Abstract
We attempted to evaluate the history of sentinel node navigation surgery (SNNS), technical aspects, tracers, and clinical applications of SNNS using Infrared Ray Electronic Endoscopes (IREE) combined with Indocyanine Green (ICG). The sentinel lymph node (SLN) is defined as a first lymph node (LN) which receives cancer cells from a primary tumor. Reports on clinical application of SNNS for gastric cancers started to appear since early 2000s. Two prospective multicenter trials of SNNS for gastric cancer have also been accomplished in Japan. Kitagawa et al reported that the endoscopic dual (dye and radioisotope) tracer method for SN biopsy was confirmed acceptable and effective when applied to the early-stage gastric cancer (EGC). We have previously reported the usefulness of SNNS in gastrointestinal cancer using ICG as a tracer, combined with IREE (Olympus Optical, Tokyo, Japan) to detect SLN. LN metastasis rate of EGC is low. Hence, clinical application of SNNS for EGC might lead us to avoid unnecessary LN dissection, which could preserve the patient’s quality of life after operation. The most ideal method of SNNS should allow secure and accurate detection of SLN, and real time observation of lymphatic flow during operation.
Keywords: Gastric cancer, Sentinel node navigation surgery, Infrared Ray Electronic Endoscopes, Indocyanine Green
Core tip: Two prospective multicenter trials of sentinel node navigation surgery (SNNS) for gastric cancer have been accomplished in Japan. Kitagawa et al reported that the endoscopic dual (dye and radioisotope) tracer method for SN biopsy was confirmed acceptable and effective when applied to the early-stage gastric cancer. The ideal method of SNNS should allow secure and accurate detection of sentinel lymph nodes, and real time observation of lymphatic flow during operation. In this review, we attempted to comprehensively evaluate the history, technical aspects, tracers, and clinical applications of SNNS with a special emphasis on the use of Infrared Ray Electronic Endoscopes with Indocyanine Green.
INTRODUCTION
Complete resection of tumor and dissection of regional lymph nodes (LNs) are basic surgical principles for patients with gastric cancer. Gastrectomy with regional LN dissection is the standard procedure for gastric cancer, while less invasive interventions, such as endoscopic submucosal dissection, have emerged as suitable techniques for EGC but not indicated for possible LN metastasis[1].
Laparoscopic gastrectomy was first performed by Kitano et al[2] for EGC in 1991. Since then, the usefulness of laparoscopic surgery is recognized, which is widely carried out for EGC in Japan[3]. While early-phase recovery after surgery has been improved by laparoscopic surgery, preservation of late-phase quality of life (QOL) by function-preserving surgery is also important. Therefore, the SN concept has been a much-discussed topic in standard gastric operations such as distal, proximal and total gastrectomy, which are associated with deterioration of QOL by post-gastrectomy syndrome.
The lymph node metastasis rate of EGC is approximately 15%-20%. Therefore, clinical application of sentinel node navigation surgery (SNNS) for EGC might be able to abrogate unnecessary lymph node dissection as well as to reduce the volume of gastric resection. As a result, the post-gastrectomy syndrome may be reduced.
The sentinel lymph node (SLN) is defined as the first possible site to receive cancer cells along the route of lymphatic drainage from the primary tumor. The SLN concept was first advocated by Morton et al[4] in patients with melanoma. SNNS has already been validated for breast cancer[5] and malignant melanoma, where a limited or no nodal dissection is performed in case of negative SN.
TNM classification has defined “The SLN is the first lymph node to receive lymphatic drainage from a primary tumor.” The absence of metastasis in SLN is believed to correlate with the absence of metastasis in downstream lymph nodes. From the TNM classification Sixth Edition, the presence or absence of metastases in SN is proposed, which is quoted in the 14th Edition of the Rules for gastric cancer in Japan[6].
In this review, we have attempted to evaluate the history of SNNS, technical aspects, tracers for the clinical application of SNNS using Infrared Ray Electronic Endoscopes (IREE) combined with Indocyanine Green (ICG) method for limited lymphadenectomy and modified gastric resection.
CURRENT STATUS OF SNNS FOR GASTRIC CANCER
Reports on clinical application of SNNS for patients with gastric cancers started to be published during early 2000s (Table 1).
Table 1.
