Abstract
The role of posterior cervical musculature in sensorimotor control, cervicocephalic pain, and stabilization of the spinal cord has been recently described. Anatomical soft tissue connections which cross the cervical epidural space link suboccipital muscle fascia and dura. These myodural bridges provide passive and active anchoring of the spinal cord. They may also be involved in a dural tension monitoring system to prevent dural infolding, and maintain patency of the spinal cord. Modulation of dural tension may be initiated via a sensory reflex to muscular contractile tissues. Unanticipated movements such as hyperflexion extension injuries stimulate deep suboccipital muscles and transmit tensile forces through the bridge to the cervical dura. Due to its larger cross sectional area, the rectus capitis posterior major myodural bridge may exert greater mechanical traction on the dura than the rectus capitis posterior minor. University ethics committee approval and anatomical donor consent was obtained for this study.
Keywords: rectus capitis posterior major, obliquus capitis inferior, myodural bridge, dura mater
Abstract
Le rôle de la musculature cervicale postérieure dans le contrôle sensorimoteur, la douleur cervico-céphalique et la stabilisation de la moelle épinière n’a que récemment fait l’objet d’une description. Les connexions anatomiques des tissus mous qui traversent l’espace épidural cervical lient le fascia et la dure-mère des muscles sous-occipitaux. Ces ponts myoduraux offrent un point d’ancrage passif et actif à la moelle épinière. Ils peuvent aussi participer au système de contrôle de la tension durale afin de prévenir le repliement dural et de maintenir la perméabilité de la moelle épinière. Les modulations de la tension durale peuvent être provoquées par un réflexe sensoriel aux tissus musculaires contractiles. Les mouvements non anticipés comme les blessures résultant d’une hyperflexion-extension stimulent les muscles sous-occipitaux profonds et transmettent des efforts de traction par le pont sur la dure-mère cervicale. En raison de sa plus grande section transversale, le pont myodural grand droit postérieur peut exercer une plus grande traction mécanique sur la dure-mère que le muscle petit droit postérieur. L’approbation du comité d’éthique de l’université et le consentement du donneur anatomique ont été obtenus pour la présente étude.
Keywords: grand droit postérieur, oblique inférieur de la tête, pont myodural, dure-mère, chiropratique
Introduction
The cervical spine is a complex anatomical structure that is of interest to anatomists, biomechanists, and clinicians. Soft tissue communications linking suboccipital muscle fascia and the dura and its role in cervical neuro-muscular control have been examined recently.1–8 These myodural bridges have been associated with the etiology of cervicocephalic headaches, and cervicocephalic pain syndromes.3,9 These epidural connections may also be involved passively as a dural anchor and as an active stabilizer of the spinal cord.4,6,10
Recent studies have described myodural communications bridging the epidural spaces between the rectus capitis posterior minor (RCPmi), rectus capitis posterior major (RCPma), and obliquus capitis inferior (OCI) suboccipital muscles and the dura mater of the cervical spine.1–8 Anatomical studies by Khan, Hack, Scali, Pontell, and others have reported on the presence of myodural bridges linking sub-occipital muscles with the dura mater of the cervical spine.1,2,4,6 Additional studies by Shinomiya, Humphreys, Nash, Zumpano and Tagil confirmed these findings.13,10–13 Connections between the suboccipital musculature fascia and cervical dura mater have implications in cervicocephalic pain syndromes, sensorimotor function, and postural control.14–17 The clinical relevance of these cervical epidural membranes and their relationship to cervicogenic and tension headache syndromes has been discussed by multiple authors including Bates, Schoenen, Haldeman, Fernandez-De-Las-Penas and others.9,14–17 Changes in cervical proprioception, balance, sympathetic tone, conversion of muscle type, and dural enfolding secondary to cervical spine injuries have been described by several authors including Palmgren, Rix, Uhlig, Cailliet, Lusczyk.18–25,
