Abstract
We report an extremely rare case of isolated retroperitoneal enteric duplication cyst with gastric mucosa causing haematuria and dysuria by communicating with the urinary system. A 9-month-old male child was admitted to our hospital with persistent haematuria, dysuria and anaemia. Investigations revealed a retroperitoneal cyst abutting the hydronephrotic non-functioning right kidney. At surgery an isolated retroperitoneal cyst communicating with the right pelviureteric junction was found. The kidney and associated cyst were excised. Histology of the cystic lesion revealed an enteric duplication cyst lined by ectopic gastric mucosa. Isolated retroperitoneal enteric duplication cyst communicating with the urinary tract has not been previously reported in the English literature. We propose that acid secretion into the right renal system was the cause of the haematuria–dysuria syndrome which promptly resolved postoperatively.
Background
Enteric duplication cysts are congenital gastrointestinal anomalies arising anywhere along the alimentary tract and present with a variety of symptoms.1–4 Retroperitoneal enteric duplication cysts are very rare.5–8 Furthermore, a communication between a retroperitoneal duplication cyst and urinary tract has not been previously reported in the literature. We report a case of a 9-month-old male child with isolated retroperitoneal duplication cyst causing haematuria and dysuria due to communicating with the upper ureter.
Case presentation
A 9-month-old male child was referred with severe dysuria associated with gross haematuria since 3 months of age. At admission, the child was pale and physical examination revealed fever (37.8°C) and a palpable mass was in the right flank. No prenatal ultrasound was available.
Investigations
The haemoglobin level was 5.5 g/dL, and the total white cell count (WCC) was 32.3×109/L. Urea and creatinine levels were 14 and 0.45 mg/dL, respectively. Urine microscopy showed 40 000 WCCs/µL of uncentrifuged urine and presence of bacteria. Urine culture detected 58 000 colony-forming units (CFU) per mL of Escherichia coli and Klebsiella producing extended-spectrum β-lactamases (ESBLs).
Ultrasound of the abdomen revealed right-sided hydronephrosis (renal pelvis anteroposterior diameter of 16 mm), focal thickening of the posterior wall of the urinary bladder and a well-defined, thick-walled cyst, which measured 3.28 cm×2.02 cm×2.28 cm and contained a layering echogenic material in the right lower quadrant of the abdomen (figure 1).
Figure 1.
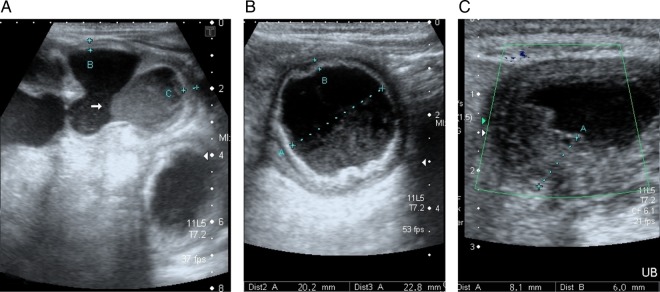
Abdominal ultrasound examination showing the dilation to the right renal pelvis (A), a thick-walled cyst, containing echogenic fluid, in the right lower quadrant of the abdomen (B) and a thickened bladder wall (C).
Abdominal CT confirmed a severe right hydronephrosis and the thickness of the posterior wall of the bladder, and a well-defined cystic lesion (3.2×2.4 cm) abutting the homolateral ureter was seen (figure 2). The cyst wall had a thickness of 9 mm and it was showing gut signature suggestive of enteric duplication. The radionuclide renal scan (DMSA) showed a non-functioning (0% in DMSA) right kidney.
Figure 2.
