Abstract
Giant aneurysms arising from the cavernous internal carotid artery (ICA) can mimic pituitary adenomas and may cause pituitary dysfunction due to their mass effect on the pituitary gland. We report a case of a 56-year-old man presenting with impotence, fatigue and panhypopituitarism who was found to have a giant unruptured aneurysm arising from the right cavernous ICA with severe mass effect on the pituitary gland. The patient underwent endovascular treatment of the giant aneurysm using two telescoping Surpass flow-diverting stents. At 6-month follow-up, repeat cerebral angiography showed Raymond grade II occlusion of the aneurysm with a small neck remnant. At the 10-month follow-up the patient showed full recovery of his pituitary function and clinical resolution of impotence and fatigue. This is the first report of occlusion of a giant cavernous carotid aneurysm using next generation Surpass flow-diverting stents leading to complete recovery of pituitary function.
Keywords: Aneurysm, Flow Diverter, Technique
Background
Giant cavernous internal carotid artery (ICA) aneurysms mimicking pituitary tumors and causing pituitary dysfunction are rare but well documented.1–7 It is estimated that they are the cause of hypopituitarism in about 0.2% of patients.5 Open surgical options offer definitive treatment of these aneurysms as well as decompression of the pituitary gland; however, they are often technically challenging and carry many risks inherent to open surgery. Conventional endovascular treatment of coiling with or without stenting is a less invasive option, but it fails to achieve pituitary decompression. With the advent of flow diverters such as the Pipeline Embolization Device (PED; Covidien, Mansfield, Massachusetts, USA), the Silk stent (Balt, Montmorency, France) and the newest flow-diverting stents including Surpass (Stryker Neurovascular, Fremont, California, USA) and FRED (Microvention, Tustin, California, USA), neuroendovascular surgeons are equipped with another powerful tool with which to treat these complex cerebral aneurysms.
We report our experience with the use of Surpass flow-diverting stents (currently under investigational use in the SCENT trial) to successfully treat an unruptured giant cavernous ICA aneurysm causing panhypopituitarism (without diabetes insipidus) with subsequent full recovery of pituitary function after treatment. To our knowledge, this is the first report of complete recovery of pituitary function after endovascular treatment of a giant cavernous ICA aneurysm using a flow-diverting stent.
Case presentation
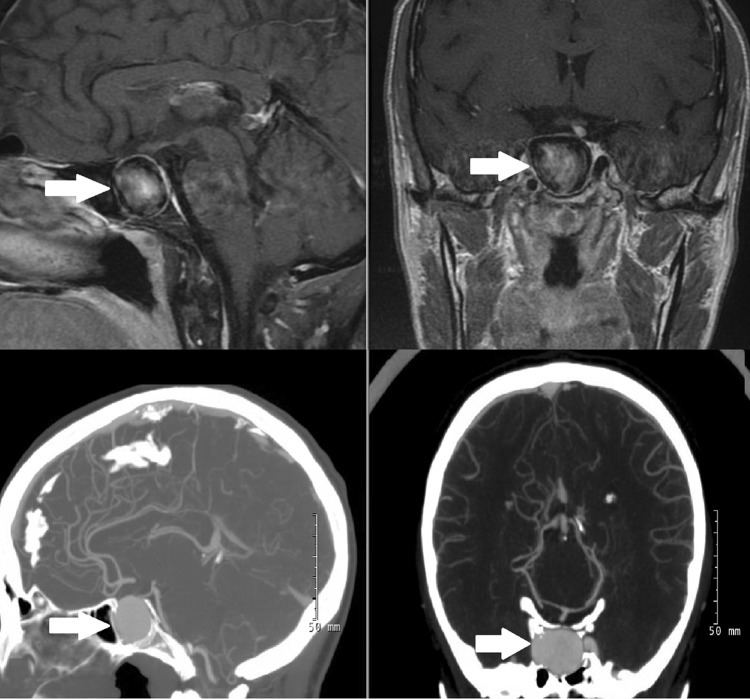
A 56-year-old man presented with impotence and generalized fatigue for 3 months. Physical examination was unremarkable with no visual deficit on ophthalmology examination. Endocrine investigation showed hypopituitarism with markedly decreased levels of 08:00 cortisol, testosterone and insulin-like growth factor 1 and low normal free thyroxine with normal thyroid-stimulating hormone (table 1). There was no evidence of diabetes insipidus. The patient was started on hydrocortisone, topical testosterone and levothyroxine for his pituitary insufficiency. MRI was obtained for panhypopituitarism investigation and showed a large well-circumscribed enhancing sellar mass with a significant mass effect on the pituitary gland; subsequent CT angiography showed a giant right cavernous ICA aneurysm (figure 1). After careful evaluation, an endovascular approach using Surpass flow-diverting stents was deemed to be the most appropriate treatment.