Reports on SN mapping for gastric cancer
| Ref. | Year | Journal | n | Detection rate | Sensitivity |
| RI method | |||||
| Kitagawa et al[31] | 2000 | Surg Clin N Am | 36 | 97% | 100% |
| Kitagawa et al[8] | 2002 | Br J Surg | 145 | 95% | 92% |
| Gretschel et al[32] | 2003 | Chirurg | 15 | 93% | 89% |
| Kim MC et al[33] | 2004 | Ann Surg | 46 | 93.50% | 84.60% |
| Uenosono et al[34] | 2005 | Br J Surg | 104 | 95.20% | 81.80% |
| Arigami et al[30] | 2006 | Ann Surg | 61 | 100% | 95.50% |
| Mochiki et al[35] | 2006 | Am J Surg | 59 | 96.60% | 83.30% |
| Yanagita et al[36] | 2008 | Ann Surg Oncol | 160 | 98.80% | 96.70% |
| Mean | 63.2 | 96% | 90% | ||
| Dye method | |||||
| Hiratsuka et al[7] | 2001 | Surgery | 77 | 99% | 90% |
| Ichikura et al[37] | 2002 | World J Surg | 62 | 100% | 85% |
| Carlini et al[38] | 2002 | J Exp Clin Cancer Res | 40 | 100% | 87% |
| Miwa et al[9] | 2003 | Br J Surg | 211 | 96% | 89% |
| Ryu et al[39] | 2003 | Eur J Surg Oncol | 71 | 92% | 100% |
| Song et al[40] | 2004 | Am J Surg | 27 | 96% | 100% |
| Osaka et al[41] | 2004 | Clin Cancer Res | 57 | 100% | 100% |
| Ishizaki et al[42] | 2006 | Eur J Surg Oncol | 62 | 85.70% | 96.40% |
| Park et al[43] | 2006 | Eur J Surg Oncol | 100 | 94.60% | 78.60% |
| Rino et al[44] | 2007 | Hepatogastroenterology | 43 | 93.00% | 81.80% |
| Mean | 70.2 | 96% | 91% | ||
| RI + Dye mthod | |||||
| Hayashi et al[45] | 2003 | J Am Coll Surg | 31 | 100% | 100% |
| Karube et al[46] | 2004 | J Surg Oncol | 41 | 100% | 92% |
| Tonouchi et al[47] | 2005 | World J Surg | 37 | 94.60% | 100% |
| Gretschel et al[48] | 2005 | Eur J Surg Oncol | 34 | 97.10% | 95.40% |
| Ichikura et al[49] | 2006 | Surgery | 80 | 100% | 92.90% |
| Saikawa et al[50] | 2006 | World J Surg | 35 | 94.30% | 50% |
| Dye + IREE method | |||||
| Nimura et al[10] | 2004 | Br J Surg | 84 | 99% | 100% |
| Ohdaira et al[11] | 2007 | Gastric Cancer | 60 | 100% | 100% |
| Kelder et al[12] | 2010 | Eur J Surg Oncol | 212 | 99.50% | 97% |
| Mean | 100% | 99% | |||
| Dye + Fluorcence method | |||||
| Miyashiro et al[22] | 2008 | Ann Surg Oncol | 3 | 100% | 100% |
| Kusano et al[23] | 2008 | Dig Surg | 22 | 90.10% | 40.00% |
| Tajima et al[51] | 2009 | Ann Surg | 56 | 96.40% | 64.70% |
| Mean | 96% | 68% |
Hiratsuka et al[7] had reported that SLN biopsy using ICG can be performed with a high success rate, and the SLN status can predict the LN status with a high degree of accuracy, especially in patients with T1 gastric cancer.
Kitagawa et al[8] evaluated the technical aspects and clinical application of radio-guided surgery using gamma detection probe technology. Endoscopic injection of technetium-99m-radiolabelled tin colloid was performed before the operation, and radioactive SNs were identified with a gamma probe. The benefit of using moderate magnitude radioisotopes is that the radioisotopes remain for an adequate period in the SN after tracer injection, and thus the identification rate of SLN becomes high even in fatty patients.
Miwa et al[9] reported the results of a regional multicenter clinical trial of SN mapping for gastric cancer using the conventional dye-guided method. Although the patient population enrolled in their study was limited, this first multicenter trial of SN mapping for gastric cancer provided several important messages. This study was designed to investigate the feasibility of SN mapping for gastric cancer using the dye-guided method as a simple method that can be conducted even in community hospitals without special equipment.
Miwa proposed the concept of a “sentinel lymphatic basin,” and reported successful mapping of the lymphatic basins in 96.2% of their patients. The dye stained one or more metastatic nodes in 31 patients, but failed to indicate a metastatic node in four patients with a large involved node[9]. This theory can provide an acceptable base for clinical application of SNNS. Their reports have demonstrated that sentinel lymphatic basins contain truly positive nodes, even in cases with a false negative SN biopsy. Therefore, the sentinel lymphatic basins are good targets for focused lymph node dissections in patients with cT1N0 gastric cancer. The distribution of sentinel lymphatic basins and the status of SLN would be useful information to decide the extent of gastric resection.
We have already suggested the clinical usefulness of IREE combined with ICG to detect illuminated SLN in patients with gastric cancer and duodenal tumors as compared with dye alone (Figure 1)[10-15]. The SN identification rate and sensitivity for IREE versus ICG alone were 99.5% vs 85.8% and 97.0% vs 48.4%, respectively[10].
Figure 1.
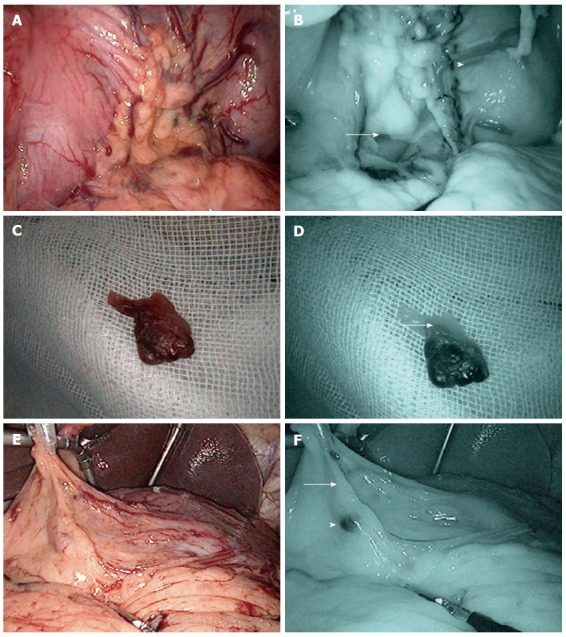
Laparoscopic observation around the left gastric vessels (LN No.3,7). Lymph vessels and LN can be easily detected by IREE with Indocyanine Green (ICG). A: Ordinary light observation of lymph vessels around the left gastric artery; B: Infrared ray observation of lymph vessels around left gastric region (Lymph vessels: arrow; ICG positive node: arrowhead); C: Ordinary light observation of lymph vessels around the right epigastric artery; D: Infrared ray observation around the right epigastric artery shows first drainage lymph vessels, and sentinel lymph node (SLN) (arrow); E: Ordinary light observation of lymph vessels; F: Infrared ray observation of lymph vessels (first drainage lymph vessels: arrow; SLN: arrowhead).
