Abstract
PURPOSE
The occlusal splint has been used for many years as an effective treatment of sleep bruxism. Several methods have been used to evaluate efficiency of the occlusal splints. However, the effect of the occlusal splints on occlusal force has not been clarified sufficiently. The purpose of this study was to evaluate the effect of occlusal splints on maximum occlusal force in patients with sleep bruxism and compare two type of splints that are Bruxogard-soft splint and canine protected hard stabilization splint.
MATERIALS AND METHODS
Twelve students with sleep bruxism were participated in the present study. All participants used two different occlusal splints during sleep for 6 weeks. Maximum occlusal force was measured with two miniature strain-gage transducers before, 3 and 6 weeks after insertion of occlusal splints. Clinical examination of temporomandibular disorders was performed for all individuals according to the Craniomandibular Index (CMI) before and 6 weeks after the insertion of splints. The changes in mean occlusal force before, 3 and 6 weeks after insertion of both splints were analysed with paired sample t-test. The Wilcoxon test was used for the comparison of the CMI values before and 6 weeks after the insertion of splints.
RESULTS
Participants using stabilization splints showed no statistically significant changes in occlusal force before, 3, and 6 weeks after insertion of splint (P>.05) and participants using Bruxogard-soft splint had statistically significant decreased occlusal force 6 weeks after insertion of splint (P<.05). There was statistically significant improvement in the CMI value of the participants in both of the splint groups (P<.05).
CONCLUSION
Participants who used Bruxogard-soft splint showed decreases in occlusal force 6 weeks after insertion of splint. The use of both splints led to a significant reduction in the clinical symptoms.
Keywords: Occlusal splint, Bruxogard-Soft splint, Occlusal force, Sleep bruxism, Strain-gage
INTRODUCTION
Sleep bruxism is an involuntary activity of the masticatory muscles that is characterized by clenching and/or grinding of the teeth during sleep.1 The occlusal splint has been frequently used as an effective treatment of sleep bruxism to protect teeth from damage caused by forceful jaw muscle contractions or to reduce orafacial pain, if present.2 However, little is known regarding the mechanism of the action of occlusal splints.3,4,5 Most of the studies have examined changes in the masticatory muscles activity before and after application of an occlusal splint4,6,7,8,9,10,11 and they showed that occlusal splint treatment resulted in a decrease in nocturnal masticatory muscle activities in patients with bruxism.2,6,12,13 Furthermore, Kurita et al.3 suggested that the use of the stabilization splint has an effect of reducing hyperactivity and asymmetry in the activity of jaw elevator muscles and consequently brings a stable and physiologically optimal occlusal force from the muscles. In addition, Holmgren et al.14 showed that splints redistribute the load borne by the teeth and masticatory system. It has been suggested that the relief of bruxism symptoms with splint treatment may be a result of redistribution of overloading.15,16 According to these suggestions, redistribution of forces and reduction of bruxism symptoms with use of occlusal splints may change maximum occlusal force that has often been studied as an indicator of functional state of the masticatory system.17,18 Nevertheless, the effect of use of the occlusal splints on occlusal force has not been clarified sufficiently. There is only one study available that evaluated the effect of occlusal splints on occlusal force in patients with masticatory muscles disorders.3
Various splints have been used for treatment of bruxism that are made up of basically two different materials. Although, these occlusal splints have slightly different appearances and properties, in fact, scientific evidence supports the use of hard acrylic resin occlusal splints12,19,20,21 that are preferentially of full coverage, located in the maxillary arch, with simultaneous, even, and bilateral contacts, and have anterior guidance and canine protected articulation.22,23 On the other hand, soft appliances have been less documented in the scientific literature, however some researchers suggest the use of soft-resin appliances24,25,26,27 that are easily fabricated, and may be inserted at an initial appointment, so practitioners may desire the use of soft appliances. One of these soft splints is easily tolerable prefabricated Bruxogard Soft splint that fit tightly to upper arch and provides flat special plane to protect dentition of sleep bruxism patients.
The present study designed to evaluate the effect of the use of occlusal splints on maximum occlusal force of patients with sleep bruxism. For this purpose, the effect of two splints basically fabricated from two different materials that are Bruxogard-soft splint and canine protected hard stabilization splints were evaluated and compared. The null hypothesis was that the use of both occlusal splints would reorganize occlusal force in patients with bruxism in accordance with the improvements of symptoms; however these improvements would stand out more in hard occlusal splint group.