Anatomical research and reviews of existing literature concerning the fascial connections between the suboccipital muscles and the cervical dura have been reported recently.1–8 In 1992 a fascial connection between was briefly mentioned by Kahn et al., in a report of the posterior intervertebral spaces of the cervical craniovertebral joint.1 It was noted however, that a true membrane connecting the posterior arch of the atlas to the laminae of the axis did not exist, but rather two fibrous planes that transected this space.1 Hack et al, reported on a myodural bridge between the fascia of the rectus capitis posterior minor (RCPmi) muscles in 1995.2,26 An examination of the posterior atlantooccipital interspace showed a continuous band of tissue with fibers oriented primarily perpendicular to the muscle and dura.2,26 A animal model study of 43 specimens in 1996 by Shinomiya et al. examined the ligamentous attachments within the cervical posterior epidural space.10 They confirmed the presence of abundant posterior epidural ligaments attaching to the posterior dura mater.10 Dissections of seven human cadaveric specimens by Rutten et al. in 1997, agreed with previous findings of an epidural connection between the RCPmi and the posterior wall of the spinal cord dura mater.24 Alix and Bates reported on previous anatomical findings and suggested that the ligamentous connection between muscle and the pain sensitive dura mater may provide an anatomic and physiological basis for cervicogenic headaches.9 After a gross anatomical dissection of 30 cadaveric specimens in 2003, followed by magnetic resonance imaging (MRI) of 4 specimens, Humphreys’ et al, also confirmed the presence of a fibrous connection bridging the epidural space linking the dura and RCPmi.13 In a case report describing an anatomical variation of a bifurcated RCPmi discovered during a routine dissection in 2005, Tagil confirmed the presence of dense connective tissue linking suboccipital muscle fascia to the cervical dura mater.3 Nash et al, employed sheet plastinations and confocal microscopy in an examination of the posterior atlanto-occipital interspace.12 They noted the presence of connective tissue attaching the RCPmi fascia and the spinal dura mater in the posterior cranio-cervical region in adult human cadavers.12 A larger study of seventy five cadavers by Zumpano et al. in 2006, examined variations in prevalence, tissue-type, gender in the soft-tissue bridge between RCPmi and dura mater.11 They reported similar findings in the structure of the RCPmi myodural bridge as previous authors.27 According to Kahkeshani and Ward, the myodural bridge has been underreported due the time necessary to properly dissect this region.27 To encourage further study; they describe a method for the deep dissection of the suboccipital triangle which preserves the RCPmi and its attachments for further inspection.27
We recently reported on two additional epidural connections to the cervical dura.4–7 Myodural bridges extending from the anterior fascia of the rectus capitis posterior major (RCPma) and obliquus capitis inferior (OCI) muscles, attaching on the cervical dura mater was documented recently by Scali, and Pontell in 2011 and 2013 (fig1).4–7 In an anatomical study by Scali et al., 13 embalmed human cadaveric specimens showed broad fascial connections traversing the cervical epidural space from the RCPma muscle fascia, anterio-inferiorly to the posterior dural surface (fig 2).4 RCPma myodural tissues from 11 specimens stained with hematoxylin and eosin indicated that the fascial connection inserted directly into the fascia surrounding the RCPma and attached to the posterior surface of the dura (fig 3).5 Immunohistochemical analysis using anti-neurofilament protein fluorescent antibody staining showed a pattern of nerve distribution throughout one tissue sample (fig 4).5 Pontell et al. dissected nine human cadaveric specimens, examining 14 OCI muscles and surrounding tissue.6 We documented a continuous fibrous tissue originating at the anterior fascia of the OCI muscle belly and projecting anteriorly across the atlanto-axial interspace and attaching to the posterolateral aspect of the cervical dura mater between the first and second cervical vertebrae.6 Histological analysis was performed on 12 OCI suboccipital muscles, connective tissue, and dura mater from human cadavers between the ages of 49 to 81.7 Microscopic examination of OCI myodural tissues stained with hematoxylin and eosin showed the connective tissue emanating from the ventral OCI muscular fascia and inserted directly into the posterolateral aspect of the cervical dura mater.7 A single OCI myodural connection stained for immuno-peroxidase using Dako’s neurofilament protein monoclonal antibodies revealed fascicles traveling perpendicular, and parallel with the OCI myodural bridge.7 Due to proximity, the RCPma and OCI muscles appear to form a single atlantoaxial myodural bridge, they are however, separate structures.7 We were unable to find a similar connection between the obliquus capitis superior and the dura mater.7 To examine the prevalence of these structures, T-2 weighted magnetic resonance imaging (MRI) of the atlanto-axial interspace of 240 individuals was performed in 2012 by Scali et, al.8 Sixty four percent of the MRI’s reviewed demonstrated a posterior concavity of the cervical dura mater consistent with a ligament attachment site.8 Of this group, 24% also had oblique, linear hypointense fibers which appeared to attach to the cervical dura mater.8 The breadth of studies which have examined these soft tissue dural connections, precludes them being considered variations of normal anatomy.1–8,11–13,27
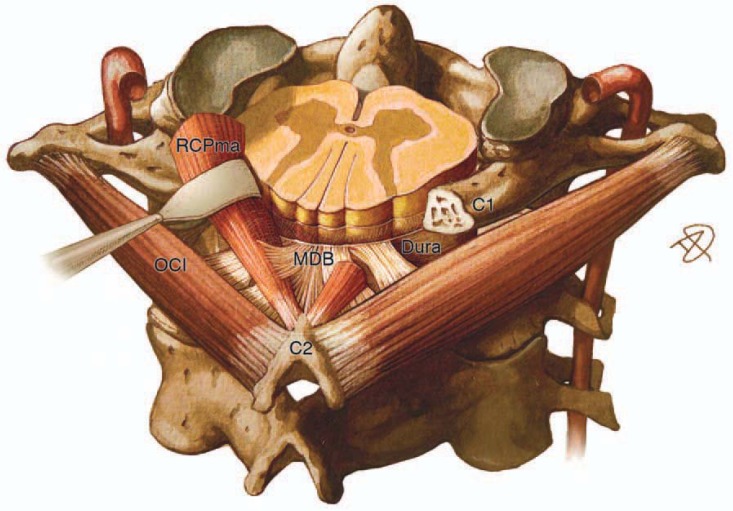
Figure 2.
