Abstract
Background
Dual eligibles, persons who qualify for both Medicare and Medicaid coverage, often receive poorer quality care relative to other Medicare beneficiaries.
Objectives
To determine whether dual eligibles are discharged to lower quality post-acute skilled nursing facilities (SNFs) compared with Medicare-only beneficiaries.
Research Design
Following the random utility maximization model, we specified a discharge function using a conditional logit model and tested how this discharge rule varied by dual-eligibility status.
Subjects
A total of 692,875 Medicare fee-for-service patients (22% duals) who were discharged for Medicare paid SNF care between July 2004 and June 2005.
Measures
Medicare enrollment and the Medicaid Analytic Extract files were used to determine dual eligibility. The proportion of Medicaid patients and nursing staff characteristics provided measures of SNF quality.
Results
Duals are more likely to be discharged to SNFs with a higher share of Medicaid patients and fewer nurses. These results are robust to estimation with an alternative subsample of patients based on primary diagnoses, propensity of being dual eligible, and likelihood of remaining in the nursing home.
Conclusions
Disparities exist in access to quality SNF care for duals. Strategies to improve discharge planning processes are required to redirect patients to higher quality providers, regardless of Medicaid eligibility.
Keywords: Health economics, skilled nursing facility care, quality of care
Dual eligibles, persons who qualify for both Medicare and Medicaid coverage, comprise ∼20% of Medicare beneficiaries (about 8.9 million individuals) (The Henry J. Kaiser Family Foundation 2009). They are considered to be the most vulnerable patients in the public insurance system (Thorpe and Philyaw 2010). Quality of care has been an important concern for the dual-eligible population (Merrill, Colby, and Hogan 1997; Haber and Mitchell 1999; Komisar, Feder, and Kasper 2005) and findings suggest that this population is less likely to receive specific types of preventative care, follow-up services, and screening. Studies have also found that nursing homes with a higher proportion of Medicaid-supported residents are associated with more quality deficiencies (Harrington et al. 2000), complaints (Stevenson 2006), lower family member satisfaction (Steffen and Nystrom 1997), and more hospitalizations (Carter and Porell 2003). Existing research on duals' nursing home care, however, has largely focused on the quality of care for long-stay residents. This study extends this literature by focusing on post-acute care in skilled nursing facilities (SNFs). In particular, we focus on disparities in SNF placement between dual beneficiaries and their Medicare-only counterparts.
We build our analyses using the random utility maximization (RUM) model developed by McFadden (1974, 1978), where the key notion is that the selection of a particular SNF is based on all available information about competing SNFs. During the hospital discharge process, discharge planners generally provide a list of local nursing homes that provide SNF care to patients and their families and may help identify which SNFs have vacancies. Theoretically, the decision-makers and their advocates (patients, families, and discharge planners) rank available SNFs using attributes such as facility characteristics and proximity to the patient's homes and then select the SNF with the highest ranking. We call this ranking function the discharge function. The key feature of this framework is that it incorporates all observable attributes and proximity of the competing SNFs simultaneously in the discharge decision-making process. The purpose of this study is to estimate this discharge function and to show how this decision rule differs across dual-eligible and Medicare-only beneficiaries.
Studies have documented different factors that drive the discrepancy in the quality of medical care across different income groups. Arguably, the most important of all these factors is the difference in ability to pay for care. Medicare covers up to 100 days of SNF care, providing full coverage for the first 20 days and then requiring a patient co-payment for the remaining eligible days of care. For calendar year 2012, the average SNF length of stay was roughly 27 days and the copayment amount was $144.50 per day (Medpac 2012). For duals, the copay is supposed to be paid through Medicaid, but in many states, SNFs do not receive this copayment (AHCA 2013).
Another key factor contributing to differential quality of care is residential neighborhood. Quality of care has been shown to vary with geographic region (Welch et al. 1993; O'Connor et al. 1999; Baicker et al. 2004; Baicker, Chandra, and Skinner 2005; Baicker, Buckles, and Chandra 2006). Like many health care providers, SNFs in high poverty neighborhoods are likely to have poor quality (Feng et al. 2011). Distance has been shown to play an important role in the nursing home decision process (e.g., Zwanziger, Mukamel, and Indridason 2002; Shugarman and Brown 2006). In the presence of such distance preference, residential neighborhood acts as an important determinant of the quality of SNF care provided. Our framework directly incorporates distances of all the alternative SNFs from the residential neighborhood and originating hospital in the sorting process. In so doing, we separate the effect of neighborhood from the quality of the SNF per se.
This article aims to identify whether any difference exists in the quality of the destination SNFs to which dual-eligible and Medicare-only beneficiaries are discharged after accounting for residential neighborhood, originating hospital, and other observable characteristics. A finding that dual eligibles are discharged to lower quality SNFs would suggest a failure of the public health insurance system to provide parity of care for all Medicare beneficiaries.
Method
Data and Study Population
The study uses two types of individual-level data: the minimum dataset (MDS) for nursing home resident assessment and Medicare Claims and Enrollment records. We also obtained a measure of Medicaid eligibility from the Medicaid Analytic Extract (MAX) data. At the nursing home level, the primary source of data was the Online Survey, Certification, and Reporting (OSCAR) system. We also included ZIP code-level census 2,000 aggregates for information about patients' residential neighborhood.
We used the Medicare Standard Analytic File (inpatient and SNF files) and the Medicare enrollment records to identify fee-for-service Medicare beneficiaries who were discharged from a general inpatient hospital to an SNF. We merged these data with individuals' MDS assessment records using the Health Insurance Claim number. We applied the residential history file algorithm to the MDS assessments and Medicare SNF claims to determine patients' past use of nursing home care (Intrator et al. 2011). We excluded individuals who had a nursing home stay since 1999. Medicaid eligibility status came from the MAX data. SNF provider characteristics were obtained from OSCAR, which contains data detailing the resident population, nurse staffing, and the physical address of the facility. Hospitals were matched to the 2005 American Hospital Association database to obtain the hospitals' physical addresses. The ZIP code-level data from the 2000 US Census were matched to the beneficiaries' residential ZIP code.