The lymphatic flow of the stomach is complicated and skip metastases were observed even in EGC. We reported that the group 2 LN metastases were judged as SNs in 32%[11]. The most common locations of the SLN were stations left gastric artery in each of the upper-, middle-, and lower-thirds of the stomach[11]. Our SLN procedure with IREE can detect the SLN and is better than ICG alone. The lymphatic basin dissection (LBD) of the SN basin is required for accurate intra-operative diagnosis of lymph node metastases. LBD dissection based on IREE is an acceptable method of nodal dissection in patients with T1 or limited T2 tumors[12-14].
Ryu et al[15] reported a meta-analysis of feasibility studies on SNNS for gastric cancer between 2001 and 2009. The SN identification rate and sensitivity were 97.6% and 87.8%, respectively. Therefore, they advocated that SNB in gastric cancer is probably not clinically applicable for limited lymphadenectomy due to the unsatisfactory sensitivity and heterogeneity among practicing surgeons, and that more than four SLN should be harvested to improve sensitivity. They also advocated that a tumor-specific SNB method should be developed[16].
Can et al[16] investigated a number of reports on SNB for gastric cancer from single institute experiences in order to augment the relevant knowledge base, and demonstrated that the currently established double tracer method (dye and radio-isotope tracers) appeared to be the most efficacious and reliable procedure for identifying true SLN. They commented while conventional dye tracers were still useful, ICG deserves more attention for the current applications. IREE, florescence imaging and near-infrared technology represent the future direction in which the SNNS concept is advancing[17].
Recently, two multicenter prospective studies for SNNS were organized in Japan. The Gastric Cancer Surgical Study Group of the Japan Clinical Oncology Group (JCOG) organized a multicenter prospective study of SN mapping by the dye-guided method using intraoperative subserosal injection of ICG and observation by the naked eye[18]. Another study group was the Japan Society of SNNS, which conducted a multicenter prospective trial of SN mapping by a dual tracer method with blue dye and radioactive colloid[19].
The JCOG study was performed by the dye-guided method using intraoperative subserosal injection of ICG and observed by the naked eye in patients with T1 gastric cancer. Green-stained nodes, representing SLN, were removed first, and then gastrectomy with lymphadenectomy was performed. However, this clinical trial was discontinued because the proportion of false negatives was much higher than expected. Miyashiro et al[17] reported that the JCOG0302 trial revealed the unreliability of frozen section examination using just one plane, and highlighted the impact of the learning curve. Nevertheless, we reported that the SN identification rate and sensitivity of ICG alone with the naked eye were 85.8% and 48.4% respectively, which indicates that detection of SN with dye alone is insufficient[10].
Kitagawa et al[18] conducted a multicenter, single-arm, phase II study of SN mapping that used a standardized dual tracer endoscopic injection technique. Patients with previously untreated cT1 or cT2 gastric adenocarcinomas < 4 cm in gross diameter were eligible for inclusion in this study. SN mapping was performed by using a standardized dual tracer endoscopic injection technique. The SN detection rate was 97.5%. Of 57 patients with lymph node metastasis by conventional hematoxylin and eosin staining, 93% had positive SNs, and the accuracy of nodal evaluation for metastasis was 99%. Only four false-negative SN biopsies were observed, and pathologic analysis revealed that three of those biopsies were pT2 or tumors > 4 cm. They concluded that the endoscopic dual tracer method for SN biopsy is acceptable and effective when applied to superficial, relatively small gastric adenocarcinomas.
TRACERS AND METHODS OF SNNS
At present, two methods are predominantly used in the detection of the SLN, injection of dye and/or injection of a radio-isotope (RI) with a gamma probe. The SLN is stained blue or green by dye and the hot LNs are identified by the uptake of RI, after injection around the tumor with dye or RI colloid.
Usually, 99mTechnetium (99mTc)-tin colloid was endoscopically injected into the submucosa of the gastric wall around the tumor one day before surgery, and lymphoscintigraphy was performed 2 h later. During surgery, the uptake of the RI in each lymph node was counted using Navigator GPS. The half-life of 99mTc is short, it produces secure radioactive elements, and the particle size is relatively large. Therefore, 99mTc is judged to remain in the lymph nodes for approximately 12 h. However, tight regulation and costs of radioactive substances limit the wide-spread use of the probe-guided method in general hospitals.
The dye (Patent blue, lymphazurin, and ICG)-guided method is used in surgery and is safe, convenient, inexpensive and excellent in depiction of not only LNs but also the lymphatic vessels. Particulate-activated carbon and dye have been used to study lymphatic flow previously in Japan[20]. The advantage of these methods is that their transition to the lymphatic system allows intra operative real time evaluation of the lymph flow. Because carbon particles are small and diffuse rapidly to the distal LNs, carbon was judged to be unsuitable for detection of SLN in thick adipose tissue, such as in laparoscopic surgery.
We reported the clinical usefulness of infrared ray IREE combined with ICG to illuminate SLNs in patients with gastric cancer[10-14].