MATERIALS AND METHODS
Twelve students of Dental School of the University of Gazi (ranging age from 18 to 27) with sleep bruxism participated in the present study. This research was reviewed and approved by the Ethics Committee of University of Gazi (Process, 6/7/2007-3). Informed consent was obtained from each participant according to the ethical guidelines recommended by The Helsinki Declaration. The initial inclusion criteria were: Patients who had no reported systemic disease or apparent facial asymmetry, no craniofacial trauma or surgery, no use of any medication, and had full permanent dentition (not including third molars), vital first molars without mesio-occluso-distal restorations. The selected sleep bruxism patients had the following criteria suggested by Rompre et al.28: (a) a history of frequent tooth grinding occurring at least 3 nights per week for the preceding 6 months, as confirmed by a sleep partner; (b) clinical presence of tooth wear; (c) masseter muscle hypertrophy; and (d) report of jaw muscle fatigue or tenderness in the morning.
After these initial inclusion criteria, clinical examination of temporomandibular joint (TMJ) was performed for all the individuals according to the Craniomandibular Index (CMI) of Fricton and Schiffman29 before and 6 weeks after the insertion of splints. The CMI measures tenderness and dysfunction in the stomatognathic system and divided to the subscales: Dysfunction Index (DI) and the Palpation Index (PI). Dysfunction Index (DI) includes items related to limits in range of motion, deviation and/or pain in movement, TMJ noise during movement, TMJ tenderness, and Palpation Index (PI) reflects the muscle tenderness at intraoral jaw muscles and extraoral jaw and neck muscles. In this way, these indexes separate joint problems from muscle problems. CMI has a 0-1 scale and is calculated according to the formula (DI + PI) / 2.
Two types of maxillary occlusal splints were constructed: canine protected hard stabilization splint and Bruxogard-soft splint (Myofunctional Research Co, Waalwijk, Netherlands). Participants were randomly assigned to either of two splint groups. Six of bruxism patients received hard stabilization splints fabricated from autopolymerizing acrylic resin (Akribel, Belmar, Izmir, Turkey). The splints were fabricated covering the maxillary teeth completely, with 2 mm thickness of acrylic resin between maxillary and mandibular first molar teeth. The hard stabilization splint had even, simultaneous occlusal contacts with mandibular buccal cusp tips and incisal edges in the centric relation and had canine protection to separate the opposing posterior teeth during eccentric movement (Fig. 1).
Fig. 1.
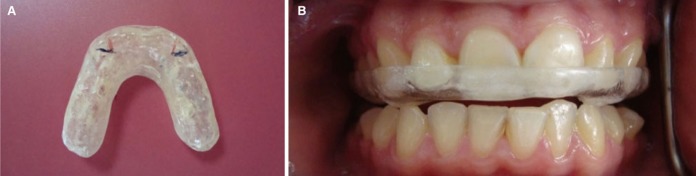
Canine protected hard stabilization splint (A) extraoral view and (B) inraoral view.
Six bruxism patients were used Bruxogard-soft splints that were prepared easily without impression. It was placed into the boiled water for 30 seconds and then soft inner surface of splint inserted to mouth that V-cut of splint was in the centre line of anterior teeth. Then, it was pushed with fingers to seat. Patients were asked close upper and lower teeth slightly just to hold splint in position. The harder occluded surface of splint compared to the inner surface was flat without indents of the lower teeth. Then, Bruxogard soft splint was removed from the mouth and placed in cold water for 20 seconds (Fig. 2).
Fig. 2.
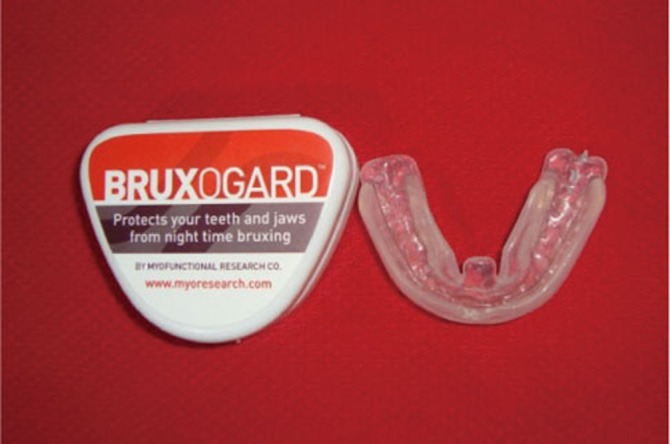
Broxogard Soft splint.
