Abstract
Acne scarring is a consequence of abnormal resolution of wound healing after damage that occurs in the sebaceous follicle during acne inflammation. No trial to date has evaluated the efficacy of the combination of microdermabrasion and photodynamic therapy for acne scarring. This single-center, double-blinded pilot study enrolled subjects with moderate-to-severe acne scarring who were randomly assigned in a blinded fashion to use aminolevulinic acid and vehicle in a split-face fashion after full-face treatment with microdermabrasion. On average, 80 percent of the patients displayed more improvement in scarring on the aminolevulinic acid split face versus the vehicle split face after five treatments. Using two different noninvasive mechanisms of targeting acne scarring provided for a safe treatment regimen characterized by more efficacious results with respect to higher rates of scarring improvement.
Acne affects nearly 80 percent of adolescents and young adults. A recent community-based study of close to 800 subjects reported the overall acne scarring prevalence to be 14 percent in women and 11 percent in men.1 Severe scarring caused by acne is associated with substantial physical and psychological distress and has been associated with poor self-esteem, emotional debilitation, and lowered academic performance.2
Acne scarring is a consequence of abnormal resolution of wound healing after damage that occurs in the sebaceous follicle during acne inflammation.3 The cause is due to either increased formation of tissue (hypertrophic scars or keloids) or damage to tissue (ice pick, rolling, and boxcar scars), leaving atrophic scars. All types of acne, from papulopustular to nodulocystic disease, can cause scarring; therefore, adequate treatment must be started early.4 Of the therapeutic approaches available for acne scarring, microdermabrasion represents a noninvasive efficacious treatment for contour irregularities. A molecular trial showed that after a single microdermabrasion treatment, matrix metalloproteinases involved in dermal remodeling and wound healing were upregulated in the biopsies taken from subjects with severe acne scarring.5
Photodynamic therapy (PDT) involves the topical administration of aminolevulinic acid (ALA) and has been successfully utilized as a noninvasive treatment modality for acne. While not photosensitive by itself, ALA is converted by keratinocytes to protoporphyrin IX, which is a photosensitive compound that is activated by a blue light source. The reactive oxygen species formed in this reaction produce beneficial immunological changes. In the murine contact hypersensitivity model, PDT-ALA was found to cause local immunosuppression by decreasing the number of epidermal Langerhans cells, a finding which suggests that PDT has a potential immunological contribution to clinical efficacy for inflammatory diseases.
Additionally, PDT has been shown to stimulate various matrix metalloproteinases, which may explain the collagen remodeling produced by this method. The side effect profile of topical ALA-PDT is extremely favorable, with mild pain and temporary cutaneous photosensitivity reported as the most frequent documented adverse effects. Many studies concerning the anti-inflammatory effects of PDT on acne have been published; however, a study specifically focusing on the use of PDT for acne scarring has yet to be conducted.
No trial to date has evaluated the efficacy of the combination of microdermabrasion and ALA-PDT for acne scarring. However, targeting acne scarring with microdermabrasion followed by ALA-PDT appears to be logical. The authors hypothesize that the ability to increase the permeability barrier via the use of microdermabrasion will enhance the absorption of 5-ALA and thereby increase the efficacy of the combination treatment for acne scarring. They also hypothesize that utilizing microdermabrasion prior to application of ALA will speed the acid’s absorption, shortening the incubation time needed to 60 minutes, which could greatly enhance both patient convenience and physician productivity.
The efficacy of the combination procedure may provide for a faster, yet longer-sustained clearance effect. In summary, by using two different mechanisms of targeting acne scarring, the authors expect to have more efficacious results with respect to higher rates of scarring improvement. They also hope to bring to the forefront a new therapeutic regimen for acne scarring, which combines two provider-applied modalities.
