Abstract
We reviewed the literature on nonrecreational prescription medication sharing. We searched PubMed, EMBASE, PsycINFO, and a customized multidatabase for all relevant articles published through 2013; our final sample comprised 19 studies from 9 countries with 36 182 participants, ranging in age from children to older adults, and published between 1990 and 2011.
The prevalence rate for borrowing someone’s prescription medication was 5% to 51.9% and for lending prescription medication to someone else was 6% to 22.9%. A wide range of medicines were shared between family members, friends, and acquaintances.
Sharing of many classes of prescription medication was common. Further research should explore why people share, how they decide to lend or borrow, whether they are aware of the risks, and how they assess the relevance of those risks.
Medication sharing is defined as the lending or borrowing of prescription medications where the recipient of those medicines is someone other than the person for whom the prescription is intended.1 In other contexts, “lending” and “borrowing” imply a temporary transfer that will be returned, but these terms are used loosely in the literature regarding prescription medications, which are often not replaced into the supply of the person to whom the medication was prescribed. A previous review article pointed out the negative consequences of medicine sharing, such as unanticipated adverse events, complications of incorrect use, delay in seeking professional help, antibiotic resistance, and addiction or misuse related to the addictive properties of some medications,2 but empirical research is limited.
Medication sharing has 2 distinct types; recreational and nonrecreational. Recreational sharing is the sharing of abusable prescription medications to get high, to relax, or for experimentation. Nonrecreational sharing is the sharing of any prescription medication for medical use or altruistic reasons.3 Both represent nonprescribed use of medication.
Past research on medication sharing has tended to focus on recreational sharing.4–10 Nonrecreational sharing has not received much research attention,2,3 and little information describing prevalence and practices of nonrecreational sharing has been published. Moreover, no previous systematic review has attempted to reveal the types of medicines shared, determinants of nonrecreational sharing, and consequences of sharing practices.
Researchers have reported a correlation between sociodemographic variables and prescription medicine diversion practices (i.e., trading, selling, or sharing of prescribed medicines).5,7,10,11 By and large, adolescent girls are more likely than adolescent boys7 and younger adults are more likely than older adults10 to share medications. Lower socioeconomic status and having drug addiction problems are also positive predictors of receiving medicines from others.10 Furthermore, disparities in health care access and utilization have been noted among ethnic groups,12,13 and these can lead to sharing of prescription medicines. Medicine sharing could also be driven by inappropriate self-treatment,14,15 and it is also possible that inappropriate drug information on the Internet inspires inappropriate self-treatment and sharing of prescribed medicines.
A systematic review of prescription medicine sharing could be useful in several ways for health planners, health care practitioners, and patients. For instance, understanding the determinants of sharing behaviors could aid in the development of specific interventions and targeted educational messages about safe medication use for patients. Moreover, the findings could help drug regulatory authorities and pharmaceutical companies to design messages targeted at reducing the risks of medicines sharing, for example, in product packaging, advertising and promotion, or public awareness campaigns.
We conducted a systematic review of the available literature on nonrecreational prescription medication sharing. Our objectives were to
identify the sources and types of medicines shared,
investigate determinants of medication sharing,
identify reasons for sharing prescription medicines,
explore the positive and negative consequences of medication sharing, and
explore the impact of medication sharing on the patient–health care provider relationship.
METHODS
In close consultation with an expert librarian, we searched PubMed and the OvidSP databases EMBASE and PsycINFO for published articles on medicine-sharing practices. We selected these databases because they contain a wide range of both health (medical) and social science literature. To ensure the retrieval of all relevant research reports, we also conducted a customized multidatabase search (Table 1). We identified further articles by scanning the reference lists of all articles retained for eligibility testing and by using an advanced Google search. Databases varied in the dates of their earliest articles; we scanned all of them through March 31, 2013, and set auto-alerts on the same searches and followed up to August 15, 2013, to ensure the inclusion of the latest articles. However, we identified no relevant articles published after March 31.
TABLE 1—
Customized Multidatabase Search for Systematic Review of Studies of Nonrecreational Prescription Medication Sharing
| Database | Type |
| Australasian Medical Index | Index |
| Google Scholar | Search engine |
| International Pharmaceutical Abstracts | Index |
| ProQuest Central | Index |
| Psychology and Behavioral Sciences Collection | Index |
| ScienceDirect | Index |
| Scopus | Index |
| Springer | Electronic journals and books |
| DRUG | Index |
| ABI/INFORM Complete | Index |
We used the following MeSH terms, combined with Boolean operators: “prescription” AND [“medication” OR “medicine” OR “drug”] AND [“sharing” OR “borrowing” OR “lending” OR “loaning” OR “swapping”] AND NOT [“cost sharing” OR “needle sharing” OR “syringe sharing”]. To ensure automatic term mapping and explosion of MeSH terms, we did not use truncation or wild cards in the database searches. However, in advanced Google search, we conducted phrase searching by enclosing the phrases “medication sharing,” “medication lending,” “medication loaning,” “medication swapping,” and “medication borrowing” in double quotes. In all searches, we avoided the use of hyphens and abbreviations. To maximize the chance of finding relevant articles, we searched literature on both recreational and nonrecreational sharing and differentiated them by reading the abstracts.
To capture all relevant studies, we did not impose language, date of publication, age, gender, or type of article limitations or any other restrictions in database searches. However, we did not identify any relevant articles in languages other than English.
Inclusion and Exclusion Criteria
An article was eligible if (1) its main aim or a major theme was assessing nonrecreational sharing of medications; (2) it described a study that employed a well-defined method of measuring medication-sharing behaviors, or a verbatim description of sharing practices in the case of a qualitative study; (3) it clearly described the study’s objectives, methods, and findings; and (4) it was a peer-reviewed research article or a conference abstract or proceeding. We excluded
books, book chapters, personal communications, case reports, review articles, and commentaries;
letters, if they did not report original or primary data;
studies whose full text could not be retrieved;
studies with a primary focus on sharing of over-the-counter medicines or recreational use of prescription medications; and
unpublished research reports.
