Abstract
Objective: To assess the effect of chocolate on acne exacerbation in males between the ages of 18 and 35 with a history of acne vulgaris. Design: Double-blind, placebo-controlled, randomized, controlled trial. Setting: Single-site, outpatient, research, clinical facility at an academic research institution. Participants: Fourteen men between the ages of 18 and 35 were assigned to swallow capsules filled with either unsweetened 100-percent cocoa, hydrolyzed gelatin powder, or a combination of the two, at baseline. Measurements: Lesions were assessed and photographs were taken at baseline, Day 4, and Day 7. Results: Of the 14 subjects, 13 completed this Institutional Review Board approved study. A statistically significant increase in the mean number of total acneiform lesions (comedones, papules, pustules, nodules) was detected on both Day 4 (p=0.006) and Day 7 (p=0.043) compared to baseline. A small-strength positive Pearson’s correlation coefficient existed between the amount of chocolate each subject consumed and the number of lesions each subject developed between baseline and Day 4 (r=0.250), while a medium-strength positive correlation existed between baseline and Day 7 (r=0.314). No serious adverse events occurred. Conclusion: It appears that in acne-prone, male individuals, the consumption of chocolate correlates to an increase in the exacerbation of acne.
The effect that chocolate has on acne has been debated in the literature. Although it has been hypothesized that several factors, including body mass index (BMI), hormonal levels, glucose levels, emotional stress, and glycemic index, may have an effect on acne, the role of the diet in the generation and/or worsening of acne remains controversial.1 In 2002, Cordain et al2 demonstrated that Westerners have a higher percentage of the population suffering from acne vulgaris than two non-Westernized populations, including Kitavan Islanders of Papua New Guinea and Aché hunter-gatherers of Paraguay.2 Despite this, few studies have evaluated the effects of chocolate on acne.
One study of note was conducted in 1969 by Fulton et al.3 Sixty five subjects were assigned to consume either a chocolate bar that contained 10 times the amount of bittersweet chocolate of a normal 45g chocolate bar or a chocolate-less placebo bar that contained 28 percent vegetable fat corresponding with the fat content in chocolate liqueur and cocoa butter. Both bars weighed between 112 and 114g, although the control bar had 592 more calories than the experimental bar. The results demonstrated no significant difference between the two groups, suggesting that chocolate had no effect on acne.3 However, Mackie and Mackie4 criticized the study for the ingredients in the placebo bar that attempted to mimic the lipid and sugar contents of the chocolate bar. In addition, they criticized that the xanthine content was not mentioned for either bar.4 Rasmussen5 criticized Fulton’s method for lesion quantification, as all types of lesions (comedones, papules, and pustules) were accounted equally, thus not assessing the severity of the acne.
One other study that assessed the effect of chocolate on acne was conducted by Anderson. Twenty-seven medical students were administered six servings of 39g chocolate bars for seven days. Facial acneiform lesions were counted at baseline and then daily during the seven-day study. Although the methods used were not appropriately stated, the author did not observe a causal relationship between chocolate consumption and acne proliferation.6
Review of the literature in 2009 showed that there were no studies assessing the effects of chocolate with 100-percent content of cocoa on acne. In turn, the authors’ study team felt that it was necessary to conduct a study assessing pure chocolate on acne. In a recent pilot study published in the Journal of the American Academy of Dermatology, Berman et al7 assessed the effect of 100-percent cocoa on the exacerbation of acne in men between the ages of 18 and 35 years. At baseline, the study team had 10 healthy male subjects consume up to six ounces of 100-percent chocolate (Ghirardelli baking bars). Lesions were counted, assessed, and documented appropriately at baseline, Day 4, and Day 7. Statistical significance was achieved when the total mean number of acneiform lesions, including comedones, papules, and pustules, on Days 4 and 7 were compared to baseline (P=0.031 and 0.050 for Days 4 and 7, respectively). Additionally, strong positive Pearson’s correlations were calculated analyzing the amount of chocolate each subject consumed and the number of lesions subjects developed on Days 4 (r=0.510) and 7 (r=0.608). This dose-dependent relationship that was found suggested that chocolate did exacerbate acne in men with a history of acne vulgaris.7 However, this study did have limitations as only 10 subjects were included, and the study was not double-blinded nor placebo controlled. Therefore, the authors decided to expand on this pilot study and created an Institutional Review Board (IRB)-approved protocol to analyze the effect of chocolate’s exacerbation on acne in a double-blind, placebo-controlled study.
