Abstract
Objectives. We evaluated health outcomes associated with in-home interventions in low-income urban households with children with asthma.
Methods. A comprehensive health and environmental assessment and subsequent intervention were completed in 116 households with 170 enrolled children with asthma. Home health workers provided household safety, asthma prevention education, and targeted environmental intervention to decrease asthma triggers and improve household safety. We collected environmental data with questionnaire and dust samples and health information with a questionnaire incorporating the American Academy of Pediatrics Children’s Health Survey for Asthma and other instruments at baseline and at follow-up 11 to 12 months later to evaluate the impact of the intervention on the health of the child and family in Lowell, Massachusetts, from September 2009 to January 2012.
Results. The diverse study population of low-income children showed a statistically significant health improvement from baseline to follow-up. The cost of the interventions (not including personnel) was $36 240, whereas the estimated medical savings over a 4-week assessment period was $71 162, resulting in an estimated annual savings of about $821 304.
Conclusions. Low-cost, multicomponent interventions decrease all measures of asthma severity and health care utilization in a diverse population of urban children.
The Lowell Healthy Homes Program in Massachusetts targeted asthma, the most common chronic childhood disease. Asthma has many known indoor environmental triggers, including dust, pests, smoke, and pets. Children are particularly vulnerable to home hazards and may develop lifelong health problems because of their home environment.1 In-home interventions to decrease triggers of childhood asthma involving remediation and education provided by community health workers has been reported.2–4 The federal government funded this initiative in Lowell, Massachusetts, in part because of its diverse demographic urban communities that have old, substandard housing and associated health risks. The project goal was to reduce the asthma burden and improve health outcomes for children with asthma and their families through home environmental assessments and individualized interventions focused on reducing indoor allergen levels and asthma triggers.
Massachusetts is located in the Northeast, where asthma rates are higher than are those in other regions of the United States.5 Lowell schoolchildren’s asthma prevalence (13.0%) is higher than the statewide average (10.9%).6
The 2010 US Census showed that Lowell’s population was 106 519, of which 47.2% were minority residents and 11.3% were of Puerto Rican descent (the largest subset of the 17.3% Hispanic residents).7 According to the National Health Statistics report on asthma prevalence in the United States, those of Puerto Rican descent have the highest asthma rate, twice the rate of the general population (16.6% vs 8.2%).5 The local and state rates for emergency department discharges and inpatient hospitalizations for asthma reveal that the hospitalization rate for Lowell’s children with asthma is almost twice the state average for the composite years 2006 to 2008.8
The University of Massachusetts, Lowell directed this community intervention with local collaborators, including a federally funded community health center, housing authority, community development corporation, multiservice community action agency, and first-time home buyers education program. The project drew on our team’s unique experience in developing cross-cultural healthy home interventions to improve the quality of housing in Lowell through a multitrigger, multicomponent, personalized home environmental intervention with home health assessment workers (HHAWs) and an environmental assessor.
METHODS
In this observational study, we assessed the health of enrolled children with asthma before and 11 to 12 months after the home and educational intervention.
Participants and Recruitment
We recruited participants using outreach through pediatricians’ offices and the Lowell Community Health Center, appearances on local radio and television shows, and flyer distribution and presentations at community partners’ events. The Coalition for a Better Acre’s outreach worker also conducted regular door-knocking campaigns that generated several recruitment leads.
HHAWs from the Lowell Community Health Center conducted enrollment screening during follow-up telephone interviews. To be eligible, families had to have at least 1 child younger than 15 years whom a doctor had diagnosed as having asthma; they had to reside in Lowell, Massachusetts, and the child had to spend the majority of nights in that household.
Families were enrolled between September 2009 and February 2011. Final assessments were done 11 to 12 months later, between September 2010 and January 2012. We obtained informed consent forms in English, Khmer, or Spanish from each participating family. We gave families completing the full program a $50 gift card to a local department store.