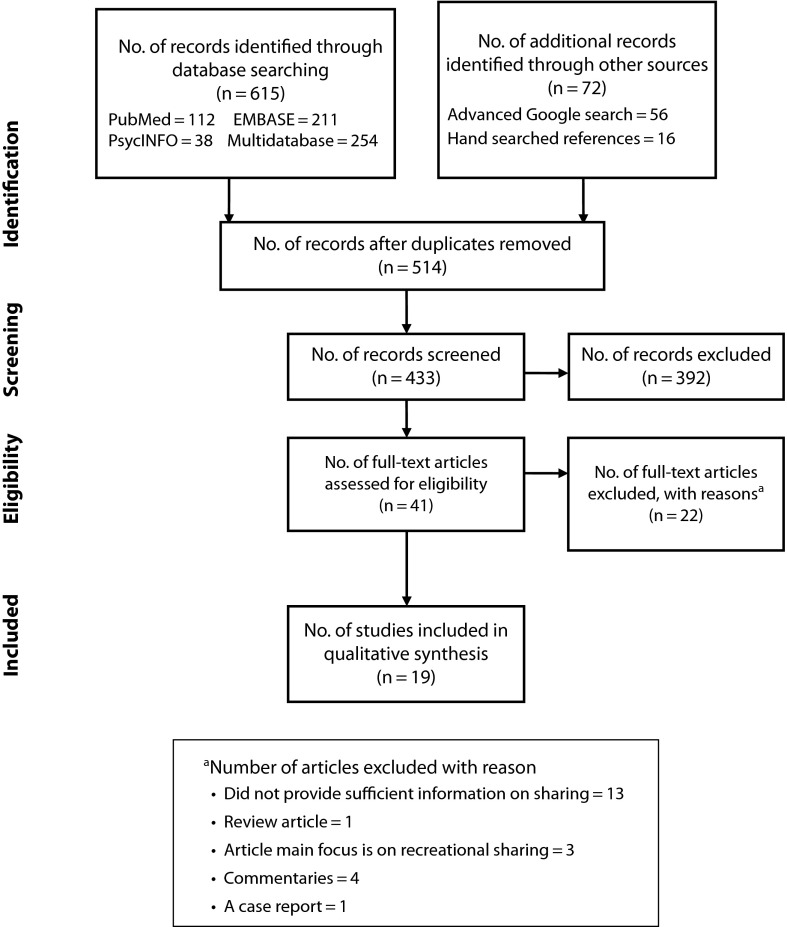
K. B. conducted the initial screening and assessment of the eligibility of retrieved articles, according to the predetermined inclusion and exclusion criteria. All authors independently assessed all articles retained for eligibility testing (Figure 1). We evaluated the eligibility of retrieved articles by reading the title and abstract; for articles whose eligibility could not be determined by these, we read the full text. Articles eliminated by reading titles concerned bank loans and were irrelevant to the review. We eliminated 3 studies because they reported both recreational and nonrecreational sharing, and the data were difficult to separate. In 1 instance, we resolved a disagreement on eligibility by discussion. We held a series of meetings to ensure the quality of the overall review process. Figure 1 is a flow diagram describing the selection procedure in detail, according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).16
FIGURE 1—
Preferred Reporting Items for Systematic Reviews and Meta-Analyses diagram summarizing selection procedure for studies of nonrecreational prescription medication sharing.
Quality Assessment and Data Analysis
K. B. performed the initial quality appraisal and abstracted data for eligible articles with a data abstraction form we designed for this review. The other authors rechecked the data; we resolved disagreements through group discussion. We compared the setting, design, study population, sample size, response rate, findings, and recommended interventions of eligible studies.
The heterogeneity of the eligible studies rendered available validated systematic quality evaluation tools inappropriate. However, we evaluated the studies according to the following criteria:
Did the study have a clear definition for medication sharing?
Were the objectives of the study sound?
Was the method used to measure sharing behaviors (in quantitative studies) appropriate?
Was the data analysis technique appropriate?
Was the study setting appropriate?
The studies in our review used qualitative, quantitative, and mixed-methods research designs; thus, statistical combination of eligible articles was not possible. Furthermore, the study settings, characteristics of participants, and data collection methods varied. The analysis process largely involved answering the preset review objectives. Table 2 displays the studies in chronological order to show the focus of medication-sharing research over time. As far as possible we followed PRISMA reporting guidelines.16
TABLE 2—
Summary of Studies in Systematic Review of Nonrecreational Prescription Medication Sharing
| Study (Year of Publication) | Location | Design | Sample Size, No. | Response Rate, % | Type of Shared Medicines | Reported Reasons/Sources | Recommended Interventions |
| Hogan et al. (1990)17 | University hospital, Saskatoon Saskatchewan, Canada | Cross-sectional survey with one-on-one interviews of randomly selected dermatology outpatients with diverse sociodemographics | 114 | NR | Topical corticosteroids, topical antifungals and antibiotics, oral antibiotics, topical antiacne medications, crotamiton cream, codeine with acetylsalicylic acid | Got from family members or friends | Asking patients with cutaneous disorders about previous use of medications from all sources while delivering care |
| Anglin and White (1999)18 | Community health clinic and other settings in rural eastern Kentucky | Ethnographic research: interviews with health and social workers and nonprofessional staff and observation of clinic | 16 | NA | Not specified | Ran out of medications, obtained from another person or health care provider, lacked money to pay for prescribed medications, to make prescriptions last longer, self-medication, got medicines through social networks | Close monitoring of medication use by health care providers, educating patients through pharmacy and nurses, reducing poverty and improving medication access, tightening communication between physicians and pharmacists to reduce overprescribing and leftover medicines |
| Thompson and Stewart (2001)19 | Metropolitan areas of Melbourne, Australia | In-home interviews with noninstitutionalized persons aged ≥ 65 y | 204 | 87 | Central nervous system and musculoskeletal agents; genitourinary agents; alimentary, cardiovascular, respiratory agents; NSAIDs | Ran out of medications, person asked to share medication, forgot own medication, to try the medication | Promoting pharmacy collection of unwanted medicines from customers |
| Daniel et al. (2003)1 | United States | Analysis of data from Youthstyles (mail survey of respondents aged 9–18 y) | 1568 | 52 | NR | Got from family members, leftover medicines; had prescription for same medicine; had the same medical problem as the person who had the medicine; wanted something strong for pimples or oily skin; ran out of medications; emergency; cost; needed for pain, headache, or sleep; wanted to relax or feel good; influenced by advertising | Educating girls and their parents about the need to take medication safely, targeting educational messages to adolescents on safe use of medications |
| Sorensen et al. (2003)20 | Australia, 4 states | Cross-sectional survey (researcher-administered questionnaires) of community-dwelling, older war veterans and widowers at risk for medication misadventures and living in their own homes | 1086 | NR | NSAIDs, COX-2 inhibitors, benzodiazepines, cardiovascular medications, H-2 antagonists and proton pump inhibitors, codeine or dextropropoxyphene combinations, paroxetine, thyroxin sodium, warfarin, α-2 receptor agonists (inhalers), latanoprost, quinine, allopurinol, bethamethasone (ointment), diphenoxylate with atropine sulfate, prochlorperazine | Shared with spouse | NR |
| Hamrosi et al. (2006)21 | Community health centers and hospitals in midwestern New South Wales, Australia | Qualitative in-depth interviews with Aboriginal health workers | 11 | NA | Not specified | Shared between family and friends | Providing education that considers community culture and giving appropriate and adequate education training for Aboriginal health workers |
