SUMMARY
The use of a stapler for pharyngeal closure during total laryngectomy was first described in 1971. It provides rapid watertight closure without surgical field contamination. The objective of our study was to compare the incidence of pharyngocutaneous fistula after total laryngectomy with manual and mechanical closures of the pharynx. This was a non-randomised, prospective clinical study conducted at two tertiary medical centres from 1996 to 2011 including consecutive patients with laryngeal tumours who underwent total laryngectomy. We compared the incidence of pharyngocutaneous fistula between two groups of patients: in 20 patients, 75 mm linear stapler closure was applied, whereas in 67 patients a manual suture was used. Clinical data were compared between groups. The groups were statistically similar in terms of gender, age, diabetes mellitus, smoking and alcohol consumption and tumour site. The group of patients who underwent stapler-assisted pharyngeal closure had a higher number of patients with previous tracheotomy (p < 0.001) and previous chemoradiation (p < 0.001). The incidence of pharyngocutaneous fistula was 30% in the mechanical closure group and 20.9% in the manual suture group (p = 0.42). In conclusion the use of the stapler does not increase the rate of fistulae.
KEY WORDS: Surgical staplers, Suture techniques, Cutaneous fistula, Laryngectomy, Laryngeal neoplasms, Carcinoma, Squamous cell
RIASSUNTO
L'uso della suturatrice meccanica Stapler per la chiusura del faringe durante la laringectomia totale è stato descritto per la prima volta nel 1971. Questa tecnica consente una rapida chiusura a buona tenuta senza contaminazione del campo operatorio. L'obiettivo del nostro studio è stato quello di confrontare l'incidenza di fistola faringo cutanea dopo laringectomia totale con chiusura manuale o meccanica del faringe. Questo studio clinico non randomizzato prospettico è stato realizzato arruolando pazienti consecutivi dal 1996 al 2011 affetti da tumore della laringe e candidati a laringectomia totale. Abbiamo confrontato l'incidenza di Fistola faringo cutanea fra due gruppi: nel primo gruppo di 20 pazienti la chiusura del faringe è stata realizzata mediante una suturatrice meccanica di 75 mm "Linear stapler", mentre nel secondo gruppo di 67 pazienti la chiusura era stata realizzata manualmente. I gruppi erano statisticamente sovrapponibili in termini di sesso, età media, prevalenza di fattori di rischio quali diabete mellito, fumo, dimensioni del tumore e assunzione di alchool. Nel gruppo di pazienti in cui la chiusura del faringe è stata realizzata con suturatrice meccanica, tuttavia, era più alto il numero di pazienti sottoposti precedentemente a tracheotomia (p < 0,001) e radio chemioterapia (p < 0,001). L'incidenza di Fistola faringocutanea nella nostra casistica era del 30% nei pazienti in cui la chiusura del faringe era stata realizzata con suturatrice meccanica e del 20,9% nei pazienti in cui la sutura era stata realizzata manualmente. Dal punto di vista statistico questa differenza non era significativa (p = 0,42). In conclusione l'uso della suturatrice meccanica stapler non aumenta il tasso di incidenza di Fistola faringo cutanea dopo laringectomia totale.
Introduction
Pharyngocutaneous fistula is the most common surgical complication after total laryngectomy. It is associated to a higher incidence of morbidity, hospitalisation and costs 1 2.
Although a stapler has only recently been used for pharynx closure, it has been widely applied in gastrointestinal surgeries. The use of a stapler during the resection of Zenker diverticula was described for the first time in 1969 3.
The use of a stapler for pharyngeal closure after total laryngectomy seems to be adequate for endolaryngeal tumours 1. It was first described in 1973 4. The closure is watertight and the contamination of the surgical field by secretions from mouth and pharynx decreases. As a result, the occurrence of pharyngocutaneous fistula is minimised, even in recurrent cases after radiation therapy 5. Furthermore, pharynx closure is faster 6-9.