METHODS
The objective of this study was to assess the effect of chocolate on acne exacerbation in men between the ages of 18 and 35 with a history of acne vulgaris in a double-blind, placebo-controlled fashion. To this end, a single-center, prospective, double-blind, placebo-controlled study was conducted in which male subjects with very mild acne at baseline were assigned to swallow capsules filled with either unsweetened 100-percent cocoa, hydrolyzed gelatin powder, or a combination of the two, during a one-time binge consumption. The study team hand-filled the capsules with either six ounces of hydrolyzed gelatin, six ounces of cocoa powder, or a combination of varying quantities of cocoa powder (1, 2, 3, 4, or 5 oz) plus hydrolyzed gelatin (5, 4, 3, 2, or 1 oz, respectively) totaling six ounces, using a capsule encapsulation sheet (240 capsules were required for 6 oz of powder). All subjects were randomly assigned by blinded envelope to treatment dose (2 patients per treatment dose of 0, 1, 2, 3, 4, 5, or 6 oz cocoa). Subjects were intended to ingest the same number of total capsules; however, to account for varying quantities of ingestion in subjects, the combinations of cocoa/gelatin in varying quantities was homogenized prior to capsule filling. In order to be enrolled in the study, strict inclusion/exclusion criteria needed to be met.
Subjects needed to be postpubescent males between the ages of 18 and 35 years with minimal facial acne lesions defined as no less than one comedone and/or papule and no more than four comedones and/or papules at screening/baseline. In addition, subjects had no facial pustules at baseline, but had a history of acne vulgaris. Patients with pustules were excluded so that the researchers could better attribute any flare to their intervention in subjects who are predisposed to developing pustules, but who were currently well-controlled so that they could demonstrate the precipitation of the inflammatory flare triggered by cocoa, not confounded by another concurrent and pre-existing inflammatory process. Investigators ensured that subjects achieved a score of 0 or 1 on the Investigator’s Global Assessment Scale. Subjects signed an informed consent form, needed to have minimal sun exposure during the study, and needed to remain in the South Florida area during the one-week time period.
Female subjects were intentionally excluded from the study in order to remove the hormonal effects of menstruation on acne development. Additionally, patients with a history of diabetes mellitus or hypertriglyceridemia, as well as subjects diagnosed with obesity defined as a BMI of 30 or greater, were excluded. Patients known to have an allergic reaction to chocolate, those who were on any medications and/or supplements, and patients applying any over-the-counter or prescribed anti-acne medication including, but not limited to, retinoic acid, benzoyl peroxide, etc., over the past six weeks were not included. Subjects with a history of taking anti-acne oral medication (i.e., isotretinoin) during the past six months; taking drugs known to be photosensitizers, including phenothiazines, amiodarone, quinine, thiazides, tetracyclines, sulfonamides, quinolones; those who used facial topical, injectable, or systemic steroids six weeks prior to screening/baseline and during the study; or subjects currently taking any over-the-counter or prescribed medication for any condition, including but not limited to oral supplements and vitamin A, over the past two weeks were excluded. These subjects were excluded in order to minimize any possibly confounding effects on resultant lesions during the study period that could have possibly been attributed to inflammation from a local or systemic drug reaction. Finally, subjects with more than four comedones and/or papules at screening/baseline or those with one or more pustules and/or nodules at screening/baseline, did not meet inclusion criteria for enrollment.
After appropriate screening, informed consent was obtained at baseline. All appropriate demographic data, past and ongoing medical problems, concomitant medications, and acne score assessments, as well as IGA score assessments were recorded on the appropriate Case Report Forms (CRFs). The patient had photographs taken (one frontal view and two photos at 45° angles of each side of the face) using a NikonD70 digital camera. Following this, subjects were double-blindly assigned to swallow capsules filled with either unsweetened 100-percent cocoa, hydrolyzed gelatin powder, or a combination of the two at baseline during a one-time binge consumption.
At Day 4 (+/- 1 day) and Day 7 (+/- 1 day) of the study, similar procedures were performed with study personnel recording any adverse events, and medications were reviewed and recorded. Additionally, acne scores from lesions were enumerated and an Investigation Global Assessment (IGA) was performed. Photographs were repeated in an identical fashion to that at baseline and subject self-assessments were documented on the appropriate CRF pages. After gathering data, statistical analyses were performed using a standard student’s t-test as well as Pearson’s correlation coefficient.
