Abstract
Background.
The purpose was to test the effectiveness of two transdiagnostic group interventions compared to care as usual (CAU) for patients with anxiety, depressive or stress-related disorders within a primary health care context.
Objectives.
To compare the effects of cognitive-based-behavioural therapy (CBT) and multimodal intervention (MMI) on the quality of life and relief of psychological symptoms of patients with common mental disorders or problems attending primary health care centre.
Methods.
Patients (n = 278), aged 18–65 years, were referred to the study by the GPs and 245 were randomized to CAU or one of two group interventions in addition to CAU: (i) group CBT administered by psychologists and (ii) group MMI administered by assistant nurses. The primary outcome measure was the Mental Component Summary score of short form 36. Secondary outcome measures were Perceived Stress Scale and Self-Rating Scale for Affective Syndromes. The data were analysed using intention-to-treat with a linear mixed model.
Results.
On the primary outcome measure, the mean improvement based on mixed model analyses across post- and follow-up assessment was significantly larger for the MMI group than for the CBT (4.0; P = 0.020) and CAU (7.5; P = .001) groups. Participants receiving CBT were significantly more improved than those in the CAU group. On four of the secondary outcome measures, the MMI group was significantly more improved than the CBT and CAU groups. The course of improvement did not differ between the CBT group and the CAU group on these measures.
Conclusions.
Transdiagnostic group treatment can be effective for patients with common mental disorders when delivered in a primary care setting. The group format and transdiagnostic approach fit well with the requirements of primary care.
Key words: CBT, common mental disorders, MMI, primary health care, quality of life, transdiagnostic group interventions.
Introduction
Depression, anxiety and stress-related disorders are common among patients in primary health care (1), with many left untreated or even undiagnosed (2). These conditions are associated with high societal costs, functional disability (3,4) and are the main cause of increasing work absenteeism among patients in primary health care (1). There is currently very limited research on how to best treat these patients within a primary health care context (5), a context often characterized by limited access to psychologists and need for brief interventions that can be applied to a wide range of psychiatric disorders. Nevertheless, a variety of different treatment models are used, such as training GPs to treat patients with mental disorders, consultation, collaborative care and counselling. With a few exceptions, little evidence on the effectiveness of these treatments exists to date (5–7). Several attempts to improve care and decrease work absenteeism for this group of patients have been made, both in primary health care and in occupational health, with mixed results (8–10). Although validated treatments such as cognitive-behavioural-based therapy (CBT) exist to treat anxiety and depression, the protocols are designed for highly trained therapists working in specialty clinics and have rarely been tested in primary health care (11). So far, cognitive behavioural interventions to relieve psychological symptoms of mental disorders in primary health care have not produced convincing results (5), though there are promising treatments under development (12,13). Barlow et al. (12) recently presented results that show substantial reductions in symptoms of primary and co-morbid states of anxiety and depression in an individual treatment. Transdiagnostic treatment protocols, meaning that patients with, for example various anxiety and depressive disorders are treated the same way and often in groups may be particularly suited for primary health care where many patients often present a range of mild to moderate symptoms of more than one common mental disorder (14). There are some promising trials of transdiagnostic cognitive behavioural group treatments of anxiety disorders (15,16), but to our knowledge, there are no formal studies of this approach to the wider primary care patient population of concern in the present study. Neither has the non-expert multimodal intervention (MMI) model, used in this study, been empirically validated. Therefore, our aim was to test the effectiveness of two transdiagnostic group treatments, CBT and MMI, compared to care as usual (CAU) for patients with anxiety, depressive and stress-related disorders in a randomized controlled trial (RCT) conducted within a primary health care context. We hypothesized that group interventions coupled with CAU would improve quality of life and relieve psychological symptoms better than would CAU alone.
Methods
Trial design
We performed a RCT with two group interventions (CBT and MMI) and a CAU as control. During the first 4 months of the inclusion period, the CBT condition was not available due to a delay in the recruitment of therapists. Therefore, the randomization scheme was adjusted and changed twice during the recruitment period in order to finally reach approximately the same number in each condition. The randomization was computer generated. When a patient was about to be allocated to one of the three conditions, an email was sent with a code number to a statistician who was not involved otherwise in conducting the study.
