
- 10.Herrick J, Gilhooly ML, Geddes DA. Non-attendance at periodontal clinics: Forgetting and administrative failure. Journal of dentistry. 1994;22:307–9. doi: 10.1016/0300-5712(94)90068-x. [DOI] [PubMed] [Google Scholar]
- 11.Hallberg U, Camling E, Zickert I, Robertson A, Berggren U. Dental appointment no-shows: Why do some parents fail to take their children to the dentist? International journal of paediatric dentistry / the British Paedodontic Society [and] the International Association of Dentistry for Children. 2008;18:27–34. doi: 10.1111/j.1365-263X.2007.00867.x. [DOI] [PubMed] [Google Scholar]
- 12.Mandall NA, Matthew S, Fox D, Wright J, Conboy FM, O’Brien KD. Prediction of compliance and completion of orthodontic treatment: Are quality of life measures important? European journal of orthodontics. 2008;30:40–5. doi: 10.1093/ejo/cjm077. [DOI] [PubMed] [Google Scholar]
- 13.Reekie D, Devlin H, Worthington H. The prevention of failed appointments in general dental practice. British dental journal. 1997;182:139–43. doi: 10.1038/sj.bdj.4809325. [DOI] [PubMed] [Google Scholar]
- 14.Richardson A. Failed appointments in an academic orthodontic clinic. British dental journal. 1998;184:612–5. doi: 10.1038/sj.bdj.4809709. [DOI] [PubMed] [Google Scholar]
- 15.Rodd HD, Clark EL, Stern MR, Baker SR. Failed attendances at hospital dental clinics among young patients with cleft lip and palate. The Cleft palate-craniofacial journal: official publication of the American Cleft Palate-Craniofacial Association. 2007;44:92–4. doi: 10.1597/05-162. [DOI] [PubMed] [Google Scholar]
- 16.Wogelius P, Poulsen S. Associations between dental anxiety, dental treatment due to toothache, and missed dental appointments among six to eight-year-old danish children: A cross-sectional study. Acta odontologica Scandinavica. 2005;63:179–82. doi: 10.1080/00016350510019829. [DOI] [PubMed] [Google Scholar]
- 17.Lin KC. Behavior-associated self-report items in patient charts as predictors of dental appointment avoidance. J Dent Educ. 2009;73:218–24. [PubMed] [Google Scholar]
- 18.Maserejian NN, Trachtenberg F, Link C, Tavares M. Underutilization of dental care when it is freely available: A prospective study of the new england children’s amalgam trial. Journal of public health dentistry. 2008;68:139–48. doi: 10.1111/j.1752-7325.2007.00074.x. [DOI] [PubMed] [Google Scholar]
- 19.Murray BP, Wiese HJ. Satisfaction with care and the utilization of dental services at a neighborhood health center. Journal of public health dentistry. 1975;35:170–6. doi: 10.1111/j.1752-7325.1975.tb00708.x. [DOI] [PubMed] [Google Scholar]
- 20.Horsley BP, Lindauer SJ, Shroff B, Tufekci E, Abubaker AO, Fowler CE, et al. Appointment keeping behavior of medicaid vs non-medicaid orthodontic patients. American journal of orthodontics and dentofacial orthopedics: official publication of the American Association of Orthodontists, its constituent societies, and the American Board of Orthodontics. 2007;132:49–53. doi: 10.1016/j.ajodo.2005.08.042. [DOI] [PubMed] [Google Scholar]
- 21.Farr C, Whistler B, Robb S. Summary report: Survey of alaska dental offices failed appointments and patient medicaid status. The Oral Health Program; 2011. [Google Scholar]
- 22.Starr P, Heiserman KJ. Factors associated with missed appointments of patients in a cleft lip and palate clinic. The Cleft palate journal. 1975;12:461–4. [PubMed] [Google Scholar]
- 23.Christensen AA, Lugo RA, Yamashiro DK. The effect of confirmation calls on appointment-keeping behavior of patients in a children’s hospital dental clinic. Pediatric dentistry. 2001;23:495–8. [PubMed] [Google Scholar]
- 24.The invisible barrier: Literacy and its relationship with oral health. A report of a workgroup sponsored by the national institute of dental and craniofacial research, national institute of health, u.S. Public health service, department of health and human services. Journal of public health dentistry. 2005;65:174–82. doi: 10.1111/j.1752-7325.2005.tb02808.x. [DOI] [PubMed] [Google Scholar]
- 25.Pleasant A, McKinney J, Rikard R. Health literacy measurement: A proposed research agenda. Journal of health communication. 2011;16:11–21. doi: 10.1080/10810730.2011.604392. [DOI] [PubMed] [Google Scholar]
- 26.Nielsen-Bohlman LT, Panzer AM, Kindig DA, editors. Health literacy: A prescription to end confusion. National Academies Press; 2004. p. 368. [PubMed] [Google Scholar]
