Abstract
The patient was an otherwise usually fit and well 25-year-old man who presented to A&E department in extremis. The initial working diagnosis was a tension pneumothorax, and he was subsequently treated with needle thoracocentesis causing a release of air. A chest radiograph was taken, after which a chest drain was inserted. Bilious fluid was drained from the chest drain. The patient was taken for an emergency CT, which demonstrated a Bochdalek diaphragmatic hernia, with the spleen and bowel found to be causing a near total left lung collapse. He was taken to the theatre to return the bowel to the correct anatomical position, in addition to undergoing a sleeve gastrectomy, and diaphragmatic defect repair. The patient has had a complex and protracted recovery in the intensive therapy unit (ITU) with complications including wound dehiscence, gastrectomy leak requiring additional surgical repair, fluid overload and bilateral pleural empyema.
Background
This case highlights a rare and interesting surgical emergency, namely that of a tension gastrothorax. In this particular case, it was caused by a Bochdalek hernia, which is extremely rare in adults, with only approximately 100 cases reported in the literature.1 It has mimicked the presentation of a tension pneumothorax, and should be suspected if needle thoracocentesis does not lead to an improvement in clinical condition in a patient with a suspected tension pneumothorax.
Case presentation
The patient was a 25-year-old man who is otherwise fit and well. He had a 4-day history of progressively worsening abdominal pain. He was brought to A&E department in extremis, conscious but extremely distressed: heart rate 170 bpm, respiratory rate 50, pH 7.2, lactate 7, base excess −12 and creatinine 250 indicative of an acute kidney injury.
On examination, the patient had right-sided heart sounds, right tracheal deviation, left-sided hyper-resonance and a left-sided reduction in breath sounds, all consistent with tension pneumothorax. Needle thoracocentesis was performed leading to a release in air, but with minimal improvement in clinical condition. An additional needle thoracocentesis was undertaken, before the patient underwent a chest radiograph (figure 1). Following this, a chest drain was inserted, which released the bilious content.
Figure 1.
Radiograph on admission.
The patient was immediately taken for a chest and abdominal CT (figures 2 and 3), which revealed that the spleen and a substantial amount of bowel had herniated through a diaphragmatic defect (thought to be an undiagnosed congenital bochdalek diaphragmatic defect). It also demonstrated a near total collapsed left lung, free gas and fluid in the pleura and peritoneum, the intercostal drain lying in the mesentery and large bowel faecal impaction.
Figure 2.
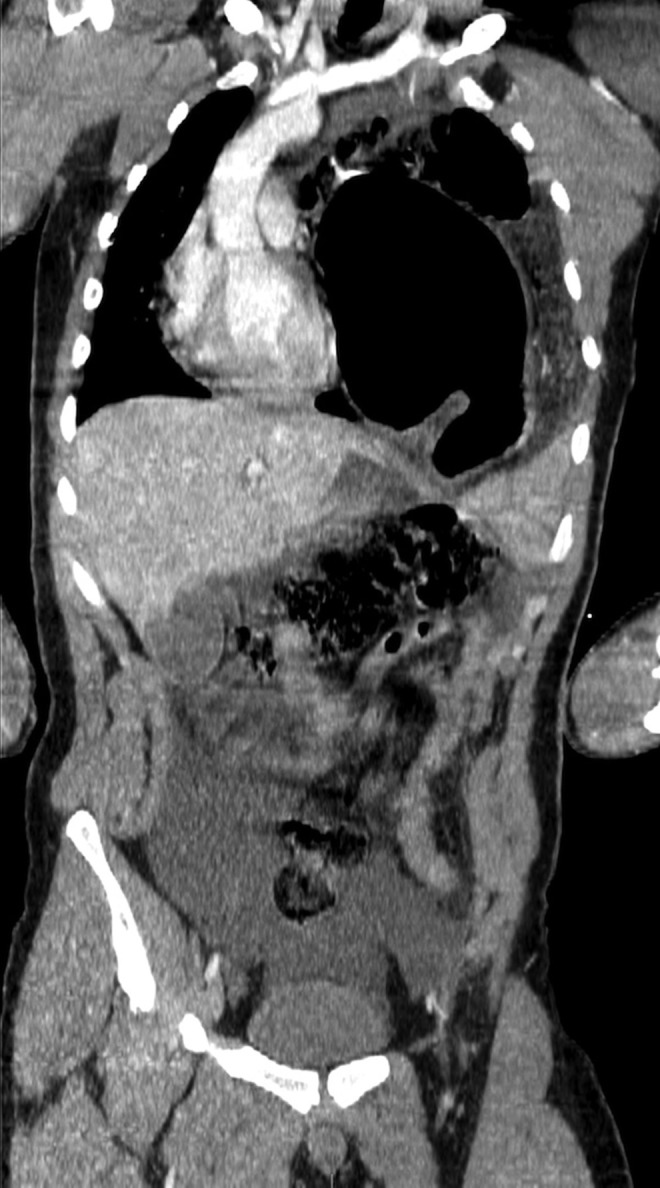
Initial CT scan (coronal view).
Figure 3.

Initial CT scan (axial view).