Participants and recruitment
Patients were recruited between January 2006 and July 2007 from a population of patients seeking care at a large primary health care centre in Stockholm, Sweden, serving 36000 inhabitants. Twenty-nine GPs or resident physicians at the primary health care centre referred 278 patients to the study. The physicians were instructed to ask all patients aged 18–65 years who had common mental disorders including depression, anxiety, stress and somatoform disorder to participate. Patients were excluded if (i) they met diagnostic criteria for bipolar or psychotic disorder or severe personality disorder; (ii) they were judged to be at risk of committing suicidal acts and (iii) they had undergone MMI earlier. We paid no consideration to whether patients were treated with e.g. SSRI medication (serotonin selective reuptake inhibitors).
Interventions
Both group interventions took place at the primary health care centre. In both instances, the groups consisted of six participants. During group therapy, the GPs cared for the participants in the same way they cared for patients in the control group, e.g. prescribing medication and/or sick-listing.
Cognitive-behavioural-based therapy
Group CBT was based on generally acknowledged cognitive and behavioural treatment principles from the domain of anxiety and mood disorders. In this protocol, the group CBT treatment comprised one 120-minute group session per week for 12 weeks led by one of two licenced clinical psychologists with training and experience in delivering CBT. They received regular supervision by a psychologist with specialist training and extensive experience of CBT. The first four sessions focussed on developing conceptualizations of patients’ problems, and psycho-education on the role of thoughts and behaviours for psychiatric symptoms. Rationales were provided for exposure interventions for anxiety disorders and behavioural activation for depression, respectively. Sessions five to eleven focussed on exposure to feared stimuli and emotional awareness training. The final session focussed on acquiring new skills to handle risk situations for relapse. Each session opened with a recap of the previous session and proceeded with homework follow-up, psycho-education and practicing new skills. Homework assignments were formulated individually for each participant, at the end of the session.
Multimodal intervention
This was a group intervention following a protocol created by one of the authors (RS) consisting of a mix of existing group interventions and exercises utilized in a variety of therapeutic schools. Prior to the start of group treatment, participants met an assistant nurse for an individual appointment where a brief description of the treatment was given. During this session, the nurse also collected detailed information about the participants’ psychiatric problems and participants were asked to write down their goals and ideas for solutions to their problems. The group intervention comprised 150-minute group sessions twice a week for 6 weeks and sessions were led by one of three assistant nurses with only brief training. The main components of the treatment in the first week were a unified goal setting among the group members, psycho-education about thoughts, emotions and behaviours that are common in persons with depressive and anxiety symptoms. During the second week of treatment, the participants were introduced to an exercise where one participant shares a personal problem with the group and obtains feedback. Focus was also on the importance of physical training and participants were taught to do a few yoga exercises. The focus of the third and fourth weeks of the intervention was on understanding the difference between emotions and thoughts and strategies on how to deal with conflicts were presented. During the fifth week, participants were asked to invite important people in their lives to attend two sessions to work on team building. Participants and their guests were encouraged to take part in small group activities. During the final two sessions in the sixth week, strategies for handling difficult thoughts and emotions in highly stressful situations were presented. Following group therapy, each participant also had two additional individual sessions with the assistant nurse to discuss individual goals set prior to group therapy. Three assistant nurses administered the MMI intervention. They had no formal psychotherapeutic education and their training prior to this study was to take part in a MMI group treatment as a member and subsequently as an observer, except for one of the assistant nurses who had administrated the intervention for a couple of years at the primary health care centre prior to the study. They were thoroughly recruited and selected on the basis of their personal interest and judged suitability for the task. All three assistant nurses received weekly supervision by the originator of MMI or a group therapist.
Care as usual
Participants of the control group were not offered group therapy. CAU given by GPs at the primary health care centre consisted of appointments with GPs who were prescribing medication and sick-listing when necessary, referrals to the counsellor at the primary health care and more rarely to a psychiatric clinic. The GPs did not get any special training but were given information about inclusion and exclusion criteria.
Outcomes
Since participants had different psychiatric symptoms and diagnoses, we used the Mental Component Summary (MCS) score of short form 36 (SF-36) (17) as the primary outcome. As secondary outcome measure of anxiety and depressive symptoms, we used the Self-Rating Scale for Affective Syndromes (CPRS-S-A) (18) that is based on the Comprehensive Psychopathological Rating Scale (CPRS) and consists of 19 items that measure severity of depression, anxiety and symptoms of obsessive-compulsive disorders (OCD). The Perceived Stress Scale (PSS) (19) was used to measure severity of stress symptoms. Assessment points were at baseline (pre-treatment), directly following treatment (post-treatment) and 1 year after treatment completion (1-year follow-up).
