Abstract
Intrauterine devices (IUDs) are one of the most reliable and cheapest contraception methods. Our aims are to evaluate misplaced IUDs with radiological findings and to emphasise the importance of radiological imaging. We report two cases with radiological findings, one of complete migration to the abdomen without colonic perforation and one of partial migration to the bladder lumen with pregnancy. Uterine perforation and migration of IUDs are rare and undesirable complications. Suspected intra-abdominal IUDs can be evaluated with CT for precise localisation and possible complications without pregnancy.
Background
Intrauterine devices (IUDs) are one of the most reliable and cheapest contraception methods and are commonly used throughout the world.1 Although IUDs are effective, various complications, including bleeding, infection, ectopic pregnancy and uterine perforation, have been identified.2 The uterine wall might be eroded completely or partially by an IUD, causing uterine perforation, with an incidence of 0–1.3/1000 insertions.3 Although a rare complication, perforation can lead to IUD migration into the bladder, bowel, peritoneum or the appendix2 and to serious morbidities associated with peritoneal and omental adhesion, volvulus, urethrocutaneous fistula and bowel perforation.4 In this report, we present 2 cases of an ectopic IUD in the bladder and intra-abdominal cavity with sonographic and radiographic findings.
Case presentation
Case 1
A 46-year-old woman was admitted to our clinic with secondary amenorrhoea for 5 weeks and lower abdominal pain lasting for 2 years. The medical history of the patient revealed that a copper-T-Cu 380-A IUD had been inserted into the uterine cavity by a gynaecologist.
Case 2
A 34-year-old woman was admitted to our clinic with lower left abdominal pain lasting for 1 year. The patient's medical history revealed that a copper-T-Cu 380-A IUD had been inserted into the intrauterine cavity by a gynaecologist.
Investigations
Case 1
The IUD strings were not visible on gynaecological examination. Transabdominal ultrasonography (US) showed a hyperechogenic IUD partially embedded in the wall of the cervix and extending into the bladder lumen (figure 1). A gestational sac compatible with 5 weeks with a yolk sac was also detected in the uterine cavity (figure 2). Fetal cardiac activity and the embryo were not visualised due to early gestational age.
Figure 1.
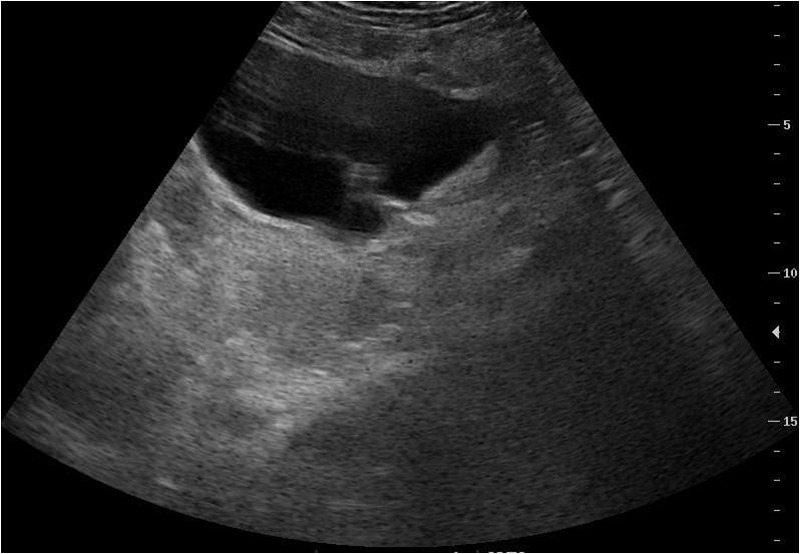
Transabdominal ultrasonography showed hyperechogenic misplaced intrauterine device partially embedded in the wall of the cervix and extended to the bladder lumen.
Figure 2.
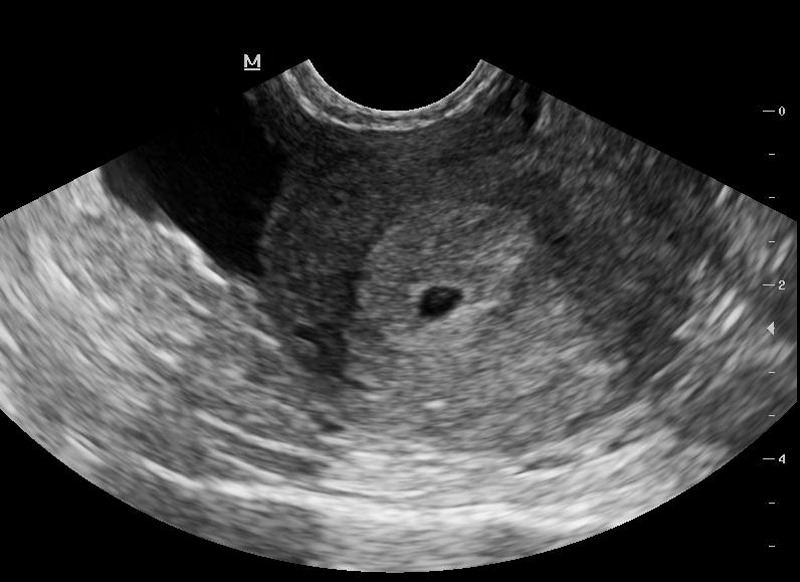
Transabdominal ultrasonography showed approximately 5 weeks gestational sac in the uterine cavity.