A myodural bridge (MDB) extending from the anterior fascia of the rectus capitis posterior major (RCPma) and obliquus capitis inferior (OCI) muscles, attaching on the cervical dura mater. The myodural bridge (MDB) communicates with the posterior aspect of the cervical dura mater between the C1 and C2 vertebrae. Used with permission from: The Obliquis Capitis Inferior Myodural Bridge, Clin Anat 2013 26:450 45. Pontell M, Scali F, Marshall E, Enix D. (Original anatomical artwork by Danny Quirk)
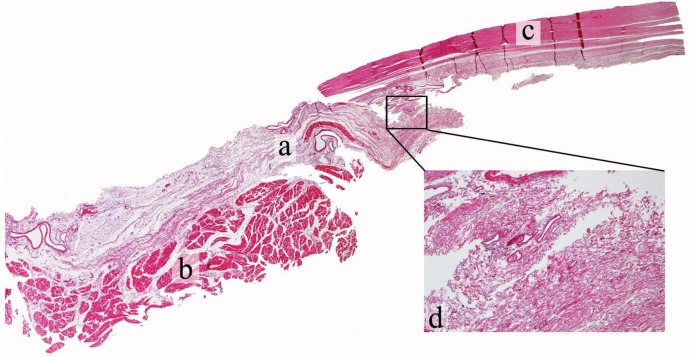
Figure 3.
Hematoxylin and eosin stained tissues of left side sagittal section showing the soft tissue communication (a) between the RCPma (b) and the cervical dura mater (c) in a male cadaveric specimen. The magnified area shows the soft tissue communication at the point of contact with the dura mater (d). Used with permission from: Histological Analysis of the Connection between the Rectus Capitis Posterior Major’s myodural bridge, The Spine Journal 13 (2013) 558–563., Scali F, Pontell M, Enix D, Marshall E.
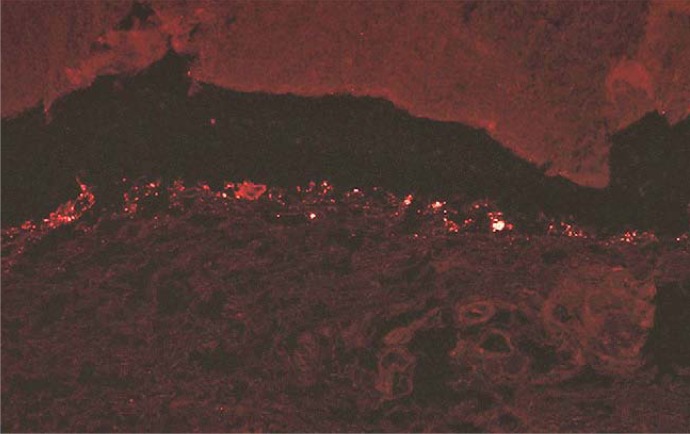
Figure 4.
Sagittal section of the myodural bridge between the rectus capitis posterior major and the cervical dura mater depicting positive fluorescence after staining with antineurofilament protein antibodies. Used with permission from: Histological Analysis of the Connection between the Rectus Capitis Posterior Major’s myodural bridge, The Spine Journal 13 (2013) 558–563., Scali F, Pontell M, Enix D, Marshall E.
In this article, we focus on the anatomical, functional significance, and clinical relevance of the RCPma and OCI myodural bridge. Consideration of its function as a passive and active stabilizer of the cervical spinal cord is discussed.