Sample size
Assuming a treatment effect of 7% points in MCS and a SD of 15% points, a minimum of 74 persons per group would be needed to achieve 80% statistical power at 5% significance level. With an expected drop-out rate of 10%, ~80 patients were randomly allocated to each condition.
Blinding
Participants and investigators were not blinded to intervention allocation.
Trial procedures
Baseline assessment of patients referred by the GPs at the primary health care centre was conducted by two of the investigators using the Structured Clinical Interview for DSM-IV Axis I Disorders (20) to obtain Diagnostic and Statistical Manual of Mental Disorders (DSM)-IV diagnoses. Self-rating scales, PSS and CPRS-S-A were used and information on background factors such as education, family situation and employment were collected. After providing participants with a description of the study, written informed consents were collected from all participants. A total of 82% (n = 200) provided data at post-treatment assessment and 96% (n = 235) completed assessment at 1-year follow-up. For 24 participants, the 1-year follow-up assessment was delayed 4–19 months.
Statistical methods
The data were analysed using intention-to-treat. The primary end points were analysed using a linear mixed model where the response at post-assessment and 1-year follow-up were included as dependent variables, and group, time and baseline value of the response variable were added as fixed factors in the model. The intercept of each subject was added as a random factor. Based on the linear mixed model, inferences could be made on the difference between groups and over time. The association between group and time was evaluated and found non-significant. The model assumptions were controlled using standard checks, such as evaluation of the distribution of residuals. Effect sizes were calculated using Cohen’s d.
In addition to the primary analyses, several sensitivity analyses were performed to assess the robustness of the results. The sensitivity analysis consisted of tests that included different definitions of the data set, such as completers, last observation carried forward and analysing the effect of different randomization schemes. The sensitivity analyses also included different variants of the statistical model such as considering time as a continuous variable and adjusting for potentially influential baseline variables. Since the sensitivity analyses produced the same results as did primary analysis, the former are not shown here.
Ethical committee
We obtained ethical approval from The Regional Ethics Committee of Stockholm Dnr 2005/447-31.
Results
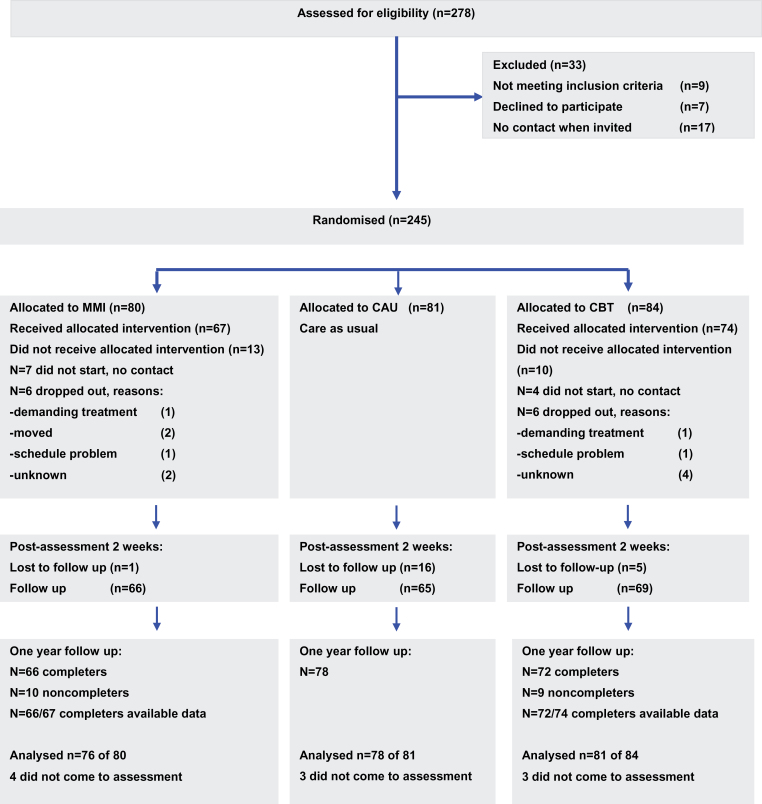
A participant recruitment flow chart is shown in Figure 1. Background data (Table 1) showed that most participants were middle-aged women with an average to high educational level. Mood disorders were the predominant diagnoses among the participants (n = 139; 57%) and in this group major depression was the most common diagnosis (73.4%). Anxiety disorders were diagnosed in 91 participants (37.3%) with unspecified anxiety being most prevalent (37.4%) followed by specific phobia (30.8%). For about one-fourth of the participants, no diagnosis according to DSM-IV criteria was present at the time of the interview. There were markedly fewer in the MMI group than in the other conditions that lacked a diagnosis. This and other differences in baseline characteristics are discussed in the Statistical methods section. Attrition rates did not differ between intervention groups (16% in MMI, 12% in CBT).