We identified 810,362 fee for service Medicare beneficiaries aged 65 years and over discharged from a hospital to an SNF between July 1, 2004 and June 30, 2005 without prior nursing home use. We dropped individuals for whom SNF, hospital, and residential ZIP code identification did not match with the OSCAR, AHA, and census data, respectively. We also excluded beneficiaries not residing in the contiguous 48 states and not from general hospitals, leaving us with 692,875 (85.50% of discharges to SNF) beneficiaries in the study population. Appendix SA2 Table 1 presents the number of individuals after each stage of exclusion.
Variables
The main independent variable of interest is a patient's dual eligibility status. We obtained this measure from the 2004–2005 MAX data, which includes monthly Medicaid eligibility status. We defined a patient as dual eligible if the individual was Medicaid-eligible for at least one of the 6 months before SNF admission. Those beneficiaries who spent-down (Liu, Doty, and Manton 1990) following the SNF admission were not considered to be dually eligible for the purpose of this study.
We assume that patients compare alternative SNFs based on proximity. We calculated distances to all the potential SNFs where a patient could have been admitted from two origins: patients' residential ZIP code and the address of the discharging hospital. All hospitals and SNFs' physical addresses were geo-coded. The five-digit ZIP code centroids in the US Census data were used as the residential location of the Medicare beneficiaries. We used the Haversine formula to calculate the two distance measures. We also used the distances to all the SNFs from each hospital to define a patient's choice set as discussed below.
Skilled nursing facility attributes included in our analyses are the number of full-time equivalent (FTE) registered nurses (RNs), licensed practical nurses, and certified nursing assistants and the proportion of Medicaid residents. It has been argued that more nursing staff (as measured by number of FTEs) is a marker for better quality (Castle 2008; Castle and Anderson 2011; Hyer et al. 2011). In addition, the proportion of Medicaid residents approximates the level of resources at the facility and has been found to be associated with quality deficiencies (Harrington et al. 2000; Mor et al. 2004), complaints (Stevenson 2006), family member satisfaction (Steffen and Nystrom 1997), and hospitalizations (Carter and Porell 2003). We controlled for additional nursing home–level variables from the OSCAR data in the models including the occupancy rate, total number of beds, membership in a chain (yes/no), ownership status (for-profit = yes/no), hospital affiliation (hospital-based = yes/no), ProPAC acuity index (Kane, Priester, and Kane 2008), and a weighted health inspection deficiency score (Centers for Medicare and Medicaid Services 2010; Hyer et al. 2011). In addition, MDS data were aggregated to the nursing home level to measure the proportion of residents that were black and the average Resource Utilization Groups III case mix index.
Patient-level characteristics included age, gender (male = yes/no), race (white = yes/no, black = yes/no), education level (high school degree = yes/no, more than a high school degree = yes/no), Elixhauser comorbidity index (calculated from the diagnoses listed on the Medicare claims; Elixhauser et al. 1998), Deyo comorbidity index calculated from the diagnoses listed on the Medicare claims (Deyo, Cherkin, and Ciol 1992), hospital length of stay, and length of stay in the SNF (>20 days = yes/no). Individual characteristics were not incorporated into the statistical model directly but were used to create groups of patients that are observably homogenous. We estimated the discharge equation within those groups.
Analyses
Comparison of SNF Characteristics
We compare the key destination SNF characteristics between duals and nonduals. We first calculate the raw difference and then measure the differences after controlling for patient demographics, clinical attributes, and origin ZIP code fixed effects. We next plot the two key SNF characteristics associated with quality, the share of Medicaid paid patients, and the share of RN among all nurses in the facility, separately for duals and nonduals within small groups of patients who have a similar likelihood (propensity score) of being dual-eligible. The propensity score is estimated using a logistic regression model based on demographic characteristics, education, Elixhauser and Deyo indices, length of hospital stay, several characteristics of patients' residential ZIP code, and hospital admission diagnosis-related groups fixed effects.
Previous research has suggested that quality differences are related to other facility characteristics. Therefore, we expect that different nursing home attributes will affect the discharge decision simultaneously and that the decision makers make tradeoffs between these attributes. For example, a patient might be willing to travel longer to be treated in an SNF with better quality. This provides the rationale for estimating the discharge function described below where all these characteristics are taken into account simultaneously, allowing us to understand their relative importance in the discharge process between duals and nonduals.
Discharge Function
Our discharge function specification is based on the RUM model developed by McFadden (1974, 1978). Here each individual patient, labeled i, faces a choice set CSi, which is composed of j alternative SNFs. The decision makers rank all the SNFs in the choice set and the patient is discharged to the one receiving the highest ranking. Following McFadden's argument, the probability of patient i being discharged to SNF j in choice set CSi can be specified as a multinomial logit model:
| 1 |
We allow Vij to be different for patients with different Medicaid eligibility. Thus,
| 2 |
Here,  denotes the distance of SNFj from the residential ZIP code of patient i. Similarly,
denotes the distance of SNFj from the residential ZIP code of patient i. Similarly,  indicates the distance of SNFj from the discharging hospital of patient i. Xj are the SNF attributes and we incorporated k such attributes in our model. Xj includes the number of FTE nurses, share of Medicaid paid residents, health deficiency score, ownership status, hospital affiliation, total number of beds, and occupancy rate, as well as measures of acuity. Our aim is to interpret the coefficient as change in the likelihood of being discharged due to a change in one relevant characteristic while all others remain unchanged. DEi is a binary variable which is 1 if individual i is dually eligible and 0 otherwise. Alphas (α) represent the preference coefficient of the nondual patients, whereas the betas (β) represent how different those parameters are for the duals. In this specification, for example, the estimated coefficient (alpha) on the RN variable suggests how the probability of going to an SNF for an average nondual patient changes (ceteris paribus) if it has one extra FTE RN. The corresponding beta implies how that valuation of that additional RN FTE differs for duals relative to nonduals.
indicates the distance of SNFj from the discharging hospital of patient i. Xj are the SNF attributes and we incorporated k such attributes in our model. Xj includes the number of FTE nurses, share of Medicaid paid residents, health deficiency score, ownership status, hospital affiliation, total number of beds, and occupancy rate, as well as measures of acuity. Our aim is to interpret the coefficient as change in the likelihood of being discharged due to a change in one relevant characteristic while all others remain unchanged. DEi is a binary variable which is 1 if individual i is dually eligible and 0 otherwise. Alphas (α) represent the preference coefficient of the nondual patients, whereas the betas (β) represent how different those parameters are for the duals. In this specification, for example, the estimated coefficient (alpha) on the RN variable suggests how the probability of going to an SNF for an average nondual patient changes (ceteris paribus) if it has one extra FTE RN. The corresponding beta implies how that valuation of that additional RN FTE differs for duals relative to nonduals.
