Abstract
Introduction: Patients with abdominal pain often return multiple times despite no definitive diagnosis. Our objective was to determine if repeat emergency department (ED) use among patients with non-specific abdominal pain might be associated with a diagnosis of moderate to severe depressive disorder.
Methods: We screened 987 ED patients for major depression during weekday daytime hours from June 2011 through November 2011 using a validated depression screening tool, the PHQ-9. Each subject was classified as either no depression, mild depression or moderate/severe depression based on the screening tool. Within this group, we identified 83 patients with non-specific abdominal pain by either primary or secondary diagnosis. Comparing depressed patients versus non-depressed patients, we analyzed demographic characteristics and number of prior ED visits in the past year.
Results: In patients with non-specific abdominal pain, 61.9% of patients with moderate or severe depression (PHQ9≥10) had at least one visit to our ED for the same complaint within a 365-day period, as compared to 29.2% of patients with no depression (PHQ9<5), (p=0.013).
Conclusion: Repeat ED use among patients with non-specific abdominal pain is associated with moderate to severe depressive disorder. Patients with multiple visits for abdominal pain may benefit from targeted ED screening for depression. [West J Emerg Med. 2014;15(3):325–328.]
INTRODUCTION
Patients with gastrointestinal (GI) complaints are common to emergency departments (EDs) and may be recipients of inefficient and expensive testing.1 ED patients with non-specific abdominal pain may have an association with psychiatric disorders similar to the association observed with functional GI disorders, a highly prevalent class of diseases that comprise 40% of U.S. gastroenterology practice and are strongly associated with depression and anxiety.2,3 Despite an increase in testing, many ED patients are discharged with a diagnosis of non-specific abdominal pain.4 New diagnostic and therapeutic strategies are needed to care for this large group of patients. This study is important to identify a group of patients who may clinically benefit from targeted psychiatric screening to improve their quality of care and ultimately provide more efficient use of diagnostic tests. Our objective was to determine if repeat ED use among patients with non-specific abdominal pain might be associated with a diagnosis of moderate to severe depressive disorder.
METHODS
This research was conducted at an academic urban ED that has approximately 70,000 visits annually. We used a cross-sectional design with an oversample of patients with a history of 4 or more visits in the 365-day period. Patients were selected from the general pool of ED patients. Inclusion criteria were English fluency, aged 18 years or older, and chief complaint of a non-psychiatric complaint. Exclusion criteria included the presence of a primary psychiatric complaint, prisoner status, intoxication, mental status changes and critical illness. Subjects were enrolled by trained research assistants from June 2011 through November 2011 on weekdays between 9AM and 8PM. We measured patient illness with standard physician diagnostic codes (International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9]). We analyzed the subset of respondents with non-specific abdominal pain as their primary or secondary diagnosis (ICD-9 code of 789.xx). Eligible patients were asked questions about their demographic, psychiatric, medical and healthcare characteristics. Each patient was screened with the Patient Health Questionnaire-9 (PHQ-9), a 9-item depression scale based on the Diagnostic and Statistical Manual Fourth Edition (DSM-IV.)
To determine repeat use, we captured the index visit date of each patient's ED visit at the time of enrollment, and the number of previous ED visits in the prior year (365 days) was captured by the electronic health record (Picis 5.0.) ED visit frequency was determined by the number of visits during a 365-day period (including the index visit). We chose ED use risk factors according to a literature review, which we grouped into patient demographic, illness and concurrent healthcare use categories. Demographic factors were measured at the index ED visit.
Our principal outcome was the number of repeat ED visits, defined as 1 or more visits for abdominal pain within a 364-day period prior to the index visit. We conducted a chi-squared analysis to compare multiple ED visits among abdominal pain patients with a positive depression screen versus those with a negative depression screen. Results were computed using STATA version 11. The study was approved by our medical center's institutional review board.