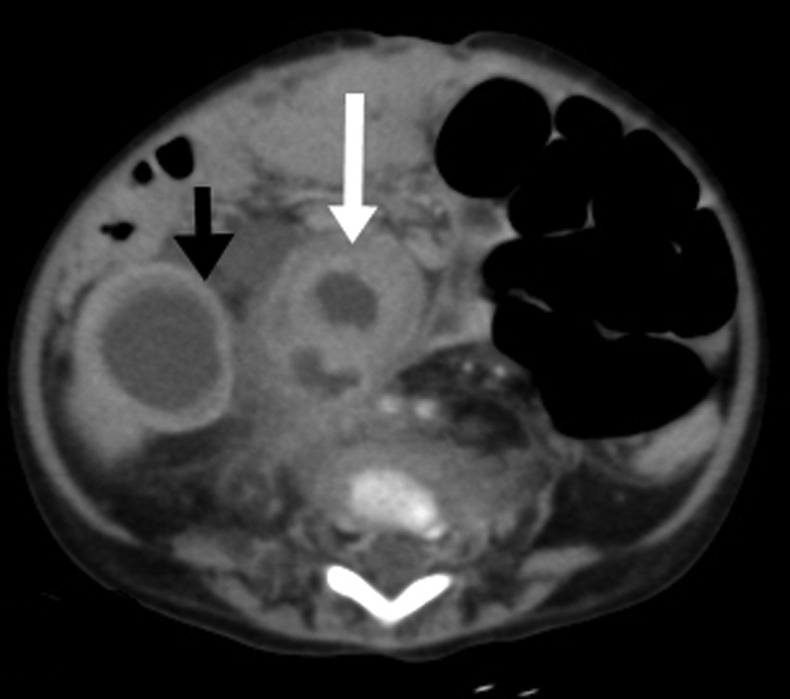
CT of the abdomen showing gross right-sided hydronephrosis with thinning of renal parenchyma (black arrow) and a well-defined cystic lesion of size 3.2×2.4 cm (white arrow) seen in the right paracaval location, showing gut signature, with thickened wall up to 9 mm, perilesional marked fat stranding with the surrounding mild fluid collection. The lesion was abutting the right upper ureter.
Treatment
The infant was initially treated with intravenous antibiotics and blood transfusion. On 11th day following admission, elective laparotomy revealed gross hydronephrosis of the right kidney and a separate cystic mass communicating with the upper ureter and the pelviureteric junction from the medial aspect. There were marked inflammatory adhesions surrounding this communication. The renal pelvis, ureter and the cyst opened into a common cavity filled with a brownish haemorrhagic fluid. The cyst was spherical and thick walled, measuring 3.5 cm×2 cm, located between the right proximal ureter and the inferior vena cava (figure 3). The cyst did not communicate with the alimentary tract nor shared any blood supply with it. Right nephrectomy and excision of the cyst were performed.
Figure 3.
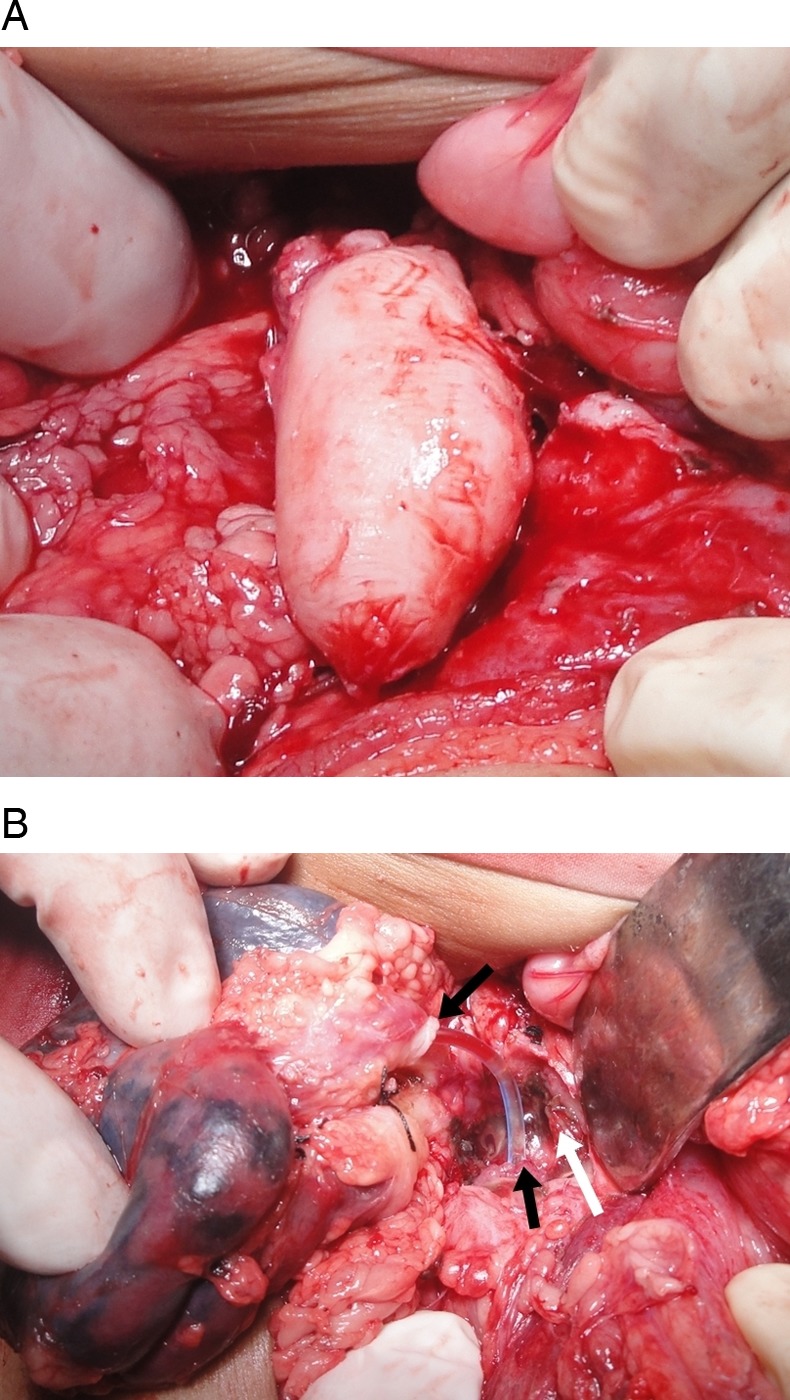
Intraoperative image showing (A) a spherical, isolated, thick-walled cyst, (B) the renal pelvis, ureter and cyst opening into a common cavity; black arrows showing continuity of pelviureter where the feeding tube is passed; white arrow showing opening of the cyst into the cavity.
Histopathological examination confirmed the diagnosis of a gastric duplication cyst containing circular and longitudinal muscle layers (figure 4).
