Abstract
Toxocariasis is a consequence of human infection by Toxocara larvae. There are symptomatic (visceral, ocular) and asymptomatic course of toxocariasis. The ocular form is very rare. We present a 6-year-old patient who developed an ocular form of toxocariasis caused by Toxocara cati. He demonstrated lesions in the peripheral retina of the right eye. White granuloma was present in the superior peripheral retina. A positive immunological assay for toxocariasis essentially completed the outcomes. On the basis of clinical manifestations and conducted examinations, a diagnosis of ocular form of toxocariasis was established. Albendazole and corticosteroids were applied in treatment. Current results clearly highlight the usefulness of excretory-secretory antigens derived from larvae of Toxocara cati for the fine diagnosis ocular larva migrans caused by Toxocara larvae.
Keywords: Toxocara cati, Ocular larva migrans, Immunodiagnosis
1. Introduction
Toxocara is a nematode parasite, commonly found in dogs [Toxocara canis (T. canis)] or cats [Toxocara cati (T. cati)]. Humans can be infected by ingesting the ova from dirt contaminated by dog or cat feces[1]. The disease may also result from eating of larvae in uncooked meat of infected parasitic hosts such as chicken, cattle and sheep[2]. Ingested ova produce larvae in the human intestine that invade the intestinal walls, penetrate the blood vessels and lymphatic system, and produced to the liver, lung, and eyes. Toxocara larvae may have a predilection for the retina, which is known as ocular larva migrans (OLM)[3]. As the larvae move through the retinal tissue, they leave tracks and can cause hemorrhage, necrosis, inflammation and ocular lesions that often lead to loss of vision in the affected eye[4].
Diagnosis of ocular toxocariasis is based on clinical findings and specific laboratory tests. An enzyme-linked immunosorbent assay (ELISA) specific using Toxocara excretory-secretory (ES) antigen has been developed. Many authors have reported ocular T. canis infection[5],[6]. Here, we present the case of a 6-year-old boy with ocular toxocariasis who had positive antibodies response to T. cati ES antigen.
2. Case report
A 6-year-old boy was admitted to the Department of Ophthalmology at Khalili Hospital, Shiraz University of Medical Sciences with fever of unknown reasons for 3 months. He complained of blurred vision in the right eye. The ophthalmoscope revealed lesions in the peripheral retina of the right eye. White-masses were present in the superior peripheral retina, with cells in the vitreous. The track of larvae revealed in the fundus examination (Figure 1). Laboratory tests showed a white blood cells count of 8 500/µL with 17% eosinophilia; and platelet count, 23.4×104 µL. Serum chemical examination results were AST, 65 IU/L; ALT, 115 IU/L; and total bill, 0.77 mg/dL (Table 1). Results of the examination of feces for the presence of eggs and larvae of parasites were negative. Antibodies specific to Toxocara purified ES antigens were detected in the serum sample and vitreous fluid by ELISA.
Figure 1. Fundus photograph showing white lesions caused by the migration of T. cati larvae (arrows).
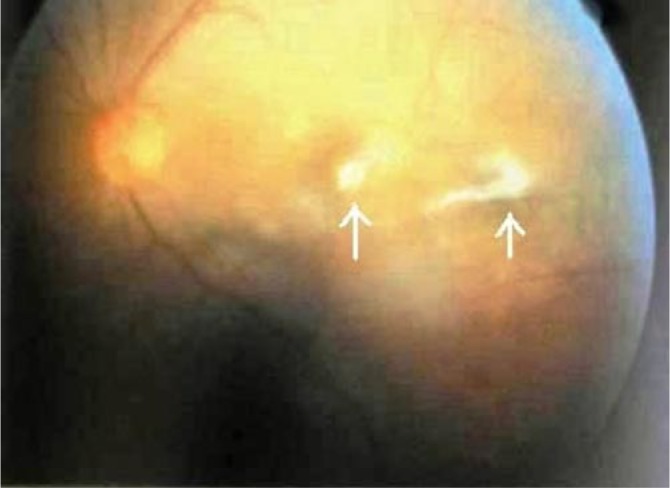
Table 1. Results of patient's blood cell count and serum chemical examinations.