Anatomy of the suboccipital muscles
The RCPma and OCI muscles share a common innervation by the suboccipital nerve and some actions, with the RCPma acting to extend and slightly ipsilateral rotate the head and neck, while the OCI muscle ipsilaterally rotators the cervical spine.3,4,22 Cervical suboccipital muscles are richly innervated and contain relatively high muscle spindle content.18,21 Muscle spindle fibers found in the RCPma and OCI muscles are a source of primary afferents, representing major contributors to cervical spine neuro-muscular control.3,18,19,28,29 Consistent with their function of complex coordination and organization, high muscle spindle concentrations are typically found in smaller muscle groups responsible for fine motor skills.18,29,30 Kulkarni et al. documented the density of muscle spindles in fetal tissue per gram of muscle tissue.18 A large number of muscle spindles were noted in both the OCI and RCPma suboccipital muscles, with 242 and 98 spindles per gram of muscle tissue, compared to the trapezius and latissimus dorsi postural muscles with 2.2 and 1.4 muscle spindles per gram.18 Muscle spindles are typically more concentrated in regions richest in slow fibers, and while the OCI muscles have been reported as a blend of unevenly dispersed type I and II fibers, their muscle spindles are distributed disproportionately in the deep areas richest in slow twitch fibers.18,29 This unique configuration of muscle types suggests that these muscles may serve multiple functions including monitoring kinesthetic changes, maintaining constant force for eccentric head posture, and creating fast phasic movements when needed.18,29,31 An electromyographic examination showed the RCPmi to be under active contraction while the head is in an upright neutral position, with muscle activity increasing significantly during cervical retraction.32 The cervical muscles are subject to conversion from slow twitch to fast twitch muscles with injury.20,21 Alteration in muscle type, to a more glycogenic morphology creates a muscle prone to facilitation.21,31 This change can alter the discharge of primary afferents to the central nervous system effecting cervical neuromuscular control.19–21,31 Additionally, a loss of proprioceptive inhibition of nociceptors at the dorsal horn of the spinal cord can result in chronic pain.3,25
Clinical implications
The spinal canals’ midsagittal diameter of 10 mm which increases with flexion and decreases with extension, can impact the patency of the cervical cord.22,25 In a study of 19 cadaveric specimens by Hong et. al., showed significant differences in dural thickness between different levels in the thoracic and lumbar spines, with the dura slightly thicker in men than women.33 Buckling of cervical ligaments and dura mater have been reported with cervical spine extension.22–25,34 Cervical extension can create infolding of the ligamentum flavuum, which encroaches upon the cord.30 It is the elastin fibers found in the in the ligamentum flavuum that function to inhibit this inward buckling of the ligament into the spinal cord.22,24,34,35 The dura mater, which is densely populated with nociceptors, also contains elastin fibers which are oriented in such a way as to resist the load placed on them.34,35 The strain on the posterior side being greater than on the anterior side.25,34,35 Our recent histological analysis of cervical dura elastin fibers in eight cadaveric specimens, confirms that elastin density changes from caudal to cranial as well as the orientation of fibers which run parallel and perpendicular to each other. Cervical extension may therefore also cause inward buckling of the dura itself, compromising the dorsal subarachnoid space.31,34,36 In a prospective analysis of fifty patients receiving cervical injections under myelography; six percent demonstrated dural infolding on cervical extension, narrowing the posterior subarachnoid space.36 Traumatic and iatrogenic tears to the cervical dura can effect up to 36% of cervical spine injuries.23 Inflammation of the meninges, subdural hematomas, epidural infections, and nerve root compression and postural headaches are all the sequel of cerebral spinal fluid leaks with dural tears.23,25 Meningeal vascular irritation can also cause hypertonicity of the posterior neck muscles, resulting in permanent tension on the dura, stimulating nociceptive dural fibers.23,26,37 Considering the close proximity of the leptomeninges to the dura mater, a system to maintain the integrity of the subarachnoid space and, cerebrospinal fluid flow may exist.14,15,25,28 Similar to the denticulate ligaments which secure the spinal cord within the subarachnoid space, the myodural bridge crosses the epidural space to anchor the spinal dura during head and neck motion.4,6,10,23,25,28
Neuromuscular stabilization of the spinal cord