Table 1.
Pre-procedural and post-procedural endocrine laboratory values demonstrating pituitary function recovery
| Endocrine panel | Pre-procedural | Reference* | Post-procedural† | Reference |
|---|---|---|---|---|
| FSH | N/A | 1.2–8.6 | 3.3 | 1–10 |
| LH | 0.8 | 1–10 | 2.5 | 1–10 |
| Total testosterone | 33 | 175–780 | 833 | 250–1100 |
| Free testosterone | 3 | 50–247 | 69.9 | 35–155 |
| TSH | 2.8 | 0.35–4.94 | 2.9 | 0.4–4 |
| Free T4 | 0.7 | 0.7–1.5 | 1.1 | 0.7–1.5 |
| ACTH | 12 | 6–50 | 29 | 6–50 |
| Cortisol (08:00) | 2.6 | 3.7–19.4 | 12.3 | 3.7–19.4 |
| Prolactin | 13.5 | 2.6–13.1 | 14 | 3–16 |
| IGF-1 | 20 | 50–317 | 88 | 50–317 |
| Serum sodium | 142 | 135–145 | 143 | 135–145 |
*Preoperative reference ranges are different because they were obtained at outside hospital.
†IGF-1 normalized at 10-week follow-up; adrenal axis normalized at 15 weeks; gonadal axis normalized at 23 weeks; thyroid axis normalized at 10-month follow-up.
ACTH, adrenocorticotrophic hormone; FSH, follicle-stimulating hormone; IGF-1, insulin-like growth factor 1; LH, luteinizing hormone; T4, thyroxine; TSH, thyroid-stimuilating hormone.
Figure 1.
MRI (top) and CT angiogram (bottom) demonstrating a giant right cavernous internal carotid artery aneurysm with significant mass effect on the pituitary gland.
Treatment
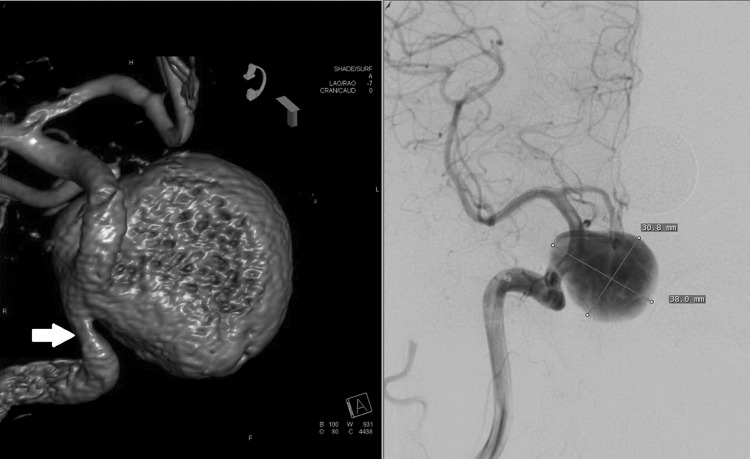
The patient was taken to the endovascular suite and underwent general anesthesia with therapeutic aspirin and clopidogrel levels (aspirin reaction units <550, P2Y12 reaction units <230) as well as heparinization to keep the activated clotting time >250. The right ICA was catheterized and three-dimensional angiography demonstrated the giant right cavernous carotid aneurysm measuring 3.8 cm×3.0 cm with neck measuring 7 mm and focal stenosis proximal to the neck (figure 2). Two Surpass flow-diverting stents (4×30 mm and 5×25 mm) were successfully deployed across the neck of the aneurysm with a 50% overlap to fully cover the aneurysm neck. Intraprocedural Dyna CT angiography demonstrated good patency of the stents and tight opposition of the stents against the vessel wall (figure 3). Balloon angioplasty was performed for the stenosis proximal to the neck aneurysm to prevent further stenosis in the future.
Figure 2.
Anteroposterior, lateral and three-dimensional angiogram demonstrating the giant right cavernous internal carotid artery aneurysm measuring 3.8 cm×3.0 cm with a 7 mm neck and a focal stenosis of the carotid artery just proximal to the aneurysm neck (arrow).
Figure 3.