ICG is a tricarbocyanine dye that has been used clinically for over 50 years for hepatic clearance, cardiovascular function testing, and retinal angiography on the basis of its dark green color, which is typically administered at concentrations of 2.5 mg/mL at a typical total dose of 25 mg in adults. ICG conjugates with albumin, which becomes an excellent vascular agent for evaluating both the blood and lymph systems in off-label studies. The incidence of mild adverse reactions of ICG was 0.05% for severe adverse reactions, with no deaths after 1923 procedures[21,22].
It is a known fact that, if combined with plasma protein, ICG has a maximum absorption wavelength of 805 nm. Irradiated with light near the maximum absorption wavelength, the ICG-injected area in the tissue absorbs the light and becomes darker. In the background areas, the light is reflected and those areas become brighter. This is the mechanism of the infrared light absorption observation with ICG (hereinafter referred to as light absorption observation). On the other hand, it is known that ICG which has absorbed the light emits a maximum fluorescence wavelength of 830 nm after it is excited. Compared to the reflected light, the intensity of fluorescence is extremely weak. Thus, infrared fluorescence observation with ICG (herein after referred to as fluorescence observation) is enabled by completely cutting the reflected light and receiving the light near the maximum fluorescence wavelength (Figures 2 and 3).
Figure 2.
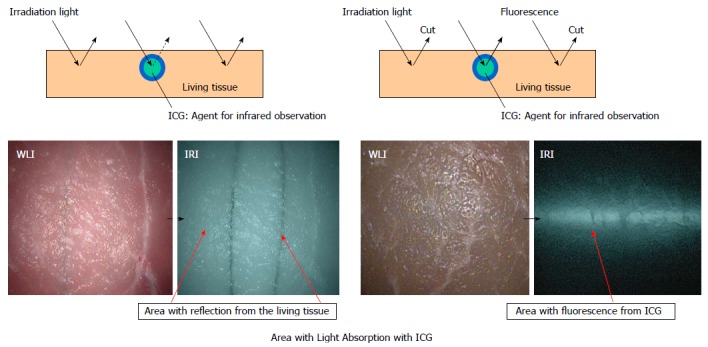
Mechanism of absorption with indocyanine green and fluorescence from indocyanine green. Irradiated with light near the maximum absorption wavelength, the ICG-injected area in the tissue absorbs the light and becomes darker. In the other areas in the background, the light is reflected and those areas become brighter. ICG: Indocyanine Green.
Figure 3.
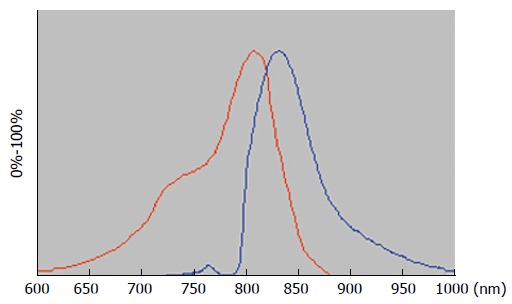
Wavelength of the indocyanine green. Indocyanine green (ICG) has a maximum 805 nm of absorption wavelength. Absorption wavelength band of ICG: Red line; Fluorescence wavelength band of ICG: Blue line.
Utilizing this principle of ICG, the light absorption observation became possible in the conventional infrared endoscope system. The light from the xenon lamp in the light source unit becomes light near the maximum 805 nm of absorption wavelength after passing through the infrared filter which is switchable with the white light filter. Then the light passes through the light guide and the laparoscope to irradiate the subject. The light reflected from the subject is received by an infrared-sensitive charge-coupled device (CCD) incorporated in the camera head, enabling light absorption observation. One of the characteristics of this system is that switching the observation mode between the light absorption observation and the fluorescence observation is made possible.
Recently, ICG with the use of CCD cameras and light-emitting diodes has emerged as an alternative modality in SLN biopsy. The fluorescence method is revolutionary in that it can be observed through a thick adipose tissue, but this needs to be performed in a dark operating room with light off to observe the fluorescence of the LNs[23,24].
In order to solve this problem, a system that can describe the ICG near-infrared fluorescence image on the color screen of bright field (hyper eye medical system: HEMS, Mizuho Medical Instruments) has been developed[25], and the usefulness of SNNS of fluorescence observation for breast cancer has been reported[26]. However, these two models do not allow insertion through a trocar, and therefore cannot be used in laparoscopic surgery. In this regard, IREE is especially suitable for use in the SNNS in laparoscopic surgery.
SKIP AND MICRO-METASTASIS OF THE LNS
The precise detection of LN metastasis including micro-metastasis is important for SNNS[27]. Kikuchi et al[28] analyzed the topographical pattern of lymph node metastasis for pN1 patients with curative resection. Skip metastasis occurred in 5%, and the common stations for such a metastasis were No. 7 and No. 8a. This pattern of metastasis was found in 14% of the patients with single positive nodes. They noted that although perigastric nodes were important first sites of drainage, the distribution of positive nodes depended on the tumor location. Accordingly, in view of both the complexity of the lymphatic flow and skip metastasis, previous studies have recommended the routine use of systemic D2 dissection. However, the feasibility and reliability of SNNS is a prerequisite to less invasive gastric surgery.
Tokunaga et al[29] reported that lymphatic flow in LGA and in RGEA are main lymphatic drainage routes of the stomach. Skip metastases were observed in 10%, which were observed in the station 7, 8a, 9, or 11p. The lymphatic stream of the stomach is complicated and multidirectional. Understanding and mapping the complex lymphatic streams of the stomach will allow surgeons to perform more effective lymph node dissection during gastric cancer surgery.