Contraction of the RCPma, RCPmi, and OCI sub-occipital muscles which puts the myodural bridge under tension, transmitting forces across it to place the dura under tension and stabilize the spinal cord.4,6,26,38,39 In addition to active contraction, the suboccipital muscles respond reflexively to involuntary and unanticipated movements of the head and neck.20,25 Modulation of dural tension may also be initiated via a sensory reflex to muscular contractile tissues.5,7 Central nuclei that exert control over the deep suboccipital muscles, including the RCPma, RCPmi and OCI muscles could respond reflexively as a feedback control of dural tension.5,7,25,28 Like many systems involving a feedforward or feedback mechanism of control, dural tension regulated through muscular contraction of suboccipital muscles is dependent on internal and external factors affecting those systems.4,6,28,31 The regulation of tension across the myodural bridge as a spinal cord stabilizer may prevent dural infolding, reducing stimulation of nociceptive pain mechanisms.5,7,39 Hypertrophy of suboccipital muscles or a failure of this system to maintain constant tension, may result in clinical manifestations arising from increased dural tension.1,4,6,9,20
Discussion
Functional anatomy of the myodural bridges
Many authors have speculated on the functional significance of the myodural bridge, generally attributing a mechanical advantage to it in stabilizing the spinal cord from dural enfolding.1–13 The reflexive myotatic response of suboccipital muscles has been proposed by several authors as a likely mechanism to place the dura under tension.4–9,38,39 In a study of 20 cadavers, Nakagawa reported that cervical cephalocaudal stresses may be due to the parallel orientation of elastin fibers in the dura and concluded its function was to resist hyperextension and compressive infolding of the dura.34 Hack suggested that the purpose of the RCPmi myodural bridge might be to assist in resisting dural infolding, previously noted by Burt.2,36 Shinomiya et. al., concluded that the role of the posterior cervical epidural ligaments is to provide an anchor to stabilize the dura mater from anterior translation during flexion.10 Without a posterior epidural attachment, the dural canal can shift anteriorly compressing the spinal cord causing flexion myelopathy.10 Rutten reported on high muscle spindle content in the RCPmi, postulating that the myodural bridges function may to monitor stresses on the cervical dura mater, reflexively preventing infolding.24 They reported that tissue injury from cervical whiplash could affect mechanoreceptive properties, causing the monitoring system that maintains dural tension to fail.21,24,31 Alix & Bates also discussed the duras tendency to fold inward on the spinal cord, and the myodural bridges ability to resist this movement.9 McPartland and Brodeur proposed that the RCPmi plays a role in preventing dural crimping when the head is extended or moved backward, inhibiting normal circulation of cerebrospinal fluid.38 Humphries reported on previous studies describing the primary mechanical function of the RCPmi to resist dural buckling during cervical extension, preventing damage to the spinal cord.13 In a case report describing an anatomical variation of the suboccipital muscles, Tagil also noted that the spinal cord is believed to be protected by the dense connective tissue that links the suboccipital muscles to the cervical dura mater.3 Kahkeshani and Ward indicated that a direct connection linking the musculoskeletal system to the dura mater provides a mechanical explanation for the efficacy of cervical massage and manipulative treatment for headaches.27
Along with the description of the RCPma myodural bridge by Scali et al., we proposed that modulation of cervical dural tension may include factors other than a myotatic reflex.4,5 Myodural biofeedback may play a role in maintaining the integrity of the subarachnoid space.4,5 We noted during dissection that manual traction applied to the RCPma caused movement of the spinal root within several levels.4 Due to its larger cross sectional area, the rectus capitis posterior major myodural bridge may exert greater mechanical traction on the dura than the rectus capitis posterior minor.4 We described another soft tissue connection traversing the epidural space between the OCI muscle fascia and the posterior sleeve of the dura mater in a paper by Pontell et al.6 It was reported that the OCI myodural connections function dynamically to prevent dural infolding during cervical extension, similar to the RCPmi and RCPma bridges.6,7
We agree with previous authors who describe a stabilizing function of the RCPmi muscle myodural bridge and propose a similar role for the RCPma and OCI muscle myodural bridges. In addition to the passive anchoring of the dura described by Nakagawa, Hack, Humphries, and Shinomiya, a myo-reflexive response described by Rutten provides an active stabilizing component.2,7,10,13,19,34,28,34 Besides the reflexive myotatic response of the suboccipital muscles, the presence of neuronal fibers in these tissues, may suggest functions other than the passive anchoring of these muscles to the posterolateral dura mater.5,7
The clinical relevance of these soft tissue connections to dural generated pain mechanisms, cervicocephalic headaches, subarachnoid space and cord impingement make this an area of great interest.9,13–17,20,39 The anatomical and histological evidence of these soft tissue communications bridging the epidural space from the RCPma and OCI muscles to the dura mater offers insight into the cervical spines’ complex function of neuromuscular control.5,7,18,39 Further examination of the tensile forces in the myodural bridge is needed. Biomechanical testing to confirm the tensile forces on these tissues currently in progress.
