Abstract
A 65-year-old woman was referred with hypercalcaemia and found to have a four cm retrotracheal mass on CT. The patient also suffered from neurofibromatosis and a recently diagnosed gastric mass. Tc99 sestamibi scintigraphy revealed an area of intense uptake in the right upper mediastinum. Endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) was used to confirm the diagnosis of parathyroid adenoma and thoracoscopic resection was subsequently performed. EBUS-TBNA biopsy can be a helpful diagnostic tool to confirm diagnosis of mediastinal parathyroid masses in patients with atypical or complex clinical presentations.
Background
Primary hyperparathyroidism is a leading cause of hypercalcaemia. In around 85% of cases this is due to a parathyroid adenoma necessitating surgical excision. In a small percentage of patients parathyroid adenomas are deeply embedded in the mediastinum.1 Although Tc99 sestamibi scintigraphy scans are a useful tool to diagnose and locate mediastinal parathyroid adenomas, some complex clinical scenarios may warrant further investigations preoperatively to confirm the diagnosis. We present a case where endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) proved useful to confirm the diagnosis of a large parathyroid adenoma, which was then excised by a video-assisted thoracoscopy (VATS) approach.
Case presentation
A 65-year-old woman was referred for surgical excision of a mediastinal parathyroid adenoma. The diagnosis of hyperparathyroidism was established previously with an elevated calcium level of 3.68 mmol/L (normal range: 2.0–2.6 mmol/L), normal parathyroid hormone levels and a well-defined retrotracheal mass measuring 4cm×3cm×2 cm on CT (figure 1). Tc99 sestamibi scintigraphy showed focal intense uptake in the upper right side of the mediastinum. The patient's medical history also included a diagnosis of type 1 neurofibromatosis and a recent upper gastrointestinal bleeding investigated by endoscopy and biopsy of an antral gastric mass that proved to be benign.
Figure 1.

CT thorax showing a right paratracheal mass (arrow).
Investigations
Further characterisation of the mass was deemed necessary due to its size to differentiate between a parathyroid carcinoma and an enlarged lymph node. Owing to appreciable differences in management, surgical versus non-surgical ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) was performed as a means of obtaining a histopathological diagnosis (figure 2). The features of the biopsy specimen were consistent with a parathyroid adenoma.
Figure 2.
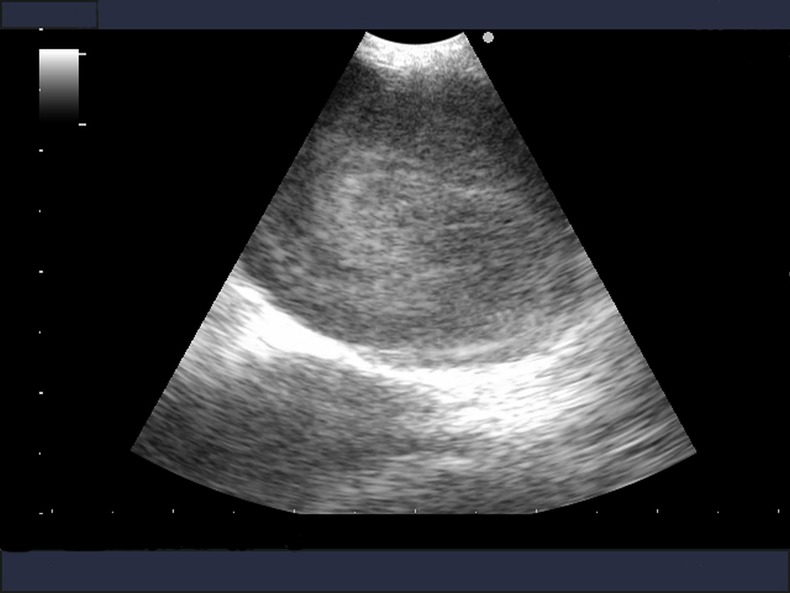
Endobronchial ultrasound of right paratracheal mass.