Healthy Home Intervention
We grounded the intervention on a health and environmental assessment involving environmental assessor and HHAW field visits to the participants’ homes. The number of visits to each participant family’s home over the 1-year period ranged from 4 to 9 depending on the need for education, remediation, and outside contract work. The environmental assessor used a checklist-style walkthrough assessment tool that identified the presence and extent of asthma triggers in the home and a questionnaire designed to capture behavioral factors that influence the indoor environment. As the environmental assessor conducted the walkthrough portion of the assessment, the HHAW conducted the health questionnaire with the caregiver. The entire home visit lasted 1 to 2 hours, depending on the number of children with asthma who were assessed (1–4). The project staff met to review assessment data after the initial assessment to individualize the remediation plan.
We implemented the customized remediation plan over 1 to 6 home visits (some families had additional visits by outside contractors), depending on the extent of remediation needed. Remediation plans included integrated pest management, commercial cleaning, providing healthy home cleaning equipment and supplies (e.g., vacuums with high-efficiency particulate absorption filters, green cleaning chemicals), education, and, in some cases, structural interventions (data available as a supplement to the online version of this article at http://www.ajph.org). During these visits, we taught caretakers how to recognize and mitigate asthma triggers and safety hazards.
About 6 months after the initial home assessment and at least 1 month after completing the intervention (to provide time for the intervention to take effect), HHAWs conducted a midterm assessment using abbreviated versions of the initial assessment tools to reinforce the healthy homes education. They reiterated educational items and replenished supplies as needed. The HHAW conducted a final assessment 11 to 12 months after the initial assessment to ensure the baseline and final assessments were collected in the same season to control for seasonal factors that might influence asthma symptoms. The final assessment consisted of the full health assessment tool and an abbreviated version of the environmental assessment tool to measure health and environmental indicator changes.
Assessment Tools
Asthma status measures and utilization data.
The study protocol included the use of the Children’s Health Survey for Asthma (CHSA), which the American Academy of Pediatrics developed. The validity and reliability of this questionnaire tool has been studied and tested.9,10 The CHSA is used to describe the health of children and families in 5 domains: physical health of the child, social activity of the child, social activity of the family, emotional health of the child, and emotional health of the family. We included additional questions focusing on asthma plan and management, rhinitis, eczema, cough, phlegm, inhaler use, family member ages, and household income.
The CHSA also collected data on hospitalizations, doctor office visits, and emergency department visits. The CHSA questionnaire is designed for use with a 2-, 4-, or 8-week recall period. Our study used a 4-week recall period (e.g., During the past 4 weeks, how many times has your child stayed overnight in the hospital because of asthma?).
Environmental checklist and questionnaire.
The environmental assessor administered a general, outdoor allergens, and safety survey, which included questions to identify the following potential asthma triggers: pests (roaches and mice), combustion sources, moisture and mold, dust mites, furry pets, outdoor allergens, general indoor air pollution, and smoking. We also employed a general environmental health and safety checklist to examine the overall home and each room.
In addition to the questionnaire and visual assessment, if the presence of mice or cockroaches was suspected or reported, we collected a floor dust allergen sample in the kitchen using the US Department of Housing and Urban Development’s Healthy Homes Vacuum Dust Sample Collection Protocol for Allergens. Indoor Biotechnologies (Charlottesville, VA) then analyzed samples for roach allergen (Bla g1) and mouse allergen (Mus m1).
Health Care Cost Savings Assessment
To determine the reduction in urgent care cost resulting from our interventions, we obtained data from the Massachusetts Department of Public Health for hospitalization for asthma per usage cost of an average of $4922 and an average emergency department visit for asthma per usage cost of $834 in Lowell hospitals.
In addition, we determined an average cost of $100 per doctor visit for asthma from local pediatricians’ offices. We then calculated the utilization cost savings by multiplying the decreased number of occurrences in urgent care by per utilization cost to determine total cost reductions in utilization.
Analysis
We used double entry of health data from the health questionnaire to ensure validity of questionnaire entry. We then checked data for comparability, cleaned the data, and reconciled discrepancies with the original paper questionnaires.