The Choice Set
The first step of the estimation procedure is the specification of the choice set. Our choice sets are hospital specific (we assume that all the patients from the same hospital are presented with similar SNF options) and each choice set is the union of three sets of SNFs: (1) SNFs within a 22 km radius from the hospital (the 80th percentile of the distance travelled by all the patients to reach the SNF), (2) the nearest 15 SNFs from the hospital, and (3) all the SNFs where patients from this hospital have been discharged. If we include only those SNFs within a 22 km radius, the choice set becomes very small for hospitals in low population density areas, but for high population density areas, it becomes very large. On the other hand, if we take only the closest 15 SNFs, the choice set becomes relatively small for areas with a high population density, as there are lots of SNFs close to those hospitals. If we do not include all the SNFs where patients have been discharged from a given hospital, those patients who travelled longer distances will be dropped from the analysis, resulting in biased distance parameters. Finally, we eliminated all the out-of-state SNFs from the choice set allowing us to cluster individuals by state in the regression analysis. Only 2% of the patients in our sample were discharged to SNFs that are not in the same state as the discharging hospital. Given that this share is the same for both duals and nonduals, we do not believe this has biased the analyses. An average nondual patient faces 59 alternative SNFs in the choice set, while dual eligibles have 58 alternatives.
To model choice sets for individuals, we expand the dataset such that the number of observations for a given individual is equal to the number of SNFs in his/her choice set. We create a dichotomous variable “choice,” which is 1 if the observation identifies the SNF where individual i is discharged and 0 otherwise. We estimate the discharge function using the clogit command in Stata with choice as the dependent variable, distances and SNF attributes as independent variable, and individual identification as the group variable. This model predicts the probability of going to each SNF in the choice set, such that the summation of the probabilities for a given individual is 1. As the estimation procedure is computationally intensive, we selected a random 20% sample of the individuals (N = 128,785 and 22.2% dual-eligible) to estimate the discharge function.
Calculating the Marginal Effects
The marginal effects from conditional logit have to be alternative specific and cannot be calculated in conventional ways. For example, the marginal effect of an additional RN for a given SNF “X ” is the change in likelihood of an individual being discharged to SNF “X ” due to an extra RN in that facility with other characteristics of that SNF and all the characteristics of competing SNFs remaining unchanged. Similarly, one can calculate cross marginal effects, that is, the change in likelihood of being discharged to SNF “Y ” due to a change in characteristic of SNF “X ”. Davies and colleagues provide an example of calculating marginal effects after conditional logit estimation in the context of U.S. state-to-state migration, showing how changes in the unemployment rate in a given state change the likelihood of migration to that state as well as to other states (Davies, Greenwood, and Li 2002).
We calculated the marginal effect based on a randomly selected SNF in the choice set using the following steps. (1) We predicted the probability of each individual going to alternative SNFs in the choice set based on SNF characteristics and estimated parameters. (2) We randomly selected one SNF in the choice set for each individual patient. (3) We altered the value of relevant SNF characteristics for that randomly selected SNF and predicted the probability of the individual patient going to that SNF. (4) The marginal effect is calculated as the mean of the change in the predicted probability for randomly selected SNFs. We presented marginal effects of the Medicare-only patients and the difference in the marginal effects between dual-eligible and Medicare-only patients along with parameters in equation (2).
In addition to direct effects, we also calculate the cross effects, that is, the effect of change in characteristics of an SNF on the likelihood of being discharged to a competing SNF. We calculated cross marginal effects by using the nearest SNF to the patient's residence. In this case, we changed the characteristics of the nearest SNF and projected the change in the likelihood of individuals being admitted to the 10 nearest SNFs. We presented the mean of the effects separately for Medicare only and dual-eligible patients.
Sensitivity Analyses
An important concern with the above specified discharge function is that, apart from originating neighborhood/hospital, important differences may exist between duals and nonduals in terms of clinical and demographic characteristics and therefore these two groups might not be comparable. Given the nature of our model, which effectively incorporates individual fixed effects, we cannot control for these observable patient characteristics directly. Thus, we conducted a series of robustness checks using various patient subgroups.
First, we select patients with the same race and primary hospital diagnosis (e.g. hip-fracture, heart-failure, stroke, and COPD/asthma) and estimated the discharge function separately for each group. Second, because being dually eligible is correlated with demographic characteristics like race, education, and marital status, we divided our sample into quintiles of the propensity score and estimated the discharge function within each quintile. Third, our primary model focuses on SNF care only and ignores the role of other types of postacute care settings. Since inpatient rehabilitation facilities (IRFs) are a potential substitute for SNF care, we estimated the discharge functions separately for hospitals with and without an IRF. We also estimate the discharge function separately for hospitals with and without their own hospital-based SNFs. Finally, the size of the choice set and the fraction of dual-eligibles may differ across rural and urban areas. Thus, we divided patients into two groups based on the median value of the fraction of rural population in the residential ZIP code and estimated the discharge function separately for the rural and urban populations.
Results
Descriptive Results
Table1 describes the individual characteristics of the sample by dual-eligibility status. Dual eligibles are, on average, 1 year younger, less likely to be white and male, less educated, and more likely to reside in lower income neighborhoods than their Medicare-only counterparts. Clinically, dual-eligible patients have higher comorbidity and experienced longer hospital lengths of stay.