METHODS
This single-center, double-blinded study enrolled subjects with moderate-to-severe acne scarring who were randomly assigned in a blinded fashion to use ALA and vehicle in a split-face fashion after full-face treatment with microdermabrasion. Each subject was advised to wash the treatment area with soap and water. The treatment area was then degreased with isopropyl alcohol. A standard aluminum oxide microdermabrasion system was utilized to perform three passes in different directions (vertical, horizontal, and oblique) over the treated skin area. Either a solution of 20% δ-aminolevulinic acid (commercially available as Levulan Kerastick, Dusa: ALA-PDT) or vehicle solution alone (vehicle-PDT, supplied by Dusa) was applied topically to either the right or left sides of the face for a 60-minute incubation period. After incubation, lesions were illuminated with 417nm blue light (Blu-U Blue Light Photodynamic Therapy Illuminator) with irradiance of 10mW/cm2 for 1,000 seconds, with a total light dose of 10J/cm2.
A therapeutic course of five consecutive treatments four weeks apart was used. The acne scarring treatment response was evaluated by utilizing the Physician’s Global Assessment of Acne Scarring scale (PGA, Table 1) and with the help of clinical digital photography, on entry into the study and at each follow-up visit prior to treatment. Adverse effects, including pain, phototoxic parameters (e.g., erythema, edema, and crusting), and pigmentary changes, were documented using a 10-point scale (0=none; l-3=mild; 4-6=moderate; 7-9=severe) during and immediately after each treatment.
TABLE 1.
Physician Global Scale for Acne Scar Severity (PGA)
| CATEGORY | SCORE | DESCRIPTION |
|---|---|---|
| Clear | 0 | No visible scars from acne |
| Almost clear | 1 | Hardly visible scars from 2.5m away |
| Mild | 2 | Easily recognizable; less than half the face involved |
| Moderate | 3 | More than half the face involved |
| Severe | 4 | Entire face involved |
| Very severe | 5 | Entire face with prominent atrophic or hypertrophic scars |
Overall, six patients were enrolled with five patients completing the study (Table 2). Healthy adult patients with either ice pick, rolling, or boxcar atrophic acne scars on the face with a PGA of at least 3 (moderate severity) were included. Females of childbearing potential were required to have a negative urine pregnancy test prior to study treatment initiation and agreed to use an approved method of birth control during the study period (barrier, oral, injection, intrauterine). Females who were pregnant, breastfeeding, or attempting to conceive were excluded as well as those with a history of known or suspected intolerance to any of the excipients of ALA or any of its vehicle components. Subjects with a history of cutaneous photosensitization (including porphyria or systemic lupus erythematosus), active skin malignancy or infection, and those taking any photosensitizing medications were excluded. All medications, topical and oral, known to alter the course of acne scarring or acne vulgaris taken within two weeks of initiation or during the study period were prohibited.
Table 2.
Patient characteristics
| PATIENT NUMBER | FITZPATRICK SKIN TYPE | AGE(YEARS) | SEX | PREDOMINANT SCAR TYPE | SCAR AGE(YRS) |
|---|---|---|---|---|---|
| 1 | 1 | 46 | F | ice pick > boxcar | 25 |
| 2 | 3 | 45 | F | boxcar | 33 |
| 3 | 4 | 28 | F | ice pick> atrophic | 5 |
| 4 | 4 | 39 | F | boxcar > icepick | 10 |
| 5 | 4 | 26 | F | atrophic > boxcar | 10 |
RESULTS
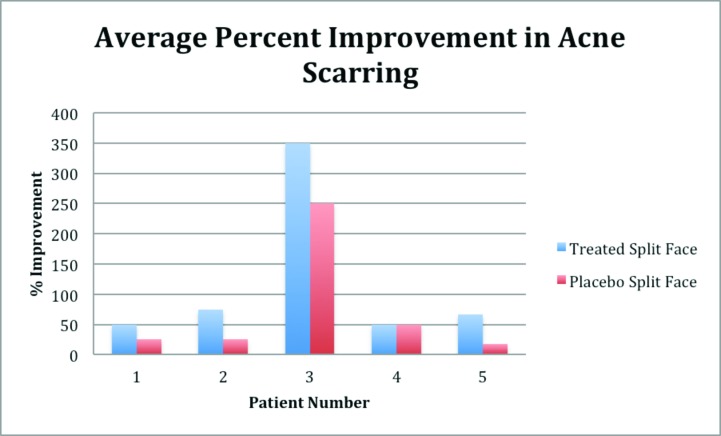
Two blinded assessors reviewed pretreatment and end-of-study split- and full-face photographs taken at each visit and evaluated acne scar severity (Figure 1). On average, 80 percent of the patients displayed more improvement in scarring on the ALA split face versus the vehicle split face (Figure 2). Subject three had a significantly higher improvement of acne scarring (250% improvement on the placebo side, 350% improvement on the treatment side) as compared to the other subjects. Patient questionnaires revealed that 80 percent of patients appreciated an improvement in the acne scarring. At the end of study visit, three of the five patients were able to correctly discern which split face was treated with ALA versus vehicle.
