Abstract
Background:
A specially designed wire-reinforced endotracheal tube — the Fastrach silicone tube (FTST) designed to facilitate endotracheal intubation through intubating laryngeal mask airway (ILMA) are expensive and not readily available. Hence, it is worth considering alternative such as polyvinyl chloride tracheal tube (PVCT), which is disposable, cheap and easily available. The aim of the present study was to compare the clinical performance of FTST with conventional PVCT for tracheal intubation through ILMA.
Methods:
After informed consent, 60 ASA I-II adults with normal airway undergoing elective surgery were randomly allocated to undergo blind tracheal intubation through ILMA with a FTST or conventional PVCT. Overall success rate, ease of insertion, number of attempts for successful intubation, critical incidence during intubation and post-operative sore throat were compared.
Results:
The overall success rate with FTST was 96.63% and 93.33% with PVCT; in addition, the first-attempt success rate was 86.25% with FTST compared to 82.14% with PVCT. The time taken for intubation was 18.6 ± 6.8 s. in FTST group and 22.42 ± 8.5 s. in PVCT group. Incidence of sore throat was 21.42% in PVCT group compared with 6.89% in FTST group.
Conclusion:
Blind tracheal intubation through an ILMA with the conventional PVCT instead of FTST is a feasible alternative in patients with normal airways.
Keywords: Intubating laryngeal mask airway, polyvinyl chloride tracheal tube, silicon wire-reinforced tracheal tube
INTRODUCTION
Difficult tracheal intubation remains one of the most important cause of mortality and morbidity in anesthesia.[1] The introduction of laryngeal mask airway (LMA) in 1985 by Brain,[2] was a major breakthrough in difficult airway management; however, its role in facilitating tracheal intubation is limited. Intubating laryngeal mask airway (ILMA) was designed to overcome this limitation and since than there have been a number of reports of successful intubation through the ILMA in cases of unanticipated and anticipated difficult airway.[3,4,5,6]
The manufacturers of LMA advocate use of specially designed silicone wire-reinforced tracheal tube Fastrach™ silicone tube (FTST) for tracheal intubation through the ILMA. This tube is straight, soft which follows the curvature of the shaft of the ILMA. They are expensive, less readily available and the lifespan is considerably shorter than that of ILMA itself. There have been few reports of successful tracheal intubation through the ILMA using a conventional as well as reinforced polyvinyl chloride tubes, which are cheap, disposable and readily available.[3,7,8,9]
We therefore designed this study to compare the tracheal intubation through the ILMA with the FTST and Rusch polyvinyl chloride tracheal tube (PVCT) in terms of success rate, ease of tracheal intubation and complication rate.
METHODS
After institutional ethics committee approval and written informed consent, 60 ASA status I and II adults of either sex scheduled for elective surgeries under general endotracheal anesthesia were recruited in the study. Exclusion criteria were patients with Mallampati scores ≥3, morbid obesity and risk of aspiration, upper respiratory tract pathology and mouth opening less than 2 fingers. The patients were randomly allocated by the sealed envelope technique to FTST group (n = 30) or PVCT group (n = 30) to undergo blind tracheal intubation through ILMA. A size 3 ILMA and a 7.0-mm tracheal tube were chosen for women and a size 4 ILMA and a 7.5-mm tracheal tube for male patients. The PVCT was softened by immersion in a sterile water bath heated to 40°C for 1 min.
All patients received oral diazepam 5 mg, ranitidine 150 mg and metoclopramide 10 mg on the morning of surgery. In the operation theater, standard monitors (electrocardiography, oxygen saturation [SaO2 ], NIBP, EtCO2) were applied, intravenous line was secured and Inj. glycopyrrolate 0.2 mg and fentanyl 2 μg/kg IV were given. After preoxygenation, patients were induced with 2 mg/kg propofol and 8% sevoflurane with 50% N2O at a flow rate of 6 L/min. Inhaled induction of anesthesia was continued for 3 min and to achieve adequate depth of anesthesia for insertion of ILMA. ILMA was inserted as per standard guidelines and its cuff was inflated until adequate seal was obtained (max. 30 ml). Appropriate placement and ventilation with ILMA was determined by chest inflation, auscultation of breath sounds, a square-wave capnography and no oropharyngeal leak with peak airway pressures ≥20 cm H2O. If any one of the above criteria were not met, ILMA was repositioned, removed and reinserted or changed to a different size. If ventilation continued to be a problem, patient was excluded from the study. After successful placement of ILMA, anesthesia was maintained with 1-2% isoflurane, 66% nitrous oxide in 33% oxygen and vecuronium bromide.
