Abstract
Objective:
One of the major complications of cardiac surgery is the presence of post-operative bleeding. The aim of the present study was to investigate the topical application of tranexamic acid in the pericardial cavity on post-operative bleeding in off-pump coronary artery bypass graft (CABG) surgery.
Materials and Methods:
This study was on 71 patients who underwent off-pump CABG. The anesthesia and surgery methods were the same for all patients. Patients were assigned to two equal groups. In the first group, 1 g of tranexamic acid in 100 mL of normal saline solution (NSS) was applied to pericardium and mediastinal cavity at the end of surgery. In the second group, only 100 mL of NSS was applied. Chest drainage of the patients after 24 h and the amounts of blood and blood products transfusion were also recorded during this time.
Results:
Patients were the same regarding demographic information and surgery. The average volume of blood loss after 24 h was 366 mL for the first group and 788 mL for the control group. There was a statistically significant difference between the two groups (P < 0.001). The amount of packed red blood cells transfusion in the first group was less than that of the control group, which was not statistically significant. There was no statistically significant difference between the amount of hemoglobin, hematocrit, platelets, prothrombin time and partial thromboplastin time in the post-operative stage in the two groups.
Conclusion:
The topical application of tranexamic acid in off-pump CABG patients leads to a decreased post-operative blood loss.
Keywords: Blood, coronary artery bypass graft, off-pump, topical application, tranexamic acid
INTRODUCTION
Post-operative hemorrhage is considered as one of the major concerns in cardiovascular surgery,[1] which may lead to not only an increased need for blood transfusion and its products, but also lengthening of hospital stay. One of the main causes of this blood loss is fibrinolysis. Many fibrinolytic drugs have been used to decrease the post-operative blood loss of coronary artery bypass graft (CABG) surgery including ε-aminocaproic acid, aprotinin and tranexamic acid.[2] Tranexamic acid is a synthetic antifibrinolytic drug, which controls fibrinolysis through blocking of attachment of plasminogen to fibrin.[3] It is used both systemically and topically. The systemic application of tranexamic acid in CABG surgery may exposes the patient to the risk of thrombo embolic complications and consequently, the early occlusion of coronary grafts.[2] Today, there has been a greater tendency to the use of CABG without cardiopulmonary bypass (CPB) to reduce the complications of the application of CPB. Despite the lack of application of CPB during the off-pump CABG surgery, there is blood loss due to the activation of the fibrinolytic pathway that induced by factors such as sternotomy, pericardiotomy, excision of venal and arterial grafts and other factors such as residual heparin, platelet dysfunction and surgical bleeding.[4] This off-pump population is specifically at greater risk for thrombosis in early post-operative period than on-pump patients because CPB induce a degree of hypocoagulability that protects patients from thrombosis in the early post-operative period. To avoid the complications of the use of systemic antifibrinolytic drugs, their topical application can be considered to prevent further incidence of these complications.[5] It has been demonstrated that the topical application of the antifibrinolytic drugs leads to a decreased serum level compared with their intravenous administration. Thus, some studies have investigated the effects of the topical application of these drugs in gynecological, dental, ear-nose-throat and cardiovascular surgery.[6,7,8,9] The goal of the present study was to investigate the topical application of tranexamic acid in the pericardial cavity on post-operative blood loss in off-pump CABG.
MATERIALS AND METHODS
Having obtained the approval of the Committee of Ethics at the Cardiovascular Research Center at Yazd Shahid Sadoughi University of Medical Sciences, this prospective double-blind clinical trial study was conducted on 71 patients underwent the 1st time elective off-pump CABG from September to March 2011 in Yazd Afshr Hospital. The subject exclusion criteria included clotting disorders, kidney failure (Cr> 1.7), allergy to tranexamic acid, consumption of antiplatelet drugs, prescription of heparin 48 h prior to surgery and patients with ejection fraction (EF) <40. The demographic information as age, sex, weight and EF and graft numbers was recorded in the questionnaire. After obtaining the informed written consent, the patients were assigned to two groups using the random numbers table. In the first group (tranexamic acid group), 1 g of tranexamic acid in 100 mL of normal saline solution (NSS) was applied to the pericardium and mediastinal cavity at the end of surgery. In the second group (30 control groups), only 100 mL of NSS was applied as placebo. Both solutions were prepared by one individual in two syringes of the same form and size. The surgeon, scrub nurse and anesthesiologist were blind in this regard. The solution was applied to pericardium, mediastinal cavity and mediastinal ridge at the end of surgery before the surgeon closed the sternum while the chest tubes were clamped. Patient's drains were opened after the complete closure of the sternum. The anesthesia method was the same for all patients. Patient's premedication included morphine 0.1 mg/kg and promethazine 0.5 g/kg administered intramuscularly 30 min before the operation. The induction of anesthesia was performed by sodium thiopental 3-5 mg/kg, fentanyl 2-5 μg/kg and pancoronium bromide 0.1 mg/kg and maintenance of anesthesia was done by propofol 100 μg/kg/h. All patients received heparin 150 IU/kg after separating the internal mammary artery. The patient's Activated Clotting Time (ACT) was measured the target of which was greater than 300 s. At the end of surgery, heparin was neutralized by protamine sulphate and the ACT target was at 150-180 s. Patient's hemoglobin (Hb), hematocrit (HCT), platelet counts, international normalized ratio, prothrombin time (PT) and partial thromboplastin time (PTT) were checked pre-operatively and 24 h after the operation. After transporting the patients to the intensive care unit, their chest tube drainages were measured hourly and their 24 h blood loss was recorded. Blood transfusion criteria were the same for all patients. In the case of HCT <24% and Hb <8 mg/dL, blood transfusion was done in the form of packed red cells. The criterion for fresh frozen plasma (FFP) prescription was a PT, which was 1.5 times greater than the basic rate accompanied by disseminated bleeding and the criterion for platelet prescription was disseminated bleeding and a platelet count <50,000/mm3.