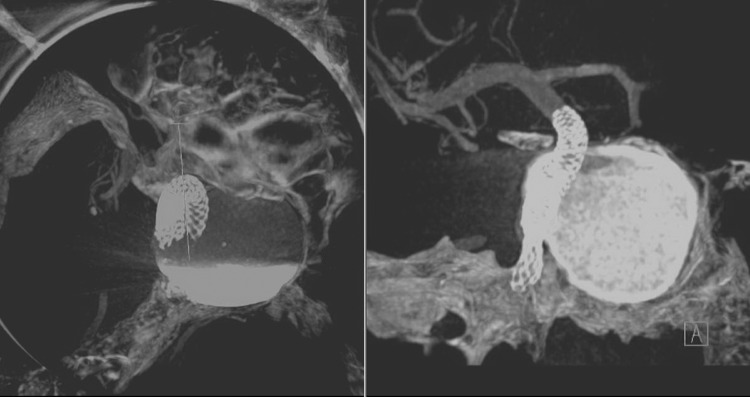
Intra-procedural Dyna CT angiogram demonstrating good patency of the stents and tight opposition of the stents against the vessel wall.
Outcome and follow-up
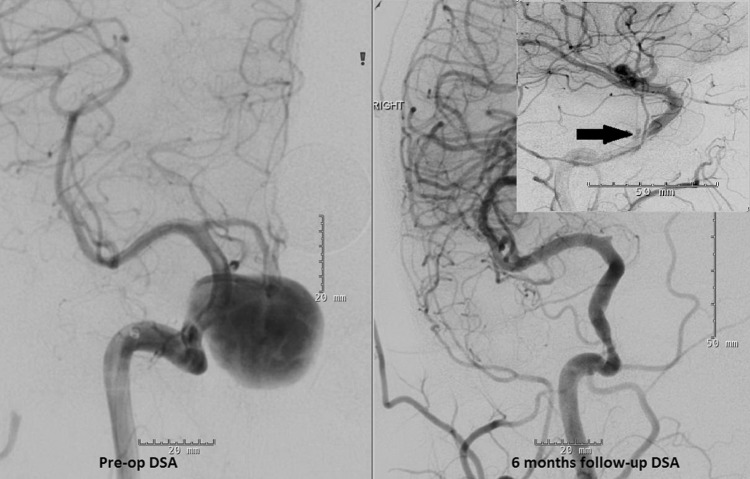
The patient tolerated the procedure well without any complications. He was kept on dual antiplatelet regimen as well as hormonal replacement therapy after the procedure. The patient remained clinically well and the 6-month follow-up diagnostic angiogram demonstrated Raymond grade II occlusion of the giant aneurysm with a small neck remnant measuring 2 mm (figure 4). The stenosis just proximal to the aneurysm neck was stable. This was thought to be due to the residue mass effect from the aneurysm itself; since the stenosis is elastic and not atherosclerotic, angioplasty during the initial intervention had minimal effect on the stenosis, as seen in the follow-up angiogram. Clopidogrel was discontinued at this time. The patient was weaned off all hormonal replacement therapy and showed complete recovery of endocrine function at the 10-month follow-up visit (table 1).
Figure 4.
Pre-procedural digital subtraction angiogram (DSA) demonstrating the giant right cavernous internal carotid artery aneurysm (left); follow-up angiogram at 6 months demonstrating Raymond grade II occlusion of the aneurysm (right) with a small neck remnant (arrow).
Discussion
Pituitary dysfunction is a rare manifestation of giant cavernous ICA aneurysms due to compression of the pituitary gland.1–7 The most common pituitary dysfunction associated with giant ICA aneurysms in the cavernous region is hypogonadism, followed by adrenal insufficiency and hypothyroidism.8 The mechanisms of the endocrine dysfunction may be due to either direct mechanical compression of the pituitary gland, or vascular compression of the superior hypophyseal artery subsequently causing pituitary ischemia.9 Other symptoms due to mass effect such as headaches and visual deficit frequently accompany endocrine disturbances in these patients.9 Hypopituitarism, if present, is usually permanent in most of the cases even after treatment of the giant paraclinoid/cavernous aneurysms.3 8 There are only a few reports documenting recovery of endocrine function after surgical clipping of the giant ICA aneurysm and decompression of the pituitary gland.7 10 To our knowledge, recovery of pituitary function after endovascular treatment of giant cavernous ICA aneurysms with flow-diverting stents has not been reported in the literature.