Each group's designated tracheal tube was inserted through ILMA after proper lubrication. The PVCT was passed into the ILMA with its inherent curve facing forward. Intubation was considered successful if the endotracheal tube (ETT) could be passed through the ILMA and tracheal placement was confirmed by end-tidal CO2. The ease of tracheal intubation was judged by the time taken to intubate the trachea (time from disconnection of the breathing circuit of the ILMA to confirmation of tracheal tube placement by auscultation and display of a square-wave capnograph trace) and the number of attempts to achieve successful intubation. In each patient, intubation through the ILMA was limited to three attempts. Intubation was considered successful on the first attempt if tracheal tube could be passed without any resistance through the ILMA. If resistance was encountered, twisting of the tracheal tube was carried out to align the bevel and this was considered second attempt. If still intubation was not successful, up-and-down movement of the tracheal tube was tried and this was considered as third attempt. Following successful tracheal intubation, the ILMA was removed using the standard technique and the stabilizing rod. When intubation was unsuccessful after three attempts, the procedure was abandoned and tracheal intubation was performed under direct laryngoscopy.
Any critical incident such as accidental extubation or tube displacement, bronchospasm, SaO2 <90% during the procedure were recorded. The incidence of trauma in successfully intubated patients as evidenced by blood on the tracheal tube after removal was noted. The post-intubation sore throat was assessed on the next day by verbal analog scale (0-10) and scale >3 was considered as positive.
Statistical analysis
Data were analyzed with SPSS Version 10 (SPSS Inc., Chicago, IL). Demographic data and the time taken for tracheal intubation were presented as mean ± SD and analyzed using student t-test. Chi-square analysis was used for comparing nominal data. P ≤ 0.05 was considered statistically significant. A sample size was determined through power analysis (α =0.05, β =0.08) to detect a difference in the overall success rate between two groups, which indicated sample size of 30 patients in each group.
RESULTS
Demographic data were comparable in both groups [Table 1]. Placement of the ILMA was successful in all patients and there were no immediate adverse events. In 3 of 60 patients, blind tracheal intubation was not successful after three attempts; hence, the tracheal tube was placed under direct laryngoscopy. These patients were excluded from further analysis.
Table 1.
Demographic data
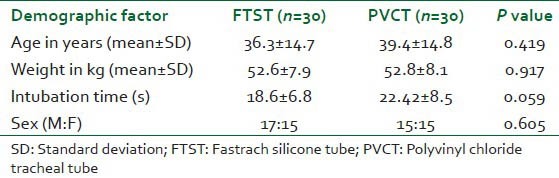
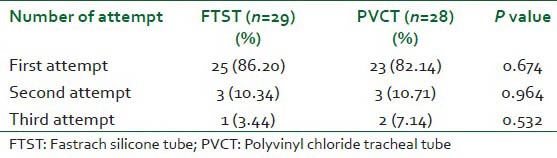
Blind tracheal intubation through the ILMA was successful in (29/30) 96.63% in FTST group compared with (28/30) 93.33% in PVCT group. Ease of insertion as judged by the time taken for intubation was 18.6 ± 6.8 s. in FTST group and 22.42 ± 8.5 s. in PVCT group (P > 0.05). Table 2 shows the number of attempts required in both groups for successful intubation.
Table 2.
No. of attempts
All patients were adequately ventilated and oxygenated throughout the intubation process.
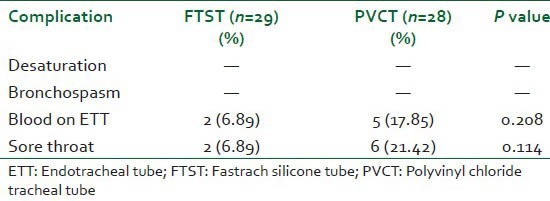
Incidence of blood on tracheal tube and post-intubation sore throat was higher in PVCT group compared to FTST group, but not statistically significant [Table 3].
Table 3.
Complication rate
DISCUSSION
A specially designed silicone wire-reinforced tracheal tube is recommended for insertion through ILMA as it is designed to follow the curvature of the shaft of the ILMA. The reported success rate of FTST passed blindly through ILMA ranges from 89% to 99.3%.[10,11,12,13] This high success rate is attributed to design of FTST, which is a straight, soft wire reinforced tube with a distal inch terminating in a conical Tuohy-like tip. The ILMA directs this flexible tube toward the plane of the glottis without distortion of the anatomy. The conventional PVCT because of its stiffness, lateral opening bevel and curvature show varying success rate when passed blindly through the ILMA. Kundra et al.[14] demonstrated overall success rate of 96% and first-attempt success rate of 86% with both FTST as well as PVCT, which is comparable with our study. Kanazi et al.[15] reported 90% overall success rate with FTST compared with 57% with PVCT. This lower success rate was attributed to the impingement of the tip of the ETT on the tubercle of the epiglottis. Lu et al.[16] reported a 96.7% success rate (75% on the first attempt), with a Sheridan PolyvinylChloride tube, whereas Kapila et al.[7] achieved a 93% success rate (72% on the first attempt) with a Portex PVC tube. Our success rate on the first attempt is higher with PVCT compared to previous investigators. Softening of the tube by prewarming to 40°C might have contributed to higher success rate.