In spite of being a relatively simple technique with potential advantages, there is a lack of comparative studies available in the literature. Our objective was to evaluate the incidence of pharyngocutaneous fistula after total laryngectomy comparing manual and mechanical closures of the pharynx in patients with laryngeal cancer.
Materials and methods
This survey was approved by the board of the hospitals were it was performed.
This non-randomised prospective study included consecutive patients with laryngeal squamous cell carcinoma who underwent total laryngectomy with curative intent in two tertiary reference hospitals from 1996 to 2011. The patients were operated on by the same surgical team.
Patients with hypopharyngeal carcinoma, extralaryngeal tumours or tumours involving the base of the tongue were excluded from the stapler group. However, T4a patients with only invasion of the thyroid cartilage were eligible for stapler use, since this invasion is external to the laryngeal frame and the oncological margins can be clearly verified independently of the type of pharyngeal closure employed. In the control group, patients with tension in the suture line not eligible for primary closure were excluded. Tumours were staged according to the TNM staging system adopted by AJCC and UICC.
These two groups were compared according to gender, age at the time of the operation, diabetes mellitus, smoke and alcohol habits, primary site of the lesion, previous tracheotomy, previous treatment (in case of salvage surgery), operation time, neck dissection and the development of pharyngocutaneous fistula. Clinical characteristics are presented in Table I.
Table I.
Clinical data of patients (n = 87).
| Mechanical suture (n = 20) | Manual suture (n = 67) | p | |
|---|---|---|---|
| Gender (M/F) | 19/1 | 61/6 | 0.51 |
| Age (years) | 62.0 ± 11.1 | 62.0 ± 11.2 | 1.00 |
| Diabetes mellitus | 1/20 | 3/67 | 1.00 |
| Smoking | 19/20 | 65/67 | 1.00 |
| Alcohol assumption | |||
| Clinical staging | |||
| T2 | 4 | 3 | < 0.001 |
| T3 | 12 | 46 | 0.01 |
| T4a | 4 | 18 | 0.05 |
| Primary tumour site | 1.00 | ||
| Supraglottic | 3 | 10 | |
| Glottic | 17 | 57 | |
| Hypoglottic | 0 | 0 | |
| Previous tracheotomy | 13 | 17 | < 0.001 |
| Previous radiation therapy | 15 | 15 | < 0.001 |
| Neck dissection | |||
| No | 3 | 3 | 0.003 |
| Unilateral selective | 2 | 2 | 0.04 |
| Bilateral selective | 12 | 12 | < 0.001 |
| Unilateral radical | 1 | 9 | 0.02 |
| Bilateral radical | 2 | 41 | < 0.001 |
There were 30 cases of residual or recurrent laryngeal tumours after organ preservation protocol, with radiation therapy doses between 6,000 and 7,020 cGy and weekly cisplatin 40 mg/m2. The radiation therapy was interrupted at 5,040 cGy due to tumour increasing. The time between detection of therapeutic failure and salvage surgery varied from 4 weeks to 7 months. Previous chemoradiation organ sparing treatment was not employed in any patient.