RESULTS
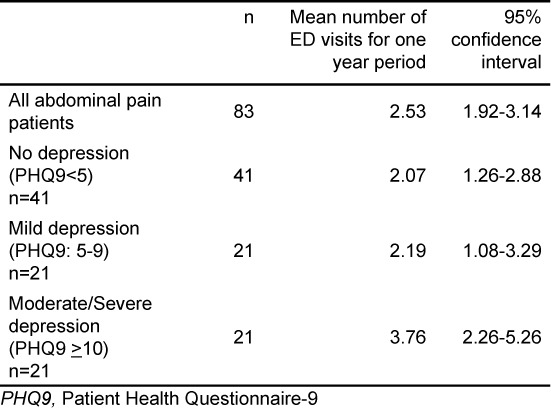
We approached a total of 1,116 patients over the course of the study, and 1,012 patients (90.7% response rate) consented to screening. Of those who consented, 987 respondents (97.5%) completed the PHQ-9 and had information available about prior visits. Eighty-three subjects were given a primary or secondary diagnosis of non-specific abdominal pain (74 primary, 9 secondary). The average age of patients with non-specific abdominal pain was 36.2 and 73% were female. Of patients with non-specific abdominal pain, 41 (49.4%) had a negative depression screen (PHQ-9< 5); 21 (25.3%) had a mild depression screen (PHQ-9, 5-≤9); and, 21 (25.3%) had moderate or severe depression screen (PHQ-9>10) (Table 1). Overall, 34 (41.0%) patients with non-specific abdominal pain had more than one visit to the ED in the year prior to index visit. When analyzing by depression, 61.9% of patients with moderate/severe depression had at least one prior visit for abdominal pain as compared to only 29.2% of patients with a negative depression screen. (Table 2). On average, patients with non-specific abdominal pain with moderate/severe depression had 3.76 visits (95% confidence interval [CI] 2.26–5.26) as compared to 2.19 visits among patients with abdominal pain and mild depression (95% CI 1.08–3.29) and 2.07 visits (95% CI 1.26–2.88) among patients with abdominal pain and a negative depression screen (Table 3).
Table 1.
Demographics and characteristics of patients in the emergency department per level of depression for depression cohort (n=83).
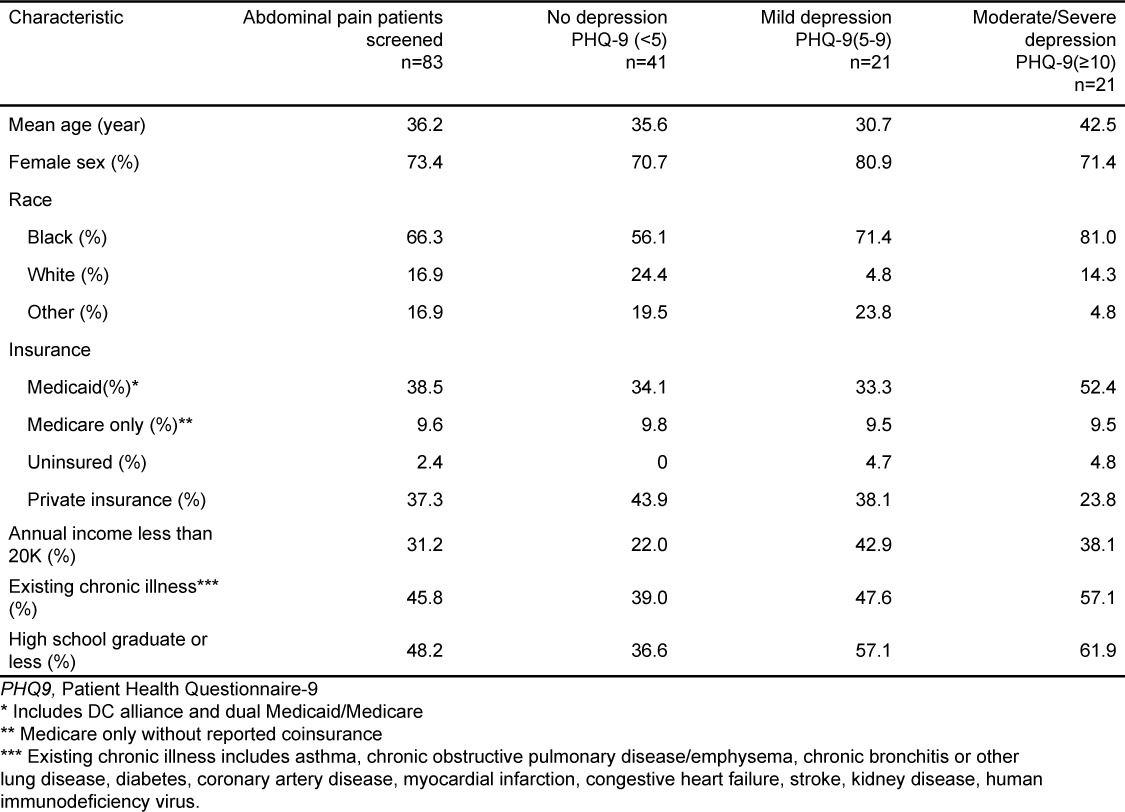
Table 2.
Emergency department (ED) use for patients with primary or secondary diagnosis of abdominal pain (n=83) analyzed by level of depression.