| Goldsworthy et al. (2008)22 | United States, 20 cities | Cross-sectional survey (one-to-one interviews), of respondents aged 12–44 y, with diverse sociodemographic characteristics | 700 | NR | Allergy medications (e.g., Allegra, Claritin), pain medications (e.g., Darvoset, OxyContin), antibiotics (e.g., amoxicillin, doxycyclin, Bactrim/Septra), mood medications (e.g., Paxil, Zoloft, Valium, Ritalin), acne medication (e.g., Accutane), birth control pills | Got from family members; had leftover medicines; had prescription for same medicine; had the same medical problem as the person who had the medicine; wanted something strong for pimples or oily skin; ran out of medications; emergency; cost; needed for pain, headache, or sleep; wanted to relax or feel good; influenced by advertising; got from someone who knew about medications; helped a friend | NR |
| Petersen et al. (2008)23 | United States | Analysis of data from 2001– 2006 US Healthstyles survey (cross-sectional mail survey of individuals), with emphasis on women of reproductive age (n = 7400) | 26 289 | 72.2 | Allergy medications, pain medications, antibiotics, mood medications, birth control pills, acne medications | Got from family member; already had prescription but ran out; had the same medical problem as the person who had the medicine; needed for pain, headache or sleep; emergency; had leftover medicines; cost; wanted to relax or feel good; wanted something strong for pimples or oily skin; influenced by advertising | Discussing the risk of sharing with the patient during prescribing, designing programs to promote safe disposal of unwanted medicines, ensuring access to health care and medications for women of reproductive age |
| Goldsworthy and Mayhorn (2009)24 | United States, public spaces of 11 urban and suburban areas | Cross-sectional survey (one-on-one interviews) of demographically diverse adolescents aged 12–17 y | 594 | NR | Allergy medications, pain medications, mood medications, antibiotics, acne medications, birth control pills | To avoid health care provider visit | Providing training to health care providers on the risk of borrowed medications and educating patients on the proper use of medications and risks of sharing; developing messages on sharing, e.g., within product label; public awareness campaigns |
| Mayhorn and Goldsworthy (2009)25 | United States, 11 locations across country | Cross-sectional survey (one-on-one interviews) of demographically diverse individuals | 2773 | NR | Allergy medications (e.g., Zyrtec, Clarinex, Flonase), pain medications (e.g., Darvoset, OxyContin), antibiotics (e.g., amoxicillin, doxycyclin, Bactrim/Septra), mood medications (e.g., Paxil, Zoloft, valium, Ritalin), acne medication (e.g., Accutane), birth control pills | NR | Increasing public awareness on medication sharing dangers, adding sharing prohibition messages to labeling, providing training to health care providers |
| Ali et al. (2010)26 | Universiti Sains Malaysia | Cross-sectional survey (one-on-one interviews) of randomly sampled female students | 481 | 90.7 | Not specified | Got from family or friends, leftover medicines | NR |
| Goulding et al. (2011)27 | University College Cork, Ireland | Cross-sectional survey (anonymous electronic questionnaire) of students, aged 18–25 y | 343 | NR | Contraceptives, antibiotics, analgesics | Got from family or friend, cost, inconvenience of visiting doctors, didn't feel sick enough to see doctor | Educating about adverse drug events of medications, discouraging patients from sharing; advising patients to safely dispose of medications |
| Auta et al. (2011)28 | University of Jos, Nigeria | Cross-sectional survey (self-administered questionnaire) of randomly sampled students | 730 | 81.6 | Cold/flu medications, pain medications, antibiotics, dermatological medications, mood medications, antimalarials | Emergency, had the same medical problem as the person who had the medicine, influenced by advertising, ran out of medicines, got from someone who knew about medicines or from family members, leftover medicines | Educating public on danger of medication sharing |
| Goebel et al. (2011)29 | California, 2 hospitals and 6 affiliated community sites | Cross-sectional cohort study (one-on-one interviews), analysis of self-reported substance misuse for pain management among veterans | 343 | NR | NR | For pain management | NR |
| Ward et al. (2011)30 | New York, 4 clinical sites at an urban academic medical center | Cross-sectional survey (one-on-one interviews) of randomly sampled individuals aged ≥ 18 y | 641 | 80 | Opioids (Schedule II–IV), NSAIDs and COX-2 inhibitors, benzodiazepines, antibiotics, antihypertensives, others | Got from family members, friends, someone from street, or Internet; to get high, convenience, self-medication, cost | Regularly asking patients about medication use, cautioning patients about borrowing medications even if they deny the behavior |
| Ellis et al. (2011)31 | Illawarra region, New South Wales, Australia | Mixed methods (focus group discussion followed by self-administered survey); convenience sample of independently living adults aged ≥ 65 y | focus group, n = 28; survey, n = 226 | 65 | Antihypertensive, heart disease medications, arthritis or joint inflammation medications, strong pain medications, diabetic medications, depression/anxiety medications, antibiotics, others | Got from family members, ran out of medicines, forgot to fill prescriptions, severe pain, cost, could not go to chemist or doctor, self-medication, tried medication before visiting doctor, medication similar to previous prescription | NR |
| Kheir et al. (2011)32 | Qatar | Cross-sectional telephone interview with randomly sampled household representatives | 49 | 18 | Antidiabetic medications, anti-infective medications, inhaled bronchodilators, inhaled corticosteroids, oral corticosteroids | Shared with family members | NR |
| Hodgetts et al. (2011)33 | Central North Island, New Zealand | Focus group discussion with community health workers with heritage linkage with Māori people and employed by Māori tribal health provider | 7 | NA | Most prescription medications | Shared among family members and social networks, avoided visits to general practitioner/pharmacy, ran out of medications, obtained prescription medicines from general practitioner by presenting false proxy symptoms, cost, cultural barrier | Integrating medication-sharing concerns into training of health care providers |
| Kamutingondo et al. (2011)34 | Hamilton, New Zealand | Ethnographic research (interviews, photographs, diaries, mapping, material objects, and media content) among 4 Zimbabwean households | 17 | NA | NR | To demonstrate care among family members during illness, to sustain and nurture social relationship among households | NR |
Note. COX = cyclooxygenase; NA = not applicable; NR = not reported; NSAID = nonsteroidal anti-inflammatory drug.