Figure 1.
Blinded assessments of acne scarring
Figure 2.
Improvement in acne scarring seen bilaterally, but more apparent on panels A and B, baseline and end of study for ALA-PDT. A. Left split face: baseline; B. Left split face: end of study ALA-PDT; C. Right split face: baseline; D. Right split face: end of study vehicle-PDT
DISCUSSION
Acne scarring represents a common dermatological complaint for which there is no gold standard in management. A recent study showed that not everyone who develops acne has a propensity to scar. Comparing biopsies of inflamed lesions taken from acne subjects who tend to scar versus those who do not, Holland et al3 showed an elevation of cellular activation, represented by a macrophagic infiltration, in biopsies from the scarring cohort. The authors believed that this chronic delayed-type hypersensitivity reaction resulted from persistent antigen-like Propionibacterium acnes, the bacterium that not only is responsible for forming inflammatory acne, but also has been found to remain intracellularly. The disparity in cell profiles could explain the differences in the quality of wound repair. Lymphocytes and macrophages secrete an extensive array of cytokines and growth factors, which are known to modulate dermal fibroblast recruitment and proliferation. This immunological effect is hypothesized to contribute to wound remodeling and contraction, which represent contributory factors in scarring. Thus, the type and magnitude of the inflammatory response in resolving lesions from scarring subjects may lead to abnormal healing and eventual pathological lesions.3
Current noninvasive treatment modalities for atrophic acne scars include chemical peels, soft tissue augmentation, sub-scision, and punch excision. However, none of these accepted modalities are able to affect the immunological milieu responsible for scarring or prevent new subclinical lesions from appearing. This unique anti-inflammatory property of PDT makes this an ideal treatment option for acne scarring. The majority of patients enrolled in this study showed the beneficial effects of the combination treatment of microdermabrasion with PDT. However, it should be noted that microdermabrasion with blue light treatment also did provide split-face minimal relief of acne and scars in various patients. These results support the idea that blue light alone has intrinsic antimicrobial effects without the added use of photosensitizers.12
One retrospective study evaluating whether patients with histories of surgically treated nonmelanoma skin cancers who were then treated with either ALA-PDT or MAL-PDT for field cancerization prophylaxis indicated that PDT-induced scar remodeling changes did occur in surgical scars in the treatment field. The degree of improvement correlated closely with the number of treatment sessions that occurred (P<0.05 for two or three treatments). Sakamoto et al13 suggested that ALA-PDT mediated remodeling of surgical scars may involve changes to dermal collagen as a result of matrix metalloproteinase activation.
To the authors’ knowledge, this is the first trial to evaluate the efficacy of the combination of microdermabrasion and ALA-PDT for acne scarring. Their results show an improvement in acne scarring can be achieved with topical use of microdermabrasion in combination with PDT. The ideal candidate for this dual modality regimen is the subject with moderate-to-severe acne scarring who may also have concomitant mild-to-moderate acne vulgaris. Given the safety profile of these treatments, this management option would be suited for those who are looking for a less expensive and less invasive means to resurfacing the skin while also alleviating lesional and subclinical acne. It is unclear as to why Subject 3 experienced a much higher response to both the placebo and treatment sides as compared to the other subjects. This particular patient was refractory to a variety of other topical and oral treatments (doxycycline and isotretinoin) in the past, but served as an ideal candidate for this combination treatment regimen.