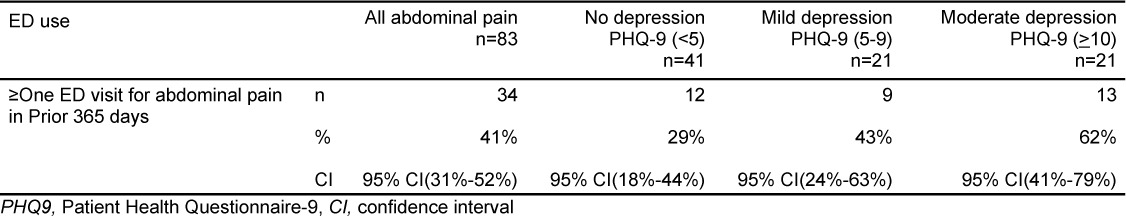
Table 3.
Average number of emergency department (ED) visits for year by category.
DISCUSSION
In our study of 83 subjects with non-specific abdominal pain, we found an association between serial visits and depression. Understanding this association may have significant public health implications. This association may be due to the fact that patients who return to the ED on multiple occasions are more likely to have a chronic medical condition. In general, chronic medical conditions are known to be associated with depression.6 In addition, functional GI disorders, which include syndromes such as irritable bowel syndrome, functional dyspepsia and cyclic vomiting syndrome, also demonstrate a strong association with psychiatric disorders such as depression and anxiety.2
Depressed patients may be less likely than non-depressed patients to have established access to healthcare avenues other than the ED. Depression is associated with cognitive symptoms such as deficits in executive functioning, memory and concentration, and the ED is a relatively easy healthcare access point compared to other mental health services.7 The cognitive symptoms associated with depression may increase the likelihood for ED recidivism.8 In general, depressed patients may be more likely to use the ED for all of their healthcare needs.
Abdominal pain may also be a form of somatization, defined as the misattribution of physical symptoms to medical rather than psychiatric causes. Somatization is a common “idiom of distress” used by both healthy and psychiatrically ill individuals to communicate intra-psychic or interpersonal stress to care givers.9 Patients with depressive illnesses frequently represent their psychological distress in physical terms. When these patients are found not to have any emergent medical illness, they may be discharged without addressing the psychiatric root of their visit. As the source of distress is left unresolved, patients may repeatedly visit the ED when intra-psychic or psychosocial stressors worsen.
For many patients with psychosocial concerns, traditional biomedical language shapes their experience. Lower socioeconomic status, limited education, alcoholism and social dysfunction in family background are known risk factors for somatoform disorders. The major complications are iatrogenic and include unnecessary surgery, repeated medical work-ups, drug dependence and side effects. In addition to depression, associated conditions include functional somatic syndromes, irritable bowel syndrome, non-ulcer dyspepsia, premenstrual syndrome, chronic pelvic pain, fibromyalgia, atypical or non-cardiac chest pain, hyperventilation syndrome, chronic fatigue syndrome, tension headache, temporomandibular joint dysfunction, atypical facial pain, globus syndrome, multiple chemical sensitivity. Particularly relevant to EM physicians, a somatoform syndrome diagnosis is difficult to make or rule out the diagnosis in a single visit.10
Patients with psychiatric disorders may fear the stigmatization of a mental health disorder. The stigma associated with depression may influence patients not to discuss the symptoms with their families, friends and healthcare providers.11 Therefore, depressed patients may be more likely to seek care in the ED rather than from mental health professionals. Since their psychiatric symptoms may not be addressed, patients may revisit frequently without appropriate diagnosis. If diagnosed, brief psychodynamic interpersonal psychotherapy is associated with improved quality of life in patients with somatoform disorder.12
The PHQ-9 was administered to all patients at index visit. A 9-item depression scale based on Diagnostic and Statistical Manual Fourth Edition (DSM-IV) diagnostic criteria for major depression, it is composed of 2 components: 1) assessment of symptoms and functional impairment to make a preliminary diagnosis of depression and 2) severity score to evaluate needed treatment. The PHQ-9 is has shown good validity in capturing both the diagnosis of depression, as well as current depression severity, and has been shown to be useful in a number of outpatient primary care settings when time limitations may be a concern. In one study, a PHQ-9 score of 10 and higher had a sensitivity of 88% and a specificity of 88% for moderate depression. Scores of 5, 10, 15, and 20 represented mild, moderate, moderately severe, and severe depression.5
LIMITATIONS
The first limitation concerns the small sample size, which has limited our ability to control for potential confounding factors such as insurance status, income levels, co-morbidities and presence of primary care. In addition, we were unable to compare the association of depression in patients with non-specific abdominal pain versus those with documented organic disease. The second limitation of this study is the result of the convenience sample that may create a selection bias. We attempted to address this issue by querying the electronic medical record for the demographics of all ED abdominal pain patients seen during study dates and demonstrated no differences in age, sex and racial characteristics. An additional limitation of the study is related to our determination that ED visits were made by retrospective review from the index visit. Ideally, we would follow patients forward to determine if depression predicted future high use. Study patients could have exhibited signs of depression at enrollment simply because they had to return to the ED again not because of the association with abdominal pain.