Table 1.
Descriptive Statistics of Individual Characteristics by Dual-Eligibility Status
| Nonduals N =539,038 (77.80%) | Duals N =153,837 (22.20%) | |||
|---|---|---|---|---|
| Mean | SD | Mean | SD | |
| Demographic characteristics | ||||
| Age | 80.9 | 7.47 | 79.7 | 8.2 |
| Male | 0.37 | 0.48 | 0.30 | 0.46 |
| White | 0.90 | 0.30 | 0.71 | 0.45 |
| Black | 0.05 | 0.21 | 0.17 | 0.37 |
| Education | ||||
| High school graduate | 0.33 | 0.47 | 0.30 | 0.45 |
| More than high school | 0.36 | 0.48 | 0.21 | 0.41 |
| Missing education | 0.16 | 0.36 | 0.13 | 0.34 |
| Residential ZIP code characteristics | ||||
| Per capita income | 23,096 | 9,477 | 19,330 | 7,437 |
| Poverty rate | 8.64 | 5.57 | 12.44 | 7.86 |
| Clinical characteristics from last hospitalization | ||||
| Elixhauser comorbidity index | 2.45 | 1.33 | 2.59 | 1.33 |
| Deyo comorbidity index | 1.58 | 1.88 | 1.78 | 1.86 |
| Length of stay at hospital | 9.17 | 7.39 | 10.01 | 9.00 |
Note. Differences in means between duals and nonduals are all statistically significant.
In comparing SNF characteristics (see Table2), we observe that dual-eligible patients were admitted to facilities with ∼55% Medicaid residents compared with 43% among their counterpart nonduals. Dual eligibles are discharged to larger facilities that have lower staffing levels. Results also suggest that dual eligibles are more likely to be discharged to free-standing and for-profit facilities with a higher average proportion of black residents. After controlling for patient characteristics, the share of Medicaid residents in a destination SNF is about 8 percentage points higher and the share of RNs among total facility nurses is about 3 percentage points lower for dual eligibles relative to Medicare only patients. This implies that patient-level demographic and clinical characteristics and residential neighborhood explain only 25% of the difference in facility quality between duals and nonduals.
Table 2.
Comparison of Discharged Nursing Home Characteristics by Dual-Eligibility Status
| Variable | Nonduals | Duals | Difference | Adjusted Difference |
|---|---|---|---|---|
| Distance from residential ZIP code (km) | 15.5 | 16.6 | 1.116** | −0.690*** |
| Distance from origin hospital (km) | 11.7 | 13.0 | 1.365** | 0.0384 |
| Occupancy rate | 0.85 | 0.86 | 0.0110** | 0.00867*** |
| Total number of beds | 117.7 | 131.1 | 13.40*** | 9.465*** |
| Percent of Medicaid residents | 42.9 | 54.9 | 11.94*** | 7.723*** |
| Member of a chain (%) | 0.57 | 0.60 | 0.0291* | 0.0244*** |
| For-profit ownership (%) | 0.60 | 0.66 | 0.0572*** | 0.0599*** |
| Percent of residents that are black | 7.8 | 13.2 | 5.472*** | 1.597*** |
| Total number of FTE CNAs | 47.2 | 51.6 | 4.386** | 2.736*** |
| Total number of FTE RNs | 9.1 | 8.7 | −0.386 | −0.362*** |
| Total number of FTE LPNs | 16.5 | 17.6 | 1.056** | 0.812*** |
| Share of RN among total nurses | 37.8 | 33.6 | −4.15*** | −2.77*** |
| Average RUGS III case-mix index | 1.1 | 1.1 | 0.00237 | −0.00175* |
| Hospital-based (%) | 0.23 | 0.18 | −0.0458*** | −0.0547*** |
| ProPAC acuity index | 94.7 | 102.6 | 7.912*** | 4.379*** |
| Health deficiency score | 8.5 | 9.5 | 1.01*** | 0.680*** |
Note.
p < 0.01
p < 0.05
p < 0.1.
To calculate the adjusted differences, we ran OLS model with corresponding SNF characteristics as outcome variable onto demographic characteristics, education, Elixhauser and Deyo indexes, length of stay at the hospital (listed in Table1), hospital admission DRG, and origin ZIP code fixed effects. Chain membership, profit status, and hospital association are binary variables. The rest are continuous variables.
CNA, certified nursing assistant; FTE, full-time equivalent; LPN, licensed practical nurse; RN, registered nurse; RUGS, resource utilization group; SNF, skilled nursing facility.
Using local linear regression smoothing, Figure1 plots the share of Medicaid-supported residents and the share of RNs relative to all nursing staff in the discharge SNF of the patients against the probability of them being dual eligible, separately for duals and nonduals. For both types of patients, as the likelihood of being dually eligible increases, the share of Medicaid in the discharged SNF increases (panel A) and the share of RNs in the discharged SNF declines (panel B). Indeed, for any given likelihood of being dually eligible, duals are always discharged to a poorer quality SNF (i.e., one with a higher share of Medicaid and a lower share of RNs).
Figure 1.