All splints were made and adjusted by the same clinicians. All participants used occlusal splints for 6 weeks, during sleep, at least 8 hours. Participants were instructed not to take any medications, such as muscle relaxants, sleeping pills, transquilizers and antidepressants during the treatment.
Maximum occlusal force was measured from each side of the dental arch using two miniature strain-gage transducers (Model VLPB, Load Cell Central, Monroeton, PA, USA) with stainless steel cases as described previously (Fig. 3).30 Two transducers were placed bilaterally on a flat metal arch. The metal surfaces of the arch were covered with plaster (Betasan, Kocaeli, Turkey). The metal arch and transducers were further covered by a disposable latex finger cot to avoid contamination during measurements. Each transducer has a height of 4 mm and a diameter of 12 mm; with these applications transducers reached a height of 6 mm. Occlusal force was detected as a two-channel signal from each side with a bio-signal acquisition device designed by Kardiosis (Tepa Inc., Kardiosis Ltd., Ankara, Turkey). The force signals were monitored online and then measured on a computer screen as kg (kilogramme), using a specific software program developed by the same company. The calibration of the transducers was performed by loading the transducer with known force values, the deviation from linearity with a load of 5 kg was + 2.66% in right transducer and + 4% in left transducer, 15 kg was + 5.2% in right transducer and + 2.6% in left transducer.
Fig. 3.

Strain gages.
Occlusal force of all participants were performed using 2 mm hard occlusal splints fabricated from hard acrylic resin to avoid damage of teeth, to prevent metal contact of teeth that suppressing maximum occlusal force and to standardize transducers on during measurement of maximum occlusal force.
During the test, participants were seated in an upright position with the head in a natural posture, keeping the Frankfort horizontal plane approximately parallel to the floor. Initially, bilateral transducers that positioned on the metal plate were placed between the first molar teeth on both sides. The transducers were also maintained parallel to the Frankfort horizontal plane during recordings. Participants were instructed to bite as forcefully as possible three times. Before the recordings, the participants were trained to perform their highest possible occlusal force. The highest value of each clenching was recorded and the mean value of the three highest clenching measurements was considered to be the maximum occlusal force. The sum of the right and left occlusal force values was considered to be the maximum occlusal force.
The experimental protocol including clinical examination and recordings of occlusal force was performed by the same investigator. Occlusal force values of participants were recorded before, 3 and 6 weeks after insertion of the splints.
The evaluation of the changes in mean occlusal force values before, 3 weeks and 6 weeks after insertion of both splints were analysed with paired sample t-test. The analysis of differences of occlusal force values between Stabilization and Bruxogard soft splint before treatment, after 3 weeks and 6 weeks was performed with independent samples of t-test. The changes in the amount and percentage of occlusal force, before and 6 weeks after treatment, were analyzed with paired sample t-test for each splint groups. The Wilcoxon test was used for the comparison of the Craniomandibular index values before and 6 weeks after the insertion of splints. Comparison CMI values of both splints before and after treatments were performed with Mann-Whithney U test. Differences at the 5% level of probability were considered statistically significant. All statistical analyses were performed by the SPSS 11.5 (Statistical Package for Social Sciences Software Inc, Chicago, IL, USA).
RESULTS
The mean occlusal force of both splint groups before, 3 and 6 weeeks after insertion of splints are listed in Table 1. There was no statistically significant differences in any intervals in canine protected hard stabilization splint group (Paired t-test; P>.05). There was only a significant difference in occlusal force value between before and 6 weeks after insertion of Bruxogard-soft splints. (Paired t-test; P<.05, P=.032). Independent samples t-test showed no difference between both splint groups before treatment, 3 and 6 weeks after treatment (P>.05: P=.27, P=.73, P=.28, respectively).
Table 1.
