Abstract
Herpes zoster and chickenpox are caused by a single virus, varicella-zoster virus. Herpes zoster ophthalmicus-associated ophthalmoplegia is well documented. Very rarely, herpes zoster and chickenpox cause external ophthalmoplegia. A 48-year-old man was diagnosed with chickenpox and treated with intravenous acyclovir. He suddenly reported diplopia and restricted left eye movement. MRI of the orbit revealed thickening and abnormal contrast enhancement of the preseptal space and lateral rectus muscle of the left eye. In this case, external ophthalmoplegia occurred following chickenpox with radiological evidence of orbital myositis. To the best of our knowledge, this is the first case report of external ophthalmoplegia of radiologically confirmed orbital myositis after chickenpox infection.
Background
Varicella-zoster virus (VZV) is a DNA virus belonging to the Herpesviridae family; it can manifest as two clinical conditions, varicella (chickenpox) and herpes zoster (shingles). Varicella usually occurs as a primary infection in childhood, whereas herpes zoster results from reactivation of the dormant virus within a sensory nerve ganglion after the primary infection, most often in older patients.1
Varicella presents with acute fever and skin rash, which can be accompanied by headache, malaise and loss of appetite. The rash first starts as macules but readily progresses to papules, which crust over and resolve after 1–2 weeks. Varicella is highly contagious and is transmitted through contact with skin lesions or through the respiratory tract in aerosol form. In most cases, however, it subsides spontaneously without complications.2 3 Primary infection in older patients, on the other hand, often has more severe symptoms and complications, including those of the respiratory and central nervous systems, which sometimes can be fatal, especially in immunocompromised individuals.3
According to de Castro et al,1 among the complications of varicella, ocular manifestations include lesions of the eyelid, conjunctiva and cornea; iridocyclitis, glaucoma, cataracts, chorioretinitis, optic neuritis, optic atrophy and internal ophthalmoplegia. External ophthalmoplegia is paralysis of the external ocular muscles. External ophthalmoplegia after herpes zoster ophthalmicus is often reported. In most cases, it results from invasion of the nerve ganglia, but it is rarely radiologically confirmed that the external ophthalmoplegia results from orbital myositis. External ophthalmoplegia as a complication from varicella rather than from herpes zoster, however, has been rarely reported, and there are no case reports of radiologically confirmed orbital myositis. We report a case of external ophthalmoplegia caused by isolated unilateral lateral rectus involvement that was radiologically confirmed following primary varicella infection.
Case presentation
A 48-year-old man presented to the emergency room reported fever and chills. One week earlier, he had a headache and left ocular pain that were treated with oral non-steroidal anti-inflammatory drugs. The patient was in good medical condition except for a history of hypertension. He had no previous remarkable ocular history. The day he presented to the emergency room, multiple painful vesicular eruptions appeared on his upper and lower limbs and trunk (figure 1). He was diagnosed with chicken pox and treated with intravenous acyclovir (750 mg three times a day). The day after admission, he reported abrupt diplopia and restricted left eye movement. There was a mild pain that was aggravated when he tried to move his left eye.
Figure 1.
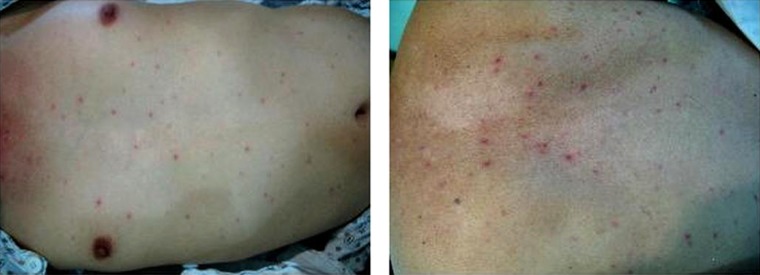
Multiple papular eruptions on the trunk.
Investigations
At initial examination, the patient's visual acuity was 20/20, and the intraocular pressure was 16 mm Hg bilaterally. His pupils were isocoric, with prompt and symmetric light reflexes and there was no ptosis. Slit-lamp examination revealed conjunctival injection in both eyes and funduscopy revealed no remarkable lesions. Exophthalmometric findings were 12 mm in the right eye and 16 mm in the left eye, with a baseline of 119 mm. Krimsky’s test showed left esodeviation of 30 prism dioptres at near and far fixation (figure 2). Hess test revealed marked underaction of the lateral rectus in the left chart and marked overaction of the medial rectus in the right chart (figure 3). Laboratory tests revealed that the anti-VZV IgG levels were 10 times higher than normal. Diffusion-weighted MRI and fluid-attenuated inversion recovery sequences of the orbit showed thickening and abnormal contrast enhancement of the preseptal space and lateral rectus muscle of the left eye (figure 4).