Figure 4.
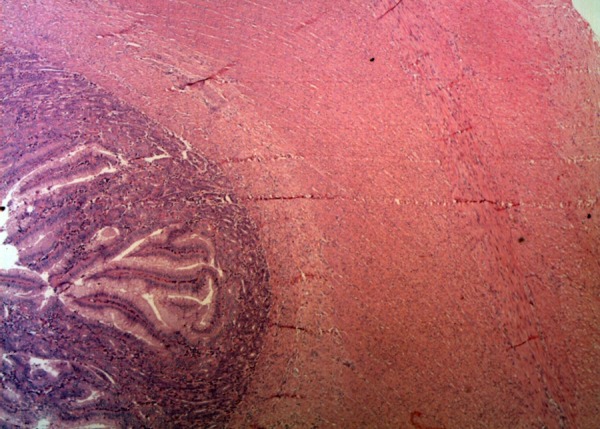
Histopathological microphotographs of the duplication cyst containing circular and longitudinal muscle layers (H&E stain under ×50 magnification).
Outcome and follow-up
Postoperative course was uneventful with cessation of haematuria and dysuria immediately after the surgery. The child was discharged on third postoperative day. A repeat abdominal ultrasonography was performed on fifth postoperative day as outpatient showed a decrease in urinary bladder wall thickening. The child remained asymptomatic until the last follow-up at 5 months.
Discussion
Enteric duplication cysts are congenital malformations that are found anywhere from the mouth to the anus.1 2 9The following three criteria are proposed for gastric duplication cysts by Rowling: (1) the cyst must be attached to the stomach and contiguous with its wall; (2) the cyst must be surrounded by a smooth-muscle coat, fusing with the muscle of the stomach and (3) the cyst must be lined by alimentary epithelium.10 Completely isolated retroperitoneal enteric duplication cysts without any communication with the alimentary tract are very rare. To the best of our knowledge, 14 such cases of isolated retroperitoneal enteric cysts have been reported previously, some with a prenatal diagnosis.6 7 11–19 Three cases of retroperitoneal duplication cyst adjacent to the kidney were reported in the literature; of these, one case showed a unilateral hydronephrosis of a horseshoe kidney.5 17 20 The child described is the first reported case to present with haematuria-dysuria syndrome caused by an enteric duplication cyst communicating with the urinary tract.