Mean occlusal force (kg) and P value of participants before, 3 and 6 weeks after insertion of Bruxogard-soft splints and Stabilization splints
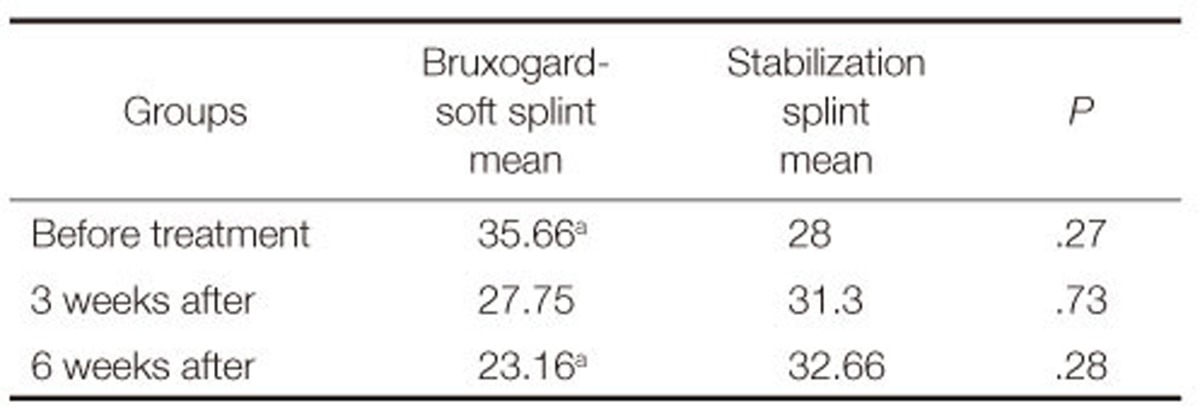
(n=6, paired t-test)
a: Significant at P<.05.
The amount and percentage of changes in mean occlusal force between before and 6 weeks after insertion of both splint groups, were presented in Table 2. The stabilization splint group showed 10 kg and 17% of mean occlusal force increase and the participants used Bruxogard-soft splint group showed 9 kg and 24% of mean occlusal force decrease, and it was statistically significant (P<.05).
Table 2.
Comparison of the changes in the amount and percentage of the mean occlusal force (kg) for both splint groups after the splint treatment
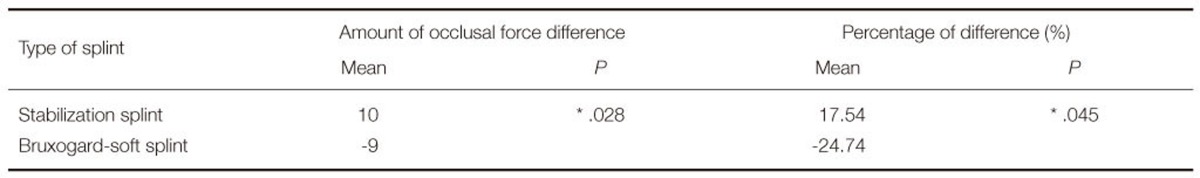
(Mann Whitney U-Test)
*: Significant at P<.05.
Participants included Bruxogard-soft splint and canine protected hard stabilization splint had statistically significant improvement in Cranimandibular index value after treatment (Table 3) (P<.05: P=.043, P=.046, respectively). The comparison of CMI values in both splint groups before and 6 weeks after insertion of splints showed no difference (P>.05: P=.69, P=.81, respectively).
Table 3.
Mean values of Craniomandibular Index (CMI) in participants and P values
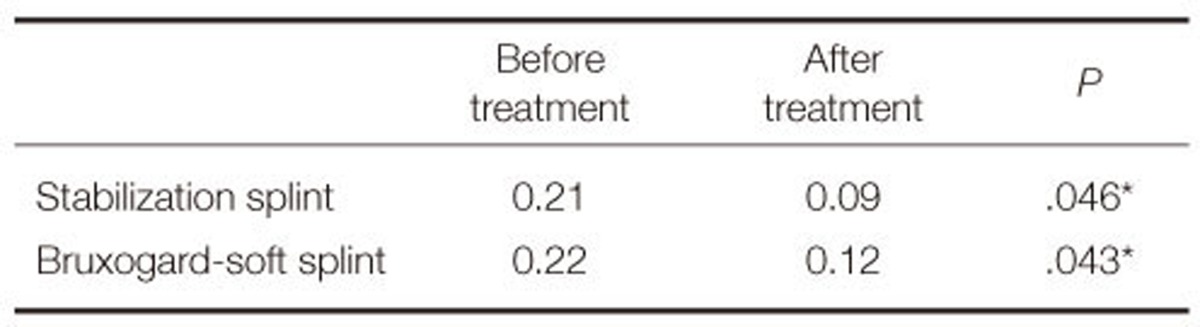
*: Significant at P<.05.