RESULTS
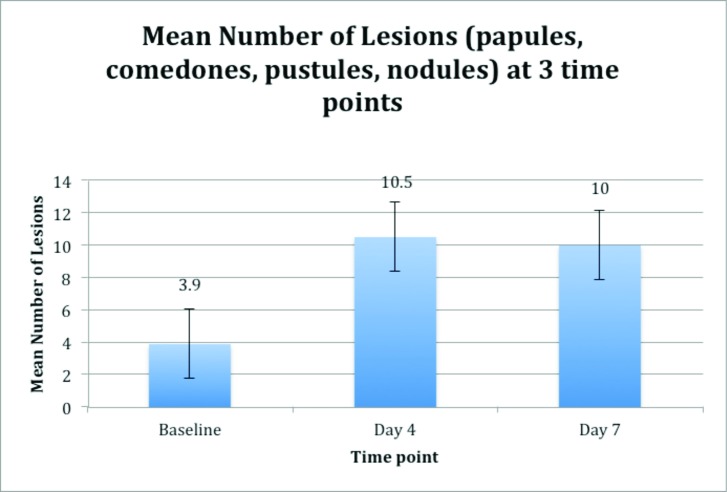
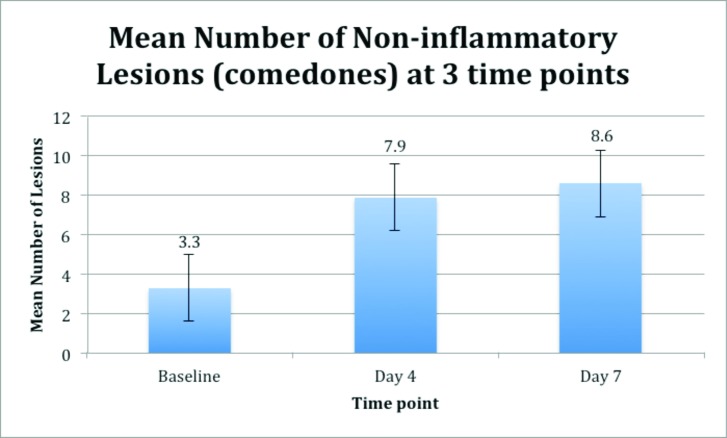
Thirteen of the 14 healthy male subjects were enrolled and completed this study. A statistically significant increase in the mean number of total acneiform lesions (comedones, papules, pustules, nodules) was detected on both Day 4 (p=0.006) and Day 7 (p=0.043) compared to baseline. However, statistical significance was not achieved when mean number of acneiform lesions on Days 4 and 7 were compared to each other (p=0.138) (Figure 1). There were significant increases from baseline at Days 4 and 7 in noninflammatory lesions (comedones), p=0.009 and p=0.042, respectively (Figure 2). Likewise, there was a significant difference from baseline to Day 4 in inflammatory lesions (papules, pustules, nodules), (p=0.008); but not from baseline to Day 7 (p=0.151) ( Figure 3). There were no statistically significant differences between Days 4 and 7 for either total (p=0.138), noninflammatory (p=0.310), or inflammatory (p=0.150) lesions (Figures 2 and 3).
Figure 1.
Effect of a one-time chocolate ingestion on total mean number of acneiform lesions (comedones, papules, pustules, nodules) at 3 time points (baseline, Day 4, and Day 7). A statistically significant increase in the mean number of total acneiform lesions (comedones, papules, pustules, nodules) was detected on both Day 4 (p=0.006) and Day 7 (p=0.043) compared to baseline. Statistical significance was not achieved when mean number of acneiform lesions on Days 4 and 7 were compared to each other (p=0.138).
Figure 2.
Effect of a one-time chocolate ingestion on the mean number of noninflammatory lesions (comedones) at 3 time points (baseline, Day 4, and Day 7). There were significant increases from baseline for Days 4 (p=0.009) and 7 (p=0.042). For Day 4 compared to Day 7, statistical significance was not achieved (p=0.310).
Figure 3.