Apart from prewarming, inappropriate positioning of the ILMA in relation to the glottis can result in an increase in the number of attempts and higher failure rate. In a study by Lu et al.,[16] the inability to obtain an optimal ILMA position was responsible for failure in 54.5% of patients. In our study, before tracheal intubation was attempted, good mask — larynx relationship was confirmed by chest inflation, auscultation of breath sounds, a square-wave capnography and no oropharyngeal leak with peak airway pressures ≥20 cm H2O. This might have resulted in higher success rate compared to other investigators.
Another principal factor that determines the success of tracheal intubation through ILMA is the angle at which tube emerges from the distal aperture of the ILMA. The PVC tube is curved and it retains the additional curvature imposed by its passage through the metal shaft of the ILMA.[17] As a result, the tip of the tube may push against the anterior portion of the glottis, which can cause an increased incidence of failed intubation. On measuring the angle of emergence of the tracheal tubes in our study, the FTST formed an angle of 40° to the plane of the ILMA [Figure 1], whereas angle of emergence of the PVCT was 50° [Figure 2]. This may explain the slightly lower success rate with PVCT. Insertion of conventional ETT with reverse orientation has been shown to increase the first time success rate by decreasing the angle of emergence compared to normal orientation.[16,18,19]
Figure 1.

Angle of emergence of Fastrach silicone tube to the plane of intubating laryngeal mask airway
Figure 2.

Angle of emergence of polyvinyl chloride tracheal tube to the plane of intubating laryngeal mask airway
The reported incidence of sore throat and hoarseness following standard LMA insertion are approximately 28.8% and 11%.[20] In our study, the incidence of sore throat was 21.42% in PVCT group, which was higher than FTST group (6.89%). All patients who had a blood tinged ETT developed a sore throat. We attribute it to the stiffness and the steep curvature of PVCT pushing the tip of the tube against the anterior portion of the glottis causing trauma. Joo et al. examined the maximal in vitro forces and pressures exerted by the tip of various tracheal tubes as they exit the ILMA. They found that the PVC ETT exerted 7-10 times higher forces and pressures than the silicone and armored ETTs.[21] Softening of the PVC tube by prewarming and avoiding force during the tracheal intubation are likely to decrease the incidence of trauma. However, it must be remembered that the softness of the PVC tube warmed to 40° is preserved only over a brief period of 40 s. All tracheal intubations were accomplished within this time in our study. Another important precaution to prevent airway trauma is to avoid excessive force while passing PVC tube through ILMA.
There are several limitations of our study. Patient population included in this study consisted of patients with normal airways, which might not apply to patients with difficult airways. Other possible limitations are lack of blinding and ascertaining good ILMA — larynx relationship clinically. Use of a fiberoptic bronchoscope during the intubation attempts may pinpoint the exact reason for failure and increased number of attempts.
In conclusion, our study showed that blind tracheal intubation through an ILMA with PVC tube is a feasible alternative to silicone wire-reinforced tube in patients with normal airways. However, further studies are needed to assess its feasibility in patients with difficult airway.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Caplan RA, Posner KL, Ward RJ, Cheney FW. Adverse respiratory events in anesthesia: A closed claims analysis. Anesthesiology. 1990;72:828–33. doi: 10.1097/00000542-199005000-00010. [DOI] [PubMed] [Google Scholar]
- 2.Brain AI. Three cases of difficult intubation overcome by the laryngeal mask airway. Anesthesia. 1985;40:353–5. doi: 10.1111/j.1365-2044.1985.tb10788.x. [DOI] [PubMed] [Google Scholar]
- 3.Joo H, Rose K. Fastrach – A new intubating laryngeal mask airway: Successful use in patients with difficult airways. Can J Anaesth. 1998;45:253–6. doi: 10.1007/BF03012911. [DOI] [PubMed] [Google Scholar]