RESULTS
Our initial database search yielded 615 articles. The advanced Google search identified 56 articles, only 1 of which was not identified by the initial database search. We identified 16 additional articles by scanning the reference lists of articles retained for eligibility testing. Combining the results of all searches and removing duplicates yielded 514 articles. We discarded 81 because they were short communications on Web sites or were written by unspecified authors (i.e., they were not journal articles and did not have an author, casting doubt on their reliability). We read the title, abstract, or full text of the remaining 433 articles and retained 41 for further eligibility tests. We evaluated the retained articles according to our predefined inclusion and exclusion criteria and excluded 22 (Figure 1 shows detailed reasons). We performed our final qualitative synthesis on the remaining 19 articles.
Overview
A summary of the characteristics of the studies is presented in Table 2. The review comprised 19 studies with 36 182 participants from 9 countries. Eight of the studies were conducted in the United States, 4 in Australia, 2 in New Zealand, and 1 each in Canada, Nigeria, Malaysia, Qatar, and Ireland. The studies were conducted between 1990 and 2011, and the majority (73.7%; 14/19) were published between 2006 and 2011. The articles were published in 18 different journals. We retrieved 1 article from a conference proceeding.25 The majority of the studies (73.7%; 14/19) used a quantitative, cross-sectional survey design, 21.1% (4/19) conducted qualitative interviews, and 5.3% (1/19) had a mixed-method design. The study participants ranged from children to older people. Three surveys investigated medication sharing among college students,26–28 and 1 study focused on women of reproductive age.23 Two studies reported on medication sharing among children and adolescents.1,24 Of the 4 qualitative studies,18,21,33,34 3 assessed the experiences and attitudes of health workers about medication sharing; respondents worked in rural areas or with indigenous people.18,21,33 Five studies focused on the sharing practices of older people17,19,20,29,31; 1 of these employed a mixed-methods research design.31 The remaining 4 studies investigated medication sharing among adults with various sociodemographic characteristics.22,25,30,32
Of the studies that reported quantitative data (n = 15), 12 had sample sizes greater than 200 participants; only 7 studies explicitly stated that they recruited participants through random sampling.1,17,23,26,28,29,32 Eight studies reported a participant response rate,1,19,23,26,28,30–32 and 6 of these reported rates of 65% or higher.19,23,26,28,30.31
Medication Sharing
We found no reported gold standard method for measuring medication sharing. However, 2 of the surveys analyzed data collected in the US Healthstyles surveys,1,23 and 5 studies adapted a question matrix used in these surveys to suit their own study.22,24,25,28,31 The Healthstyles surveys asked respondents 2 separate questions to assess their lending and borrowing practices, respectively: “Have you ever shared your prescription medication with others?” and “Have you ever borrowed prescription medication from others?” For instance, in their analysis of 2001 to 2006 Healthstyles survey data, Petersen et al. considered respondents who responded positively to the first question to have lent medicines and those who responded positively to the second question to have borrowed medications23; they considered those who responded negatively to one of the questions and do not know–not sure to the other not to have lent or borrowed medicines.
Because self-reported survey studies used various recall periods, we could not calculate the average prevalence rate of all studies. However, prevalence rates varied across the studies (Table 3). For medication borrowing, the reported rate was between 5% and 51.9%, and for lending, between 6% and 22.9%. The lowest rates for both borrowing and lending were reported in a survey among older people,31 and the maximum rates came from 2 separate surveys, of Nigerian university students28 and US adult participants.22 Of 10 studies that reported both lending and borrowing rates,1,17,19,22-25,27,28,31 the majority (n = 6) reported rates higher than 16%.23-25,27,28,34 Eight studies reported the prevalence rate of lending or borrowing, which ranged from 5% to 54.3%.1,20,22,23,26–29 Of these, 5 reported a rate higher than 27%.22,23,26–28
TABLE 3—
Prevalence of Sharing in Quantitative Survey Studies in Systematic Review of Nonrecreational Prescription Medication Sharing
| Prevalence of Sharing |
||||||
| Studies | Sample Size, No. | Response Rate, % | Borrowing, No. (%) | Lending, No. (%) | Lending or Borrowing, No. (%)a | Recall Period |
| Hogan et al.17 | 114 | NR | 20 (17.5) | 7 (6.1) | NR | 1 y |
| Thompson and Stewart19 | 204 | 87 | 14 (6.9) | 26 (12.7) | NR | Ever |
| Daniel et al.1 | 1568 | 52 | 212 (13.5) | 171 (10.9) | 210 (13.4) | Ever |
| Sorensen et al.20 | 1086 | NR | NR | NR | 49 (5) | NR |
| Goldsworthy et al.22 | 700 | NR | 188 (26.9) | 160 (22.9) | 236 (33.7) | 1 y |
| Petersen et al.23 | 26 289 | 72.2 | 6086 (23.2) | 5065 (19.3) | 7272 (27.7) | Ever |
| Goldsworthy and Mayhorn24,b | 594 | NR | 115 (19.4) | 122 (20.5) | NR | 1 y |
| Mayhorn and Goldsworthy25 | 2773 | NR | 594 (21.4) | 624 (22.5) | NR | 1 y |
| Ali et al.26 | 481 | 90.7 | NR | NR | 261 (54.3) | NR |
| Goulding et al.27 | 343 | NR | 89 (26) | 70 (20) | 117 (34.1) | Ever |
| Auta et al.28 | 730 | 81.6 | 379 (51.9) | 127 (17.4) | 385 (52.7) | 1 y |
| Goebel et al.29 | 343 | NR | NR | NR | 56 (16.3) | NR |
| Ward et al.30 | 641 | 80 | 116 (18) | NR | NR | Ever |
| Ellis et al.31 | 226 | 65 | 10 (5) | 12 (6) | NR | NR |
| Kheir et al.32 | 49 | 18 | NR | NR | NR | NR |
Note. NR = not reported.
If the rate of borrowing or lending was not provided by the authors, we calculated as No. of borrowers or lenders = No. lenders + No. of borrowers − (No. of both lenders and borrowers).
