Abstract
This case report describes a 54-year-old man who presented to his primary care physician with low back pain. During his workup, an incidental finding of a bladder mass was diagnosed. He underwent transurethral resection of the bladder tumour and the resulting pathology was consistent with extra nodal marginal zone lymphoma of mucosa-associated lymphoid tissue (MALT lymphoma). Presentation of MALT lymphoma in the urinary bladder is rare. This malignancy is more commonly found in the stomach. The prognosis for this rare tumour is excellent. Our patient showed no sign of recurrence with transurethral excision and radiation alone.
Background
Urinary bladder cancer is the sixth most prevalent malignancy in the USA accounting for approximately 7% of cancers in men and 3% of cancers in women.1–3 Bladder cancer is classified into urothelial cancers, which accounts for 90% of bladder cancers and non-urothelial neoplasms compromising the remaining 10% of primary bladder tumours.3 Mucosa-associated lymphoid tissue (MALT lymphoma) most frequently occurs in the stomach. Its location in the urinary bladder is rare and there are only sporadic case reports of MALT lymphoma noted in the medical literature.
Case presentation
A 54-year-old white man presented to his primary care physician with a 3-year history of low back pain radiating to his left leg associated with numbness. He had undergone laminectomy 2 years previously with no improvement. The patient had observed mild weakness of his left leg but possessed steady gait and good bowel and bladder control. His medical history was positive for coronary artery disease, hyperlipidaemia and hypertension but was negative for haematuria. The patient was a current smoker with 40 packs per year history and was a social drinker with less than four alcoholic beverages per week. His occupation was as an antique merchant and he had no known exposure to chemicals or aniline dyes.
An MRI of the lumbar spine was ordered to evaluate his back and leg pain and numbness. The MRI revealed lumbar spinal stenosis. An additional finding of a urinary bladder mass was noted. Subsequent CT of the abdomen and pelvis revealed an enhancing intraluminal mass in the dome of the bladder measuring up to 4 cm in maximal dimension compatible with a neoplasm (figure 1). There was also thickening and enhancement of the right posterior lateral wall of the bladder consistent with neoplastic bladder extension. The results of the patient's blood urea nitrogen, creatinine, prostate-specific antigen, haemoglobin and haematocrit as well as his complete blood count and comprehensive metabolic panel were all completely normal. His urinalysis was also normal with no trace of white or red blood cells or bacteria, and cytology was negative.
Figure 1.
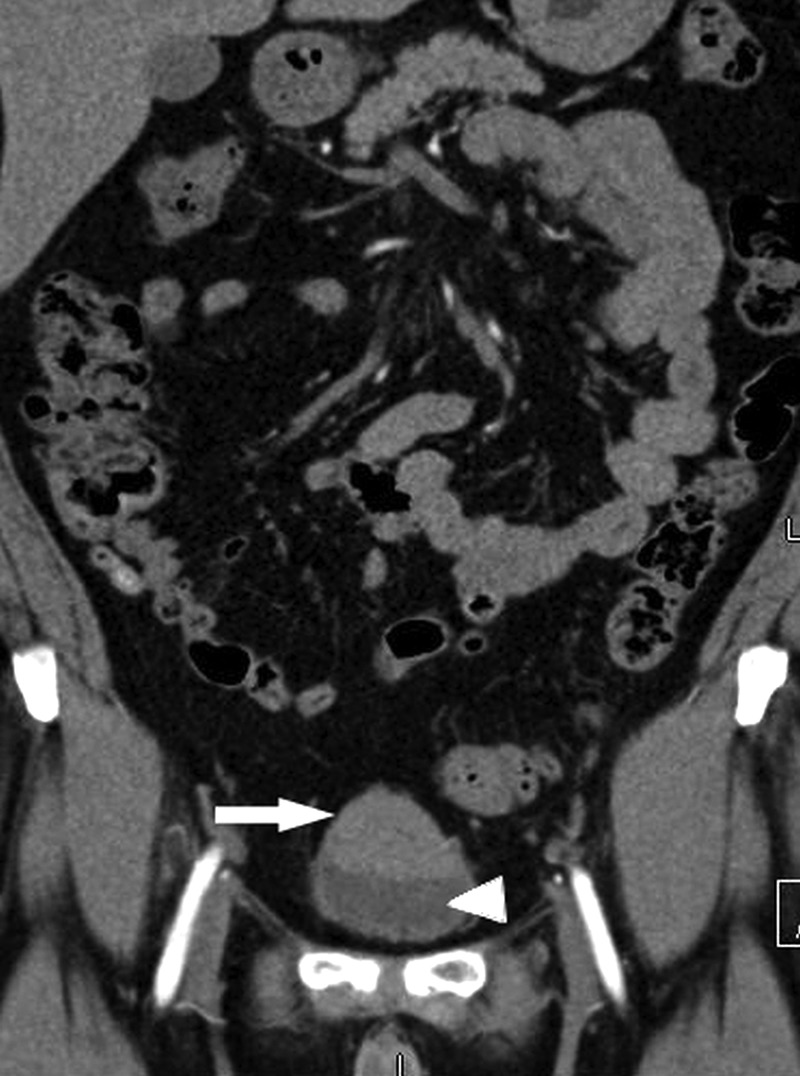
CT of the abdomen and pelvis. The enhancing bladder mass (mucosa-associated lymphoid tissue lymphoma) is identified with a white arrow and the unenhanced urine within the bladder is identified with a white arrowhead.