Technical aspects
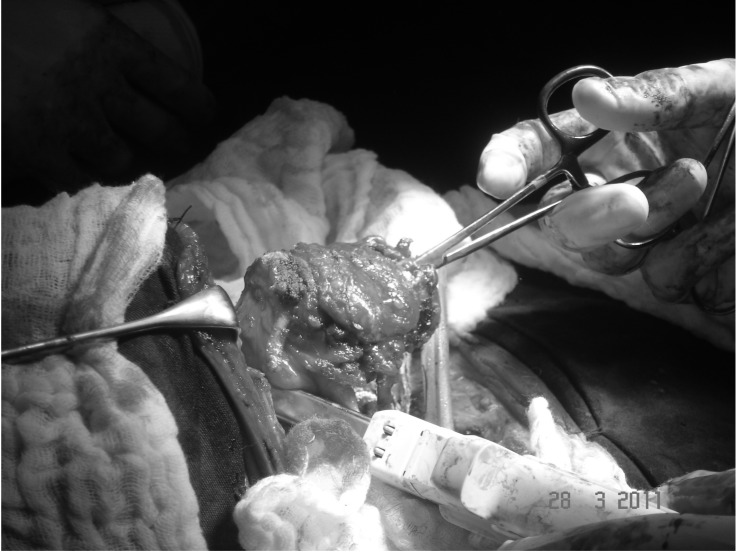
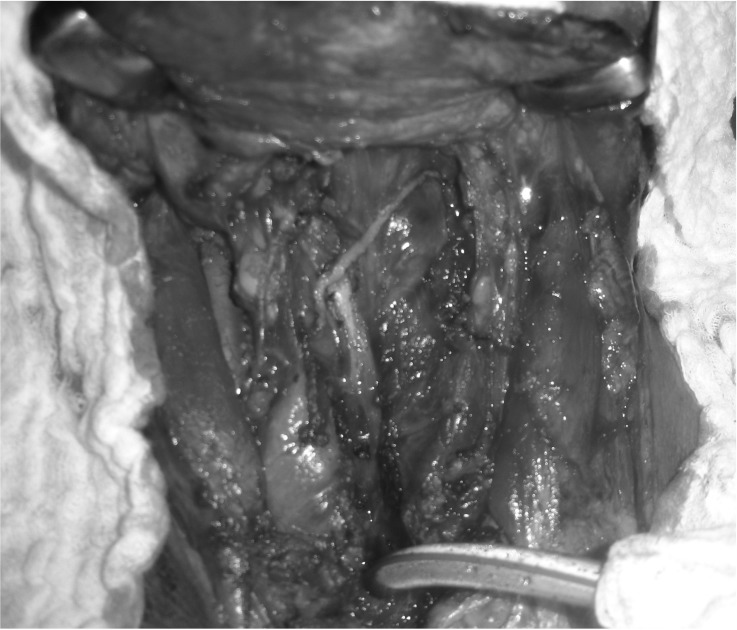
Patients received prophylactic antibiotics (clindamycin associated with amikacin) up to 24 hours postoperative, with the first dose during anaesthetic induction. After general anaesthesia with endotracheal intubation, tracheotomy was performed. Thus, direct microlaryngocsopy was performed in order to verify the tumour stage. Unior bilateral neck dissection was performed according to tumour extension and lymph node involvement with preservation of the XII nerve whenever possible. For facilitating the placement of the stapler, the pyriform sinuses and internal perichondrium of the thyroid cartilage were dissected from the lateral aspect of its lamina and the superior cornu of the thyroid cartilage, and the great cornus of the hyoid bone were cut. The epiglottic free border was pulled into the endolarynx using an Allis clamp. Thus, a 75 mm linear stapler TCL75 Ethicon® was longitudinally applied at the vallecula level, as close as possible to the thyroid cartilage lamina (Fig. 1,). The double-staggered row was established by stapler activation, splitting the pharynx (closed) from the laryngeal specimen (Fig. 2). A secondary tracheo-oesophageal puncture was performed in all cases 3 months after surgery for vocal rehabilitation.
Fig. 1.
The stapler is put in place as close as possible to the thyroid cartilage lamina so as to preserve the maximum mucous by the pyriform sinuses.
Fig. 2.
The double-staggered row is established by stapler activation, splitting the pharynx from the laryngeal specimen.
All patients were discharged from the 4th to the 7th postoperative day. In patients without any fistulas, oral feeding was started on the 10th postoperative day at the time of the nasogastric tube removal.
Statistical analysis
A p value of less than 0.05 was considered statistically significant. Univariate analysis was evaluated by χ2 test at a confidence interval of 95%.
Results
Eighty-seven patients who underwent total laryngectomy due to laryngeal squamous cell carcinoma were included in the study. Eighty patients were men (91.9%) and the age varied from 36 to 89 years, with average of 62.0 ± 11.2. The demographic and clinical characteristics of both groups are detailed in Table I.