Figure 1.
Participant recruitment flow chart.
Table 1.
Background characteristics
| Variable | MMI (N = 80) | CBT (N = 84) | CAU (N = 81) |
|---|---|---|---|
| Mean age (SD) | 44.3 (9.5) | 43.3 (10.3) | 45.0 (9.5) |
| Women, n (%) | 68 (85) | 63 (75) | 67 (82.7) |
| Mean BMI (SD) | 26.7 (5.9) | 25.7 (3.8) | 25.9 (4.6) |
| Smokers, n (%) | 18 (22.5) | 30 (35.7) | 28 (34.6) |
| Education (highest) | |||
| Elementary school | 17 (21.3) | 17 (20.2) | 20 (24.7) |
| Secondary school | 29 (36.2) | 41 (48.8) | 37 (45.7) |
| University/college | 34 (42.5) | 26 (31.0) | 24 (29.6) |
| Psychiatric diagnoses (DSM-IV)a | |||
| Mood disorders | 52 (65.0) | 46 (54.8) | 41 (51.2) |
| Anxiety disorders | 33 (41.2) | 32 (38.1) | 26 (32.5) |
| Somatoform disorders | 5 (6.2) | 2 (2.4) | 3 (3.8) |
| Eating disorders | 2 (2.5) | 1 (1.2) | 3 (3.8) |
| Alcohol dependence | 1 (1.2) | 0 | 1 (1.2) |
| Not fulfilling psychiatric disorder criteria | 11 (13.8) | 20 (23.8) | 24 (29.6) |
aPercentages do not add up to 100 since patients could have co-morbid disorders.
Primary outcome measure
Table 2 shows the means (SDs) of the different outcome variables at the three assessment points and Table 3 shows the outcome of the significance tests using linear mixed model analysis. The primary outcome measure was the MCS of SF-36. The mean improvement at post-treatment and 1-year follow-up was significantly higher among participants in the MMI group than those in the CBT and CAU group. CBT participants were significantly more improved than CAU participants. The effect size (Cohen’s d) between MMI and CAU groups was moderate on SF-36 MCS at post-treatment and 1-year follow-up and small when comparing MMI to CBT.
Table 2.
Summary of results at pre-, post- and follow-up assessment
| Variable | Group | Pre | Post | Follow-up | |||
|---|---|---|---|---|---|---|---|
| n | Mean (SD) | n | Mean (SD) | n | Mean (SD) | ||
| SF-36 MCS | MMI | 80 | 24.2 (11.5) | 65 | 40.8 (12.2) | 76 | 43.0 (12.6) |
| CBT | 84 | 27.3 (12.7) | 68 | 38.3 (12.6) | 80 | 40.4 (13.7) | |
| CAU | 81 | 25.3 (13.3) | 63 | 33.0 (14.4) | 78 | 37.1 (13.1) | |
| SF-36 PCS | MMI | 80 | 45.9 (11.0) | 65 | 48.2 (10.6) | 76 | 49.9 (10.3) |
| CBT | 84 | 43.9 (12.4) | 68 | 45.7 (11.9) | 80 | 45.1 (13.4) | |
| CAU | 81 | 45.9 (11.2) | 63 | 45.8 (11.6) | 78 | 47.8 (11.5) | |
| CPRS-S-A: Depression | MMI | 80 | 20.7 (8.2) | 66 | 10.1 (7.1) | 76 | 8.8 (7.0) |
| CBT | 84 | 18.5 (8.1) | 69 | 12.4 (8.2) | 81 | 10.7 (9.0) | |
| CAU | 81 | 19.6 (8.6) | 64 | 14.5 (8.9) | 78 | 12.3 (9.2) | |
| CPRS-S-A: Anxiety | MMI | 80 | 21.2 (8.1) | 66 | 13.0 (7.5) | 76 | 11.1 (7.2) |
| CBT | 84 | 20.5 (8.2) | 66 | 14.5 (8.1) | 81 | 13.6 (8.8) | |
| CAU | 81 | 20.3 (7.3) | 61 | 16.4 (8.3) | 78 | 14.2 (8.1) | |
| CPRS-S-A: OCD | MMI | 80 | 17.2 (7.1) | 66 | 8.8 (5.8) | 76 | 7.1 (6.1) |
| CBT | 84 | 15.2 (7.4) | 66 | 9.9 (6.9) | 81 | 8.8 (7.7) | |
| CAU | 81 | 16.4 (7.5) | 61 | 12.0 (8.6) | 78 | 9.9 (7.5) | |
| PSS | MMI | 80 | 33.5 (7.7) | 66 | 20.8 (8.5) | 76 | 20.6 (9.1) |
| CBT | 84 | 33.2 (7.4) | 69 | 24.8 (8.7) | 81 | 24.2 (8.7) | |
| CAU | 81 | 33.8 (7.7) | 65 | 27.7 (9.2) | 78 | 25.3 (9.6) | |
PCS, Physical Component Summary.