Conclusion
Anatomical soft tissue bridges which cross the cervical epidural space, connecting suboccipital muscle fascia and dura have passive and active functions to anchor the spinal cord. These myodural bridges may be involved in a dural tension monitoring system to prevent dural infolding and maintain patency of the spinal cord. Failure of this system could result in altered cerebral spinal fluid flow, changes in sensorimotor function, cervicocephalic headaches, and dural related pathologies.
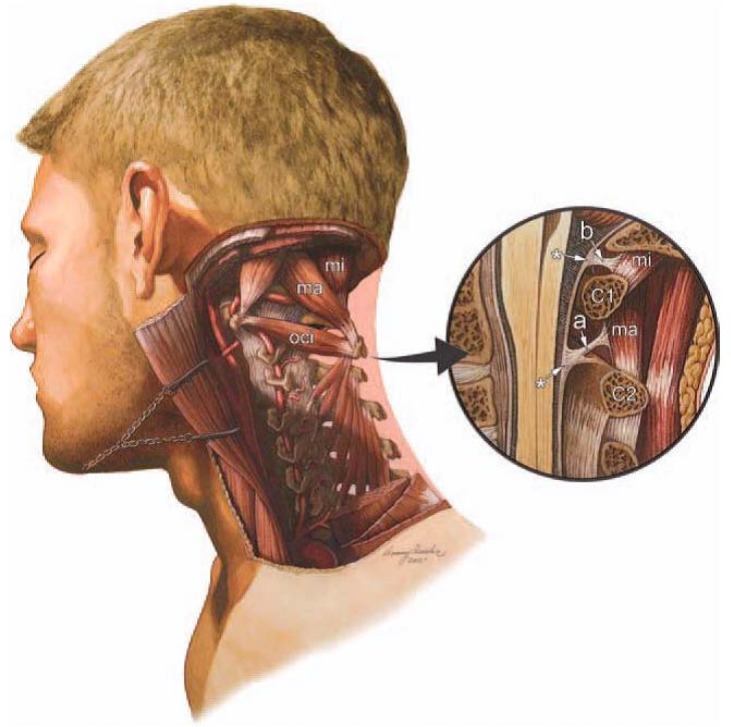
Figure 1.
Illustration of a dissection of the deep suboccipital region of the cervical spine. The rectus capitis posterior minor (RCPmi), rectus capitis posterior major (RCPma), and the obliquis capitis inferior (OCI) muscle fascia have communications with the dura mater via soft tissue. The encircled illustration (right) depicts a midsagittal dissection revealing the RCPma, RCPmi, and OCI muscles. The cervical myodural bridge (a) traverses the epidural space between the posterior elements of the C1 and C2 vertebrae. Both myodural structures link the suboccipital muscle fascia in to the cervical dura mater (*).Used with permission from: Magnetic resonance imaging investigation of the atlanto-axial interspace. Clin Anat. 2013 May; 26(4):444–9. Scali et al. (Original anatomical artwork by Frank Scali, D.C., and Danny Quirk)
Acknowledgments
The authors would like to thank Logan University graduate students Patrick Battaglia, and Robbyn Keating for assistance with cadaveric dissections and manuscript review and Dr. Jan Ryerse at the Research Microscopy Core in the Department of Pathology at Saint Louis University school of Medicine for preparation and interpretation of histological data and Danny Quirk for original illustrations.
Footnotes
Declaration: The authors have no financial associations, commercial associations or other possible conflicts of interest relevant to this study to disclose. Dr. Enix receives salary support from Logan University and partial funding support from HRSA grant # R18HP15125 and a grant from Standard Process corp.