Arigami et al[30] reported that the incidence of micrometastasis of SNs detected by RT-PCR was quite high and useful for SNNS. All metastatic lymph nodes were identified within SNs, as judged by RT-PCR. The incidences of metastasis determined by hematoxylin and eosin and IHC were 8.2% and 13.1%, respectively. Micrometastases undetectable by IHC were identified in 23.0% of SNs by RT-PCR.
We have previously reported in patients with lymph node metastasis that positive HE and IHC staining was 12.3% and 23.8%, respectively. Diagnosis of 15 patients without LN metastasis by HE correlated positively with LN metastasis by IHC staining. The 27 positive LNs of these 15 patients consisted of SN which were identified during surgery. Consequently, all these 27 positive LNs judged by IHC staining was micrometastasis or less[13]. Therefore, ICG-positive lymphatic basin dissection by SNNS with infrared ray observation seems to be an adequate method of lymph node dissection for EGC.
When the tumor is located in the lesser curvature, lymphatic fluid is frequently observed to flow from the left gastric artery to the celiac axis area.
OUR METHOD OF SNNS BY IREE
We have reported the clinical usefulness of SNNS for EGC using ICG combined with IREE[10-14].
Briefly, prior to the injection of ICG, the stomach was mobilized by dissecting through the gastrocolic ligament without disrupting the gastro-epiploic vessels. ICG was injected endoscopically in four quadrants of the submucosa surrounding the tumor with an endoscopic puncture needle. Twenty minutes after the injection, SNs stained with ICG were observed with the naked eye as well as IREE. One of the important points regarding ICG injection is that we should not perforate the gastric wall by the needle, for which steady careful injection of ICG into the submucosa is important. It is usually difficult to observe lymphatic flow and the SN if ICG is leaking outside the stomach wall. We usually observe lymphatic flow and SN around the greater and lesser curvature at first, and then the left and right gastric artery and vein by IREE with normal light and the infrared light.
With the rigid endoscope, systems have been developed and we can change normal light and infrared light by a hand switch (Figure 4). Each system has absorption and fluorescence scopes, which can be used in laparoscopic surgery. After careful observation, we make marks around the lymphatic flow area by clips and perform LBD. The portion of the stomach removed depends on the result of intraoperative pathological examination of frozen HE staining and the number of lines of lymphatic flow. If SLN is negative for metastasis and lymphatic flow is single line, we perform a wedge resection. When lymphatic flow is recognized in two directions, segmental resection, pylorus preserving gastrectomy or proximal resection is selected. If SLN is positive for metastasis, a standard gastrectomy with D2 dissection is chosen.
Figure 4.
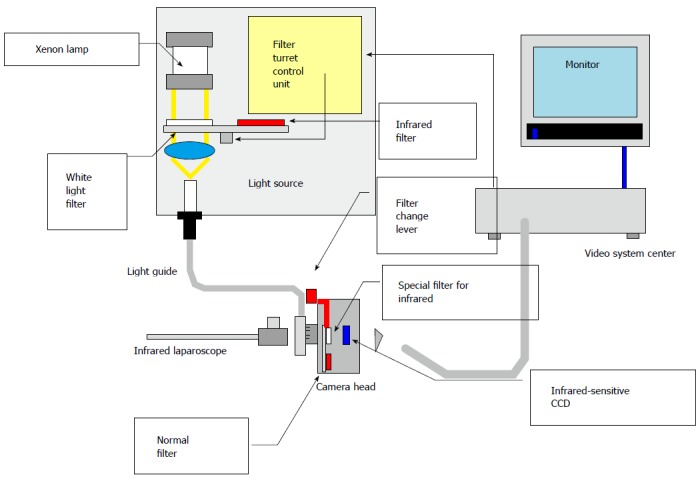
Technological overview of the new infrared observation system ordinary light and infrared ray laparoscopy system can be changed by a handle switch.
We usually take the extra 60-90 min for SNNS compared to standard operation for EGC. So, the surgeon is required to have a passion for SNNS.
CONCLUSION
Of several methods of SNNS, IREE can detect the SN easily and is superior to ICG alone, and seems to have an equal detection rate as compared to the RI + dye method. LBD of the SN basin is required for accurate intra-operative diagnosis of LN metastases. ICG-positive lymphatic basin dissection by SNNS with IREE seems to be an adequate method of lymph node dissection for EGC.