DISCUSSION
The null hypothesis was partially accepted that the use of both occlusal splint showed an improvement of the symptoms, however, contrary to our hypothesis soft splints showed statistical significant alterations in occlusal force.
In the clinical researches, several methods have been used to evaluate efficiency of the occlusal splints. The most of these studies have evaluated the masticatory muscle activities.2,4,5,6,13 It has been stated that the use of occlusal splint reduces the activities of the masseter2 and anterior temporalis muscle;8,9,10,14 and improves the degree of asymmetry in the muscle activity;11 lessens the forces placed on the TMJs and other structures within the masticatory system and in this way lessens the symptoms of bruxism.2 Although it has not been used widely, another method that is measuring the maximum occlusal force may be used to evaluate efficiency of occlusal splints. On the other hand, Holmgren et al.14 stated that the therapeutic mechanism of the occlusal splint should be related to factors that modify and reduce parafunctional activity and/or redistribute its overloading in the masticatory system. In addition, Dylina16 stated that occlusal splints balanced the force distribution in the entire masticatory system. In fact, maximum occlusal force has an influence on muscle efficiency and functional state of masticatory system.17,18 However, there is only one study performed by Kurita et al.3 They have recorded the occlusal force of the patients in masticatory muscle disorders before, 2 and 4 weeks after the use of the stabilization splints. As different from the present study, Kurita et al.3 used Dental Prescale system for measurement of occlusal force. They stated that the occlusal loads in the higher level decreased and, in contrast, those in the lower level increased with the use of the stabilization splint and concluded that the use of splints has the effect of normalizing the occlusal force in patients with masticatory muscle disorders. In the present study, occlusal force of participants who used stabilization splint showed no statistically significant differences after the splint treatment. According to the results of our previous study, the mean maximum occlusal force of healthy participants was 30.16 kg30 and in the present study, the occlusal force value of participants recorded before and after the use of stabilization splint was close to the occlusal force of the healthy participants. It was considered that the lack of difference might be related to the severity of the bruxism and small number of the participated subjects.
On the other hand, CMI values in both splint groups were similar before insertion of splints, and after 6 weeks, participants who used Bruxogard-soft splint and hard stabilization splint showed statistically significant improvements in clinical signs and symptoms. Bruxogard-soft splint has not been studied in the literature. Therefore, the studies related to the soft splints were included to this study to give an idea. In accordance with the result of current study, Wright et al.24 stated that the soft splint was an effective short-term treatment for reducing the signs and symptoms of masticatory muscle pain in the patients. Accordingly, Pettengill et al.27 suggested that soft and hard appliances may be equally useful in reducing the temporomandibular symptoms in short-term appliance therapy.
It has been stated that splints redistributed the load induced by the teeth and masticatory system.14,15 In the current study, while the participants used stabilization splints exerted no significant changes in occlusal force, the use of Bruxogard soft splints led to decreasing of occlusal force. Narita et al.31 stated that jaw clenching with a soft occlusal splint caused a significant decreases in occlusal force as well as significant increase in awareness of tiredness of the muscles and in contrast, the usage of the hard occlusal splint did not cause significant change in the occlusal force and an awareness of tiredness. The occlusal force results of that study is in agreement with the findings of the present study and the current study indicates that both of the splints might have different mechanism on occlusal force distribution for improvement of the clinical symptoms. These splints might redistribute occlusal force in a different way to the stomatognatic system because of their different mechanism that could depend on the splint material or occlusion of splints. However, considering the main limitation of present study which was the small number of subjects, further studies with longer evaluation period should be performed in a larger patient population in order to yield more consistent results regarding the effect of occlusal splints on occlusal force.
CONCLUSION
The use of canine protected hard stabilization splint has not showed significant differences in maximum occlusal force and use of a Bruxogard-soft splint was accompanied by decrease in occlusal force in patients with sleep bruxism. Treatments with both of splints were acceptably successful and led to a significant reduction in the clinical symptoms.
Footnotes
Present study was supported by Cumhuriyet University, Foundation of Scientific Research Projection.