There was no technical difficulty in the laryngeal preparation and stapler application. The groups were statistically similar in terms of gender, age, smoking and alcohol use and tumour site. Regarding the clinical staging of the primary site, there was a higher rate of patients of the stapler group staged as T2 and T3, whereas the rate of T4 tumours was higher in the manual suture group. T4 patients in the stapler group were in fact T4a patients with invasion of the thyroid cartilage only. Previous tracheotomy had been performed in 13 patients who underwent stapler closure (65%) and in 17 patients who underwent manual suture (25.4%; p < 0.001). Fifteen patients in the stapler group had undergone an organ preservation protocol (75%), whereas 15 patients in the manual closure group had undergone a similar approach (22.4%; p < 0.001). Regarding the neck approach, the majority of patients in the stapler group underwent bilateral selective neck dissection, whereas most of the other group underwent bilateral radical neck dissection.
The incidence of pharyngocutaneous fistula was 30% in the mechanical closure group and 20.9% in the manual suture group (p = 0.42).
Discussion
Pharyngocutaneous fistula is the most common complication encountered in the early postoperative period following total laryngectomy. Its incidence after head and neck surgery varies from 5% to 65% in the literature 1. It continues to occur with distressing frequency, causing a considerable increase in morbidity, and often necessitating a greatly prolonged hospital stay and further operative procedures 6.
The limits of the indication of stapler for pharyngeal closure regarding the extension of the primary tumour must be respected. It should be confirmed by previous suspension laryngoscopy performed in the operating room 1. The stapler is a reliable method if the limits of its indication regarding the primary tumour are considered 1 10-13. It is recommended that the procedure is reserved to cases in which, based on meticulous preoperative assessment with endoscopy and imaging, the endolaryngeal site of the tumour has been assessed 14 15. It should be considered that the tumour is not usually visualised during the resection, and a closed technique if applied improperly would compromise the oncological potential of the surgery, since it should be performed only for endolaryngeal tumours 7.
A selection bias derives from the inclusion of patients with hypopharyngeal, oropharyngeal or extralaryngeal extension in the control group (manual suture). In fact, these patients are prone to have a wider pharyngeal resection in order to assure safe oncological margins. It could be considered one important factor for developing a pharyngo- cutaneous fistula. However, patients with tension in the suture line and at an increased risk of fistula did not undergo primary closure and, as a result, were excluded from this study.
Some technical aspects should be observed. During performance of closed techniques, in some cases, it is difficult to keep the suprahyoid part of the epiglottis outside the jaws of the stapler. It has been suggested to introduce a hook or an Allis clamp into the laryngeal lumen through the trachea and, after taking the apex of the epiglottis, retract it towards the lumen, which we routinely perform. Another option is transforming the closed technique into a "semi-closed" one by creating a small opening in the mucosa of the vallecula epiglottica, through which the epiglottis can be extracted. As the linear stapler closure is performed, the second surgeon must take care to keep the edges of such mini-pharyngotomy well above the jaws of the stapler. As this opening is small, the operating field is not contaminated by pharyngeal secretions 15.
Although the pharyngeal constrictor muscles have been considered as a sophisticated "neuromuscular compartimentalisation" 16 and many surgeons advocate a second layer closure of the constrictor muscles, this has been considered unnecessary with no change in fistula rates 17.
Favourable outcome, which includes a tension-free suture line, watertight closure of the pharynx and haemostasis with preserved viability of the mucosa, support stapler closure of the pharynx. At the end of the procedure, double- staggered rows of staples remain in the pharynx and laryngeal specimen, and minimise the risk of contamination of the surgical field by pharyngeal secretions 1 13.
The absence of pyriform sinuses, aryepiglottic and glossoepiglottic folds and vallecula involvement allow that there is no excessive resection of hypopharyngeal mucosa 5. In our study, patients staged like this were not eligible to the stapler group and constitutes a selection bias.
The material applied on the mechanical suture has an excellent tolerance by tissues because of minimum inflammatory reaction. The absence of tissue necrosis was the main differential element between manual and mechanical sutures. In the former, necrosis is nearly inevitable, due to repeated aggression by clamps through ischaemia by surgical knots and frequent inclusion of mucosa in the suture line 5.