We computed the CHSA scales using SAS, version 9.2 (SAS Institute, Cary, NC) with the method detailed in the CHSA user’s guide.11 We determined the score from answers to questions on the CHSA. The score uses a scale of 0 to 100 in 5 domains. If data were missing, we could not determine a domain score for that child.
We performed a further, postdata collection analysis to classify each child with asthma as high risk or non–high risk. We developed the definition of high risk on the basis of severity of asthma as outlined in the National Asthma Education and Prevention Program Expert Panel Report 3, Guidelines for the Diagnosis and Management of Asthma.12 As we could not fully classify children by asthma severity in an analysis using the questionnaire data collected, we placed children in the high risk category if they met one of the following 5 criteria: hospitalized in the past 4 weeks, had 2 or more emergency department visits in the past 4 weeks, reported sleeping difficulties because of asthma all of the time in the past 4 weeks, ever used steroids more than 4 times in 6 months, or were ever intubated.
We compared pre- and postintervention CHSA scores using the change in the paired participant pre- and postscores. We determined the change in health care utilization using the paired participant change as well. We analyzed the change in medication use with the paired pre- and postintervention data using a test of proportion.
We used the Wilcoxon rank sum test to analyze the change in CHSA scores for the high-risk participants. We performed all statistical analysis using SAS, version 9.2, or Stata, version 11 (StataCorp LP, College Station, TX).
RESULTS
We enrolled 160 households with 245 children with asthma younger than 15 years; 116 households with 170 children with asthma completed the full yearlong study.
The baseline demographics of the children who completed the study and those who did not are presented in Table 1. The 2 groups were very similar, with the only statistically significant difference being that Whites (12% of study participants) were more likely to complete the study. The population was diverse, with Hispanic being the most frequent ethnic origin identified. The mean age at enrollment was 6 years, and boys were more often represented than were girls. Pests were the most common indoor allergen in our population, with 29% of households reporting rodents and 30% reporting cockroaches.
TABLE 1—
Demographics of Children Not Completing Study Vs Children Completing Study: Healthy Homes Program; Lowell, MA; September 2009–January 2012
| Variable | Children Not Completing Study (n = 75), No.a (%) or Mean | Children Completing Study (n = 170), No.a (%) or Mean |
| Respondent | ||
| Parent | 68 (90.7) | 162 (94.7) |
| Other | 7 (9.3) | 9 (5.3) |
| Respondent gender | ||
| Male | 4 (5.3) | 7 (4.1) |
| Female | 71 (94.7) | 163 (95.9) |
| Child race/ethnicity | ||
| Black | 5 (6.7) | 8 (4.7) |
| White* | 3 (4) | 21 (12.4) |
| Asian | 8 (10.7) | 26 (15.3) |
| Hispanic | 43 (57.3) | 90 (52.9) |
| Other | 16 (21.3) | 25 (14.7) |
| Child sex | ||
| Male | 41 (54.7) | 101 (59.4) |
| Female | 34 (45.3) | 69 (40.6) |
| Parent marital status | ||
| Married | 9 (12) | 38 (22.4) |
| Not married | 66 (88.8) | 132 (77.7) |
| Mother’s education | ||
| Any college | 20 (27) | 56 (33.3) |
| High school | 22 (29.7) | 57 (33.9) |
| < high school | 31 (41.9) | 52 (31) |
| Don’t know | 1 (1.4) | 3 (1.8) |
| Father’s education | ||
| Any college | 10 (25.6) | 18 (20.2) |
| High school | 16 (41) | 41 (46.1) |
| < high school | 6 (15.4) | 19 (21.4) |
| Don’t know | 7 (18) | 11 (12.4) |
| Household income | ||
| 0%–50% area median income | 58 (90.7) | 144 (84.7) |
| ≥ 51% area median income | 3 (4) | 12 (7.1) |
| Not reported | 4 (5.3) | 14 (8.2) |
| Smoker in primary home | 10 (13.3) | 28 (16.5) |
| Smoker in secondary home | 1 (2.2) | 2 (2.1) |
| High-risk asthma group | ||
| Yes | 33 (44) | 65 (38.2) |
| No | 42 (56) | 105 (61.8) |
| Child age, y | 5.97 | 6.08 |
Because of missing values, numbers for some variables do not equal the total number of children completing the study and children not completing the study.