Table 3.
Estimates of treatment effects based on mixed model analyses and Cohen’s d
| Measure | Comparison | Treatment effect | Cohen’s d | ||
|---|---|---|---|---|---|
| Meana (95% CI) | P-value | Post | Follow-up | ||
| SF-36 MCS | MMI versus CAU | 7.5 (4.1 to 10.9) | 0.001 | 0.59 | 0.46 |
| CBT versus CAU | 3.5 (0.2 to 6.9) | 0.039 | 0.39 | 0.25 | |
| MMI versus CBT | 4.0 (0.6 to 7.4) | 0.020 | 0.20 | 0.20 | |
| SF-36 PCS | MMI versus CAU | 2.1 (−0.3 to 4.5) | 0.085 | 0.22 | 0.19 |
| CBT versus CAU | 0.0 (−2.4 to 2.4) | 1.0 | −0.01 | −0.22 | |
| MMI versus CBT | 2.1 (−0.3 to 4.5) | 0.084 | 0.22 | 0.40 | |
| CPRS-S-A: Depression | MMI versus CAU | 4.3 (2.3 to 6.3) | 0.001 | 0.55 | 0.43 |
| CBT versus CAU | 1.3 (−0.7 to 3.3) | 0.198 | 0.25 | 0.18 | |
| MMI versus CBT | 3.0 (1.0 to 5.0) | 0.003 | 0.30 | 0.24 | |
| CPRS-S-A: Anxiety | MMI versus CAU | 3.7 (1.9 to 5.6) | 0.001 | 0.43 | 0.40 |
| CBT versus CAU | 1.0 (−0.9 to 2.8) | 0.302 | 0.23 | 0.07 | |
| MMI versus CBT | 2.8 (0.9 to 4.6) | 0.003 | 0.19 | 0.31 | |
| CPRS-S-A: OCD | MMI versus CAU | 3.1 (1.3 to 4.9) | 0.001 | 0.44 | 0.41 |
| CBT versus CAU | 0.7 (−1.1 to 2.4) | 0.450 | 0.27 | 0.15 | |
| MMI versus CBT | 2.4 (0.6 to 4.2) | 0.009 | 0.17 | 0.24 | |
| PSS | MMI versus CAU | 5.4 (3.1 to 7.7) | 0.001 | 0.78 | 0.50 |
| CBT versus CAU | 1.6 (−0.7 to 3.8) | 0.165 | 0.32 | 0.12 | |
| MMI versus CBT | 3.8 (1.6 to 6.1) | 0.001 | 0.47 | 0.41 | |
CI, confidence interval; PCS, Physical Component Summary.
aAverage difference at post and follow-up adjusted for baseline difference.
Secondary outcome measures
On all three subscales of the CPRS-S-A and PSS, MMI showed a significantly higher treatment effect than did both CBT and CAU, whereas CBT did not differ from CAU on any of these measures. At post-treatment and 1-year follow-up, the effect sizes between the MMI and CAU group were moderate on the CPRS-S-A (depression subscale) and the PSS, whilst small on anxiety and obsessive–compulsive subscales of the CPRS-S-A. The effect sizes between CBT and CAU were small on SF-36 MCS, CPRS-S-A Depression, Anxiety and PSS. Finally, the effect sizes between MMI and CBT groups were small on SF-36 MCS, Physical Component Summary, CPRS-S-A Depression and PSS. At 1-year follow-up, all but one of the effect sizes were reduced.