- 27.Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: An updated systematic review. Annals of internal medicine. 2011;155:97–107. doi: 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- 28.Atchison KA, Black EE, Leathers R, Belin TR, Abrego M, Gironda MW, et al. A qualitative report of patient problems and postoperative instructions. Journal of oral and maxillofacial surgery: official journal of the American Association of Oral and Maxillofacial Surgeons. 2005;63:449–56. doi: 10.1016/j.joms.2004.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jones M, Lee JY, Rozier RG. Oral health literacy among adult patients seeking dental care. J Am Dent Assoc. 2007;138:1199–208. doi: 10.14219/jada.archive.2007.0344. quiz 266-7. [DOI] [PubMed] [Google Scholar]
- 30.Miller E, Lee JY, DeWalt DA, Vann WF., Jr. Impact of caregiver literacy on children’s oral health outcomes. Pediatrics. 2010;126:107–14. doi: 10.1542/peds.2009-2887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Parker EJ, Jamieson LM. Associations between indigenous australian oral health literacy and self-reported oral health outcomes. BMC oral health. 2010;10:3. doi: 10.1186/1472-6831-10-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Vann WF, Jr., Lee JY, Baker D, Divaris K. Oral health literacy among female caregivers: Impact on oral health outcomes in early childhood. Journal of dental research. 2010;89:1395–400. doi: 10.1177/0022034510379601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Richman JA, Lee JY, Rozier RG, Gong DA, Pahel BT, Vann WF., Jr. Evaluation of a word recognition instrument to test health literacy in dentistry: The reald-99. Journal of public health dentistry. 2007;67:99–104. doi: 10.1111/j.1752-7325.2007.00022.x. [DOI] [PubMed] [Google Scholar]
- 34.Gong DA, Lee JY, Rozier RG, Pahel BT, Richman JA, Vann WF., Jr. Development and testing of the test of functional health literacy in dentistry (tofhlid) Journal of public health dentistry. 2007;67:105–12. doi: 10.1111/j.1752-7325.2007.00023.x. [DOI] [PubMed] [Google Scholar]
- 35.Valerio MA, Kanjirath PP, Klausner CP, Peters MC. A qualitative examination of patient awareness and understanding of type 2 diabetes and oral health care needs. Diabetes research and clinical practice. 2011;93:159–65. doi: 10.1016/j.diabres.2011.03.034. [DOI] [PubMed] [Google Scholar]
- 36.Sabbahi DA, Lawrence HP, Limeback H, Rootman I. Development and evaluation of an oral health literacy instrument for adults. Community Dent Oral Epidemiol. 2009;37:451–62. doi: 10.1111/j.1600-0528.2009.00490.x. [DOI] [PubMed] [Google Scholar]
- 37.Atchison KA, Gironda MW, Messadi D, Der-Martirosian C. Screening for oral health literacy in an urban dental clinic. Journal of public health dentistry. 2010;70:269–75. doi: 10.1111/j.1752-7325.2010.00181.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Brieman L, Friedman J, Olshen R, Stone C. Classification and regression trees. Wadsworth; Belmont CA: 1984. [Google Scholar]
- 39.Lee S-YD, Arozullah AM, Cho YI, Crittenden K, Vicencio D. Health literacy, social support, and health status among older adults. Educational gerontology. 2009;35:191–201. [Google Scholar]
- 40.Zickuhr K, Smith A. Digital differences. Pew Research Center; 2012. [Google Scholar]
- 41.Shmarak KL. Reduce your broken appointment rate:How one children and youth project redued its broken appoinment rate. American journal of public health. 1971;61:2400–04. doi: 10.2105/ajph.61.12.2400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Cohen AJ, Weinstein P, Wurster C. The effects of patient-initiated phone confirmation strategies on appointment keeping at a hospital dental clinic. Journal of public health dentistry. 1980;40:64–8. doi: 10.1111/j.1752-7325.1980.tb01850.x. [DOI] [PubMed] [Google Scholar]
- 43.Schmalzried HD, Liszak J. A model program to reduce patient failure to keep scheduled medical appointments. Journal of community health. 2012;37:715–8. doi: 10.1007/s10900-011-9505-0. [DOI] [PubMed] [Google Scholar]
- 44.DeWalt D, Callahan L, Hawk V, Broucksou K, Hink A, Rudd R, et al. In: Health literacy universal precautions toolkit. Prepared by North Carolina Network Consortium TCGSCfHSR, editor. The University of North Carolina at Chapel Hill; Rockville, MD.: 2010. under Contract No. HHSA290200710014., editor, January 2012 edition. [Google Scholar]