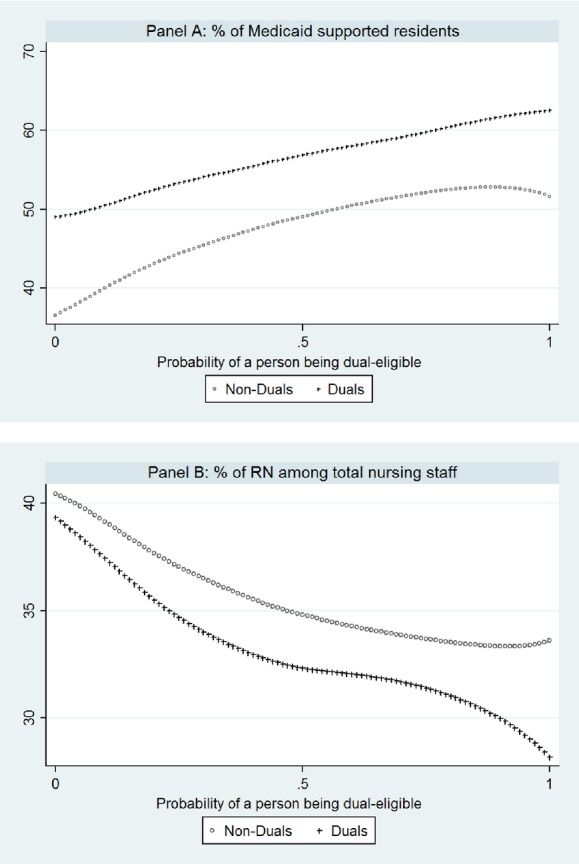
Destination Nursing Home Characteristics over Likelihood (Propensity Score) of Being Dual Eligible
Conditional Logit Results
Table3 presents the results of a conditional logit model controlling for the SNF characteristics listed in Table2 (except the share of RNs among all nurses). Column 1 displays the alphas (the discharge coefficients for Medicare-only patients) and Column 2 reports the betas (how the discharge coefficients differ for duals from Medicare-only patients). As expected, the further the SNF from the patient's residential ZIP code, the lower the likelihood that the patient will be discharged there. Based on the marginal effects, if the distance of a randomly selected SNF from the residential ZIP code increases by 1 kilometer, the likelihood of being discharged to that SNF declines by 0.15 percentage points for Medicare-only patients and 0.14 percentage points for duals.
Table 3.
Estimated Discharge Parameters and Marginal Effects (Based on Random 20% of the Patients N = 128,785)
| Medicare Only | Difference of Dual Eligibles | |||
|---|---|---|---|---|
| Coefficient (Alpha) | Marginal Effects | Coefficient (Beta) | Marginal Effects | |
| Distance from residential ZIP code | −0.0810*** [−15.61] | −0.150 | 0.0125*** [3.743] | 0.01 |
| Distance from origin hospital | −0.0651*** [−14.93] | −0.153 | 0.0183*** [6.106] | 0.024 |
| Occupancy rate | 0.622*** [3.505] | 0.0182 | −0.139 [−1.269] | 0.0023 |
| Total number of beds | 0.00172** [2.111] | 0.0041 | 0.00149*** [3.237] | 0.0004 |
| Percent of Medicaid residents | −0.0185*** [−23.65] | −0.044 | 0.01000*** [10.60] | 0.021 |
| Member of a chain | 0.0853** [2.345] | 0.210 | 0.102*** [3.497] | 0.34 |
| For-profit ownership | 0.196*** [4.186] | 0.501 | 0.00618 [0.187] | 0.12 |
| Percent of residents that are black | −0.0192*** [−8.995] | −0.045 | 0.0158*** [12.72] | 0.035 |
| Total number of FTE CNAs | −0.00532** [−2.517] | −0.013 | 0.000712 [0.455] | 0.001 |
| Total number of FTE RNs | 0.0186*** [6.020] | 0.0451 | −0.0139*** [−4.477] | −0.032 |
| Total number of FTE LPNs | 0.0268*** [7.225] | 0.065 | −0.0103** [−2.423] | −0.02 |
| Average RUGS III case-mix index | 2.667*** [16.85] | 0.142 | 0.270** [2.058] | 0.042 |
| Hospital-based | 0.555*** [8.018] | 0.016 | 0.159*** [2.688] | 0.009 |
| ProPAC acuity index | −0.00481*** [−9.489] | −0.012 | 0.00169* [1.922] | 0.001 |
| Health deficiency score | −0.00183 [−0.497] | −0.004 | 0.00414 [1.542] | 0.002 |
Note.
p < 0.01
p < 0.05
p < 0.1.
Column 1 presents the coefficients of different SNF characteristics for Medicare-only patients and column 2 shows the coefficients of those characteristics interacted with dual-eligibility dummy, that is, how different the coefficients for duals compared with the nonduals. Marginal effects are calculated as percentage change in likelihood of being discharged to an SNF in response to a one unit of change in corresponding characteristics. Robust z-statistics (clustering at state level) in brackets.
CNA, certified nursing assistant; FTE, full-time equivalent; LPN, licensed practical nurse; RN, registered nurse; RUGS, resource utilization group.
The estimated coefficients indicate that an increase in the share of Medicaid patients would reduce the chance of being discharged to that SNF for both types of patients, but the negative effect is about two times larger for Medicare-only patients compared with the duals. If the share of Medicaid increases in a random SNF in the choice increases by 10%, then the probability of being discharged to that SNF declines by 0.4 percentage points for the Medicare-only patients but only by 0.2 percentage points for the dual eligibles. Similarly, as shown in Appendix SA2 Table 1, if the share of Medicaid in the SNF that is nearest to the residence of the patient increases by 10%, the likelihood of going to that SNF decreases by 1.5 percentage points for nondual patients and by 0.8 percentage points for duals. An extra RN in a randomly selected SNF in the choice set increases the probability of going to that SNF by 0.04 percentage points for Medicare-only patients and by 0.01 percentage points for the dual eligibles.
In Table2 and Figure1, we compared characteristics of admitted SNFs between duals and nonduals. We can make a similar comparison using the predicted probabilities derived from the estimated conditional logit model. Based on the predicted probabilities, the share of Medicaid is about 12 percentage points higher and the percentage of RN among total nurses is about 4 percentage points lower for duals than Medicare-only patients (the same as the figures calculated from Table2). If all the estimated betas were 0, then the predicted probabilities imply that the share of Medicaid would be 3.5 points higher and the share of RNs among total nurses to be 1% lower in facilities selected by duals. Thus, dual-eligibility status explains 75% of the difference in the quality of the SNF to which the patient is discharged and the remaining difference is attributable to the residential neighborhood and originating hospital.