Investigations
The patient underwent cystourethroscopy for evaluation of the bladder mass. A large mass was seen at the dome of the bladder, which appeared to be of the same colour as the surrounding bladder mucosa. The mass did not have the usual appearance of a common urinary bladder cancer since it did not have an erythematous velvety appearance or any sign of inflammation.
He underwent transurethral resection of the bladder tumour and samples were sent for pathological evaluation. The pathology results were consistent with extranodal marginal zone lymphoma or MALT lymphoma.
Lymphoma workup was performed which included bone marrow biopsy and this was negative. A staging workup was performed using positron emission tomography (PET)/CT scan and upper endoscopy. There was no gastric involvement and no metastasis was found at distant sites or at the regional lymph nodes.
Treatment
In consultation with urological surgeons, radiation oncology and chemotherapeutic oncology and with the patient's preference a decision was made to treat with radiation alone. The regimen consisted of a three three-dimensional conformal treatment plan utilising a mix of 6 and 15 mV photons, including LAO, RAO and AP fields. The patient was treated with a dose of 30.6 Gy in 1.8 Gy per fraction ×17 fractions.
Outcome and follow-up
Three years after transurethral resection and radiation treatment the patient has shown no sign of recurrence.
Discussion
MALT lymphoma is most frequently found in the stomach.2 Its location in the urinary bladder is rare1 but when present it involves the transitional epithelium (urothelium).
Secondary involvement of the bladder by systemic lymphoma is relatively common and has been documented in 10–20% of all patients with non-Hodgkin's lymphoma at necropsy.4
MALT lymphomas have tumour cells that are in a nodular pattern with associated marginal cell differentiation. MALT lymphoma tumour cells are typically CD20 positive, CD3 negative, CD10 negative, cyclin D1 negative and BCL6 negative. When these findings are present it supports the diagnosis of MALT lymphoma (figures 2 and 3).
Figure 2.
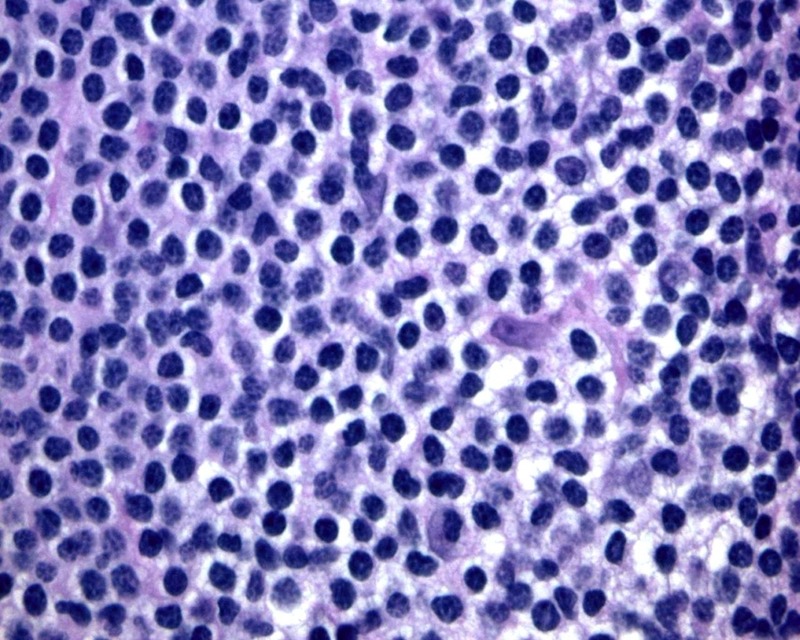
High power of the urinary bladder biopsy revealing lymphoid cells with small round to slightly irregular nuclei with abundant pale cytoplasm typical of marginal zone B-lymphocytes and consistent with mucosa-associated lymphoid tissue lymphoma (H&E, ×400).