References
- 1.Kahn JL, Sick H, Kortiké JG. Les espaces intervertébraux postérieurs de la jointure crânio-rachidienne. Acta Anat. 1992;144:65–70. [PubMed] [Google Scholar]
- 2.Hack GD, Kortizer RT, Robinson WL. Anatomic relation between the rectus capitis posterior minor muscle and the dura mater. Spine. 1995;20:2484–6. doi: 10.1097/00007632-199512000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Tagil SM, Ozçakar L, Bozkurt MC. Insight into understanding the anatomical and clinical aspects of supernumerary rectus capitis posterior muscles. Clin Anat. 2005;18:373–375. doi: 10.1002/ca.20106. [DOI] [PubMed] [Google Scholar]
- 4.Scali F, Marsili ES, Pontell ME. Anatomical connection between the rectus capitis posterior major and the dura mater. Spine. 2011;36:E1612–4. doi: 10.1097/BRS.0b013e31821129df. [DOI] [PubMed] [Google Scholar]
- 5.Scali F, Pontell ME, Enix DE, Marshall E. Histological analysis of the rectus capitis posterior major’s myodural bridge. The Spine Journal. 2013;13(5):558–563. doi: 10.1016/j.spinee.2013.01.015. [DOI] [PubMed] [Google Scholar]
- 6.Pontell ME, Scali F, Marshall E, Enix DE. The obliquus capitius, inferior myodural bridge. Clin Anat. 2013;26(4):450–4. doi: 10.1002/ca.22134. [DOI] [PubMed] [Google Scholar]
- 7.Pontell M, Scali F, Enix DE, Marshall E. Histological examination of the human obliquus capitis inferior myodural bridge. Annals Anatomy. 2013;195(6):522–26. doi: 10.1016/j.aanat.2013.04.013. [DOI] [PubMed] [Google Scholar]
- 8.Scali F, Pontell ME, Welk AB, Malmstrom TK, Marshall E, Kettner NW. Magnetic resonance imaging investigation of the atlanto-axial interspace. Clin Anat. 2013;26(4):444–9. doi: 10.1002/ca.22094. [DOI] [PubMed] [Google Scholar]
- 9.Alix ME, Bates DK. A proposed etiology of cervicogenic headache: the neurophysiologic basis and anatomic relationship between the dura mater and the rectus capitis posterior minor muscle. J Man Manip Ther. 1999;22:534–9. doi: 10.1016/S0161-4754(99)70006-0. [DOI] [PubMed] [Google Scholar]
- 10.Shinomiya K, Dawson J, Spengler DM, Konrad P, Blumenkopf B. An analysis of the posterior epidural ligament role on the cervical spinal cord. Spine. 1996;21:2081–8. doi: 10.1097/00007632-199609150-00005. [DOI] [PubMed] [Google Scholar]
- 11.Zumpano MP, Hartwell S, Jagos C. Soft tissue connection between rectus capitis posterior minor and the posterior atlanto-occipital membrane. Clin Anat. 2006;19:522–527. doi: 10.1002/ca.20220. [DOI] [PubMed] [Google Scholar]
- 12.Nash L, Nicholson H, Lee ASJ, Johnson G M, Zhang M. Configuration in the posterior atlanto-occipital interspace. Spine. 2005;30:1359–1366. doi: 10.1097/01.brs.0000166159.31329.92. [DOI] [PubMed] [Google Scholar]
- 13.Humphreys BK, Kenin S, Hubbard B, Cramer G. Investigation of connective tissue attachments to the cervical spinal dura mater. Clin Anat. 2003;16:484–493. doi: 10.1002/ca.10109. [DOI] [PubMed] [Google Scholar]
- 14.Bogduk N. Cervicogenic Headache: anatomic basis and pathophysiologic Mechanisms. Current Pain and Headache Reports. 2001;5:382–386. doi: 10.1007/s11916-001-0029-7. [DOI] [PubMed] [Google Scholar]
- 15.Haldeman S, Dagenais S. Cervicogenic headaches: a critical review. Spine J. 2001;1(1):31–46. doi: 10.1016/s1529-9430(01)00024-9. [DOI] [PubMed] [Google Scholar]
- 16.Fernandez-De-Las-Penas C. Clinical evaluation of cervicogenic headache: a clinical perspective. J Man Manip Ther. 2008;16:81. doi: 10.1179/106698108790818440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schoenen J, Fumal A. Tension-type headache: current research and clinical management. Lancet Neurology. 2008;7(1):70–83. doi: 10.1016/S1474-4422(07)70325-3. [DOI] [PubMed] [Google Scholar]
- 18.Kulkarni V, Chandy MJ, Babu KS. Quantitative study of muscle spindles in suboccipital muscles of human fetuses. Neurol India. 2001;49(4):355–9. [PubMed] [Google Scholar]
- 19.Palmgren PJ, Andreasson D, Eriksson M, Hägglund H. Cervicocephalic kinesthetic sensibility and postural balance in patients with nontraumatic chronic neck pain – a pilot study. Chiropractic & Osteopathy. 2009;17:6. doi: 10.1186/1746-1340-17-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rix GD, Bagust J. Cervicocephalic kinesthetic sensibility in patients with chronic, nontraumatic cervical spine pain. Arch Phys Med Rehabil. 2001;82:911–9. doi: 10.1053/apmr.2001.23300. [DOI] [PubMed] [Google Scholar]