Footnotes
P- Reviewers: Iacono C, Mizuguchi S, Santoro GA S- Editor: Qi Y L- Editor: O’Neill M E- Editor: Zhang DN
References
- 1.Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2010 (ver. 3) Gastric Cancer. 2011;14:113–123. doi: 10.1007/s10120-011-0042-4. [DOI] [PubMed] [Google Scholar]
- 2.Kitano S, Iso Y, Moriyama M, Sugimachi K. Laparoscopy-assisted Billroth I gastrectomy. Surg Laparosc Endosc. 1994;4:146–148. [PubMed] [Google Scholar]
- 3.Shiraishi N, Yasuda K, Kitano S. Laparoscopic gastrectomy with lymph node dissection for gastric cancer. Gastric Cancer. 2006;9:167–176. doi: 10.1007/s10120-006-0380-9. [DOI] [PubMed] [Google Scholar]
- 4.Morton DL, Wen DR, Wong JH, Economou JS, Cagle LA, Storm FK, Foshag LJ, Cochran AJ. Technical details of intraoperative lymphatic mapping for early stage melanoma. Arch Surg. 1992;127:392–399. doi: 10.1001/archsurg.1992.01420040034005. [DOI] [PubMed] [Google Scholar]
- 5.Veronesi U, Paganelli G, Viale G, Luini A, Zurrida S, Galimberti V, Intra M, Veronesi P, Robertson C, Maisonneuve P, et al. A randomized comparison of sentinel-node biopsy with routine axillary dissection in breast cancer. N Engl J Med. 2003;349:546–553. doi: 10.1056/NEJMoa012782. [DOI] [PubMed] [Google Scholar]
- 6.Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma 14th ed. Berlin: Springer; 2010. pp. 11–12. [DOI] [PubMed] [Google Scholar]
- 7.Hiratsuka M, Miyashiro I, Ishikawa O, Furukawa H, Motomura K, Ohigashi H, Kameyama M, Sasaki Y, Kabuto T, Ishiguro S, et al. Application of sentinel node biopsy to gastric cancer surgery. Surgery. 2001;129:335–340. doi: 10.1067/msy.2001.111699. [DOI] [PubMed] [Google Scholar]
- 8.Kitagawa Y, Fujii H, Mukai M, Kubota T, Otani Y, Kitajima M. Radio-guided sentinel node detection for gastric cancer. Br J Surg. 2002;89:604–608. doi: 10.1046/j.1365-2168.2002.02065.x. [DOI] [PubMed] [Google Scholar]
- 9.Miwa K, Kinami S, Taniguchi K, Fushida S, Fujimura T, Nonomura A. Mapping sentinel nodes in patients with early-stage gastric carcinoma. Br J Surg. 2003;90:178–182. doi: 10.1002/bjs.4031. [DOI] [PubMed] [Google Scholar]
- 10.Nimura H, Narimiya N, Mitsumori N, Yamazaki Y, Yanaga K, Urashima M. Infrared ray electronic endoscopy combined with indocyanine green injection for detection of sentinel nodes of patients with gastric cancer. Br J Surg. 2004;91:575–579. doi: 10.1002/bjs.4470. [DOI] [PubMed] [Google Scholar]
- 11.Ohdaira H, Nimura H, Mitsumori N, Takahashi N, Kashiwagi H, Yanaga K. Validity of modified gastrectomy combined with sentinel node navigation surgery for early gastric cancer. Gastric Cancer. 2007;10:117–122. doi: 10.1007/s10120-007-0419-6. [DOI] [PubMed] [Google Scholar]
- 12.Kelder W, Nimura H, Takahashi N, Mitsumori N, van Dam GM, Yanaga K. Sentinel node mapping with indocyanine green (ICG) and infrared ray detection in early gastric cancer: an accurate method that enables a limited lymphadenectomy. Eur J Surg Oncol. 2010;36:552–558. doi: 10.1016/j.ejso.2010.04.007. [DOI] [PubMed] [Google Scholar]
- 13.Yano K, Nimura H, Mitsumori N, Takahashi N, Kashiwagi H, Yanaga K. The efficiency of micrometastasis by sentinel node navigation surgery using indocyanine green and infrared ray laparoscopy system for gastric cancer. Gastric Cancer. 2012;15:287–291. doi: 10.1007/s10120-011-0105-6. [DOI] [PubMed] [Google Scholar]
- 14.Mitsumori N, Nimura H, Takahashi N, Watanabe A, Sasaki T, Kashiwagi H, Yanaga K. Sentinel node navigation surgery for early malignant tumor of the duodenum. Jikeikai Med J. 2009;56:11–17. [Google Scholar]
- 15.Ryu KW, Eom BW, Nam BH, Lee JH, Kook MC, Choi IJ, Kim YW. Is the sentinel node biopsy clinically applicable for limited lymphadenectomy and modified gastric resection in gastric cancer? A meta-analysis of feasibility studies. J Surg Oncol. 2011;104:578–584. doi: 10.1002/jso.21995. [DOI] [PubMed] [Google Scholar]
- 16.Can MF, Yagci G, Cetiner S. Sentinel lymph node biopsy for gastric cancer: Where do we stand? World J Gastrointest Surg. 2011;3:131–137. doi: 10.4240/wjgs.v3.i9.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Miyashiro I, Hiratsuka M, Sasako M, Sano T, Mizusawa J, Nakamura K, Nashimoto A, Tsuburaya A, Fukushima N. High false-negative proportion of intraoperative histological examination as a serious problem for clinical application of sentinel node biopsy for early gastric cancer: final results of the Japan Clinical Oncology Group multicenter trial JCOG0302. Gastric Cancer. 2014;17:316–323. doi: 10.1007/s10120-013-0285-3. [DOI] [PubMed] [Google Scholar]