A repeated surgery was performed to control blood loss when the drainage of the chest tubes was more than 300 mL during 2 h while observing simultaneously the patient's correct clotting tests. Patient's demographic information, graft numbers, the use of the left internal mammary artery, duration of procedure and the incidence of repeated surgery to control bleeding were recorded for all patients. Patients were examined to find any deep veins thrombosis (DVT), renal failure and cerebrovascular accident (CVA). The amount of blood products including packed red blood cells (RBCs), FFP and platelets were recorded for each group. The data were collected, controlled and written in the SPSS 16. The required tables, indices and coefficients were prepared. To analyze the quantitative independent and dependent variables, t-test and paired t-test were used, respectively. To determine the correlation between qualitative variables, Chi-square and Fisher exact test were used.
RESULTS
A total of 71 patients qualified to undergo the off-pump CABG surgery in the experimental and control groups (35 subjects in the experimental and 36 in the control group). The sample included 53 males (74.6%) and 18 females (25.4%). The mean age of the sample was 60.56 ± 10.96 with an age range of 40-89. The mean body mass index was not statistically significant in the two groups (P = 0.888). The mean of EF was 46.3 ± 10.2 in the experimental group and 47.48 ± 9.6 in the control group. The mean of graft numbers in the sample was 2.36 ± 0.57 with a range of 1-3 and the two groups were not significantly different with a P value of 0.480. Blood loss volume from the chest tube via 24 h post-operative drainage after the elective procedure of off-pump CABG graft in the two experimental and control groups was studied. The results are presented in Table 1.
Table 1.
Mean volume of diurnal blood loss in the experimental and control groups
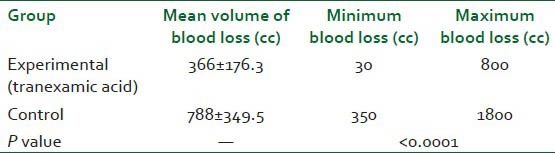
The difference of blood loss volume was significant in the two groups (P < 0.0001). Regarding the rate of packed RBCs transfusion, the average need for transfusion was less in the tranexamic acid compared with the control subjects. The difference was tested using t-test with the assumption of the inequality of the variances. The mean of Hb, HCT and platelets of two groups before and after CABG is presented in Table 2.
Table 2.
The mean of Hb platelet level of the two groups before and after CABG
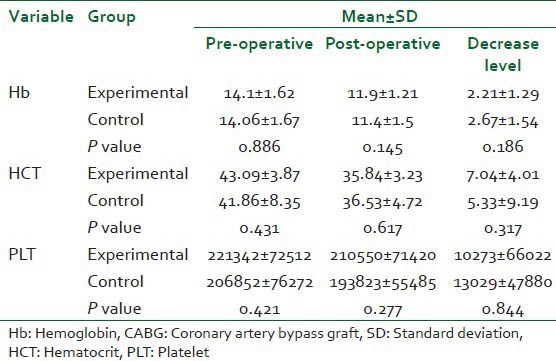
There was no statistically significant difference between the two groups regarding PT, PTT and platelets count before the CABG surgery. Furthermore, there was no significant difference between the two groups regarding PT and PTT, post-operatively. Patients were examined for complications as DVT, renal failure and CVA and there was no report of them. No patients need to surgery for control of bleeding.