Part of larger study by Mayhorn and Goldsworthy.25
Four studies reported that medication lending was more common among female than male participants1,17,22,23; however, in 2 other studies lending behavior was not significantly associated with gender.24,28 Two studies found no gender difference in the rate of borrowing.22,23 Medication sharing was also associated with age,23,26,28 and those aged 18 to 24 years were more likely to report medicine sharing.23,26 For medication borrowing, a study reported a higher rate among women of reproductive age (18–44 years) than among older women (≥ 45 years).23 Findings about medication lending were not consistent across studies. For example, Petersen et al. documented a higher rate of lending among reproductive-aged than older women,23 but Goldsworthy and Mayhorn did not find age to be a significant predictor of medication lending.24
In 4 studies, race/ethnicity was associated with medication sharing.22–24,26 Ali et al. reported a higher rate of sharing among participants of Malay ethnic origin and Chinese college students26; however, they did not report the comparison group. Another study documented higher odds of sharing among US non-Hispanic White reproductive-aged women than among women who were Hispanic or whose race/ethnicity was not White, Black, or Hispanic.23 However, in 3 other studies race or ethnicity was not associated with either lending or borrowing.25,29,30 Thirteen of the surveys in our review did not assess the association between income and medication sharing.17,19,20,22,24–32 However, in a study among US children and adolescents (aged 9–18 years), lower income was associated with sharing prescription medicines with family members or friends (P < .01).1 Many of the reviewed studies did not explore or report the influence of the Internet on medication sharing. Petersen et al. noted that those who accessed health information from the Internet were more likely than those who did not to report medication sharing (relative risk = 1.50; 95% confidence interval = 1.44, 1.56).23
Daniel et al.1 and Petersen et al.23 found that a larger household size was a positive predictor of medication sharing. A study that assessed the use of nonprescribed medications for pain management among veterans found substance use disorders (P = .006) and pain interference activities (P = .047) to be positive predictors of sharing.29
A study among adults visiting an urban medical center in the United States reported less likelihood of medication borrowing among participants with Medicare insurance (P = .03) or a primary health care provider who frequently asked about medication usage (P = .049).30 Petersen et al. reported less likelihood of lending or borrowing among reproductive-aged women who used a multivitamin daily (relative risk = 1.28; 95% confidence interval = 1.18, 1.40).23
Commonly Shared Prescription Medicines
Study participants reported sharing a wide range of prescription medicines. Twelve of the 15 surveys reported the types of medicines shared.17,19,20,22–25,27,28,30–32 Seven of the surveys used a predetermined list of medications and asked participants to indicate the medications they shared from the list.1,22–25,28,31 The qualitative studies mainly explored the reasons behind prescription medicine sharing and did not report the specific types of shared medicines.
A study of US adults that involved one-on-one interviews found allergy medications, pain medications, and antibiotics to be the most commonly shared medication classes.22 Acne medications were also found to be widely shared.17,22–24 Petersen et al. reported a high rate of isotretinoin sharing (25%) among women of child-bearing age.23 Four studies documented sharing of birth control pills among women.22–24,27 Hogan et al. reported the sharing of prescription topical corticosteroids and other dermatologic medications among randomly selected dermatology outpatients.17 Sharing of antibiotics among the general adult population was also common.17,22–24,27,28,30–32 In addition, studies reported sharing of antidiabetic, cardiovascular, and antihypertensive medications.19,20,22,30–32
Seven surveys gave respondents a predetermined list of reasons and asked them to indicate those that influenced them to share their medicines.1,19,22,23,28,30,31 In 4 of these studies, respondents received an additional list of hypothetical scenarios to assess situations in which they would be willing to share.1,22,23,31 In 3 studies, the main situation in which borrowing occurred involved a person already taking a medicine but running out of it or having the same medical problem as the person who had the medicine.22,23,31 Participants also expressed their willingness to borrow medications if they were obtaining the medicines from a family member or a friend,1,30 if the medicine was unaffordable,31 if the situation was an emergency,1,22 if they obtained a lot information about the medicine from advertisements and commercials,23,28 for convenience,30 or for pain management.1 The primary explanations for lending behavior were having leftover medication22,23 and the desire to help others.22 Respondents were also willing to lend their medicines if asked by a family member or friend or by a person with a similar problem or taking similar medicine and or in emergency circumstances.19,22
Consequences of Medication Sharing
Although the surveys in our review focused on investigating the adverse consequences of sharing, the qualitative studies reported both benefits and adverse consequences. Kamutingondo et al., in a qualitative study among 4 Zimbabwean households in New Zealand, noted that sharing medicines during illness is a means of expressing a caring relationship among family members in a time of sickness.34 Hodgetts et al., in a focus group discussion with 7 Māori health workers in New Zealand, reported that sharing is a convenient means of accessing prescription medicines among Māori.33 Moreover, the research team revealed a process of accessing medications on behalf of others by the use of proxy symptoms (i.e., pretending they were ill to obtain prescriptions from general practitioners) among members of a whānau (an extended family group that may span 3–4 generations). Anglin and White documented that sharing was a means of accessing prescription medicines in a rural eastern Kentucky neighborhood largely populated by poor and unemployed people.18
In a study among 594 adolescents recruited from 11 cities,24 which was part of a larger survey (n = 2773) designed to investigate medication sharing in the United States,25 among respondents who borrowed medicines (n = 115), 37.4% had experienced a side effect or an allergic reaction and only about half reported receiving either verbal (55.6%) or written (47.8%) instructions from the person lending the medicine. Moreover, 75% (n = 86) of the borrowers were trying to avoid a medical visit; however, 26.7% (23/86) of these ended up visiting health care providers after their effort to self-medicate with borrowed medicines failed, and one third (28/86) did not inform their health care providers during their next medical visit about the medications they borrowed.
Recommended Interventions
The studies suggested various interventions to reduce the harms and risks of sharing medications. Daniel et al.1 noted that sharing behaviors might be formulated early in the life course, during childhood or adolescence, and they suggested providing targeted messages about the safe use of prescription medications to parents and their children. Authors also recommended providing health messages on the risks of sharing.23,24,30 These included alerting women to the dangers of sharing teratogenic medications,23 regular cautioning of patients about risks of inappropriate medication usage,30 and adding messages that prohibit sharing in product packaging.24 Researchers also recommended informing patients about appropriate disposal practices for leftover medications27 and reexamining the cost of health care access, particularly for low-income persons.33 Recommended strategies to increase access were reconsidering physicians’ fee structures and reducing prescription charges in pharmacies.33
Authors also suggested methods to identify medication borrowers and lenders. One suggested technique was inquiring about patients’ medication usage during health care provision.30 Even when patients deny borrowing or lending medications, researchers advocate cautioning them about the risks as a potentially effective deterrent.30
DISCUSSION
To our knowledge, ours was the first review to systematically summarize research on nonrecreational medication sharing. The reviewed literature mainly investigated medication sharing from a medical—rather than a sociological or cultural—perspective. Furthermore, most of the studies were conducted in developed countries, where access to and affordability of health care services might be different than in developing countries. Authors of the reviewed articles conducted their studies with varying aims and methods. Differences in cultures, health care systems, economics, education, and medication use behaviors across the study settings made comparing findings challenging. However, we were able to draw instructive conclusions on medicine sharing.