Discussion
The aim of this study was to investigate whether two psychological group interventions (CBT and MMI) in addition to CAU improved patients’ quality of life and relieved psychological symptoms better than CAU alone. We hypothesized that both CBT and MMI would be better than CAU, whereas no difference was thought to exist between CBT and MMI. The primary outcome measure (SF-36 MCS) showed that both treatments were significantly better at improving quality of life than CAU, and in the same way MMI was shown to be more effective than CBT. On the secondary outcome measures, only MMI had significantly larger effects than CAU. The results were obtained in a primary care setting with participants mainly consisting of middle-aged women with a medium to high educational level.
We view these results as important for several reasons. Many patients display an array of health problems that call for a variety of interventions, beyond those contained in any diagnosis-specific treatment protocol. In addition, there is a lack of properly trained therapists in primary care to treat these patients (1). Although the effect sizes we observed were small to moderate, our results hint towards the need to continue developing these treatments further to complement CAU for patients with common psychiatric disorders attending primary health care centres. This would enable highly trained therapists to focus on the severe cases, whereas those with less training could take on the milder cases, as is done in psychiatric outpatient clinics in England under the Increased Access to Psychological Treatment (21) program. Our study showed that MMI as a group intervention given by non-expert therapists may be a promising treatment for mild to moderate mental disorders and problems in primary health care.
One of the limitations of this study was the fact that the CBT protocol was based on principles derived mainly from treatments validated as individual treatments or group treatments confined to patients with anxiety disorders. The present protocol was implemented within a primary health context without previous trials. The reason for this was that no generally accepted treatment manual for CBT group treatment for the mixed diagnostic population of concern existed at the time the study began. Usually a protocol must have already been in use for some time and changed accordingly to accommodate the participants. Another limitation was that the two group interventions differed both in total treatment and composition (number of group versus individual sessions). CBT consisted of twelve 120-minute group sessions and one individual session, whereas MMI consisted of twelve 150-minute group sessions and three individual sessions. The total treatment time for CBT was 24 hours plus one individual session and for MMI 30 hours plus three individual sessions (one before and two after the group treatment). Hence, it is possible that the more than 25% longer treatment time for MMI may have had a positive bias on the outcomes, including a so-called attention placebo effect. Another possibility is that the differences in treatment intensity during the early phase of the treatment may have differential impact on outcome. A further limitation is the fact that we did not compare the two new transdiagnostic group interventions with a single evidence-based treatment for group or individual format. Therefore, it would be interesting to compare MMI with an evidence-based form of CBT. The investigators who conducted the follow-up assessment should ideally have been independent from the study and blinded to which intervention had been delivered to the participants. The potential bias is probably limited as only self-rating formulas were used and no ratings were made by the investigators. As an important possible limitation, it should finally be pointed out that one of the investigators had designed the MMI intervention and has afterwards delivered this treatment within a private company. However, even though he participated in the planning of the study and approved of the final manuscript, he took no part in the assessments of the participants or analysis of the data.
Conclusions
We could tentatively conclude that MMI and CBT were more effective than CAU in improving patients’ quality of life. Both interventions were in a group format rather than as individual treatment and they were designed to apply to several diagnoses at once, which is a promising approach for patients with various anxiety and depressive disorders presented in primary health care, even in regards to long-term outcome.
Declaration
Funding: Stockholm County Council; Centre for Knowledge and Common Development (LS 0901-0006).
Ethical approval: the Regional Ethics Committee of Stockholm (Dnr 2005/447-31).
Conflict of interest: RS has, after the trial, started a private company that provides treatment based on the MMI used here, under the name Inner Leadership Development (ILD).
Acknowledgements
Authors’ contributions: KE, RS, AE, LB, MA and LGB designed the study. L-GO, JR and RS designed the different interventions. KE and LGB performed the patient interviews. KE, LGB and L-GO analysed and classified the data. LB planned and preformed the statistical analysis. All authors contributed to the manuscript. All authors read and approved the final manuscript. The RCT was indexed at www.clinicaltrials.gov (ID number NCT01565213).