- 4.Shung J, Avidan MS, Ing R, Klein DC, Pott L. Awake intubation of the difficult airway with the intubating laryngeal mask airway. Anesthesia. 1998;53:645–9. doi: 10.1046/j.1365-2044.1998.429-az0533.x. [DOI] [PubMed] [Google Scholar]
- 5.Parr MJ, Gregory M, Baskett PJ. The intubating laryngeal mask. Use in failed and difficult intubation. Anesthesia. 1998;53:343–8. doi: 10.1046/j.1365-2044.1998.00319.x. [DOI] [PubMed] [Google Scholar]
- 6.Fukutome T, Amaha K, Nakazawa K, Kawamura T, Noguchi H. Tracheal intubation through the intubating laryngeal mask airway (LMA-Fastrach) in patients with difficult airways. Anaesth Intensive Care. 1998;26:387–91. doi: 10.1177/0310057X9802600408. [DOI] [PubMed] [Google Scholar]
- 7.Kapila A, Addy EV, Verghese C, Brain AI. The intubating laryngeal mask airway: An initial assessment of performance. Br J Anaesth. 1997;79:710–3. doi: 10.1093/bja/79.6.710. [DOI] [PubMed] [Google Scholar]
- 8.Cros AM, Colombani S. Preliminary study of intubation with a new laryngeal mask for difficult intubation. Anesthesiology. 1997;87:482. [Google Scholar]
- 9.Asai T, Shingu K. Tracheal intubation through the intubating laryngeal mask in patients with unstable necks. Acta Anaesthesiol Scand. 2001;45:818–22. doi: 10.1034/j.1399-6576.2001.045007818.x. [DOI] [PubMed] [Google Scholar]
- 10.Pandit JJ, MacLachlan K, Dravid RM, Popat MT. Comparison of times to achieve tracheal intubation with three techniques using the laryngeal or intubating laryngeal mask airway. Anesthesia. 2002;57:128–32. doi: 10.1046/j.0003-2409.2001.02401.x. [DOI] [PubMed] [Google Scholar]
- 11.Brain AI, Verghese C, Addy EV, Kapila A, Brimacombe J. The intubating laryngeal mask. II: A preliminary clinical report of a new means of intubating the trachea. Br J Anaesth. 1997;79:704–9. doi: 10.1093/bja/79.6.704. [DOI] [PubMed] [Google Scholar]
- 12.Avidan MS, Harvey A, Chitkara N, Ponte J. The intubating laryngeal mask airway compared with direct laryngoscopy. Br J Anaesth. 1999;83:615–7. doi: 10.1093/bja/83.4.615. [DOI] [PubMed] [Google Scholar]
- 13.Kihara S, Watanabe S, Taguchi N, Suga A, Brimacombe JR. A comparison of blind and lightwand-guided tracheal intubation through the intubating laryngeal mask. Anesthesia. 2000;55:427–31. doi: 10.1046/j.1365-2044.2000.01324.x. [DOI] [PubMed] [Google Scholar]
- 14.Kundra P, Sujata N, Ravishankar M. Conventional tracheal tubes for intubation through the intubating laryngeal mask airway. Anesth Analg. 2005;100:284–8. doi: 10.1213/01.ANE.0000139348.00435.33. [DOI] [PubMed] [Google Scholar]
- 15.Kanazi GE, El-Khatib M, Nasr VG, Kaddoum R, Al-Alami A, Baraka AS, et al. A comparison of a silicone wire-reinforced tube with the parker and polyvinyl chloride tubes for tracheal intubation through an intubating laryngeal mask airway in patients with normal airways undergoing general anesthesia. Anesth Analg. 2008;107:994–7. doi: 10.1213/ane.0b013e31817ef110. [DOI] [PubMed] [Google Scholar]
- 16.Lu PP, Yang CH, Ho AC, Shyr MH. The intubating LMA: A comparison of insertion techniques with conventional tracheal tubes. Can J Anaesth. 2000;47:849–53. doi: 10.1007/BF03019663. [DOI] [PubMed] [Google Scholar]
- 17.Brain AI, Verghese C, Addy EV, Kapila A. The intubating laryngeal mask. I: Development of a new device for intubation of the trachea. Br J Anaesth. 1997;79:699–703. doi: 10.1093/bja/79.6.699. [DOI] [PubMed] [Google Scholar]
- 18.Joo HS, Rose DK. The intubating laryngeal mask airway with and without fiberoptic guidance. Anesth Analg. 1999;88:662–6. doi: 10.1097/00000539-199903000-00036. [DOI] [PubMed] [Google Scholar]
- 19.Ye L, Liu J, Wong DT, Zhu T. Effects of tracheal tube orientation on the success of intubation through an intubating laryngeal mask airway: Study in Mallampati class 3 or 4 patients. Br J Anaesth. 2009;102:269–72. doi: 10.1093/bja/aen365. [DOI] [PubMed] [Google Scholar]
- 20.Figueredo E, Vivar-Diago M, Muñoz-Blanco F. Laryngo-pharyngeal complaints after use of the laryngeal mask airway. Can J Anaesth. 1999;46:220–5. doi: 10.1007/BF03012599. [DOI] [PubMed] [Google Scholar]
- 21.Joo HS, Kataoka MT, Chen RJ, Doyle J, Mazer CD. PVC tracheal tubes exert forces and pressures seven to ten times higher than silicone or armoured tracheal tubes – An in vitro study. Can J Anaesth. 2002;49:986–9. doi: 10.1007/BF03016888. [DOI] [PubMed] [Google Scholar]