| Indicator | The patient's values | Normal |
| White blood count (×1 000/µL) | 8.51 | 5.0-14.5 |
| Red blood count (×106/µL) | 4.56 | 3.9-5.3 |
| Platelets ((×103/µL) | 234 | 150-440 |
| Eosinophil (%) | 17.0 | 2.0-7.0 |
| Erythrocyte sedimentation rate (mm/h) | 27.0 | 0.0-15.0 |
| AST (IU/L) | 65.0 | 57.0-67.0 |
| ALT (IU/L) | 115.0 | 112.0-118.0 |
| Total protein (mg/dL) | 0.77 | 0.1-1.2 |
| Uric acid (mg/dL) | 55.4 | 3.6-8.2 |
Antibodies titer against T. cati was strongly positive (ELISA) in sera and vitreous fluid with the third-stage larvae ES antigen. Antibodies titers in sera for ascariasis, trichostrongyliasis, hydatidosis, toxoplasmosis, and leishmaniasis were negative. ELISA using T. canis ES antigen showed a low antibodies titer in the patient serum. The patient was treated with albendazole (400 mg twice daily) and oral prednisolone for 3 weeks. Two months later, the patient was improved following treatment.
3. Discussion
Human toxocariasis is a common helminth zoonosis that has a worldwide distribution and is also endemic in the Iran. Sero-epidemiological studies in Iran report a Toxocara seroprevalence rate of 25.6% amongst the children and up to 5.2% amongst people at risk[7],[8]. In a study, we have previously reported that 42.6% of stray cats in our area were positive for T. cati[9].
Ocular abnormalities are a frequent complication of toxocariasis. Ocular toxocariasis is typically a monocular disease of young children. Patient with this disease present with chronic unilateral uveitis and a marked vitreous opacification that overlies a primary eosinophilic granuloma. Exudative retinal detachment, posterior synechiae, and a cyclitic membrane may be present. Toxocara granuloma is white, dome-shape, and confined principally to the retina[10]. Serological tests like ELISA with Toxocara infective larval ES antigen is the gold standard for diagnosis of ocular toxocariasis.
In our case, serum eosinophilia early suggested a possible helminthic infection. Peripapillary lesions with a highly reflective mass protruding from the thickened retina into the vitreous observed in ophthalmoscopy. In the case discussed here, ELISA using T. canis ES antigen showed that antibodies titer was lower, whereas using T. cati ES protein revealed high antibodies titer. Hence, we believe that ocular toxocariasis is caused by T. cati. In a study examining the serodiagnosis of ocular toxocariasis, Sakai et al. reported that T. cati could cause ocular toxocariasis in human[11].
However, it was our choice to combine anti-helminthic therapy and use steroids for 4 weeks which led to clinical and ophthalmologic improvement corroborating the diagnosis of ocular toxocariasis. The use of steroids is controversial that should be administered in ocular involvement[12]. As evidenced by clinical recovery and ophthalmology improvement in our patient, we suggest simultaneous administration of immunosuppressant and albendazole in ocular infection by T. cati larvae.
We concluded that although ocular involvement is common in toxocariasis with T. canis, an ocular infection caused by T. cati is rare. It draws attention of ophthalmologists to the possibility of ocular toxocariasis particularly in the children with eosinophilia and that ocular involvement can be caused by T. cati, and a test using T. cati ES should be performed to confirm the disease.
Comments
Background
Toxocariasis is a consequence of human infection by Toxocara larvae. There are symptomatic (visceral, ocular) and asymptomatic course of toxocariasis. The ocular form is very rare. The authors of this paper presented a 6-year-old patient who developed an ocular form of toxocariasis.
Research frontiers
The current report presents a 6-year-old patient who developed an ocular form of toxocariasis.
Related reports
Ocular toxocariasis was based on clinical findings and the presence of vitreous antibodies. Sakai et al. reported that T. cati could cause ocular toxocariasis in human.