Figure 2.
Nine cardinal photographs of the patient showing limitation of left lateral gaze. He had a left esotropia of 30 prism dioptres in the primary position.
Figure 3.
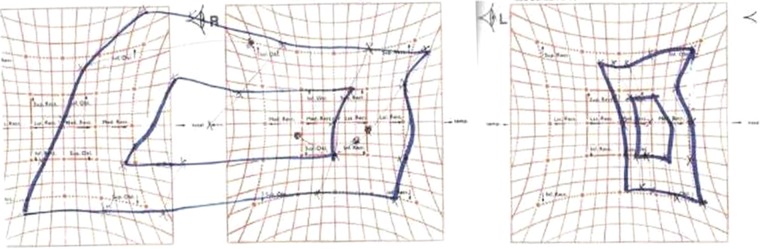
Hess screen test showing an underaction of the lateral rectus muscle of the left eye and an overaction of the medial rectus muscle of the right eye.
Figure 4.
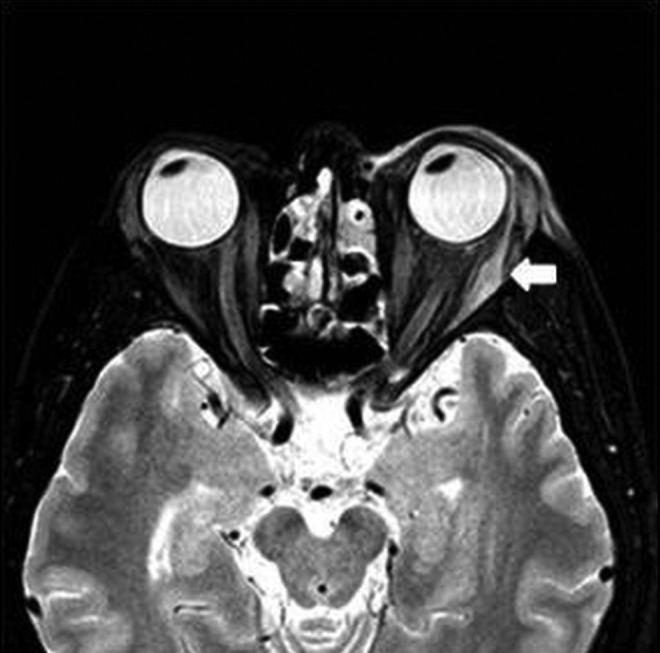
T1-weighted MRI showing thickening and enhancement (arrow) of the lateral rectus muscle.
Outcome and follow-up
After being diagnosed with an orbital pseudotumour, the patient was started on intravenous methylprednisolone (650 mg). Ten days later, his skin lesions and proptosis had improved, but there was no significant change in his ocular motility. Two months after the chickenpox infection, ocular motility showed no improvement.
Discussion
The VZV causes both varicella and herpes zoster. After varicella infection, VZV does not disappear from the body but becomes dormant within the dorsal root and cranial nerve sensory ganglia for decades. The virus gets reactivated when VZV-specific cell-mediated immunity is weakened, resulting in herpes zoster. In particular, the term herpes zoster ophthalmicus refers to the condition in which the ophthalmic division of the fifth cranial nerve is involved.
Herpes zoster mostly invades sensory neurons, and motor neurons are rarely involved. External ophthalmoplegia from herpes zoster ophthalmicus is reported in up to one-third of the cases.4 5 In general, external ophthalmoplegia after herpes zoster ophthalmicus is considered to result from cranial nerve palsy. Most cases show remission within 1 year; the third cranial nerve is most often affected and the fourth cranial nerve is least often affected.6 In addition to neuronal involvement, external ophthalmoplegia cases resulting from orbital myositis after herpes zoster ophthalmicus have been reported.5 Previously reported cases of radiologically confirmed orbital myositis were determined to result from herpes zoster ophthalmicus-associated ophthalmoplegia.