DISCUSSION
The results of the study revealed that the mean volume of blood loss in the experimental group who received topical tranexamic acid was 366 mL during the first 24 h after the procedure. This amount was more than twice for the control group who lost 788 mL of blood, which was statistically significant (P < 0.0001). This means that the topical application of tranexamic acid decreased the post-operative blood loss after off-pump CABG. The mean of the need for packed RBCs transfusion is smaller in the experimental patients, but there was no statistically significant difference between the two groups (P = 0.054). Furthermore, the same was true for clotting factors tests of PT and PTT. There were no cases of renal failure, CVA and DVT in any of the groups. The study by Fawzy et al. investigated the effect of application of tranexamic acid on the mediastinal cavity decreasing blood loss after the on-pump CABG procedure. A total of 36 patients participated in the study. The tranexamic acid group received 1 g of tranexamic acid and the control subjects received 100 mL of NSS. The findings of this study showed that the mean of blood loss during the first 24 h after the surgery was 626 mL in the tranexamic acid and 1040 mL in the control groups. Hence, the amount of blood loss in the experimental group was less than the controls and was significantly different. Further, the difference in the amount of the need for blood transfusion was not statistically significant in the two groups. Yet, the rate of platelet infusion in the experimental group was less than that of the control group. Ultimately, Fawzy et al. concluded that the topical application of tranexamic acid for the patients undergoing CABG surgery induced a decrease in post-operative blood loss without imposing extra risks on the patients.[2] These findings are consistent with those of our study.
In addition, in Fawzy's et al. study, the amount of platelet infusion in the experimental group was less than that in the control group. Yet, our two groups were not significantly different regarding platelet counts and no group needed platelet infusion. The cause of blood loss decrease in the tranexamic acid group was the bonding of tranexamic acid to the points of attachment of the lysine present on plasminogen. The occupation of these loci by tranexamic acid leads to the displacement of plasminogen from the fibrin surface and ultimately controlling of fibrinolysis. In our study, there was no significant difference between the two groups regarding the decrease in Hb and hematocrit value postoperatively. This might be due to greater transfusion of blood by the control group.
The study by Abul-azm and Abdullah 2006 evaluated the effect of topical application of tranexamic acid to the mediastinal cavity on post-operative blood loss in patients undergoing open heart surgery. The researcher assigned 100 candidates of elective open heart surgery to two groups. The experimental group received 2 g of tranexamic acid and the control group received just NSS. The findings showed that blood loss in the experimental group was less than control groups, which was statistically significant.[9] These findings are consistent with those of our study. The rate of blood transfusion in the tranexamic acid was less than that in the control group. This is not consistent with our finding. The above-mentioned study used 2 g of tranexamic acid while we used 1 g, yet, the results are not much different. The bypass of coronary artery in Abul-azm and Abdullah study was with CPB in which the rate of blood loss and transfusion was greater compared with the off-pump CABG surgery.[9] The average amount of blood transfusion by both groups was less in our study compared with the above-said research. In this study, eight cases of reoperation surgery for the control of bleeding were observed while in our study, no case was reported. This can be due to the lack of the use of cardiopulmonary pump in off-pump CABG in which the inflammatory system and complement are less affected by the procedure, this being one advantage for the off-pump procedure. Of course, the fibrinolysis system is moderately activated by factors as cardiac manipulation, sternotomy and pericardiotomy.
Another study conducted in 2010 tried to investigate the effect of topical tranexamic acid with 1.5 and 3 g doses on decreasing the post-operative blood loss after total arthroplasty of the knee joint. The researchers concluded that the topical application of tranexamic acid on the site of surgery decreased blood loss by 20-30%. In addition, there were no significant differences among the groups under study regarding the emergence of complications as deep vein thrombosis and pulmonary embolism. Furthermore, the serum level of tranexamic acid was measured in this study showing its low systemic absorption.[10] This study is consistent with ours regarding the lack of drug complications between the two groups. Further, the findings of this study indicate no insignificant systemic absorption of drug in its topical application.
Baric et al. investigated the application of antifibrinolytic drugs on decreasing the post-operative bleeding after cardiac surgery in a clinical trial.[5] In this study, 300 adult cardiac patients who underwent cardiac surgery were divided into three groups. In the first group aprotinin, in the second group tranexamic acid and in the third group (control group) NSS was used. The findings demonstrated a decrease in post-operative blood loss as a result of the topical application of aprotinin and tranexamic acid. Furthermore, the rate of blood loss in the aprotinin group was the least among groups, but it was not significantly different from the tranexamic acid. This study showed that the most amount of effect of tranexamic acid and aprotinin was during the first 12 h after the surgery, which is due to the 3-4 h half-life of the antifibrinolytic drugs. Further, the application of tranexamic acid is economically more cost-effective than aprotinin. Another finding of this study was the lack of significant differences among the three groups with respect to blood transfusion. In our study, too, the need for blood transfusion was not significantly different among the two groups, though it was less in the tranexamic acid. The possible reason may be the flexibility of blood transfusion criteria.