Results of the Estimation with Selected Subgroups
Results of the robustness checks (with an alternate specification of the sorting function and using specific patient populations) are displayed in Table4. Among patients of the same race, duals are persistently more likely to be discharged to SNFs with a higher fraction of Medicaid paid residents and with lower nursing staff FTEs. The results also suggest that even though the proportion of dual eligibles among the different primary diagnosis varies substantially (hip fracture = 19%, COPD/Asthma = 29%), the estimated parameters are roughly the same as those we found for the overall sample. Similarly, results from the regression using the quintiles of the propensity score of being dual eligible reveal that the coefficients are roughly the same for all of the groups with the exception of the highest quintile, suggesting that the observable characteristics that are correlated with being dual eligible are not driving the estimated differential discharge coefficients.
Table 4.
Estimated Discharge Function Based on Alternative Subsamples
| N | % of Dual Eligibles | % of Medicaid Residents | FTE RNs | FTE LPNs | ||||
|---|---|---|---|---|---|---|---|---|
| Medicare Only (alpha) | Diff. of Dual Eligibles (beta) | Medicare Only (alpha) | Diff. of Dual Eligibles (beta) | Medicare Only (alpha) | Diff. of Dual Eligibles (beta) | |||
| Original sample | 128,785 | 22.20 | −0.0185*** | 0.01000*** | 0.0186*** | −0.0139*** | 0.0268*** | −0.0103** |
| White | 119,035 | 18.36 | −0.0181*** | 0.0117*** | 0.0196*** | −0.0126*** | 0.0272*** | −0.00772** |
| Black | 9,924 | 51.64 | −0.0218*** | 0.00714*** | 0.0224*** | −0.0195*** | 0.0315*** | −0.0139*** |
| Hip fracture (100% sample) | 69,847 | 19.11 | −0.0188*** | 0.00880*** | 0.0204*** | −0.0119*** | 0.0266*** | −0.00776 |
| Heart failure (100% sample) | 27,268 | 25.09 | −0.0176*** | 0.00812*** | 0.0163*** | −0.0135*** | 0.0237*** | −0.0101*** |
| COPD (100% sample) | 14,302 | 28.64 | −0.0174*** | 0.00864*** | 0.0168*** | −0.00788** | 0.0223*** | −0.0102*** |
| Stroke (100% sample) | 43,066 | 26.66 | −0.0164*** | 0.00840*** | 0.0142*** | −0.0139*** | 0.0245*** | −0.0122*** |
| Quintiles of probability of being a dual† | ||||||||
| 1 | 26,239 | 13.37 | −0.0218*** | 0.00924*** | 0.0180*** | −0.0175*** | 0.0270*** | −0.0123* |
| 2 | 26,212 | 16.63 | −0.0206*** | 0.0100*** | 0.0210*** | −0.0185*** | 0.0308*** | −0.0159*** |
| 3 | 26,279 | 20.82 | −0.0185*** | 0.00855*** | 0.0190*** | −0.0147*** | 0.0279*** | −0.00980* |
| 4 | 25,927 | 27.54 | −0.0167*** | 0.00775*** | 0.0192*** | −0.0163*** | 0.0271*** | −0.0105** |
| 5 | 26,034 | 33.71 | −0.0145*** | 0.00928*** | 0.0161*** | −0.0018*** | 0.0214*** | −0.00171 |
| From hospitals that own IRF | ||||||||
| No | 73,701 | 22.00 | −0.0188*** | 0.0112*** | 0.0189*** | −0.0084*** | 0.0289*** | −0.00639 |
| Yes | 49,989 | 21.87 | −0.0187*** | 0.00954*** | 0.0199*** | −0.0176*** | 0.0251*** | −0.00960** |
| From hospitals that own SNF | ||||||||
| No | 83,029 | 22.46 | −0.0190*** | 0.0117*** | 0.0150*** | −0.00919** | 0.0253*** | −0.00929** |
| Yes | 40,661 | 20.91 | −0.0161*** | 0.00946*** | 0.0296*** | −0.0161*** | 0.0295*** | −0.00154 |
| Rurality | ||||||||
| Low | 69,071 | 21.14 | −0.0202*** | 0.0094*** | 0.0191*** | −0.0167*** | 0.0301*** | −0.0153*** |
| High | 69,029 | 23.31 | −0.0161*** | 0.0101*** | 0.0175*** | −0.0069** | 0.0217*** | −0.0034 |
Note.
p < 0.01
p < 0.05
p < 0.1.
The probabilities are estimated using demographic characteristics, education, Elixhauser and Deyo indexes, length of stay at the hospital, hospital admission DRG, and origin ZIP code fixed effects.
Robust z-statistics in brackets.
CNA, certified nursing assistant; FTE, full-time equivalent; IRF, inpatient rehabilitation facility; LPN, licensed practical nurse; RN, registered nurse; RUGS, resource utilization group.
Although the estimated discharge functions for hospitals with different IRF or SNF ownership exhibit similar patterns, differential discharge in terms of RN staffing is higher for hospitals that own an SNF or IRF. When we estimate the discharge function separately for rural and urban areas, we find that differential discharge in terms of staffing is relatively lower in rural areas. However, an average urban patient has 78 alternative SNFs in the choice set, whereas a rural patient chooses from only 38 SNFs.
Discussion
Using a detailed, national database of hospitalized patients discharged to an SNF for the first time, we found that dual-eligible patients from the same hospital are discharged to SNFs with worse quality of care compared with their Medicare-only counterparts. This discrepancy is not due to the residential location of the patients. Moreover, these findings hold regardless of diagnosis, demographic characteristics, and whether the patient lives in an urban or rural setting.
Financial considerations may explain why dual eligibles are discharged to lower quality SNFs. For the first 20 days, the SNF care of dual eligibles is reimbursed at the same level as other Medicare beneficiaries. However, after 20 days, there is a copayment, typically paid out-of-pocket or through supplemental insurance for the Medicare-only population. For dually eligible patients, the copayment is supposed to be paid through Medicaid, but most states pay a reduced rate, or nothing at all (AHCA 2013). Historically, the federal government has made up some of this “bad debt,” but some uncertainty exists as to whether this will continue, moving forward. Moreover, today's short-stay patient in an SNF is often tomorrow's long-stay nursing home resident. After dual-eligibles exhaust their SNF eligibility, their care is reimbursed by Medicaid, a less generous payer of nursing home services. For nonduals, long-stay care is typically paid at a higher private-pay price. Thus, in an effort to maximize revenue before, during, and after the SNF stay, nursing homes prefer non–dually eligible beneficiaries. This preference has invariably led to some sorting in which higher quality SNFs differentially attract the highest revenue beneficiaries.