References
- 1.Cosme DC, Baldisserotto SM, Canabarro Sde A, Shinkai RS. Bruxism and voluntary maximal bite force in young dentate adults. Int J Prosthodont. 2005;18:328–332. [PubMed] [Google Scholar]
- 2.Harada T, Ichiki R, Tsukiyama Y, Koyano K. The effect of oral splint devices on sleep bruxism: a 6-week observation with an ambulatory electromyographic recording device. J Oral Rehabil. 2006;33:482–488. doi: 10.1111/j.1365-2842.2005.01576.x. [DOI] [PubMed] [Google Scholar]
- 3.Kurita H, Ikeda K, Kurashina K. Evaluation of the effect of a stabilization splint on occlusal force in patients with masticatory muscle disorders. J Oral Rehabil. 2000;27:79–82. doi: 10.1046/j.1365-2842.2000.00498.x. [DOI] [PubMed] [Google Scholar]
- 4.Roark AL, Glaros AG, O'Mahony AM. Effects of interocclusal appliances on EMG activity during parafunctional tooth contact. J Oral Rehabil. 2003;30:573–577. doi: 10.1046/j.1365-2842.2003.01139.x. [DOI] [PubMed] [Google Scholar]
- 5.Al-Saad M, Akeel RF. EMG and pain severity evaluation in patients with TMD using two different occlusal devices. Int J Prosthodont. 2001;14:15–21. [PubMed] [Google Scholar]
- 6.Hiyama S, Ono T, Ishiwata Y, Kato Y, Kuroda T. First night effect of an interocclusal appliance on nocturnal masticatory muscle activity. J Oral Rehabil. 2003;30:139–145. doi: 10.1046/j.1365-2842.2003.01017.x. [DOI] [PubMed] [Google Scholar]
- 7.Yap AU. Effects of stabilization appliances on nocturnal parafunctional activities in patients with and without signs of temporomandibular disorders. J Oral Rehabil. 1998;25:64–68. doi: 10.1046/j.1365-2842.1998.00194.x. [DOI] [PubMed] [Google Scholar]
- 8.Williamson EH, Lundquist DO. Anterior guidance: its effect on electromyographic activity of the temporal and masseter muscles. J Prosthet Dent. 1983;49:816–823. doi: 10.1016/0022-3913(83)90356-6. [DOI] [PubMed] [Google Scholar]
- 9.Fitins D, Sheikholeslam A. Effect of canine guidance of maxillary occlusal splint on level of activation of masticatory muscles. Swed Dent J. 1993;17:235–241. [PubMed] [Google Scholar]
- 10.Sheikholeslam A, Holmgren K, Riise C. Therapeutic effects of the plane occlusal splint on signs and symptoms of craniomandibular disorders in patients with nocturnal bruxism. J Oral Rehabil. 1993;20:473–482. doi: 10.1111/j.1365-2842.1993.tb01633.x. [DOI] [PubMed] [Google Scholar]
- 11.McCarroll RS, Naeije M, Kim YK, Hansson TL. Short-term effect of a stabilization splint on the asymmetry of submaximal masticatory muscle activity. J Oral Rehabil. 1989;16:171–176. doi: 10.1111/j.1365-2842.1989.tb01330.x. [DOI] [PubMed] [Google Scholar]
- 12.Okeson JP. The effects of hard and soft occlusal splints on nocturnal bruxism. J Am Dent Assoc. 1987;114:788–791. doi: 10.14219/jada.archive.1987.0165. [DOI] [PubMed] [Google Scholar]
- 13.Roark AL, Glaros AG, O'Mahony AM. Effects of interocclusal appliances on EMG activity during parafunctional tooth contact. J Oral Rehabil. 2003;30:573–577. doi: 10.1046/j.1365-2842.2003.01139.x. [DOI] [PubMed] [Google Scholar]
- 14.Holmgren K, Sheikholeslam A, Riise C. Effect of a full-arch maxillary occlusal splint on parafunctional activity during sleep in patients with nocturnal bruxism and signs and symptoms of craniomandibular disorders. J Prosthet Dent. 1993;69:293–297. doi: 10.1016/0022-3913(93)90109-2. [DOI] [PubMed] [Google Scholar]
- 15.Zarb GA, Speck JE. The treatment of temporomandibular joint dysfunction: a retrospective study. J Prosthet Dent. 1977;38:420–432. doi: 10.1016/0022-3913(77)90096-8. [DOI] [PubMed] [Google Scholar]