The extent and type of medicine regulation varied across states and countries. Whether a medicine requires a prescription or is available over the counter varies internationally.35 Thus, we could not determine an appropriate denominator to report the average sharing prevalence for all studies. Overall, we documented high prevalence rates of medication lending (6%–22.9%) and borrowing (5%–51.9%). The studies that reported the highest rates of borrowing22,24,26–28 or lending22–25,27,28 were undertaken between 2008 and 2011; studies conducted before 2005 reported relatively lower rates of lending or borrowing.1,17,19,20 This might be attributable to a general increase in self-medication with prescription medicines in recent years.36,37
In 6 studies, lending was generally less prevalent than borrowing,1,17,22,23,27,28 and this could be attributable to response bias. As noted by Caviness et al., people may be more willing to admit receiving medication from others than giving (or lending) it to someone else.10 The existence of drug vendors who offer prescription medicines without a prescription38 is a possible explanation for the much higher rate of borrowing (51.9%) reported among Nigerian college students than borrowing rates in other studies.28
Similar to studies investigating recreational sharing of prescribed medications,5,7,9 our review revealed that the most common source of shared medicines was either a family member or a friend. It is likely that participants preferred to obtain medications from trusted sources than through other channels, such as theft or prescription fraud.
Studies that examined the types of medicines shared found pain medications, allergy medications, and antibiotics to be the most commonly shared classes of medicines. In light of the addictive potential of some pain medications,39 the possibility of adverse reactions from allergy medications,40 and the development of bacterial resistance associated with uncontrolled use of antibiotics,41 health care providers should take proactive measures to limit the sharing of these medicines. Sharing of medicines with high teratogenic potential, such as isotretinoin (a US Food and Drug Administration category X drug), observed among women of child-bearing age, carries a risk of birth defects, particularly if women do not inform their health care provider about their borrowing practices.23
Four surveys found that the odds of medication lending were higher in female than male respondents1,17,22,23; this might be associated with greater medication consumption by women than men,42 or related to the nurturing role of women in many cultures.43 The higher prevalence of sharing among younger respondents, in particular college students,27,28 was consistent with findings in other studies on recreational sharing of medications among similar groups.9,10 Exposure to new lifestyles at colleges might lead to both social and academic stress and ultimately to medication sharing for self-medication as a response to such stress.44 Furthermore, a move away from home might reduce convenient access to students' usual general practitioners.
We found the association between race/ethnicity and medication sharing inconclusive. Ethnic groups across the studies were not similar; thus, it was difficult to compare findings. Moreover, access to health care services, including availability of medications, differs across countries, and this might influence sharing practices across studies.
Several studies did not explore income as a predictor of sharing behaviors. This might be because most of the studies were carried out in developed countries, where health insurance and subsidized medicines, which are relatively affordable, are available to many. However, as noted by Costello,45 with the rising cost of health care, patients may have difficulty paying for a visit to a medical practitioner to obtain prescriptions, and they might share medicines instead.
The sharing practices documented among older people (≥ 65 years),19,20,31 although not as prevalent as in younger age groups,1,24,28 could result in adverse drug events.2 Studies reported sharing of a range of pharmacological categories, such as heart disease medications, antidepressants, antihypertensives, pain medications, and antibiotics, among older people.19,20,31 Heuberger noted that medication sharing results in polypharmacy among older people.46 Medication sharing can have other consequences, such as a delay in seeking care,25 which may complicate simple conditions or, in the worst-case scenario, result in death. Clinicians may be unaware of a patient’s sharing practices, raising the risk of adverse medication interactions. Finally, when borrowing, the recipient may not obtain adherence aids that should accompany the medicine and thus may not comply with the medication’s use instructions.
Articles that recommended interventions mainly based their proposals on research informed by a medical perspective and largely overlooked sociological or patient perspectives. Efforts to test some of the recommended interventions to minimize the harms of sharing were very limited. It is important to note that medicines are more than a chemical entity; they are an element in our social interactions, beliefs, caring relationships, moralities, and routines.47 Practically, it might also be difficult to stop people from sharing medicines. Thus, any interventions designed to reduce potential harms of sharing need to understand and take into account why people share, how they make decisions to lend or borrow, whether they are aware of the risks, and how they assess the relevance of that risk. The latter 2 issues remain unexplored and are important areas for future research.
The laws and regulations of several countries prohibit distributing prescription medicines, in the form of gifts or loans or receiving them from a person unauthorized to dispense medicines48,49; however, implementation of such laws can be challenging. The regulations also lack clarity for some medicines, which can be obtained either by prescription or over the counter. For instance, in many countries paracetamol is classified as a prescription medicine or an OTC medicine depending on the pack size, formulation and labelling.
Limitations
Most of the studies in our review adopted a similar survey tool. Although this could be useful for comparing findings, a tool developed for a certain target population in a specific country might not be appropriate for assessing the sharing practices of different population groups. Furthermore, the studies did not indicate the validity and reliability of the tool in their respective settings. No gold standard method has been established for measuring the prevalence of medication sharing, and the definitions and measures of sharing varied across the studies. The use of a long recall period (≥ 1 year) for self-reported medication sharing might also have resulted in underreporting because of recall bias. We suspect also that study participants who considered medication sharing to be illegal might not have admitted to it. Bias in participant selection could also have resulted from the voluntary nature of participation. Furthermore, in an effort to identify the types of shared medicines and reasons for sharing, many of the surveys listed predetermined factors and asked the participants to choose from them; this process might limit the discovery of other motives for sharing from the patient perspective.
The majority (73.7%; 14/19) of the reviewed studies were from the United States, Australia, and New Zealand; therefore, the findings might not represent the practice of sharing in resource-limited settings. They also may not be generalizable to the larger population the study sample was meant to represent because of nonrandom sampling. Because of the heterogeneity of the articles in our review, we could not assess risk of bias across studies. Moreover, 7 surveys did not report their response rate. The cross-sectional nature of most of the studies limited understanding of cause and effect. We did not include unpublished reports, book chapters, review articles, or commentaries; thus, some relevant information might have been omitted.