The pathophysiology by which external ophthalmoplegia arises from herpes zoster ophthalmicus remains unclear and is speculated to have multiple mechanisms.7 The two main theories to date are a direct viral cytopathic effect of the virus and a reactive immunological response to the virus.8 9 In one case, improvement of symptoms was reported following an increase in the acyclovir dose and a reduction of the prednisone dose, suggesting a direct viral cytopathic effect.10 The latter theory concerns contiguous orbital inflammation, cranial vasculitis, perineuritis, peripheral nerve demyelination, myositis, brainstem encephalitis and meningitis. Sanjay et al7 reported MRI findings of extraocular muscle enlargement (33%) and orbital soft tissue swelling (17%) as evidence for perineuritis as a pathophysiological mechanism; they also suggested that the high incidence of mydriasis (85%) and complete ptosis (70%) are evidence for a neurogenic mechanism.
It is uncertain whether the ophthalmoplegia in the present case was only of muscular origin or combined with nerve involvement. This case, however, clearly showed left lateral rectus muscle paralysis on physical examination and Hess testing, which was supported by signal enhancement in the preseptal space and lateral rectus muscle in the left orbit on MRI, in an adult patient with primary VZV infection clinically manifesting symptoms similar to previously reported herpes zoster ophthalmicus-associated ophthalmoplegia. There are a few reports of external ophthalmoplegia after varicella,11 12 but no reports of it being a complication of radiologically confirmed orbital myositis. Previous case reports were a result of cranial nerve palsies that included the oculomotor and abducens nerves.
In conclusion, primary VZV infection can clinically manifest similar to herpes zoster ophthalmicus-related external ophthalmoplegia, and this complication can be a result of orbital myositis, as was radiologically confirmed in this case. To the best of our knowledge, this is the first report of a case of external ophthalmoplegia following chickenpox combined with radiologically confirmed orbital myositis.
Learning points.
External ophthalmoplegia (paralysis of the external ocular muscles) can develop in association with primary varicella infection.
The pathogenesis of external ophthalmoplegia associated with varicella is unclear, but could be related to orbital myositis.
In patients with varicella-zoster virus-associated ophthalmoplegia, orbital MRI studies are important for determining the existence of orbital myositis.
Footnotes
Contributors: S-JL, J-HK and MK treated the patient and in doing so acquired the case data; they were also involved with drafting of the manuscript. All the authors read and approved the final manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Fernández de Castro LE, Sarraf OA, Hawthorne KM, et al. Ocular manifestations after primary varicella infection. Cornea 2006;25:866–7 [DOI] [PubMed] [Google Scholar]
- 2.Bozzola E, Tozzi AE, Bozzola M, et al. Neurological complications of varicella in childhood: case series and a systematic review of the literature. Vaccine 2012;30:5785–90 [DOI] [PubMed] [Google Scholar]
- 3.Shin MK, Choi CP, Lee MH. A case of herpes zoster with abducens palsy. J Korean Med Sci 2007;22:905–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marsh RJ, Dulley B, Kelly V. External ocular motor palsies in ophthalmic zoster: a review. Br J Ophthalmol 1977;61:677–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Volpe NJ, Shore JW. Orbital myositis associated with herpes zoster. Arch Ophthalmol 1991;109:471. [DOI] [PubMed] [Google Scholar]
- 6.Park KC, Yoon SS, Yoon JE, et al. A case of herpes zoster ophthalmicus with isolated trochlear nerve involvement. J Clin Neurol 2011;7:47–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sanjay S, Chan EW, Gopal L, et al. Complete unilateral ophthalmoplegia in herpes zoster ophthalmicus. J Neuroophthalmol 2009;29:325–37 [DOI] [PubMed] [Google Scholar]
- 8.Lexa FJ, Galetta SL, Yousem DM, et al. Herpes zoster ophthalmicus with orbital pseudotumor syndrome complicated by optic nerve infarction and cerebral granulomatous angiitis: MR-pathologic correlation. Am J Neuroradiol 1993;14:185–90 [PMC free article] [PubMed] [Google Scholar]
- 9.Naumann G, Gass JD, Font RL. Histopathology of herpes zoster ophthalmicus. Am J Ophthalmol 1968;65:533–41 [DOI] [PubMed] [Google Scholar]
- 10.Bourke RD, Pyle J. Herpes zoster ophthalmicus and the orbital apex syndrome. Aust N Z J Ophthalmol 1994;22:77–80 [DOI] [PubMed] [Google Scholar]
- 11.Farooqui AA, Tahir M, Jaiswal A, et al. Oculomotor palsy following varicella in an immunocompetent adult. South Med J 2009;102:445. [DOI] [PubMed] [Google Scholar]
- 12.Nemet P, Ehrlich D, Lazar M. Benign abducens palsy in varicella. Am J Ophthalmol 1974;78:859. [DOI] [PubMed] [Google Scholar]