Differential diagnosis
Why this presentation could be potentially mistaken for a tension pneumothorax:
Right-sided heart sounds
Right tracheal deviation
Left-sided tympanic hyper-resonance
Left-sided reduction in breath sounds
Why this presentation is not a tension pneumothorax:
In the case of tension pneumothorax, you would expect to see an absence of lung markings peripheral to the visceral pleural white line. In the initial radiograph (figure 1), this is not the case.
Bowel gas is present in the thorax—there is a clearly delineated, distended gas-filled viscus shown in the initial chest radiograph (figure 1).
The left hemi-diaphragm is not clear, whereas in a tension pneumothorax, the affected hemi-diaphragm is usually more clear and pushed inferiorly.
There was little or no improvement in clinical condition despite needle thoracocentesis.
There was left-sided tympanic hyper-resonance anteriorly in this man. It is unclear as to whether the lung bases were percussed in the initial examination. You would expect the lung base on the side of a tension pneumothorax to be hyper-resonant on percussion; however, in a tension gastrothorax, the lung base would be dull to percussion.
Treatment
The patient was taken to the theatre, and underwent operative return of bowel contents to their anatomical position, a sleeve gastrectomy for a necrotic greater curvature of the stomach, repair of two small perforations from the aforementioned thoracocentesis and repair of the diaphragmatic defect. The large bowel was also manually evacuated.
Outcome and follow-up
Following the initial surgical intervention, the patient made an excellent recovery in the intensive therapy unit (ITU) being extubated and off all inotropic support within 24 h. His postoperative radiograph demonstrates the reinflation of his left lung following the return of the gastrointestinal contents to their correct anatomical position (figure 4). Unfortunately, his abdominal wound was slow to heal, and began to dehisce. Later that week, he deteriorated becoming increasingly agitated and confused. For his own safety, he was reintubated and ventilated, and was returned to the theatre for surgical reassessment of the wound. At this point, the sleeve gastrectomy was also found to be leaking, and was subsequently repaired. The patient was returned to ITU for multiorgan support. He remained sedated for a number of days, being slowly weaned off inotropes and ventilatory support. He soon developed persistent fever ranging from 38.5°C to 40°C, with associated raised inflammatory markers despite broad-spectrum antibiotics and an antifungal agent. A repeat CT demonstrated bilateral pleural effusions with a left-sided loculated pleural empyema. Bilateral intercostal drains were inserted. Intra-pleural streptokinase was delivered into the left intercostal drain in an attempt to break down the loculation. The empyema was drained, and the patient's condition slowly improved without cardiothoracic intervention. He was discharged to a surgical ward following a prolonged stay in the ITU. At the time of writing, the patient is awaiting discharge from hospital.
Figure 4.
Postoperative chest radiograph.
Discussion
Bochdalek hernias are a rare presentation in adults, and so reported cases in the literature are scarce.1–3 The majority are left-sided like our case, although in very rare circumstances, right-sided presentations are possible.4 Many of the cases describe patients experiencing intermittent, unexplainable abdominal pain over many years. They then present at a later time with severe abdominal pain and in extremis. In addition, there have also been instances, much like our case, where chest drains have been inserted erroneously due to the severity and urgency of the presenting situation in the emergency department.2 All the cases indicate the difficulty of interpreting these particular chest radiographs, and the requirement for differential diagnoses to be sought if there is little change or continued deterioration in clinical condition despite needle thoracocentesis. In addition, the papers highlight the need for early CT and surgical intervention when a symptomatic congenital diaphragmatic hernia is diagnosed.5 Portable ultrasonography at the bedside is being utilised with increasing frequency for fast diagnosis of intrathoracic pathologies, and could have been of benefit in this case.
Learning points.
Bochdalek hernias are an extremely rare presentation in adults, but can present with abdominal pain, pleuritic pain and dyspnoea.
Delays in the diagnosis of Bochdalek hernias should be minimised where possible, as they are associated with significant mortality.
A tension gastrothorax is an important, but rare differential for tension pneumothorax, and should be suspected if needle thoracocentesis does not lead to an improvement in clinical condition.
Acknowledgments
The author would like to thank Dr Paul Margetts (ITU specialist trainee) who offered his guidance on submitting this case report.
Footnotes
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Giannoulis K, Sutton R. Bochdalek hernia presenting in adult life: report of an unusual case and review of the literature. Ann Gastroenterol 2004;17:109–12 [Google Scholar]
- 2.Karanikas ID, Dendrinos SS, Liakakos TD, et al. Complications of congenital posterolateral diaphragmatic hernia in the adult. Report of two cases and literature review. J Cardiovasc Surg (Torino) 1994;35:555–8 [PubMed] [Google Scholar]
- 3.Losanoff JE, Sauter ER. Congenital posterolateral diaphragmatic hernia in an adult. Hernia 2004;8:83–5 [DOI] [PubMed] [Google Scholar]
- 4.Sofi FA, Ahmed SH, Dar MA, et al. Nontraumatic massive right-sided Bochdalek hernia in an adult: an unusual presentation. Am J Emerg Med 2011;29:356.e5–7 [DOI] [PubMed] [Google Scholar]
- 5.Naunheim KS. Adult presentation of unusual diaphragmatic hernias. Chest Surg Clin N Am 1998;8:359–69 [PubMed] [Google Scholar]