Conclusions
Although sharing of prescription medicines has received limited attention from researchers, our review demonstrated that nonrecreational prescription medication sharing is common. Studies reported that broad classes of prescribed medicines were shared, and sharing was more common among younger adults and adolescents. The main circumstances for borrowing were already taking a medicine but running out of it and having the same medical problem as the person who had the medicine; motivations for lending were having leftover medication and the desire to help others.
The literature to date has mainly taken a medical perspective and largely overlooked investigating medication sharing from patients’ perspectives; many gaps exist in the research. Future studies should explore medication sharing from a patient and societal perspective.
Acknowledgments
We thank Bruce Arroll, Department of General Practice and Primary Health Care, University of Auckland, for reviewing the draft of the article and providing helpful suggestions.
Human Participant Protection
No protocol approval was needed because this was a review of previously published research.
References
- 1.Daniel KL, Honein MA, Moore CA. Sharing prescription medication among teenage girls: potential danger to unplanned/undiagnosed pregnancies. Pediatrics. 2003;111(5 pt 2):1167–1170. [PubMed] [Google Scholar]
- 2.Ellis J, Mullan J. Prescription medication borrowing and sharing: risk factors and management. Aust Fam Physician. 2009;38(10):816–819. [PubMed] [Google Scholar]
- 3.Goldsworthy RC. Recreational versus nonrecreational prescription borrowing: time for an expanded conceptualization? J Adolesc Health. 2010;46(4):402. doi: 10.1016/j.jadohealth.2009.12.016. author reply 403. [DOI] [PubMed] [Google Scholar]
- 4.Poulin C. Medical and nonmedical stimulant use among adolescents: from sanctioned to unsanctioned use. Can Med Assoc J. 2001;165(8):1039–1044. [PMC free article] [PubMed] [Google Scholar]
- 5.McCabe SE, Boyd CJ. Sources of prescription drugs for illicit use. Addict Behav. 2005;30(7):1342–1350. doi: 10.1016/j.addbeh.2005.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McCabe SE, Teter CJ, Boyd CJ. Medical use, illicit use, and diversion of abusable prescription drugs. J Am Coll Health. 2006;54(5):269–278. doi: 10.3200/JACH.54.5.269-278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boyd CJ, McCabe SE, Cranford JA, Young A. Prescription drug abuse and diversion among adolescents in a southeast Michigan school district. Arch Pediatr Adolesc Med. 2007;161(3):276–281. doi: 10.1001/archpedi.161.3.276. [DOI] [PubMed] [Google Scholar]
- 8.Poulin C. From attention-deficit/hyperactivity disorder to medical stimulant use to the diversion of prescribed stimulants to non-medical stimulant use: connecting the dots. Addiction. 2007;102(5):740–751. doi: 10.1111/j.1360-0443.2007.01758.x. [DOI] [PubMed] [Google Scholar]
- 9.Garnier LM, Arria AM, Caldeira KM, Vincent KB, O’Grady KE, Wish ED. Sharing and selling of prescription medications in a college student sample. J Clin Psychiatry. 2010;71(3):262–269. doi: 10.4088/JCP.09m05189ecr. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Caviness CM, Anderson BJ, de Dios MA, Kurth M, Stein M. Prescription medication exchange patterns among methadone maintenance patients. Drug Alcohol Depend. 2013;127(1–3):232–238. doi: 10.1016/j.drugalcdep.2012.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McCabe SE, West BT, Teter CJ, Ross-Durow P, Young A, Boyd CJ. Characteristics associated with the diversion of controlled medications among adolescents. Drug Alcohol Depend. 2011;118(2–3):452–458. doi: 10.1016/j.drugalcdep.2011.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gornick ME, Eggers PW, Reilly TW et al. Effects of race and income on mortality and use of services among Medicare beneficiaries. N Engl J Med. 1996;335(11):791–799. doi: 10.1056/NEJM199609123351106. [DOI] [PubMed] [Google Scholar]
- 13.Jatrana S, Crampton P, Norris P. Ethnic differences in access to prescription medication because of cost in New Zealand. J Epidemiol Community Health. 2011;65(5):454–460. doi: 10.1136/jech.2009.099101. [DOI] [PubMed] [Google Scholar]
- 14.Loyola Filho AI, Lima-Costa MF, Uchôa E. Bambuí project: a qualitative approach to self-medication. Cad Saude Publica. 2004;20(6):1661–1669. doi: 10.1590/s0102-311x2004000600025. [DOI] [PubMed] [Google Scholar]
- 15.Sharma V, Thakur S, Bhatt N, Guleria R, Singh R. Self-medication and drug use patterns in a town of Himachal Pradesh: a survey. Int J Adv Pharm Res. 2012;3(8):1058–1062. [Google Scholar]
- 16.Moher D, Liberati A, Tetzlaff J, Altman DG PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 17.Hogan DJ, Moreland A, Lane P, Lal S. Exchange of prescription medications by dermatology outpatients. J Am Acad Dermatol. 1990;23(5 pt 1):953. doi: 10.1016/s0190-9622(08)80715-3. [DOI] [PubMed] [Google Scholar]
- 18.Anglin MK, White JC. Poverty, health care, and problems of prescription medication: a case study. Subst Use Misuse. 1999;34(14):2073–2093. doi: 10.3109/10826089909039439. [DOI] [PubMed] [Google Scholar]
- 19.Thompson S, Stewart K. Prescription medication use practices among non-institutionalised older persons. Int J Pharm Pract. 2001;9(3):141–151. [Google Scholar]
- 20.Sorensen L, King MA, Ientile CS, Roberts MS. Has drug therapy gone to the dogs? Age Ageing. 2003;32(4):460–461. doi: 10.1093/ageing/32.4.460. [DOI] [PubMed] [Google Scholar]
- 21.Hamrosi K, Taylor SJ, Aslani P. Issues with prescribed medications in Aboriginal communities: Aboriginal health workers’ perspectives. Rural Remote Health. 2006;6(2):557. [PubMed] [Google Scholar]