Although preoperative tracheotomy has been suggested a local risk factor, the majority of researchers found no significant relationship between preoperative tracheotomy and pharyngocutaneous fistula development 1 2.
Although organ preservation therapy increases the risk of fistula, there are other factors that affect their development, including the clinical and laboratory parameters of the patient, extent of the surgery, surgical technique, surgeon's expertise and postoperative care 1. In the largest retrospective series with 1,415 patients undergoing total laryngectomy with mechanical closure of the pharynx, the rate of pharyngocutaneous fistula was 11.9%. The incidence among non-irradiated patients was 5%. After salvage surgery, the fistula incidence was 19.4% among patients irradiated up to 6,000-6,500 cGy, showing a greater possibility of fistula with progressively higher doses of radiation therapy 17. In a retrospective analysis of 268 patients who underwent total laryngectomy, pharyngocutaneous fistula was found in 43 patients (16%). Predisposing factors for fistula included previous radiotherapy, supraglottic primary site and concurrent radical neck dissection. Among the 43 patients who developed fistula, 41.8% had previously undergone radiotherapy (p < 0.05) 18. In our series, there were 15 patients who underwent previous chemoradiation therapy in each group. Thus, in spite of a higher rate of such patients in the stapler group (p < 0.001), there was not a significantly increased risk for pharyngocutaneous fistula (p = 0.42).
In a series of 10 consecutive patients treated with staplerassisted laryngectomy, primary tracheoesophageal prosthesis was applied at the time of the initial surgery under direct visualisation using a flexible esophagoscope without disrupting the stapler closure. All patients achieved alaryngeal speech and there were no complications 19. We prefer applying this prosthesis in a secondary fashion, 3 months after the surgery.
The surgical length was decreased by an average of 43 minutes in the mechanical suture group compared to the manual closure group 9. Data regarding the surgical time in the first operations was not available. Nonetheless, such an improvement in surgical time is clear.
In our study, the incidence of pharyngocutaneous fistula was 30% in the mechanical closure group and 20.9% in the manual suture group. However, this difference was not statistically significant (p = 0.42). We did not randomise this study because there was some difficulty in achieving extensive use of the stapler device in the beginning of the study, since it was usually applied only in gastrointestinal surgeries.
Our group of patients who underwent stapler-assisted pharyngeal closure had a higher number of patients with previous tracheotomy (p < 0.001) and previous chemoradiation therapy (p < 0.001). Even so, this procedure did no increase the rate of fistula (p = 0.42). The advantages of mechanical sutures are simple and fast application, watertight suture, prevention of field contamination, good speech and swallowing, without increasing the rate of pharyngocutaneous fistula. In spite of the cost of the stapler device, operating room expenses may also be reduced due to the decrease in operating time.
Conclusions
The use of a stapler does not increase the rate of pharyngocutaneous fistulae.