Innovations and breakthroughs
To my knowledge, this is the first report of ocular toxocariasis caused by T. cati and diagnosed by immunoassay in our area.
Applications
It draws attention of ophthalmologists to the possibility of ocular toxocariasis particularly in the children with eosinophilia and that ocular involvement can be caused by T. cati, and a test using T. cati ES should be performed to confirm the disease.
Peer review
Ocular infection with T. cati is rare. It is a good report that showed a case of ocular toxocariasis. Molecular techniques can be used to confirm diagnosis.
Footnotes
Conflict of interest statement: We declare that we have no conflict of interest.
References
- 1.Despommier D. Toxocariasis: clinical aspects, epidemiological, medical ecology and molecular aspects. Clin Microbiol Rev. 2003;16(2):265–272. doi: 10.1128/CMR.16.2.265-272.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Taira K, Saitoh Y, Kapel CM. Toxocara cati larvae persist and retain high infectivity in muscles of experimentally infected chickens. Vet Parasitol. 2011;180(3–4):287–291. doi: 10.1016/j.vetpar.2011.03.020. [DOI] [PubMed] [Google Scholar]
- 3.Zibaei M, Sadjjadi SM, Karamian M, Uga S, Oryan A, Jahadi-Hosseini SH. A comparative histopathology, serology and molecular study, on experimental ocular toxocariasis by Toxocara cati in Mongolian gerbils and Wistar rats. Biomed Res Int. 2013;2013:109580. doi: 10.1155/2013/109580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Steward JM, Cubillan LD, Cunning ET., Jr Prevalence, clinical features, and causes of vision loss among patients with ocular toxocariasis. Retina. 2005;25(8):1005–1013. doi: 10.1097/00006982-200512000-00009. [DOI] [PubMed] [Google Scholar]
- 5.de Visser L, Rothova A, de Boer JH, van Loon AM, Kerkhoff FT, Canninga-van Dijk MR, et al. Diagnosis of ocular toxocariasis by establishing intraocular antibody production. Am J Ophthalmol. 2008;145(2):369–374. doi: 10.1016/j.ajo.2007.09.020. [DOI] [PubMed] [Google Scholar]
- 6.Arevalo JF, Espinoza JV, Arevalo FA. Ocular toxocariasis. J Pediatr Ophthalmol Strabismus. 2013;50(2):76–86. doi: 10.3928/01913913-20120821-01. [DOI] [PubMed] [Google Scholar]
- 7.Sadjjadi SM, Khosravi M, Mehrabani D. Oryan A. Seroprevalence of Toxocara infection in school children in Shiraz, Southern Iran. J Trop Pediatr. 2003;46(6):327–330. doi: 10.1093/tropej/46.6.327. [DOI] [PubMed] [Google Scholar]
- 8.Yousefi H, Avigan M, Taheri AM. A survey about toxocariasis in Chaharmahal-va-Bakhtiari province in first 6 months of 2000. Iran J Infect Dis Trop Med. 2001;5(13):16–20. [Google Scholar]
- 9.Zibaei M, Sadjjadi SM, Sarkari B. Prevalence of Toxocara cati and other intestinal helminths in stray cats in Shiraz, Iran. Trop Biomed. 2007;24(2):39–43. [PubMed] [Google Scholar]
- 10.Kim YJ, Moon CH, Chang JH. Toxocariasis of the optic disc. J Neuroophthalmol. 2013;33(2):151–152. doi: 10.1097/WNO.0b013e3182893ff9. [DOI] [PubMed] [Google Scholar]
- 11.Sakai R, Kawashima H, Shibui H, Kamata K, Kambara C, Matsuoka H. Toxocara cati-induced ocular toxocariasis. Arch Ophthalmol. 1998;116(112):1686–1687. [PubMed] [Google Scholar]
- 12.Walker MD, Zunt JR. Neuroparasitic infection: nematodes. Semin Neurol. 2005;25(3):252–261. doi: 10.1055/s-2005-917662. [DOI] [PMC free article] [PubMed] [Google Scholar]