While haematuria-dysuria syndrome is a well-known complication of gastrocystoplasty, we propose the following pathogenesis of these sequelae seen in our case.21 22 The acid secretion from the gastric epithelium within the isolated retroperitoneal duplication cyst had caused fistulous communication with the right urinary system through the proximal ureter. This had caused severe inflammation of the renal pelvis, ureter and bladder wall as shown by the thickening on ultrasound and enhancement in CT scan in these regions. Erosion of the urothelium manifested as haematuria-dysuria and also made the child susceptible to infection. The combination of obstruction, inflammation and infection resulted in a non-functioning right kidney.
A correct preoperative diagnosis of retroperitoneal enteric duplication cysts can be made with a high index of suspicion and proper imaging. Ultrasound is useful in diagnosing enteric duplication cysts, including retroperitoneal cysts, by showing the typical inner hyperechoic mucosal and outer hypoechoic muscle layers (‘double-wall sign’).4 The CT scan helps in determining the nature, location and extent of the lesion and also to rule out other abdominal masses, multiple duplication cysts and vertebral anomalies. Prenatal ultrasound is useful in detecting intra-abdominal cysts. In our case, the child was referred to our institute from a remote rural area where prenatal ultrasound was not available.
Risk of bleeding, infection, intestinal obstruction and malignancy necessitates excision of enteric duplication cysts.8 12 14 23 Complete surgical excision is the treatment of choice for all enteric duplication cysts, including those located in the retroperitoneum. Most retroperitoneal enteric cysts can be excised without sacrificing the normal bowel. A minimal access approach has been used successfully in the excision of retroperitoneal enteric duplication cysts.7 17 Although we have a reasonable amount of experience with laparoscopy in children (10–12 cases/week), an open approach was considered safer in this infant due to intense inflammation on the medial aspect of the right hydronephrotic kidney with the consequent risk of injury to the adjacent inferior vena cava.
In conclusion, we report a unique case of retroperitoneal gastric duplication cyst fistulating into the right upper ureter. The resulting acid secretion caused severe inflammation upstream and downstream in the ipsilateral ureterorenal unit with destruction of the kidney and a haematuria-dysuria syndrome.
Learning points.
Isolated enteric duplication cysts can rarely occur in retroperitoneum. If juxtarenal, they can cause renal damage.
Duplication cysts become symptomatic either due to pressure effects or ectopic gastric secretion. We report a unique case where acid secretion into the ureter resulted in severe haematuria-dysuria syndrome and a non-functioning kidney.
Duplication cysts have a characteristic appearance on ultrasound and CT and these imaging modalities are useful in diagnosis.
Surgical excision is a curative treatment and pathological examination is essential to confirm the diagnosis.