Case 2
The IUD strings were not visible on gynaecological examination. Physical examination was otherwise unremarkable. Plain abdominal radiography showed the IUD in the lower left quadrant of the abdomen (figure 3). CT was performed, and a hyperdense structure compatible with an IUD was seen in the pericolic fatty tissue adjacent to the descending colon without any colonic perforation (figure 4).
Figure 3.

Abdominal-pelvic radiography revealed misplaced intrauterine device in the left lower quadrant.
Figure 4.
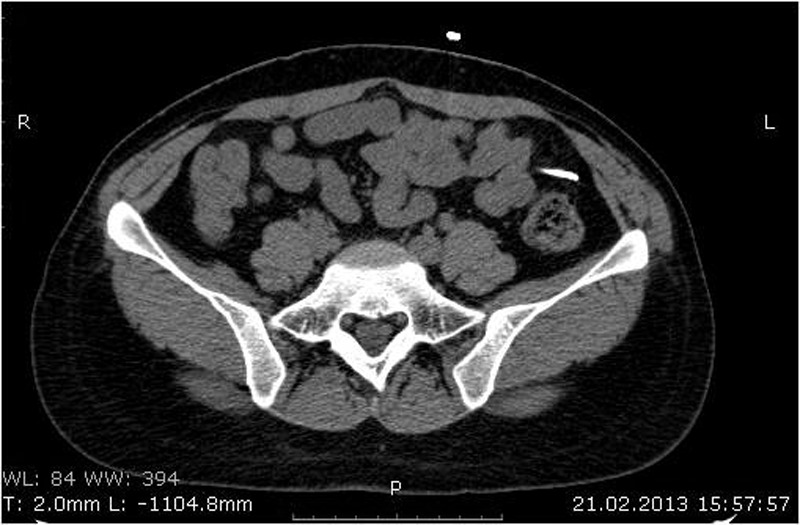
Abdominal CT demonstrated misplaced intrauterine device in the pericolic fatty tissue adjacent to the descending colon.
Differential diagnosis
Depending on the migrated plane, the differential diagnosis varies from bladder stones to foreign bodies.
Treatment
Case 1
On patient's request, the pregnancy was terminated by dilation and curettage, and the IUD removed through cystoscopy without any complications.
Case 2
The patient refused the laparoscopic abdominal surgery and did not return for follow-up examinations.
Outcome and follow-up
Case 1
The patient was discharged after removal of the IUD with antibiotic therapy.
Discussion
IUDs are the most popular reversible contraception method but, in rare cases, can cause uterine perforation. The mechanism is unknown, but there are underlying risk factors such as congenital anomalies, infections, a history of abortion5 and hypoestrogenism, which can cause thinning of the uterine wall in the first 6 months of postpartum lactation period.5 6 Perforation can be seen during the insertion of the IUD or later. In a case report and literature review, Kassab and Audra et al 7 reported migration of the IUD to the omentum, rectosigmoid, peritoneum, bladder, appendix, small intestine, adnexal and iliac vein. Migration of the IUD into the abdominal and pelvic cavity and the adjacent organs is a rare complication of uterine wall perforation. As a result of migration to the peritoneal cavity, peritoneal and omental adhesions, volvulus, enterocutaneous fistula and bowel perforation have been seen.4 Intravesical migration is rare, but 50 cases have been reported in the literature.8 IUDs can float in the bladder or be embedded in the bladder wall. In addition to asymptomatic cases, patients can present chronic pelvic pain, vaginal discharge, dysuria, haematuria, recurrent urinary tract infections and irritation during voiding. Formation of stones of diameter 1–8 cm in the bladder due to bladder migration of the IUD has also been reported in the literature.9 Patients with a pregnancy and IUD history must be evaluated for perforation of the uterus. With or without pregnancy, all intravesical IUDs must be removed because of the potential complications.