Figure 3.
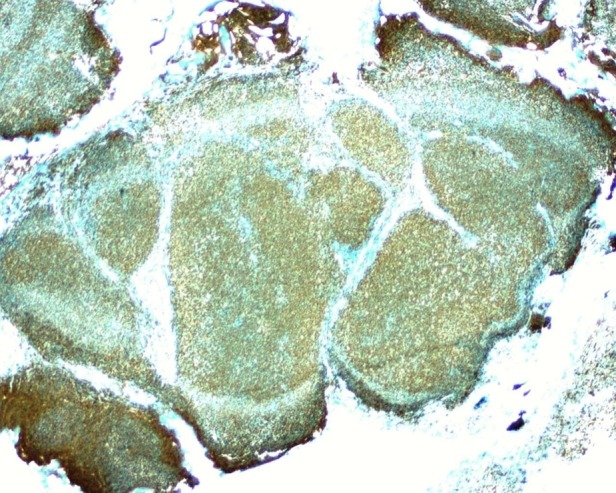
The nodules involving the urinary bladder are strongly CD 20 positive demonstrated by brown coloured immunoperoxidase stain, indicative of a B cell neoplastic process (×20).
Staging of MALT lymphoma includes performing a PET/CT scan, a bone marrow biopsy and an endoscopic gastroduodenoscopy to exclude gastrointestinal involvement. Staging helps with making treatment decisions. Treatments include chemotherapy, radiation therapy and surgical resection, depending on the size and location of the tumour. Treatment guidelines are not well established for urinary bladder MALT tumours since it is such a rare occurrence,2 but the outcomes are generally favourable.5
Learning points.
Mucosa-associated lymphoid tissue (MALT) lymphoma of the urinary bladder is rare.
MALT lymphomas are often found in the stomach.
Staging for MALT lymphoma of the urinary bladder is performed through positron emission tomography/CT scan, bone marrow biopsy and gastroduodenoscopy to exclude gastrointestinal involvement.
Treatments of MALT lymphoma of the bladder include chemotherapy, radiation therapy and surgical resection.
Footnotes
Contributors: JEMH-L, CJH and BV contributed equally to the planning, research and writing of this article.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Swerdlow SH, Campo E, Harris NL, et al. eds. WHO classification of tumors of Hematopoietic and Lymphoid Tissues. 4th edn Lyon, France: IARC Press, 2008:214–17 [Google Scholar]
- 2.Wazait H, Chahal R, Sundurum S, et al. MALT-type primary lymphoma of the urinary bladder: clinicopathological study of 2 cases and review of the literature. Urol Int 2001;66:220–4 [DOI] [PubMed] [Google Scholar]
- 3.Sharma S, Ksheersagar P, Sharma P. Diagnosis and treatment of bladder cancer. Am Fam Phys 2009;80:717–23 [PubMed] [Google Scholar]
- 4.Horasanli K, Kadihasanoglu M, Aksakal O, et al. A case of primary lymphoma of the bladder managed with multimodal therapy. Nat Clin Pract Urol 2008;5:167–70 [DOI] [PubMed] [Google Scholar]
- 5.American Cancer Society [Internet]. Atlanta: Cancer Facts & Figures, c2012. [updated 5 Jan 2012; cited 19 April 2012]. http://www.cancer.org/downloads/STT/CAFF2007PWsecured.pdg [Google Scholar]