References
- 1. Henderson M, Glozier N, Holland Elliott K. Long term sickness absence. BMJ 2005; 330: 802–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Nordström A, Bodlund O. Every third patient in primary care suffers from depression, anxiety or alcohol problems. Nord J Psychiatry 2008; 62: 250–5 [DOI] [PubMed] [Google Scholar]
- 3. Kessler RC. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry 2005; 62: 617–27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Smit F, Cuijpers P, Oostenbrink J, Batelaan N, de Graaf R, Beekman A. Costs of nine common mental disorders: implications for curative and preventive psychiatry. J Ment Health Policy Econ 2006; 9: 193–200 [PubMed] [Google Scholar]
- 5. Bower P, Knowles S, Coventry PA, Rowland N. Counselling for mental health and psychosocial problems in primary care. Cochrane Database Syst Rev 2011; 9: CD001025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Simon GE, VonKorff M, Rutter C, Wagner E. Randomised trial of monitoring, feedback, and management of care by telephone to improve treatment of depression in primary care. BMJ 2000; 320: 550–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Seekles W, Cuijpers P, Kok R, Beekman A, van Marwijk H, van Straten A. Psychological treatment of anxiety in primary care: a meta-analysis. Psychol Med 2013; 43: 351–61 [DOI] [PubMed] [Google Scholar]
- 8. van der Klink JJ, Blonk RW, Schene AH, van Dijk FJ. Reducing long term sickness absence by an activating intervention in adjustment disorders: a cluster randomised controlled design. Occup Environ Med 2003; 60: 429–37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Blonk RWB, Brenninkmeijer V, Lagerveld SE, Houtman ILD. Return to work: a comparison of two cognitive behavioural interventions in cases of work-related psychological complaints among the self-employed. Work Stress 2006; 20: 129–44 [Google Scholar]
- 10. de Vente W, Kamphuis JH, Emmelkamp PM, Blonk RW. Individual and group cognitive-behavioral treatment for work-related stress complaints and sickness absence: a randomized controlled trial. J Occup Health Psychol 2008; 13: 214–31 [DOI] [PubMed] [Google Scholar]
- 11. National Institute for Health and Clinical Excellence. Generalised Anxiety Disorder and Panic Disorder (With or Without Agoraphobia) in Adults (CG113). London: The British Psychological Society & The Royal College of Psychiatrists, 2011 [Google Scholar]
- 12. Barlow DH. Psychological treatments. Am Psychol 2004; 59: 869–78 [DOI] [PubMed] [Google Scholar]
- 13. Wilamowska ZA, Thompson-Hollands J, Fairholme CP, Ellard KK, Farchione TJ, Barlow DH. Conceptual background, development, and preliminary data from the unified protocol for transdiagnostic treatment of emotional disorders. Depress Anxiety 2010; 27: 882–90 [DOI] [PubMed] [Google Scholar]
- 14. McManus F, Shafran R, Cooper Z. What does a transdiagnostic approach have to offer the treatment of anxiety disorders? Br J Clin Psychol 2011; 49(Pt 4): 491–505 [DOI] [PubMed] [Google Scholar]
- 15. Norton PJ. An open trial of a transdiagnostic cognitive-behavioral group therapy for anxiety disorder. Behav Ther 2008; 39: 242–50 [DOI] [PubMed] [Google Scholar]
- 16. Ericson DH, Janeck AS, Tallman K. Transdiagnostic CBT for anxiety: clinical experience and practical advice. J Cogn Psychotherapy 2009; 23: 34–43 [Google Scholar]
- 17. Ware JE, Snow KK, Kosinski M, Gandek B. SF-36 Health Survey Manual and Interpretation Guide. Boston, MA: The Health Institute, New England Medical Center, 1993 [Google Scholar]
- 18. Svanborg P, Asberg M. A new self-rating scale for depression and anxiety states based on the Comprehensive Psychopathological Rating Scale. Acta Psychiatr Scand 1994; 89: 21–8 [DOI] [PubMed] [Google Scholar]
- 19. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav 1983; 24: 385–96 [PubMed] [Google Scholar]
- 20. APA. Diagnostic and Statistical Manual of Mental Disorders. 4th edn. Washington, DC: American Psychiatric Association, 1994 [Google Scholar]
- 21. Clark DM. Implementing NICE guidelines for the psychological treatment of depression and anxiety disorders: the IAPT experience. Int Rev Psychiatry 2011; 23: 318–27 [DOI] [PMC free article] [PubMed] [Google Scholar]