Two types of IUDs are commonly available in our country: copper-containing IUDs (TCu 380A (Paraguard); Barr Pharmaceuticals, Ponoma, New York, USA) and levonorgestrel-releasing IUDs (LNG 20 (Mirena); Bayer Health-care Pharmaceuticals, Wayne, New Jersey, USA). Copper wire and levonorgestrel-releasing IUDs are radiopaque in plain radiography and CT. Copper wire is hyperechoic in US; however, levonorgestrel-releasing IUDs are invisible in sonographic examinations because they include barium sulfate.6 The coexistence of pregnancy and misplaced IUDs should be evaluated first by transabdominal or transvaginal US, especially in patients with amenorrhoea. After ruling out pregnancy, the best and least expensive method for detecting a misplaced IUD is plain abdominopelvic radiography.10 US can be useful in the evaluation of patients with a suspected intravesical IUD. IUDs misplaced in the abdomen can be assessed by CT for precise localisation and for detecting accompanying complications.2
Despite the different treatment options available, surgical approaches such as laparotomy and laparoscopy are frequently recommended for the treatment of abdominal IUDs. Intra-abdominal laparoscopy is the most preferred method, with a success rate of 44–100%.11 12 In comparison, laparotomy has a limited field of view and can lead to scar formation and prolonged hospitalisation.10 Cystoscopy and suprapubic cystoscopic procedures can be used for the treatment of intravesical IUDs.1 In our first case which involved an intravesical IUD, the IUD was removed by cystoscopy without any complications, and the patient was discharged from the hospital with antibiotic therapy. In our second case, an IUD was detected in the paracolic fatty tissue; however, the patient did not accept the surgical treatment, and the surgeons decided to follow up with the patient. She was discharged from the hospital with medical advice.
Learning points.
Ultrasonography and periodic examinations should be performed after the insertion of the intrauterine device (IUD).
Pregnancy with IUD must be evaluated with sonography for uterine perforations.
Suspected intrabdominal IUD can be evaluated with plain abdominopelvic radiography and CT can be performed for the exact localisation and detection of complications for the misplaced IUD in patients without pregnancy.
Footnotes
Contributors: All authors participated in the conception and design, acquisition of data or analysis and interpretation of data, drafting the article or revising it critically for important intellectual content and final approval of the version published.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Kandirali E, Topcuoglu M, Semercioz A, et al. Double intrautein device: presented with protruding urethral stone. Marmara Med J 2008;1:61–3 [Google Scholar]
- 2.Sinha M, Gupta R, Tiwari A. Minimally invasive surgical approach to retrieve migrated intrauterine contraceptive device. Int J Reprod Contracept Obstet Gynecol 2013;2:147–51 [Google Scholar]
- 3.Heinberg EM, McCoy TW, Pasic R. The perforated intrauterine device: endoscopic retrieval. JSLS 2008;12:97–100 [PMC free article] [PubMed] [Google Scholar]
- 4.Inceboz US, Ozcakir HT, Uyar Y, et al. Migration of an intrauterine contraceptive device to the sigmoid colon: a case report. Eur J Contracept Reprod Health Care 2003;8:229–32 [PubMed] [Google Scholar]
- 5.Behtas N, Akhavan S, Mokhtar S. Pelvic mass due to transmigrated IUD. Acta Med Iran 2010;48:125–6 [PubMed] [Google Scholar]
- 6.Boortz HE, Margolis DJ, Raqavendra N, et al. Migration of intrauterine devices: radiologic findings and implications for patient care. Radiographics 2012; 32:335–52 [DOI] [PubMed] [Google Scholar]
- 7.Kassab B, Audra P. The migrating intrauterine devices. Case report and review of literature. Contracept Fertil Sex 1999;27:696–700 [PubMed] [Google Scholar]
- 8.Hick EJ, Hernandez J, Yordan R, et al. Bladder calculus resulting from the migration of an intrauterine contraceptive device. J Urol 2004;172(5 Pt 1):1903. [DOI] [PubMed] [Google Scholar]
- 9.Istanbulluoglu MO, Ozcimen EE, Ozturk B, et al. Bladder perforation related to intrauterine device. J Chin Med Assoc 2008;71:207–9 [DOI] [PubMed] [Google Scholar]
- 10.Bozkurt M, Yumru AE, Coskun EI, et al. Laparoscopic management of a translocated intrauterine device embedded in the gastric serosa. J Pak Med Assoc 2011;61:1020–2 [PubMed] [Google Scholar]
- 11.Balci O, Capar M, Mahmoud AS, et al. Removal of intra-abdominal mislocated intrauterine devices by laparoscopy. J Obstet Gynaecol 2011;31:650–2 [DOI] [PubMed] [Google Scholar]
- 12.Miranda L, Settembre A, Capasso P, et al. Laparoscopic removal of an intraperitoneal translocated intrauterine contraceptive device. Eur J Contracept Reprod Health Care 2003;8:122–5 [PubMed] [Google Scholar]