- 18.Kitagawa Y, Takeuchi H, Takagi Y, Natsugoe S, Terashima M, Murakami N, Fujimura T, Tsujimoto H, Hayashi H, Yoshimizu N, et al. Sentinel node mapping for gastric cancer: a prospective multicenter trial in Japan. J Clin Oncol. 2013;31:3704–3710. doi: 10.1200/JCO.2013.50.3789. [DOI] [PubMed] [Google Scholar]
- 19.Maruyama K, Sasako M, Kinoshita T, Sano T, Katai H. Can sentinel node biopsy indicate rational extent of lymphadenectomy in gastric cancer surgery? Fundamental and new information on lymph-node dissection. Langenbecks Arch Surg. 1999;384:149–157. doi: 10.1007/s004230050185. [DOI] [PubMed] [Google Scholar]
- 20.Polom K, Murawa D, Rho YS, Nowaczyk P, Hünerbein M, Murawa P. Current trends and emerging future of indocyanine green usage in surgery and oncology: a literature review. Cancer. 2011;117:4812–4822. doi: 10.1002/cncr.26087. [DOI] [PubMed] [Google Scholar]
- 21.Alander JT, Kaartinen I, Laakso A, Pätilä T, Spillmann T, Tuchin VV, Venermo M, Välisuo P. A review of indocyanine green fluorescent imaging in surgery. Int J Biomed Imaging. 2012;2012:940585. doi: 10.1155/2012/940585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Miyashiro I, Miyoshi N, Hiratsuka M, Kishi K, Yamada T, Ohue M, Ohigashi H, Yano M, Ishikawa O, Imaoka S. Detection of sentinel node in gastric cancer surgery by indocyanine green fluorescence imaging: comparison with infrared imaging. Ann Surg Oncol. 2008;15:1640–1643. doi: 10.1245/s10434-008-9872-7. [DOI] [PubMed] [Google Scholar]
- 23.Kusano M, Tajima Y, Yamazaki K, Kato M, Watanabe M, Miwa M. Sentinel node mapping guided by indocyanine green fluorescence imaging: a new method for sentinel node navigation surgery in gastrointestinal cancer. Dig Surg. 2008;25:103–108. doi: 10.1159/000121905. [DOI] [PubMed] [Google Scholar]
- 24.Ishizuka M, Nagata H, Takagi K, Iwasaki Y, Kubota K. Fluorescence imaging visualizes three sets of regional lymph nodes in patients with lower rectal cancer. Hepatogastroenterology. 2012;59:1381–1384. doi: 10.5754/hge11281. [DOI] [PubMed] [Google Scholar]
- 25.Nagao T, Hojo T, Kurihara H, Tsuda H, Tanaka-Akashi S, Kinoshita T. Sentinel lymph node biopsy in breast cancer patients with previous breast augmentation surgery. Breast Cancer. 2011:Epub ahead of print. doi: 10.1007/s12282-011-0280-7. [DOI] [PubMed] [Google Scholar]
- 26.Aoyama K, Kamio T, Ohchi T, Nishizawa M, Kameoka S. Sentinel lymph node biopsy for breast cancer patients using fluorescence navigation with indocyanine green. World J Surg Oncol. 2011;9:157. doi: 10.1186/1477-7819-9-157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ajisaka H, Miwa K. Micrometastases in sentinel nodes of gastric cancer. Br J Cancer. 2003;89:676–680. doi: 10.1038/sj.bjc.6601183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kikuchi S, Kurita A, Natsuya K, Sakuramoto S, Kobayashi N, Shimao H, Kakita A. First drainage lymph node(s) in gastric cancer: analysis of the topographical pattern of lymph node metastasis in patients with pN-1 stage tumors. Anticancer Res. 2003;23:601–604. [PubMed] [Google Scholar]
- 29.Tokunaga M, Ohyama S, Hiki N, Fukunaga T, Yamada K, Sano T, Yamaguchi T. Investigation of the lymphatic stream of the stomach in gastric cancer with solitary lymph node metastasis. World J Surg. 2009;33:1235–1239. doi: 10.1007/s00268-009-9985-6. [DOI] [PubMed] [Google Scholar]
- 30.Arigami T, Natsugoe S, Uenosono Y, Mataki Y, Ehi K, Higashi H, Arima H, Yanagida S, Ishigami S, Hokita S, et al. Evaluation of sentinel node concept in gastric cancer based on lymph node micrometastasis determined by reverse transcription-polymerase chain reaction. Ann Surg. 2006;243:341–347. doi: 10.1097/01.sla.0000201453.65534.f1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kitagawa Y, Fujii H, Mukai M, Kubota T, Ando N, Watanabe M, Ohgami M, Otani Y, Ozawa S, Hasegawa H, et al. The role of the sentinel lymph node in gastrointestinal cancer. Surg Clin North Am. 2000;80:1799–1809. doi: 10.1016/s0039-6109(05)70262-0. [DOI] [PubMed] [Google Scholar]
- 32.Gretschel S, Bembenek A, Ulmer Ch, Hünerbein M, Markwardt J, Schneider U, Schlag PM. [Lymphatic mapping and sentinel lymph node biopsy in gastric cancer] Chirurg. 2003;74:132–138. doi: 10.1007/s00104-002-0604-4. [DOI] [PubMed] [Google Scholar]
- 33.Kim MC, Kim HH, Jung GJ, Lee JH, Choi SR, Kang DY, Roh MS, Jeong JS. Lymphatic mapping and sentinel node biopsy using 99mTc tin colloid in gastric cancer. Ann Surg. 2004;239:383–387. doi: 10.1097/01.sla.0000114227.70480.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Uenosono Y, Natsugoe S, Higashi H, Ehi K, Miyazono F, Ishigami S, Hokita S, Aikou T. Evaluation of colloid size for sentinel nodes detection using radioisotope in early gastric cancer. Cancer Lett. 2003;200:19–24. doi: 10.1016/s0304-3835(03)00389-6. [DOI] [PubMed] [Google Scholar]