Besides financial considerations, other factors may explain the discharge of dual eligibles to lower quality SNFs. Three agents are involved in the discharge procedure: the patient, the hospital discharge planner, and the SNF admission coordinator. Although it is possible (though unlikely) that the difference we observe in SNF quality of care is a result of patient preferences, discharge planners should still refer patients to SNFs with adequate resources to provide SNF care and in close proximity to the beneficiary's residence. A large literature has stressed the importance of distance in the choice of a nursing home (e.g., Zwanziger, Mukamel, and Indridason 2002; Shugarman and Brown 2006). The fact that duals are consistently assigned to lower resource SNFs, even after controlling for their place of residence and health status, suggests a “disparity” in care that likely cannot be explained by preferences alone. Another explanation for our findings is the possible incongruity in what discharge planners believe patients want and what these patients truly prefer. Further research is needed to clarify whether sociocultural and educational incongruity between discharge planners and patients translates into misunderstandings about patients' preferences and expectations.
Research will also be needed to evaluate the extent to which stereotyping, discrimination, or bias exists in the hospital setting. Because dual eligibles typically have fewer resources, they may have less ability to take an active role in choosing an SNF relative to other Medicare beneficiaries. Although we control for race in our regression analyses, dual eligibles may experience discrimination based on their socioeconomic status from discharge planners and SNFs. As a result, dual eligibles may be disproportionately admitted to low-quality, low-resource SNFs.
This study also contributes to a growing literature which attempts to decompose disparities into “across-facility” and “within-facility” variation in services (Chandra and Skinner 2003). In the case of our study, we find large within-facility variation in Medicare-only and dually eligible patients discharged from a common hospital. Future research will need to explore the variation for these populations across states, regions (urban vs. rural), and hospital types (e.g., proprietary vs. nonprofit; large vs. small; etc.). In particular, the role of state Medicaid policy for the dually eligible population may be particularly important in this context.
Limitations
Although we estimate the choice set and discharge function for Medicare beneficiaries, we are not able to identify the exact mechanisms underlying our findings. Our results show stark discrepancies in the SNFs that duals are discharged to relative to their Medicare-only counterparts. However, additional research is needed to understand the factors that drive SNF referral decision-making from the perspective of the hospital (discharge planner), the patient, and the admitting SNF.
Our findings suggest that dual eligibles are admitted to lower quality SNFs, but we are unable to say that this directly affects their outcomes. However, given the relationship between low-quality and poor outcomes found in many previous studies, it does not seem farfetched to assume that dual eligibles experience worse health outcomes based on their differential discharge to lower quality SNFs. Future research should examine the effect of differential discharge due to dual-eligibility status on outcomes such as rehospitalization and discharge disposition.
Policy makers, hospital discharge planners, and SNF administrators should ensure equal access to high-quality care for all patients. Although much effort has been placed on eliminating racial, ethnic, and gender disparities in health care, the policy and provider communities should also focus on another vulnerable subgroup: Medicaid-eligible Medicare beneficiaries.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This work was supported by the National Institute on Aging Grants P01AG027296 (PI: Vincent Mor) and Ro1AG034179 (PI: David C. Grabowski).
Disclosure: None.
Disclaimer: None.
Supporting Information
Additional supporting information may be found in the online version of thisarticle:
Author Matrix.
Sample Selection Criterion.
Plot of Marginal Effects.
References
- AHCA. 2013. Uncompensated Care Medicare Bad Debt Coverage to Skilled Nursing Facility: A Critical Lifeline [accessed on March 20, 2013]. Available at http://www.ahcancal.org/advocacy/issue_briefs/Issue%20Briefs/IBEliminatingMedicareBadDebtPayments.pdf.
- Baicker K, Buckles KS, Chandra A. Geographic Variation in the Appropriate Use of Cesarean Delivery. Health Affairs (Millwood) 2006;25(5):w355–67. doi: 10.1377/hlthaff.25.w355. [DOI] [PubMed] [Google Scholar]
- Baicker K, Chandra A, Skinner JS. Geographic Variation in Health Care and the Problem of Measuring Racial Disparities. Perspectives in Biology and Medicine. 2005;48(1 Suppl):S42–53. [PubMed] [Google Scholar]
- Baicker K, Chandra A, Skinner JS, Wennberg JE. Who You Are and Where You Live: How Race and Geography Affect the Treatment of Medicare Beneficiaries. Health Affairs (Millwood) 2004;Suppl Variation:VA33–44. doi: 10.1377/hlthaff.var.33. [DOI] [PubMed] [Google Scholar]
- Carter MW, Porell FW. Variations in Hospitalization Rates among Nursing Home Residents: The Role of Facility and Market Attributes. Gerontologist. 2003;43(2):175–91. doi: 10.1093/geront/43.2.175. [DOI] [PubMed] [Google Scholar]
- Castle NG. Nursing Home Caregiver Staffing Levels and Quality of Care. Journal of Applied Gerontology. 2008;27(4):375–405. [Google Scholar]
- Castle NG, Anderson RA. Caregiver Staffing in Nursing Homes and Their Influence on Quality of Care: Using Dynamic Panel Estimation Methods. Medical Care. 2011;49(6):545–52. doi: 10.1097/MLR.0b013e31820fbca9. [DOI] [PubMed] [Google Scholar]
- Centers for Medicare and Medicaid Services. 2010. Design for Nursing Home Compare Five-Star Quality Rating System: Technical Users' Guide [accessed on February 15, 2010]. Available at https://www.cms.gov/CertificationandComplianc/Downloads/usersguide.pdf.