CONCLUSION
In conclusion, repeat ED use among patients with non-specific abdominal pain is associated with moderate to severe depressive disorder. ED physicians should consider the diagnosis of depression in patients with non-specific abdominal pain or consider screening patients with multiple visits for non-specific abdominal pain for depression. More study is needed to confirm this association and determine how best to manage it.
Footnotes
Conflicts of Interest: By the WestJEM article submission agreement, all authors are required to disclose all affiliations, funding sources and financial or management relationships that could be perceived as potential sources of bias. The authors disclosed none.
Supervising Section Editor: Michael P. Wilson, MD, PhD
Full text available through open access at http://escholarship.org/uc/uciem_westjem
REFERENCES
- 1.Ford JD, Trestman RL, Steinberg K et al. Prospective association of anxiety, depressive, and addictive disorders with high utilization of primary, specialty and emergency medical care. Soc Sci Med. 2004;58(11):2145–2148. doi: 10.1016/j.socscimed.2003.08.017. [DOI] [PubMed] [Google Scholar]
- 2.Design of Treatment Trials Committee. Irvine EJ, Whitehead WE et al. Design of treatment trials for functional gastrointestinal disorders. Gastroenterology. 2006;130(5):1538–1551. doi: 10.1053/j.gastro.2005.11.058. [DOI] [PubMed] [Google Scholar]
- 3.Wu JCY. Psychological co-morbidity in functional gastrointestinal disorders: Epidemiology, mechanisms and management. Neurogastroenterol Motility. 2012;18(1):13–18. doi: 10.5056/jnm.2012.18.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pines JM. Trends in the rates of radiography use and important diagnoses in emergency department patients with abdominal pain. Med Care. 2009;47(7):782–786. doi: 10.1097/MLR.0b013e31819748e9. [DOI] [PubMed] [Google Scholar]
- 5.Kroenke K, Spitzer RL, Williams JBW et al. The patient health questionnaire somatic, anxiety, and depressive symptom scales: A systematic review. Gen Hosp Psychiatry. 2010;32(4):345–359. doi: 10.1016/j.genhosppsych.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 6.Alderson SL, Foy R, Glidewell L et al. How patients understand depression associated with chronic physical disease - A systematic review. BMC Family Practice. 2012:13. doi: 10.1186/1471-2296-13-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee RSC, Hermens DF, Porter MA et al. A meta-analysis of cognitive deficits in first-episode major depressive disorder. J Affect Disord. 2012;140(2):113–124. doi: 10.1016/j.jad.2011.10.023. [DOI] [PubMed] [Google Scholar]
- 8.Girts TK, Crawford AG, Goldfarb NI et al. Predicting high utilization of emergency department services among patients with a diagnosis of psychosis in a medicaid managed care organization. Disease Management. 2002;5(4):189–196. [Google Scholar]
- 9.Surdea-Blaga T, Baˇban A, Dumitrascu DL. Psychosocial determinants of irritable bowel syndrome. World J Gastroenterol. 2012;18(7):616–626. doi: 10.3748/wjg.v18.i7.616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Simon GE, Gureje O. Stability of somatization disorder and somatization symptoms among primary care patients. Arch Gen Psychiatry. 1999;56(1):90. doi: 10.1001/archpsyc.56.1.90. [DOI] [PubMed] [Google Scholar]
- 11.Cabello M, Mellor-Marsá B, Sabariego C et al. Psychosocial features of depression: A systematic literature review. J Affect Disord. 2012;141(1):22–33. doi: 10.1016/j.jad.2011.12.009. [DOI] [PubMed] [Google Scholar]
- 12.Sattel H, Lahmann C, Gundel H et al. Brief psychodynamic interpersonal psychotherapy for patients with multisomatoform disorder: Randomised controlled trial. Br J Psychiatry. 2012;200:60–67. doi: 10.1192/bjp.bp.111.093526. [DOI] [PubMed] [Google Scholar]