*Difference is significant: P = .04.
Most children lived in pet-free and smoke-free homes and in households with incomes below 50% of area median income.
CHSA Scores and Health Care Utilization Outcomes
The health care utilization and symptoms from the questionnaire at baseline and follow-up are presented in Table 2. The mean number of symptoms (e.g., wheeze, asthma attacks) and health care utilizations related to asthma (i.e., emergency department visits, doctor visits, and hospitalizations) are presented in Table 2. The changes in reported numbers from baseline to follow-up are all statistically significant. Particularly striking is the 8 hospitalizations in the previous 4 weeks at baseline, with none reported in the follow-up period.
TABLE 2—
Change in Asthma Severity Indicators: Healthy Homes Program; Lowell, MA; September 2009–January 2012
| Variable | Baseline (n = 170),a No. (%) or Mean | Follow-Up (n = 170),a No. (%) or Mean | Changeb (95% CI) |
| Past 4 wk | |||
| Episodes of wheezing | 6.40 | 2.30 | 4.1 (2.7, 5.6) |
| Asthma attacks | 0.80 | 0.20 | 0.6 (0.2, 1.0) |
| Emergency department visits | 0.20 | 0.04 | 0.2 (0.1, 0.2) |
| Doctor visits | 0.70 | 0.20 | 0.4 (0.2, 0.6) |
| Hospitalization | 0.05 | 0.00 | 0.1 (0.01, 0.8) |
| CHSA scores | |||
| Child physical health | 66.80 | 89.30 | −23.3 (−26.9, −19.8) |
| Child activity | 84.90 | 93.00 | −8.4 (−11.5, −5.3) |
| Child emotional health | 67.90 | 88.00 | −20.5 (−25.8, −15.2) |
| Family activity | 88.70 | 97.40 | −8.7 (−11.5, −5.8) |
| Family emotional health | 71.20 | 81.10 | −9.9 (−11.9, −7.8) |
| High asthma risk group | |||
| Yes | 65 (−38.2) | 44 (−25.9) | 12.4 (2.5, 22.2) |
| No | 105 (−61.8) | 126 (−74.1) | |
| Current asthma medicine use | |||
| Every d | 58 (−34.1) | 39 (−23.9) | 11.2 (1.7, 20.7) |
| ≤ few times/wk | 112 (−65.9) | 130 (−76.5) | |
| Asthma medicine use, past 4 wk | |||
| Yes | 145 (−88.4) | 101 (−61.6) | 26.8 (17.9, 35.7) |
| No | 19 (−11.6) | 63 (−38.4) | |
| Average puffs rescue medicine/d | |||
| None | 83 (−48.8) | 99 (−58.6) | −9.8 (−20.3, −0.8) |
| Some | 87 (−51.2) | 70 (−41.4) | |
| Difficulty sleeping all the time | |||
| Yes | 20 (−11.9) | 4 (−2.4) | 9.6 (4.2, 15.0) |
| No | 148 (−88.1) | 166 (−97.7) |
Note. CHSA = Community Health Survey for Asthma; CI = confidence interval.
Because of missing values, numbers for some variables do not equal the total of baseline and follow-up participants.
Change is for paired values.