- 16.Dylina TJ. A common-sense approach to splint therapy. J Prosthet Dent. 2001;86:539–545. doi: 10.1067/mpr.2001.118878. [DOI] [PubMed] [Google Scholar]
- 17.Braun S, Bantleon HP, Hnat WP, Freudenthaler JW, Marcotte MR, Johnson BE. A study of bite force, part 1: Relationship to various physical characteristics. Angle Orthod. 1995;65:367–372. doi: 10.1043/0003-3219(1995)065<0367:ASOBFP>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 18.Kogawa EM, Calderon PS, Lauris JR, Araujo CR, Conti PC. Evaluation of maximal bite force in temporomandibular disorders patients. J Oral Rehabil. 2006;33:559–565. doi: 10.1111/j.1365-2842.2006.01619.x. [DOI] [PubMed] [Google Scholar]
- 19.Lobbezoo F, van der Zaag J, van Selms MK, Hamburger HL, Naeije M. Principles for the management of bruxism. J Oral Rehabil. 2008;35:509–523. doi: 10.1111/j.1365-2842.2008.01853.x. [DOI] [PubMed] [Google Scholar]
- 20.Sheikholeslam A, Holmgren K, Riise C. A clinical and electromyographic study of the long-term effects of an occlusal splint on the temporal and masseter muscles in patients with functional disorders and nocturnal bruxism. J Oral Rehabil. 1986;13:137–145. doi: 10.1111/j.1365-2842.1986.tb00646.x. [DOI] [PubMed] [Google Scholar]
- 21.al-Quran FA, Lyons MF. The immediate effect of hard and soft splints on the EMG activity of the masseter and temporalis muscles. J Oral Rehabil. 1999;26:559–563. doi: 10.1046/j.1365-2842.1999.00421.x. [DOI] [PubMed] [Google Scholar]
- 22.Bonfante G, Ramos Júnior L, Bonfante EA. Restoration of canine guidance on an occlusal splint using amalgam: a clinical report. J Prosthet Dent. 2003;90:420–423. doi: 10.1016/s0022-3913(03)00410-4. [DOI] [PubMed] [Google Scholar]
- 23.Klasser GD, Greene CS. Oral appliances in the management of temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:212–223. doi: 10.1016/j.tripleo.2008.10.007. [DOI] [PubMed] [Google Scholar]
- 24.Wright E, Anderson G, Schulte J. A randomized clinical trial of intraoral soft splints and palliative treatment for masticatory muscle pain. J Orofac Pain. 1995;9:192–199. [PubMed] [Google Scholar]
- 25.Wright EF. Using soft splints in your dental practice. Gen Dent. 1999;47:506–510. [PubMed] [Google Scholar]
- 26.Giedrys-Leeper E. Night guards and occlusal splints. Dent Update. 1990;17:325–329. [PubMed] [Google Scholar]
- 27.Pettengill CA, Growney MR, Jr, Schoff R, Kenworthy CR. A pilot study comparing the efficacy of hard and soft stabilizing appliances in treating patients with temporomandibular disorders. J Prosthet Dent. 1998;79:165–168. doi: 10.1016/s0022-3913(98)70211-2. [DOI] [PubMed] [Google Scholar]
- 28.Rompré PH, Daigle-Landry D, Guitard F, Montplaisir JY, Lavigne GJ. Identification of a sleep bruxism subgroup with a higher risk of pain. J Dent Res. 2007;86:837–842. doi: 10.1177/154405910708600906. [DOI] [PubMed] [Google Scholar]
- 29.Fricton JR, Schiffman EL. Reliability of a craniomandibular index. J Dent Res. 1986;65:1359–1364. doi: 10.1177/00220345860650111701. [DOI] [PubMed] [Google Scholar]
- 30.Koc D, Dogan A, Bek B, Yucel M. Effects of increasing the jaw opening on the maximum bite force and electromyographic activities of jaw muscles. J Dent Sci. 2012;7:14–19. [Google Scholar]
- 31.Narita N, Funato M, Ishii T, Kamiya K, Matsumoto T. Effects of jaw clenching while wearing an occlusal splint on awareness of tiredness, bite force, and EEG power spectrum. J Prosthodont Res. 2009;53:120–125. doi: 10.1016/j.jpor.2009.02.006. [DOI] [PubMed] [Google Scholar]