- 22.Goldsworthy RC, Schwartz NC, Mayhorn CB. Beyond abuse and exposure: framing the impact of prescription-medication sharing. Am J Public Health. 2008;98(6):1115–1121. doi: 10.2105/AJPH.2007.123257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Petersen EE, Rasmussen SA, Daniel KL, Yazdy MM, Honein MA. Prescription medication borrowing and sharing among women of reproductive age. J Womens Health (Larchmt) 2008;17(7):1073–1080. doi: 10.1089/jwh.2007.0769. [DOI] [PubMed] [Google Scholar]
- 24.Goldsworthy RC, Mayhorn CB. Prescription medication sharing among adolescents: prevalence, risks, and outcomes. J Adolesc Health. 2009;45(6):634–637. doi: 10.1016/j.jadohealth.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 25.Mayhorn CB, Goldsworthy RC. Borrowing prescription medication: implications for healthcare warnings and communications. Proc Hum Fact Ergon Soc Annu Meet. 2009;53(20):1608–1611. [Google Scholar]
- 26.Ali SE, Ibrahim MIM, Palaian S. Medication storage and self-medication behaviour amongst female students in Malaysia. Pharm Pract (Internet) 2010;8(4):226–232. doi: 10.4321/s1886-36552010000400004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Goulding E, Murphy M, Di Blasi Z. Sharing and borrowing prescription medication: a survey of Irish college students. Ir J Med Sci. 2011;180(3):687–690. doi: 10.1007/s11845-011-0698-0. [DOI] [PubMed] [Google Scholar]
- 28.Auta A, Banwat SB, Francis RA. Prevalence of prescription medication sharing behaviour among students. Int J Pharm Life Sci. 2011;2(4):651–654. [Google Scholar]
- 29.Goebel JR, Compton P, Zubkoff L et al. Prescription sharing, alcohol use, and street drug use to manage pain among veterans. J Pain Symptom Manage. 2011;41(5):848–858. doi: 10.1016/j.jpainsymman.2010.07.009. [DOI] [PubMed] [Google Scholar]
- 30.Ward L, Patel NM, Hanlon A, Eldakar-Hein S, Sherlinski K, Ward SH. Prescription medication borrowing among adult patients at an urban medical center. J Urban Health. 2011;88(6):997–1014. doi: 10.1007/s11524-011-9589-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ellis JC, Mullan J, Worsley T. Prescription medication hoarding and borrowing or sharing behaviours in older residents in the Illawarra, New South Wales, Australia. Australas J Ageing. 2011;30(3):119–123. doi: 10.1111/j.1741-6612.2010.00457.x. [DOI] [PubMed] [Google Scholar]
- 32.Kheir N, El Hajj M, Wilbur K, Kaissi R, Yousif A. An exploratory study on medications in Qatar homes. Drug Healthc Patient Saf. 2011;3:99–106. doi: 10.2147/DHPS.S25372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hodgetts D, Nikora LW, Rua M. Maori men and the indirect procurement and sharing of prescription medications. AlterNative. 2011;7(2):152–162. [Google Scholar]
- 34.Kamutingondo S, Groot S, Hodgetts D, Nikora LW. Understandings and social practices of medications for Zimbabwean households in New Zealand. MAI Rev. 2011(3):1–17. Available at: http://review.mai.ac.nz/index.php/MR/article/view/432. Accessed June 10, 2013. [Google Scholar]
- 35.Harrington P, Shepherd MD. Analysis of the movement of prescription drugs to over-the-counter status. JMCP. 2002;8(6):499–508. doi: 10.18553/jmcp.2002.8.6.499. [DOI] [PubMed] [Google Scholar]
- 36.Khan H, Maheen S, Bashir S et al. Determinants of increasing trends of self-medication: physicians, perspectives. Lat Am J Pharm. 2012;31(5):699–704. [Google Scholar]
- 37.Sallam SA, Khallafallah NM, Ibrahim NK, Okasha AO. Pharmacoepidemiological study of self-medication in adults attending pharmacies in Alexandria, Egypt. East Mediterr Health J. 2009;15(3):683–691. [PubMed] [Google Scholar]
- 38.Erhun WO, Babalola OO, Erhun M. Drug regulation and control in Nigeria: the challenge of counterfeit drugs. J Health Popul Dev Ctries. 2001;4(2):23–34. [Google Scholar]
- 39.Compton WM, Volkow ND. Major increases in opioid analgesic abuse in the United States: concerns and strategies. Drug Alcohol Depend. 2006;81(2):103–107. doi: 10.1016/j.drugalcdep.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 40.Church MK, Maurer M, Simons FE et al. Risk of first-generation H1-antihistamines: a GA2LEN position paper. Allergy. 2010;65(4):459–466. doi: 10.1111/j.1398-9995.2009.02325.x. [DOI] [PubMed] [Google Scholar]
- 41.Davies J, Davies D. Origins and evolution of antibiotic resistance. Microbiol Mol Biol Rev. 2010;74(3):417–433. doi: 10.1128/MMBR.00016-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Neutel CI, Walop W. Drug utilization by men and women: why the differences? Drug Inf J. 2005;39(3):299–310. [Google Scholar]
- 43.Zaidi ZF. Gender differences in human brain: a review. Open Anat J. 2010;2(1):37–55. [Google Scholar]
- 44.Quintero G, Peterson J, Young B. An exploratory study of socio-cultural factors contributing to prescription drug misuse among college students. J Drug Issues. 2006;36(4):903–931. [Google Scholar]
- 45.Costello D. Many who share drugs don’t know the dangers. Los Angeles Times. May 31, 2005 Available at: http://www.boston.com/news/globe/health_science/articles/2005/05/31/many_who_share_drugs_dont_know_the_dangers. Accessed May 15, 2013. [Google Scholar]
- 46.Heuberger R. Polypharmacy and food–drug interactions among older persons: a review. J Nutr Gerontol Geriatr. 2012;31(4):325–403. doi: 10.1080/21551197.2012.729902. [DOI] [PubMed] [Google Scholar]
- 47.Van der Geest S, Whyte SR, Hardon A. The anthropology of pharmaceuticals: a biographical approach. Annu Rev Anthropol. 1996;25:153–178. [Google Scholar]
- 48.New Zealand Government Parliament Counsel Office. Medicines Act 1981. Available at: http://www.legislation.govt.nz/act/public/1981/0118/latest/DLM53790.html. Accessed July 25, 2013. [Google Scholar]
- 49.US Food and Drug Administration. Federal Food, Drug, and Cosmetic Act (FD&C Act) Available at: http://www.fda.gov/RegulatoryInformation/Legislation/FederalFoodDrugandCosmeticActFDCAct. Accessed July 26, 2013. [Google Scholar]