Open surgical treatment offers definitive treatment of aneurysms and decompression of the pituitary gland,7 but it is technically challenging and has a high risk of cranial nerve palsy. The traditional endovascular approach with coiling with or without stenting fails to provide pituitary decompression, and coil embolization with or without stenting in giant aneurysms has not been successful due to their propensity for recanalization.
The advent of flow diverters provides neuroendovascular surgeons with another new tool with which to treat these formidable and complex aneurysms. Surpass is a cobalt-chromium, low porosity, self-expanding stent with metal surface coverage of 30%. This flow diverter with high metal coverage promotes aneurysm thrombosis over time by diverting blood flow away from the aneurysm. Since coiling is not always required with flow diverters, there is potential for the aneurysm mass effect and pulsation to decrease on the pituitary gland. In the case of giant cavernous carotid aneurysms causing pituitary dysfunction, aneurysm thrombosis and lack of pulsation could potentially facilitate endocrine function recovery as demonstrated in our patient. Other factors that may affect endocrine recovery after treatment may include the length of pituitary dysfunction and the extent of pituitary compression, as the prerequisite for pituitary function recovery is viable pituitary tissue. Two patients in the existing literature who had recovery of endocrine function after surgical decompression had symptoms for 6 and 7 months, respectively.7 10 Our patient had symptoms for 3 months prior to his diagnosis and treatment.
Flow-diverting stents can be a safe and effective treatment option for patients with giant ICA aneurysms causing pituitary insufficiency and offer an improved chance for pituitary function recovery.
Learning points.
Flow-diverting stents can be a safe and effective treatment option for patients with giant internal carotid artery (ICA) aneurysms.
Flow-diverting stents may offer an improved chance of pituitary function recovery in patients with pituitary insufficiency due to mass effect from giant ICA aneurysms.
This is the first report of complete recovery of pituitary function after occlusion of a giant cavernous carotid aneurysm using a flow-diverting stent.
Footnotes
Contributors: All authors contributed equally to the preparation of this manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Borges FZ, Ferreira BP, Resende EAMR, et al. Giant internal carotid artery aneurysm simulating pituitary adenoma. Arq Bras Endocrinol Metabol 2006;50:558–63 [DOI] [PubMed] [Google Scholar]
- 2.Ding D, Mehta GU, Liu KC. Pituitary insufficiency from large unruptured supraclinoid internal carotid artery aneurysm. Br J Neurosurg 2014; 28:290–2 [DOI] [PubMed] [Google Scholar]
- 3.Fernández-Real JM, Fernández-Castañer M, Villabona C, et al. Giant intrasellar aneurysm presenting with panhypopituitarism and subarachnoid hemorrhage: case report and literature review. Clin Investig 1994;72:302–6 [DOI] [PubMed] [Google Scholar]
- 4.Kayath MJ, Lengyel AM, Nogueira R, et al. Giant aneurysms of the sellar region simulating pituitary adenomas: a diagnosis to be considered. J Endocrinol Invest 1991;14:975–9 [DOI] [PubMed] [Google Scholar]
- 5.Lawson EA, Buchbinder BR, Daniels GH. Hypopituitarism associated with a giant aneurysm of the internal carotid artery. J Clin Endocrinol Metab 2008; 93:4616. [DOI] [PubMed] [Google Scholar]
- 6.Raymond LA, Tew J. Large suprasellar aneurysms imitating pituitary tumour. J Neurol Neurosurg Psychiatry 1978;41:83–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Verbalis JG, Nelson PB, Robinson AG. Reversible panhypopituitarism caused by a suprasellar aneurysm: the contribution of mass effect to pituitary dysfunction. Neurosurgery 1982;10:604–11 [DOI] [PubMed] [Google Scholar]
- 8.Heshmati HM, Fatourechi V, Dagam SA, et al. Hypopituitarism caused by intrasellar aneurysms. Mayo Clin Proc 2001;76:789–93 [DOI] [PubMed] [Google Scholar]
- 9.Tungaria A, Kumar V, Garg P, et al. Giant, thrombosed, sellar-suprasellar internal carotid artery aneurysm with persistent, primitive trigeminal artery causing hypopituitarism. Acta Neurochir (Wien) 2011;153:1129–33 [DOI] [PubMed] [Google Scholar]
- 10.Giustina A, Scalvini T, Cerudelli B, et al. Hypopituitarism secondary to suprasellar giant carotido-ophthalmic aneurysm. Normalization of the hypophyseal function after neurosurgical depression of the aneurysm. Minerva Endocrinol 1989;14:255–8 [PubMed] [Google Scholar]