- 21.Uhlig Y, Weber BR, Grob D, Muntener M. Fiber composition and fiber transformations in neck muscles with dysfunction of the cervical spine. J Orthop Res. 1995;13(2):240–9. doi: 10.1002/jor.1100130212. [DOI] [PubMed] [Google Scholar]
- 22.Cailliet R. Neck Arm Pain. 3rd edition. F. A. Davis Company; Jan, 1991. ISBN-10: 0803616104. [Google Scholar]
- 23.Lusczyk MJ, Blaisdell GY, Wiater B P, Bellabarba C, Chapman JR, Agel JA, Bransford RJ. Traumatic Dural Tears: what do we know and are they a problem? The Spine Journal. 2014;14(1):49–56. doi: 10.1016/j.spinee.2013.03.049. [DOI] [PubMed] [Google Scholar]
- 24.Rutten HP, Szpak K, van Mameren H, et al. Letter to Editor; response to Anatomic relation between the rectus capitis posterior minor muscle and the dura mater. Spine. 1997;22:924–8. doi: 10.1097/00007632-199704150-00018. [DOI] [PubMed] [Google Scholar]
- 25.Cramer GD, Darby SA. Clinical Anatomy of the Spine, Spinal Cord and ANS, 2e. 2 edition. Mosby Publishers; ISBN-10: 0323079547. [Google Scholar]
- 26.Hack GD, Hallgren RC. Chronic headache relief after section of suboccipital muscle dural connections: a case report. Headache. 2004;44:84–9. doi: 10.1111/j.1526-4610.2004.04015.x. [DOI] [PubMed] [Google Scholar]
- 27.Kahkeshani K, Ward PJ. Connection between the spinal dura mater and suboccipital musculature: Evidence for the myodural bridge and a route for its dissection – A review. Clin Anat. 2012;25(4):415–22. doi: 10.1002/ca.21261. [DOI] [PubMed] [Google Scholar]
- 28.Siegel A, Sapru HN. The spinal cord. In: Sun Betty., editor. Essential Neuroscience. 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 2011. pp. 150–60. [Google Scholar]
- 29.Richmond FJR, Singh K, Corneil BD. Marked nonuniformity of fiber-type composition in the primate suboccipital muscle obliquus capitis inferior. Exp Brain Res. 1999;125:14–18. doi: 10.1007/s002210050652. [DOI] [PubMed] [Google Scholar]
- 30.Farshadmanesh F, Chang P, Wang H, et al. Neck muscle synergies during stimulation and inactivation of the Interstitial Nucleus of Cajal (INC) J Neurophysiol. 2008;100:1677–1685. doi: 10.1152/jn.90363.2008. [DOI] [PubMed] [Google Scholar]
- 31.Korr IM. The physiological basis of osteopathic medicine. New York (Insight Publishing); 1982. [Google Scholar]
- 32.Hallgren RC, Pierce SJ, Prokop LL, Rowan JJ, Lee AS. Electromyographic activity of rectus capitis posterior minor muscles associated with voluntary retraction of the head. Spine J. 2014;14(1):104–12. doi: 10.1016/j.spinee.2013.06.011. [DOI] [PubMed] [Google Scholar]
- 33.Hong J, Suh SW, Park SY, Modi HN, Rhyu IJ, Kwon S, Yu H, Byun J. Analysis of dural sac thickness in human spine – cadaver study with confocal infrared laser microscope. The Spine Journal. 2011;11(12):1121–1127. doi: 10.1016/j.spinee.2011.11.001. [DOI] [PubMed] [Google Scholar]
- 34.Nakagawa H, Mikawa Y, Watanabe R. Elastin in the human posterior longitudinal ligament and spinal dura: A histologic and biochemical study. Spine. 1994;19(19):2164–2169. doi: 10.1097/00007632-199410000-00006. [DOI] [PubMed] [Google Scholar]
- 35.Mazgajczyk M, Scigala K, Czy M. Mechanical properties of cervical dura mater. Acta Bioeng Biomech. 2013;14:1. [PubMed] [Google Scholar]
- 36.Burt TB, Seeger JF, Carmody RF, Yang PJ. Dural infolding during C1–2 myelography. Radiology. 1986;158(2):546–7. doi: 10.1148/radiology.158.2.3753627. [DOI] [PubMed] [Google Scholar]
- 37.Hu JW, Vernon H, Tatourian I. Changes in neck electromyography associated with meningeal noxious stimulation. J Manipulative Physiol Ther. 1995 Nov-Dec;18(9):577–81. [PubMed] [Google Scholar]
- 38.McPartland JM, Brodeur RR. Rectus capitis posterior minor: a small but important suboccipital muscle. J Bodywork Movement Therapies. 1999;3(1):30–35. [Google Scholar]
- 39.Grgic V. Cervicogenic headache: etiopathogenesis, characteristics, diagnosis, differential diagnosis and therapy. Lijec Vjesn. 2007;129:230–236. [PubMed] [Google Scholar]