Given the nature of this pilot study, only five patients were enrolled, which limited the capacity to conduct advanced statistical analysis. Future studies involving more subjects with longer follow-up period would better solidify the beneficial relationship between PDT and acne scarring in terms of rate and duration of clearance of scars and lesions. Additional future trials involving the use of acne surgery prior to ALA-PDT treatments might provide for increased efficacy rate, especially for those patients with refractory comedonal acne. In conclusion, using two different noninvasive mechanisms of targeting acne scarring provided for a safe treatment regimen characterized by more efficacious results with respect to higher rates of scarring improvement.
Footnotes
DISCLOSURE:The authors report no relevant conflicts of interest.
REFERENCES
- 1.Goulden V, Stables GI, Cunliffe WJ. Prevalence of facial acne in adults. J Am Acad Dermatol. 1999;41(4):577–580. [PubMed] [Google Scholar]
- 2.Koo J. The psychosocial impact of acne: patients’ perceptions. J Am Acad Dermatol. 1995;32(5 Pt 3):S26–S30. doi: 10.1016/0190-9622(95)90417-4. [DOI] [PubMed] [Google Scholar]
- 3.Holland DB, Jeremy AH. The role of inflammation in the pathogenesis of acne and acne scarring. Semin Cutan Med Surg. 2005;24(2):79–83. doi: 10.1016/j.sder.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 4.Layton AM, Henderson CA, Cunliffe WJ. A clinical evaluation of acne scarring and its incidence. Clin Exp Dermatol. 1994;19(4):303–308. doi: 10.1111/j.1365-2230.1994.tb01200.x. [DOI] [PubMed] [Google Scholar]
- 5.Karimipour DJ, Rittie L, Hammerberg C, et al. Microdermabrasion: a molecular analysis following a single treatment. J Am Acad Dermatol. 2005;52(2):215–223. doi: 10.1016/j.jaad.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 6.Zelickson BD. Mechanisms of action of topical aminolevulinic acid. In: Goldman MP, editor. Photodynamic Therapy. 1st ed. Philadelphia: Elsevier. Saunders.; 2005. pp. 1–12. [Google Scholar]
- 7.Marcus SL, Mclntyre WR. Photodynamic therapy systems and applications. Expert Opin Emerg Drugs. 2002;7(2):321–334. doi: 10.1517/14728214.7.2.321. [DOI] [PubMed] [Google Scholar]
- 8.Hryhorenko EA, Oseroff AR, Morgan J, Rittenhouse-Diakun K. Deletion of alloantigen-activated cells by aminolevulinic acid-based photodynamic therapy. Photochem Photobiol. 1999;69(5):560–565. [PubMed] [Google Scholar]
- 9.Kalka K, Merk H, Mukhtar H. Photodynamic therapy in dermatology. J Am Acad Dermatol. 2000;42(3):389–413. doi: 10.1016/s0190-9622(00)90209-3. quiz 414-416. [DOI] [PubMed] [Google Scholar]
- 10.Nielsen KP, Juzeniene A, Juzenas P, et al. Choice of optimal wavelength for PDT: the significance of oxygen depletion. Photochem Photobiol. 2005;81(5):1190–1194. doi: 10.1562/2005-04-06-RA-478. [DOI] [PubMed] [Google Scholar]
- 11.Bruls WA, Slaper H, van der Leun JC, Berrens L. Transmission of human epidermis and stratum corneum as a function of thickness in the ultraviolet and visible wavelengths. Photochem Photobiol. 1984;40(4):485–494. doi: 10.1111/j.1751-1097.1984.tb04622.x. [DOI] [PubMed] [Google Scholar]
- 12.Dai T, Gupta A, Murray CK, et al. Blue light for infectious diseases: Propionibacterium acnes, Helicobacter pylori, and beyond? Drug Resist Update. 2012;15(4):223–236. doi: 10.1016/j.drup.2012.07.001. Epub 2012 Jul 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sakamoto FH, Izeikson L, Tannous A, et al. Surgical scar remodelling after photodynamic therapy using aminolaevulinic acid or its methyester: a retrospective, binded study of patients with field cancerization. Brit J Dermatol. 2001;166:413–416. doi: 10.1111/j.1365-2133.2011.10576.x. [DOI] [PubMed] [Google Scholar]