The study by Kurt 2011 aimed at evaluating the effects of topical and systemic application of tranexamic acid and aprotinin on the rate of patient's blood loss after the on-pump CABG procedure. A total of 100 patients were divided in to five groups. In the first group, topical tranexamic acid was sprayed to the pericardial cavity. In the second group, tranexamic acid was injected systemically. In the third group, aprotinin was applied topically. In the fourth group, aprotinin was applied systemically and the fifth group, functioned as the control group. The findings demonstrated that the rate of blood loss was less in the groups that received tranexamic acid and aprotinin compared to the controls. This study suggests the topical application of antifibrinolytic drugs to the mediastinal cavity has no systemic complication. There were no specific complications observed here.[11] The findings of this study are consistent with our findings on lack of complications in patients who used topical antifibrinolytic drugs.
CONCLUSION
Based on the findings of this study, it can be said that the topical application of tranexamic acid leads to a decrease in blood loss after off-pump CABG procedure during the first 24 h after surgery. Furthermore, the need for blood transfusion in the form of packed RBCs was not different in two groups. Finally, the topical application of tranexamic acid would not lead to an increase in complications as CVA, renal failure and DVT.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Ozal E, Kuralay E, Bingöl H, Cingöz F, Ceylan S, Tatar H. Does tranexamic acid reduce desmopressin-induced hyperfibrinolysis? J Thorac Cardiovasc Surg. 2002;123:539–43. doi: 10.1067/mtc.2002.117281. [DOI] [PubMed] [Google Scholar]
- 2.Fawzy H, Elmistekawy E, Bonneau D, Latter D, Errett L. Can local application of Tranexamic acid reduce post-coronary bypass surgery blood loss. A randomized controlled trial? J Cardiothorac Surg. 2009;4:25. doi: 10.1186/1749-8090-4-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Adler Ma SC, Brindle W, Burton G, Gallacher S, Hong FC, Manelius I, et al. Tranexamic acid is associated with less blood transfusion in off-pump coronary artery bypass graft surgery: A systematic review and meta-analysis. J Cardiothorac Vasc Anesth. 2011;25:26–35. doi: 10.1053/j.jvca.2010.08.012. [DOI] [PubMed] [Google Scholar]
- 4.Wang G, Xie G, Jiang T, Wang Y, Wang W, Ji H, et al. Tranexamic acid reduces blood loss after off-pump coronary surgery: A prospective, randomized, double-blind, placebo-controlled study. Anesth Analg. 2012;115:239–43. doi: 10.1213/ANE.0b013e3182264a11. [DOI] [PubMed] [Google Scholar]
- 5.Baric D, Biocina B, Unic D, Sutlic Z, Rudez I, Vrca VB, et al. Topical use of antifibrinolytic agents reduces postoperative bleeding: A double-blind, prospective, randomized study. Eur J Cardiothorac Surg. 2007;31:366–71. doi: 10.1016/j.ejcts.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 6.Sarris I, Arafa A, Konaris L, Kadir RA. Topical use of tranexamic acid to control perioperative local bleeding in gynaecology patients with clotting disorders: Two cases. Haemophilia. 2007;13:115–6. doi: 10.1111/j.1365-2516.2006.01386.x. [DOI] [PubMed] [Google Scholar]
- 7.Carter G, Goss A. Tranexamic acid mouthwash -A prospective randomized study of a 2-day regimen vs 5-day regimen to prevent postoperative bleeding in anticoagulated patients requiring dental extractions. Int J Oral Maxillofac Surg. 2003;32:504–7. [PubMed] [Google Scholar]
- 8.Athanasiadis T, Beule AG, Wormald PJ. Effects of topical antifibrinolytics in endoscopic sinus surgery: A pilot randomized controlled trial. Am J Rhinol. 2007;21:737–42. doi: 10.2500/ajr.2007.21.3097. [DOI] [PubMed] [Google Scholar]
- 9.Abul-Azm A, Abdullah KM. Effect of topical tranexamic acid in open heart surgery. Eur J Anaesthesiol. 2006;23:380–4. doi: 10.1017/S0265021505001894. [DOI] [PubMed] [Google Scholar]
- 10.Wong J, Abrishami A, El Beheiry H, Mahomed NN, Roderick Davey J, Gandhi R, et al. Topical application of tranexamic acid reduces postoperative blood loss in total knee arthroplasty: A randomized, controlled trial. J Bone Joint Surg Am. 2010;92:2503–13. doi: 10.2106/JBJS.I.01518. [DOI] [PubMed] [Google Scholar]
- 11.Kurt T. Evaluation of the effects of systematic or topical use of tranexamic acid and aprotinin on the blood loss and the used amount of blood products following cardiopulmonary bypass surgery. AJCI. 2011;5:116–21. [Google Scholar]