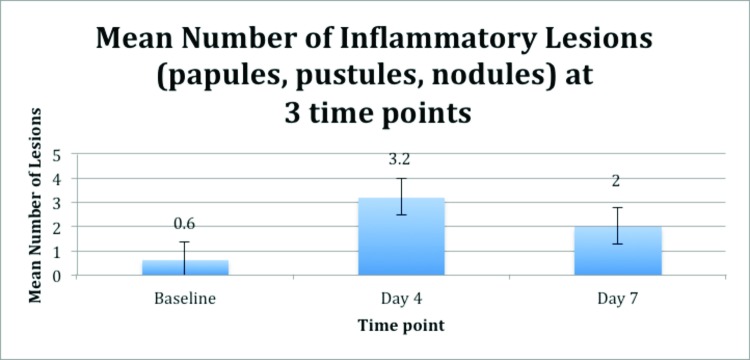
Effect of a one-time chocolate ingestion on the mean number of inflammatory lesions (papules, pustules, nodules) at 3 time points (baseline, Day 4, and Day 7). There was a significant difference from baseline to Day 4 (p=0.008), but not from baseline to Day 7 (p=0.151). For Day 4 compared to Day 7, statistical significance was not achieved (p=0.150).
When assessing correlations, a small-strength positive Pearson’s correlation coefficient existed between the amount of chocolate each subject consumed and the number of lesions each subject developed between baseline and Day 4 (r=0.250), while a medium-strength positive correlation existed between baseline and Day 7 (r=0.314) (Figure 4).
Figure 4.
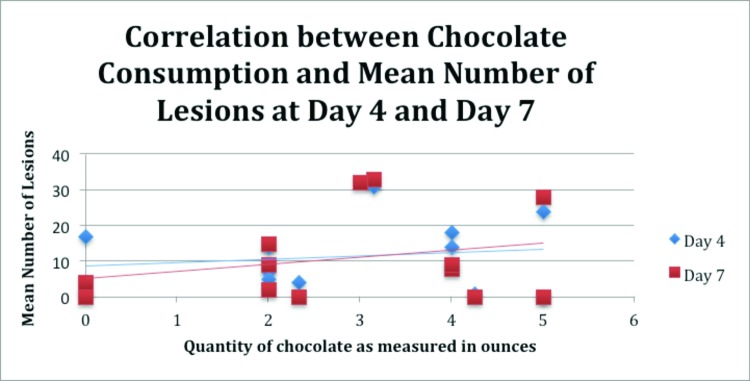
The medium-strength positive Pearson correlation coefficient between the amount of chocolate each subject consumed and the number of lesions each subject developed on Day 7 (r=0.314) and the small correlation for total lesions developed and amount of chocolate consumed between baseline and Day 4 (r=0.250). The blue diamond represents the total number of acneiform lesions a subject had on Day 4. Red squares represent the total number of acneiform lesions a subject had on Day 7.
Likewise, assessing only inflammatory lesions, and comparing baseline to Day 4 and baseline to Day 7, medium correlations existed (r=0.393 and r=0.474, respectively) (Figure 4). When comparing only noninflammatory lesions from baseline to Day 4, no correlation existed (r=0.044), while a small correlation (r=0.223) was present when comparing baseline to Day 7 (Figure 4).
No serious adverse events occurred during the study. Minor transient events included gastric discomfort, nausea, and vomiting. One subject vomited within an hour of consuming capsules and was discontinued from the study.
DISCUSSION
Despite the fact that there has been conflicting evidence regarding whether chocolate has an effect on acne or not, no studies were found in the literature that assessed the effect of 100-percent cocoa on acne exacerbation in a double-blind, placebo-controlled fashion. After ensuring that patients met stringent inclusion/exclusion criteria, and after significant attempts to remove any potentially confounding factors on the development of acne, this study supported the prior pilot study that suggested that chocolate does exacerbate acne in men between the ages of 18 and 35 years with a history of acne vulgaris.7 However, this study does have significant limitations that must be addressed.
The phenomenon of statistical significance in difference of mean inflammatory lesion count from baseline at Day 4, but not Day 7 is likely due to lack of power and small subject size, as the mean number of lesions at Day 4 was not statistically significant from the mean number of lesions at Day 7 (3.2 vs. 2, p=0.150). Although this sample size was larger than the aforementioned pilot study,7 14 subjects is a limited number. The minor transient events of gastric discomfort, nausea, and vomiting are unlikely to occur in patients who consume chocolate daily. Most people would refrain from consuming more chocolate if any gastrointestinal discomfort was experienced during consumption, and this was a one-time binge consumption of six ounces. Additionally, women were intentionally excluded, as hormonal fluctuations could have been a confounding factor in lesions that erupted during the study period. However, by not having women participate in this study, the generalizability of these results to the female population is greatly diminished. Additionally, the fact that only one brand of chocolate was used and no other brands of chocolate were studied limits the authors’ ability to generalize their results to all brands of chocolate or cocoa.