References
- 1.Calli C, Pinar E, Oncel S. Pharyngocutaneous fistula after total laryngectomy: Less common with mechanical stapler closure. Ann Otol Rhinol Laryngol. 2011;120:339–344. doi: 10.1177/000348941112000510. [DOI] [PubMed] [Google Scholar]
- 2.Dedivitis RA, Ribeiro KC, Castro MA, et al. Pharyngocutaneous fistula following total laryngectomy. Acta Otorhinolaryngol Ital. 2007;27:2–5. [PMC free article] [PubMed] [Google Scholar]
- 3.Hoehn JG, Payne WS. Resection of pharyngoesophageal diverticulum using stapling device. Mayo Clin Proc. 1969;44:738–741. [PubMed] [Google Scholar]
- 4.Lukyanchenko AG, Knowles JEA. Suturing of a laryngeal defect in laryngectomy. Vestn Otorhinolaringol. 1973;33:29–30. [Google Scholar]
- 5.Gonçalves AJ, Souza JA, Menezes MB, et al. Pharyngocutaneous fistulae following total laryngectomy comparison between manual and mechanical sutures. Eur Arch Otorhinolaryngol. 2009;266:1793–1798. doi: 10.1007/s00405-009-0945-4. [DOI] [PubMed] [Google Scholar]
- 6.Westmore GA, Knowles JE. The use of a stapling instrument for postlaryngectomy pharyngeal repair. J Laryngol Otol. 1983;97:775–778. doi: 10.1017/s0022215100094974. [DOI] [PubMed] [Google Scholar]
- 7.Agrawai A, Schller DE. Closed laryngectomy using the automatic linear stapling device. Laryngoscope. 2000;110:1402–1405. doi: 10.1097/00005537-200008000-00034. [DOI] [PubMed] [Google Scholar]
- 8.Dedivitis RA, Guimarães AV. Uso do grampeador para o fechamento da faringe após laringectomia total. Acta Cir Bras. 2004;19:66–69. [Google Scholar]
- 9.Santaolalla Montoya F, Ruiz de Galarreta JC, Sánchez del Rey A, et al. Estudio comparativo entre el empleo de la sutura manual y la sutura mecánica en el cierre del defecto mucoso en la laringectomía total. Acta Otorrinolaringol Esp. 2002;53:343–350. doi: 10.1016/s0001-6519(02)78319-2. [DOI] [PubMed] [Google Scholar]
- 10.Sessions RB, Shemen LJ, Reuter VE. Staple closure of the gullet after laryngectomy: an experimental study. Otolaryngol Head Neck Surg. 1986;95:491–499. doi: 10.1177/019459988609500413. [DOI] [PubMed] [Google Scholar]
- 11.Talmi YP, Finkelstein Y, Gal R, et al. Use of a linear stapler for postlaryngectomy pharyngeal repair: a preliminary report. Laryngoscope. 1990;100:552–555. doi: 10.1288/00005537-199005000-00021. [DOI] [PubMed] [Google Scholar]
- 12.Sofferman RA, Voronetsky I. Use of the linear stapler for pharyngoesophageal closure after total laryngectomy. Laryngoscope. 2000;110:1406–1409. doi: 10.1097/00005537-200008000-00035. [DOI] [PubMed] [Google Scholar]
- 13.Ahsan F, Ah-See KW, Hussain A. Stapled closed technique for laryngectomy and pharyngeal repair. J Laryngol Otol. 2008;122:1245–1248. doi: 10.1017/S0022215108003228. [DOI] [PubMed] [Google Scholar]
- 14.Simoncelli C, Altissimi G. Sutura meccanica della faringe in corso di laringectomia totale: proposta di una tecnica chiusa. Acta Otorhinolaryngol Ital. 1990;10:465–474. [PubMed] [Google Scholar]
- 15.Altissimi G, Frenguelli A. Linear stapler closure of the pharynx during total laryngectomy: a 15-year experience (from closed technique to semi-closed technique) Acta Otorhinolaryngol Ital. 2007;27:118–122. [PMC free article] [PubMed] [Google Scholar]
- 16.Cunsolo EM. Anatomy and physiology of the operated larynx. Acta Otorhinolaryngol Ital. 2010;30:238–243. [PMC free article] [PubMed] [Google Scholar]
- 17.Bedrin L, Ginsburg G, Horowitz Z, et al. 25-year experience of using a linear stapler in laryngectomy. Head Neck. 2005;27:1073–1079. doi: 10.1002/hed.20280. [DOI] [PubMed] [Google Scholar]
- 18.Galli J, Corso E, Volante M, et al. Postlaryngectomy pharyngocutaneous fistula: incidence, predisposing factors, and therapy. Otolaryngol Head Neck Surg. 2005;133:689–694. doi: 10.1016/j.otohns.2005.07.025. [DOI] [PubMed] [Google Scholar]
- 19.Leahy KP, Tufano RP. Primary tracheoesophageal puncture in stapler-assisted total laryngectomy. ORL J Otorhinolaryngol Relat Spec. 2010;72:124–126. doi: 10.1159/000278257. [DOI] [PubMed] [Google Scholar]