Footnotes
Contributors: HSB, SK SS and DM contributed in conception and design of the manuscript, acquisition of the data and interpretation of the data and also in drafting the article or revising it critically for important intellectual content. Final submitted version of the manuscript is approved by all the authors.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Iyer CP, Mahour GH. Duplications of the alimentary tract in infants and children. J Pediatr Surg 1995;30:1267–70 [DOI] [PubMed] [Google Scholar]
- 2.Karnak I, Ocal T, Senocak ME, et al. Alimentary tract duplications in children: report of 26 years’ experience. Turkish J Pediatr 2000;42:118–25 [PubMed] [Google Scholar]
- 3.Menon P, Rao KL, Vaiphei K. Isolated enteric duplication cysts. J Pediatr Surg 2004;39:e5–7 [DOI] [PubMed] [Google Scholar]
- 4.Hur J, Yoon CS, Kim MJ, et al. Imaging features of gastrointestinal tract duplications in infants and children: from oesophagus to rectum. Pediatr Radiol 2007;37:691–9 [DOI] [PubMed] [Google Scholar]
- 5.Pachl M, Patel K, Bowen C, et al. Retroperitoneal gastric duplication cyst: a case report and literature review . Pediatr Surg Int 2012;28:103–5 [DOI] [PubMed] [Google Scholar]
- 6.Okamoto T, Takamizawa S, Yokoi A, et al. Completely isolated alimentary tract duplication in a neonate. Pediatr Surg Int 2008;24:1145–7 [DOI] [PubMed] [Google Scholar]
- 7.Souzaki R, Ieiri S, Kinoshita Y, et al. Laparoscopic resection of an isolated retroperitoneal enteric duplication in an infant. J Pediatr Surg Case Rep 2013;1:167–70 [Google Scholar]
- 8.Kyriakos N, Andreas C, Elena S, et al. Infected completely isolated enteric duplication cyst management with percutaneous drainage and surgical excision after retreat of infection: a case report. Case Rep Surg 2013;2013:108126 (accessed 27 Sep 2013) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hambarde S, Bendre P, Taide D. Foregut duplication cyst presenting as lingual swelling: case report and review of literature. Natl J Maxillofac Surg 2011;2:2–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rowling JT. Some observations on gastric cysts. Br J Surg 1959;46:441–5 [DOI] [PubMed] [Google Scholar]
- 11.Nakazawa N, Okazaki T, Miyano T. Prenatal detection of isolated gastric duplication cyst. Pediatr Surg Int 2005;21:831–4 [DOI] [PubMed] [Google Scholar]
- 12.Upadhyay N, Gomez D, Button MF, et al. Retroperitoneal enteric duplication cyst presenting as a pancreatic cystic lesion. A case report. J Pancreas 2006;7:492–5 [PubMed] [Google Scholar]
- 13.Terry NE, Senkowski CK, Check W, et al. Retroperitoneal foregut duplication cyst presenting as an adrenal mass. Am Surg 2007;73:89–92 [PubMed] [Google Scholar]
- 14.Hata H, Hiraoka N, Ojima H, et al. Carcinoid tumor arising in a duplication cyst of the duodenum. Pathol Int 2006;56:272–8 [DOI] [PubMed] [Google Scholar]
- 15.Lo YS, Wang JS, Yu CC, et al. Retroperitoneal enteric duplication cyst. J Chin Med Assoc 2004;67:479–82 [PubMed] [Google Scholar]
- 16.Duncan BW, Scott Adzick N, Eraklis A. Retroperitoneal alimentary tract duplications detected in utero. J Pediatr Surg 1992;27:1231–3 [DOI] [PubMed] [Google Scholar]
- 17.Chen P-H, Lee J-Y, Yang S-F, et al. A retroperitoneal gastric duplication cyst mimicking a simple exophytic renal cyst in an adolescent. J Pediatr Surg 2010;45:e5–8 [DOI] [PubMed] [Google Scholar]
- 18.May DA, Spottswood SE, Ridick-Young M, et al. Case report: prenatally detected dumbbell-shaped retroperitoneal duplication cyst. Pediatr Radiol 2000;30:671–3 [DOI] [PubMed] [Google Scholar]
- 19.Alabbad SI, Ryckman J, Puligandla PS, et al. Use of transanastomotic feeding tubes during esophageal atresia repair. J Pediatr Surg 2009;44:902–5 [DOI] [PubMed] [Google Scholar]
- 20.Matsumoto F, Tohda A, Shimada K, et al. Pancreatic pseudocyst arising from ectopic pancreas and isolated intestinal duplication in mesocolon caused hydronephrosis in a girl with horseshoe kidney. J Pediatr Surg 2005;40:e5–7 [DOI] [PubMed] [Google Scholar]
- 21.Kurzrock EA, Baskin LS, Kogan BA. Gastrocystoplasty: long-term follow up. J Urol 1998;160:2182–6 [PubMed] [Google Scholar]
- 22.Plaire JC, Snodgrass WT, Grady RW, et al. Long-term followup of the hematuria-dysuria syndrome. J Urol 2000;164:921–3 [PubMed] [Google Scholar]
- 23.Wheatley K, Jayatunga R, Singh M, et al. A duplication cyst masquerading as a Meckel's diverticulum. Arch Dis Child 2012;97(Suppl 1):A15 [Google Scholar]