- Davies PS, Greenwood MJ, Li H. A Conditional Logit Approach to U.S. State-to-State Migration. Journal of Regional Science. 2002;41(2):337–60. [Google Scholar]
- Deyo RA, Cherkin DC, Ciol MA. Adapting a Clinical Comorbidity Index for Use with ICD-9-CM Administrative Databases. Journal of Clinical Epidemiology. 1992;45(6):613–9. doi: 10.1016/0895-4356(92)90133-8. [DOI] [PubMed] [Google Scholar]
- Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity Measures for Use with Administrative Data. Medical Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- Feng Z, Lepore M, Clark MA, Tyler D, Smith DB, Mor V, Fennell ML. Geographic Concentration and Correlates of Nursing Home Closures: 1999–2008. Archives in Internal Medicine. 2011;171(9):806–13. doi: 10.1001/archinternmed.2010.492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haber SG, Mitchell JB. Access to Physicians' Services for Vulnerable Medicare Beneficiaries. Inquiry. 1999;36(4):445–60. [PubMed] [Google Scholar]
- Harrington C, Zimmerman D, Karon SL, Robinson J, Beutel P. Nursing Home Staffing and Its Relationship to Deficiencies. Journals of Gerontology Series B. 2000;55:S1–10. doi: 10.1093/geronb/55.5.s278. [DOI] [PubMed] [Google Scholar]
- Hyer K, Thomas KS, Branch L, Harman J, Weech-Maldonado R, Johnson CE. The Influence of Nurse Staffing Levels on Quality of Care in Nursing Homes. Gerontologist. 2011;51(5):610–6. doi: 10.1093/geront/gnr050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Intrator O, Hiris J, Berg K, Miller SC, Mor V. The Residential History File: Studying Nursing Home Residents' Long-Term Care Histories(*) Health Services Research. 2011;46(1 Pt 1):120–37. doi: 10.1111/j.1475-6773.2010.01194.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kane RA, Priester R, Kane RL. The Future of the Nursing Home in a Rebalanced Long-Term Supportive Services (LTSS) System. Unpublished report; 2008. [Google Scholar]
- Komisar HL, Feder J, Kasper JD. Unmet Long-Term Care Needs: An Analysis of Medicare-Medicaid Dual Eligibles. Inquiry. 2005;42:171–82. doi: 10.5034/inquiryjrnl_42.2.171. [DOI] [PubMed] [Google Scholar]
- Liu K, Doty P, Manton K. Medicaid Spenddown in Nursing Homes. Gerontologist. 1990;30(1):7–15. doi: 10.1093/geront/30.1.7. [DOI] [PubMed] [Google Scholar]
- McFadden D. Conditional Logit Analysis of Qualitative Choice Behavior. In: Zarembka P, editor. Frontiers in Econometrics. New York: Academic Press; 1974. pp. 105–42. [Google Scholar]
- McFadden D. Modeling the Choice of Residential Location. In: Karlqvist A, Lundqvist L, Snickars F, Weibull J, editors. Spatial Interaction Theory and Planning Models. Amsterdam: North Holland; 1978. pp. 75–96. , and . “ .” , edited by. [Google Scholar]
- Medpac. 2012 Washington, DC: Medicare Payment Advisory Commission, A Data Book: Health Care Spending and the Medicare Program.
- Merrill K, Colby DC, Hogan C. Medicare Beneficiaries Covered by Medicaid Buy-In Agreements. Health Affairs. 1997;16(1):175–84. doi: 10.1377/hlthaff.16.1.175. [DOI] [PubMed] [Google Scholar]
- Mor V, Zinn J, Angelelli J, Teno JM, Miller SC. Driven to Tiers: Socioeconomic and Racial Disparities in the Quality of Nursing Home Care. Milbank Quarterly. 2004;82(2):227–56. doi: 10.1111/j.0887-378X.2004.00309.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Connor GT, Quinton HB, Traven ND, Ramunno LD, Dodds TA, Marciniak TA, Wennberg JE. Geographic Variation in the Treatment of Acute Myocardial Infarction: The Cooperative Cardiovascular Project. Journal of the American Medical Association. 1999;281(7):627–33. doi: 10.1001/jama.281.7.627. [DOI] [PubMed] [Google Scholar]
- Shugarman LR, Brown JA. Nursing Home Selection: How Do Consumers Choose? Volume I: Findings from Focus Groups of Consumers and Information Intermediaries. Washington, DC: Prepared for Office of Disability, Aging and Long-Term Care Policy, Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services; 2006. , and , Contract #HHS-100-03-0023. [Google Scholar]
- Steffen TM, Nystrom PC. Organizational Determinants of Service Quality in Nursing Homes. Hospital and Health Services Administration. 1997;42(2):179–91. [PubMed] [Google Scholar]
- Stevenson DG. Nursing Home Consumer Complaints and Quality of Care: A National View. Medical Care Research and Review. 2006;63:347–68. doi: 10.1177/1077558706287043. [DOI] [PubMed] [Google Scholar]
- The Henry J. Kaiser Family Foundation. 2009. Dual Eligibles: Medicaid's Role for Low-Income Medicare Beneficiaries [accessed on September 13, 2010, 2009]. Available at www.kff.org/medicaid/upload/4091_06.pdf. [PubMed]
- Thorpe KE, Philyaw M. Impact of Health Care Reform on Medicare and Dual Medicare-Medicaid Beneficiaries. Cancer. 2010;16(6):584–7. doi: 10.1097/PPO.0b013e3181ff3156. [DOI] [PubMed] [Google Scholar]
- Welch WP, Miller ME, Welch HG, Fisher ES, Wennberg JE. Geographic Variation in Expenditures for Physicians' Services in The United States. New England Journal of Medicine. 1993;328(9):621–7. doi: 10.1056/NEJM199303043280906. [DOI] [PubMed] [Google Scholar]
- Zwanziger J, Mukamel DB, Indridason I. Use of Resident-Origin Data to Define Nursing Home Market Boundaries. Inquiry. 2002;39(1):56–66. doi: 10.5034/inquiryjrnl_39.1.56. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Author Matrix.
Sample Selection Criterion.
Plot of Marginal Effects.