It should be noted that this is the only double-blind study that assesses the effect of chocolate on acne exacerbation in the literature. Therefore, although these limitations were apparent in the study, it appeared that in acne-prone, male individuals, the consumption of chocolate correlated to an increase in acneiform lesions. In addition, the small-medium dose-dependent relationship observed in subjects further supports the likelihood that the worsening of acne was due to the consumption of chocolate, supporting the results of the pilot study.7
Further investigation is warranted to investigate the specific components of cocoa that are contributing to the development of acneiform lesions in this population, and whether individual subjects’ sensitivities to these components or chemicals may be playing a role in the resultant inflammation.
ACKNOWLEDGMENT
There is no conflict of interest of other relevant industry relationships to declare by the authors. No sponsor was involved in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and/or preparation, review, or approval of the manuscript.
Footnotes
DISCLOSURE:The authors report no relevant conflicts of interest.
REFERENCES
- 1.James WD, Berger TG, Elston DM, editors. Acne. Andrews’ Diseases of the Skin: Clinical Dermatology, 10th ed. Philadelphia, PA: Saunders/Elsevier Inc; 2006. pp. 231–250. [Google Scholar]
- 2.Cordain L, Lindeberg S, Hurtado M, et al. Acne vulgaris: a disease of Western civilization. Arch Dermatol. 2002;138(12):1584–1590. doi: 10.1001/archderm.138.12.1584. [DOI] [PubMed] [Google Scholar]
- 3.Fulton JE, Jr, Plewig G, Kligman AM. Effect of chocolate on acne vulgaris. JAMA. 1969;15(11):2071–2074. [PubMed] [Google Scholar]
- 4.Mackie BS, Mackie LE. Chocolate and acne. Australas J Dermatol. 1974;15(3):103–109. doi: 10.1111/j.1440-0960.1974.tb00543.x. [DOI] [PubMed] [Google Scholar]
- 5.Rasmussen JE. Diet and acne. Int J Dermatol. 1977;16(6):488–492. doi: 10.1111/j.1365-4362.1977.tb01861.x. [DOI] [PubMed] [Google Scholar]
- 6.Anderson PC. Foods as the cause of acne. Am Fam Physician. 1971;3(3):102–103. [PubMed] [Google Scholar]
- 7.Block SG, Valins WE, Caperton CV, et al. Exacerbation of facial acne vulgaris after consuming pure chocolate. J Am Acad Dermatol. 2011;65(4):ell4–ell5. doi: 10.1016/j.jaad.2010.08.015. [DOI] [PubMed] [Google Scholar]
- 8.The Cocoa Bean. Ghirardelli Chocolate. [February 27, 2009]. www.ghirardelli.com/chocopedia/making_bean.aspx/
- 9.Berra B, Rizzo AM. Glycemic index, glycemic load, wellness and beauty: the state of the art. Clin Dermatol. 2009;27(2):230–235. doi: 10.1016/j.clindermatol.2008.04.006. [DOI] [PubMed] [Google Scholar]
- 10.Goulden V, McGeown CH, Cunliffe WJ. The familial risk of adult acne: a comparison between first-degree relatives of affected and unaffected individuals. Br J Dermatol. 1999;141(2):297–300. doi: 10.1046/j.1365-2133.1999.02979.x. [DOI] [PubMed] [Google Scholar]
- 11.Nutrition Facts Baking chocolate, unsweetened, squares. [February 27, 2009]. www.nutritiondata.com/facts/sweets/5390/2
- 12.Smith RN, Mann NJ, Braue A, et al. A low-glycemic-load diet improves symptoms in acne vulgaris patients: a randomized controlled trial. Am J Clin Nutr. 2007;86(1):107–115. doi: 10.1093/ajcn/86.1.107. [DOI] [PubMed] [Google Scholar]
- 13.Kaymak Y, Adisen E, liter N, et al. Dietary glycemic index and glucose, insulin, insulin-like growth factor-I, insulin-like growth factor binding protein 3, and leptin levels in patients with acne. J Am Acad Dermatol. 2007;57(5):819–823. doi: 10.1016/j.jaad.2007.06.028. [DOI] [PubMed] [Google Scholar]
- 14.Calories in Ghirardelli Chocolate—100% Cacau Baking Bar. My Fitness Pal. [May 1, 2014]. http://www.myfitnesspal.com/food/calories/ghirardelli-dark-chocolate-100-cacao-unsweetened-baking-bar-112470531