- 35.Mochiki E, Kuwano H, Kamiyama Y, Aihara R, Nakabayashi T, Katoh H, Asao T, Oriuchi N, Endo K. Sentinel lymph node mapping with technetium-99m colloidal rhenium sulfide in patients with gastric carcinoma. Am J Surg. 2006;191:465–469. doi: 10.1016/j.amjsurg.2005.09.002. [DOI] [PubMed] [Google Scholar]
- 36.Yanagita S, Natsugoe S, Uenosono Y, Kozono T, Ehi K, Arigami T, Arima H, Ishigami S, Aikou T. Sentinel node micrometastases have high proliferative potential in gastric cancer. J Surg Res. 2008;145:238–243. doi: 10.1016/j.jss.2007.04.037. [DOI] [PubMed] [Google Scholar]
- 37.Ichikura T, Morita D, Uchida T, Okura E, Majima T, Ogawa T, Mochizuki H. Sentinel node concept in gastric carcinoma. World J Surg. 2002;26:318–322. doi: 10.1007/s00268-001-0226-x. [DOI] [PubMed] [Google Scholar]
- 38.Carlini M, Carboni F, Petric M, Santoro R, Guadagni F, Marandino F, Castelli M, Santoro E. Sentinel node in gastric cancer surgery. J Exp Clin Cancer Res. 2002;21:469–473. [PubMed] [Google Scholar]
- 39.Ryu KW, Lee JH, Kim HS, Kim YW, Choi IJ, Bae JM. Prediction of lymph nodes metastasis by sentinel node biopsy in gastric cancer. Eur J Surg Oncol. 2003;29:895–899. doi: 10.1016/j.ejso.2003.09.008. [DOI] [PubMed] [Google Scholar]
- 40.Song X, Wang L, Chen W, Pan T, Zhu H, Xu J, Jin M, Finley RK, Wu J. Lymphatic mapping and sentinel node biopsy in gastric cancer. Am J Surg. 2004;187:270–273. doi: 10.1016/j.amjsurg.2003.11.013. [DOI] [PubMed] [Google Scholar]
- 41.Osaka H, Yashiro M, Sawada T, Katsuragi K, Hirakawa K. Is a lymph node detected by the dye-guided method a true sentinel node in gastric cancer? Clin Cancer Res. 2004;10:6912–6918. doi: 10.1158/1078-0432.CCR-04-0476. [DOI] [PubMed] [Google Scholar]
- 42.Ishizaki M, Kurita A, Kubo Y, Takashima S, Nishina T, Nishimura E. Evaluation of sentinel node identification with isosulfan blue in gastric cancer. Eur J Surg Oncol. 2006;32:191–196. doi: 10.1016/j.ejso.2005.11.013. [DOI] [PubMed] [Google Scholar]
- 43.Park DJ, Lee HJ, Lee HS, Kim WH, Kim HH, Lee KU, Choe KJ, Yang HK. Sentinel node biopsy for cT1 and cT2a gastric cancer. Eur J Surg Oncol. 2006;32:48–54. doi: 10.1016/j.ejso.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 44.Rino Y, Takanashi Y, Hasuo K, Kawamoto M, Ashida A, Harada H, Inagaki D, Hatori S, Ohshima T, Yamada R, et al. The validity of sentinel lymph node biopsy using dye technique alone in patients with gastric cancer. Hepatogastroenterology. 2007;54:1882–1886. [PubMed] [Google Scholar]
- 45.Hayashi H, Ochiai T, Mori M, Karube T, Suzuki T, Gunji Y, Hori S, Akutsu N, Matsubara H, Shimada H. Sentinel lymph node mapping for gastric cancer using a dual procedure with dye- and gamma probe-guided techniques. J Am Coll Surg. 2003;196:68–74. doi: 10.1016/s1072-7515(02)01594-6. [DOI] [PubMed] [Google Scholar]
- 46.Karube T, Ochiai T, Shimada H, Nikaidou T, Hayashi H. Detection of sentinel lymph nodes in gastric cancers based on immunohistochemical analysis of micrometastases. J Surg Oncol. 2004;87:32–38. doi: 10.1002/jso.20077. [DOI] [PubMed] [Google Scholar]
- 47.Tonouchi H, Mohri Y, Tanaka K, Kobayashi M, Ohmori Y, Kusunoki M. Laparoscopic lymphatic mapping and sentinel node biopsies for early-stage gastric cancer: the cause of false negativity. World J Surg. 2005;29:418–421. doi: 10.1007/s00268-004-7732-6. [DOI] [PubMed] [Google Scholar]
- 48.Gretschel S, Bembenek A, Ulmer Ch, Hünerbein M, Markwardt J, Schneider U, Schlag PM. Prediction of gastric cancer lymph node status by sentinel lymph node biopsy and the Maruyama computer model. Eur J Surg Oncol. 2005;31:393–400. doi: 10.1016/j.ejso.2004.11.014. [DOI] [PubMed] [Google Scholar]
- 49.Ichikura T, Chochi K, Sugasawa H, Yaguchi Y, Sakamoto N, Takahata R, Kosuda S, Mochizuki H. Individualized surgery for early gastric cancer guided by sentinel node biopsy. Surgery. 2006;139:501–507. doi: 10.1016/j.surg.2005.09.005. [DOI] [PubMed] [Google Scholar]
- 50.Saikawa Y, Otani Y, Kitagawa Y, Yoshida M, Wada N, Kubota T, Kumai K, Sugino Y, Mukai M, Kameyama K, et al. Interim results of sentinel node biopsy during laparoscopic gastrectomy: possible role in function-preserving surgery for early cancer. World J Surg. 2006;30:1962–1968. doi: 10.1007/s00268-006-0142-1. [DOI] [PubMed] [Google Scholar]
- 51.Tajima Y, Yamazaki K, Masuda Y, Kato M, Yasuda D, Aoki T, Kato T, Murakami M, Miwa M, Kusano M. Sentinel node mapping guided by indocyanine green fluorescence imaging in gastric cancer. Ann Surg. 2009;249:58–62. doi: 10.1097/SLA.0b013e3181927267. [DOI] [PubMed] [Google Scholar]