Treatment
The patient underwent surgical resection of the mediastinal tumour by VATS and positioned in a right lateral decubitus position. A camera port was placed in the right mid-axillary line in approximately the eighth intercostal space and two further ports were placed in the right anterior and posterior axillary lines. A brown mass was visualised superiorly in the tracheo-oesophageal groove and the overlying pleura were divided using a LigaSure (Covidien Ltd). The mass was dissected free with the feeding vessel divided with the LigaSure superiorly.
Outcome and follow-up
The procedure was uneventful and the patient was discharged on the fourth postoperative day without complications. Prior to discharge calcium levels had normalised to 2.2 mmol/L. The histology report confirmed the diagnosis of a fully excised parathyroid adenoma.
Discussion
Ectopic mediastinal parathyroid tissue is found in 11–25% of patients presenting with primary hyperparathyroidism.2 It is more common for the inferior parathyroid gland to have an ectopic location in the anterior mediastinum. Ectopic superior parathyroid glands, as in this case, are rare and usually located in the tracheo-oesophageal groove. Such lesions are approximately 1 cm in diameter and can be identified and localised using a combination of CT and Tc99 sestamibi scintigraphy. Although highly reliable, in most instances, concerns about the diagnosis may remain after this diagnostic strategy. The sensitivity and positive predicted value of Tc99 sestamibi scintigraphy have been reported by the current literature at 78.9% and 90.7% respectively.3 Owing to the size of the lesion there were concerns about the possible diagnosis in this case.
Given their anatomical location, some of these mediastinal parathyroid adenomas may be amenable to histopathological confirmation of the diagnosis by EBUS-TBNA. Beyond its well-established role in staging mediastinal lymph nodes in lung cancer, EBUS-TBNA is also proving useful in the diagnosis of other mediastinal lesions. Yasufuku et al4 recently reported 140 patients with various mediastinal pathologies in which diagnosis was established by EBUS-TBNA. Their report, however, did not include any parathyroid pathology. In the current case, the findings were most consistent with a parathyroid adenoma, which was confirmed after complete surgical VATS resection. Needle aspiration with parathyroid hormone concentration assay may be a useful method of confirming the diagnosis prior to resection.5
In conclusion, EBUS-TBNA may be a useful tool to confirm diagnosis of mediastinal parathyroid masses, whenever concerns about the diagnosis remain after classical imaging studies have been performed. This is especially true in patients with atypical or complex clinical presentations.
Learning points.
Endobronchial ultrasound-guided transbronchial needle aspiration is a minimally invasive procedure that should be considered in the diagnosis of mediastinal pathology beyond lung cancer staging.
In complex cases, histological diagnosis of mediastinal pathology may help in determining subsequent management.
Footnotes
Contributors: SIB and HZS were responsible for collecting the information and writing the article. The remaining authors were responsible for the surgery and reviewing the article.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Robin P, Boushey MD, Thomas RJ, et al. Middle mediastinal parathyroid: diagnosis and surgical approach. Ann Thorac Surg 2001;71:699–701 [DOI] [PubMed] [Google Scholar]
- 2.Medrano C, Hazelrigg SR, Landreneau RJ, et al. Thoracoscopic resection of ectopic parathyroid glands. Ann Thorac Surg 2000;69:221–23 [DOI] [PubMed] [Google Scholar]
- 3.Pallan S, Rahman MO, Khan AA. Diagnosis and management of primary hyperparathyroidism. BMJ 2012;344:e1013. [DOI] [PubMed] [Google Scholar]
- 4.Yasufuku K, Nakajima T, Fujiwara T, et al. Utility of endobronchial ultrasound-guided transbronchial needle aspiration in the diagnosis of mediastinal masses of unknown etiology. Ann Thorac Surg 2011;91:831–36 [DOI] [PubMed] [Google Scholar]
- 5.Vu Dh, Erickson RA. Endoscopic ultrasound-guided fine-needle aspiration with aspirate assay to diagnose suspected mediastinal parathyroid adenomas. Endocr Pract 2010;16:437–40 [DOI] [PubMed] [Google Scholar]