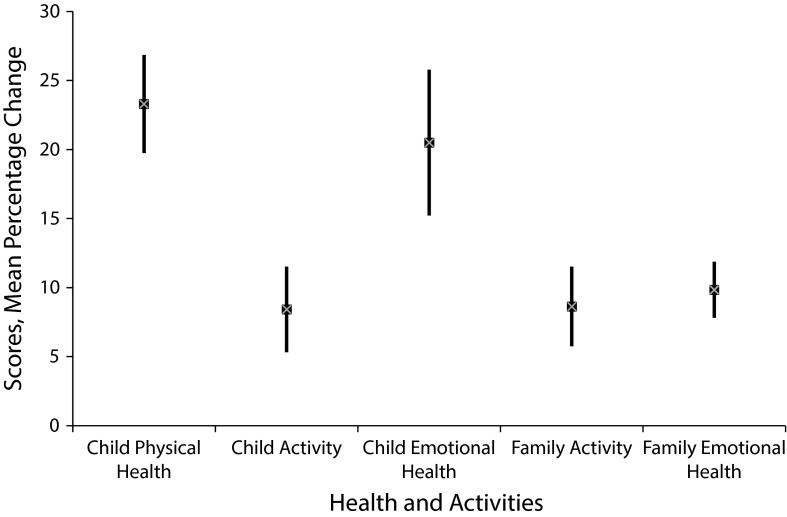
The CHSA scores are measured on a scale of 0 to 100 (higher numbers represent improved physical or emotional health). All 5 domain scores showed significant improvement from baseline to follow-up. The mean percentage change in the scores for the 5 domains is shown in Figure 1.
FIGURE 1—
Mean percentage change in Community Health Survey for Asthma scores with 95% confidence intervals: Healthy Homes Program; Lowell, MA; September 2009–January 2012.
Medication Use
Our questionnaire contained 3 questions concerning medicine use, and all 3 showed decreased use of medication at follow-up compared with baseline. One question asked whether any medications for asthma had been used in the previous 4 weeks. At baseline, 19 children were reported as using no medication. At follow-up 63 children used no medication, for a drop from 85% to 59% of our study participants (P ≤ .001 for 2-sided test of proportion). Only 5 children who did not use medication at baseline were reported using medication at follow-up, whereas 46 children reported using medication at baseline but not at follow-up.
We assigned 65 of 170 children at baseline and 44 of 170 at follow-up to the high risk category. This is a significant percentage drop from 38% to 26% (P = .02 for 2-sided test of proportion). The CHSA scores at baseline of those at high risk were lower (indicating more impairment) than were the scores of children not deemed high risk. Four of the 5 domains scored for the CHSA—physical health, activity child, emotional child, and emotional family—were statistically significantly lower for the high-risk than the non–high-risk children at baseline. At follow-up, we examined the change in CHSA scores from baseline to follow-up for high-risk and non–high-risk participants as defined at baseline. The improvement in CHSA scores in each of the 5 domains was larger for those deemed high risk. By Wilcoxon rank sum, this increase reached statistical significance for the child activity and family activity domains.
Cost
The in-home remediation cost included health and safety items that field staff provided and outside contract work, totaling $31 032 and $14 210, respectively. The cost of the in-home remediation was $192 per child, for a total of $32 640 for the 170 children who completed the study. We compared reductions in hospitalization, emergency department visits, and doctor visits owing to asthma between the 4-week period before initial assessments and the 4-week period before the final assessment 1 year later and estimated a total savings of $71 162 (Table 3).
TABLE 3—
Net Savings Resulting From Intervention: Healthy Homes Program; Lowell, MA; September 2009–January 2012
| Variable | Per Usage Cost, $ | Decrease in Occurrence | 4-Week Recall Period (∼1-Month Savings), $ | 6-Month Savings,a $ | 12-Month Savings,a $ |
| Urgent care | |||||
| Hospitalizationb | 4922 | 8 | 39 376 | 236 256 | 472 512 |
| Emergency departmentb | 834 | 29 | 24 186 | 145 116 | 290 232 |
| Doctor visitsc | 100 | 76 | 7600 | 45 600 | 91 200 |
| Decrease in costs | 71 162 | 426 972 | 853 944 | ||
| Intervention cost | 32 640 | 32 640 | 32 640 | ||
| Net savings | 38 522 | 394 332 | 821 304 |
Six- and 12-month savings calculated as 4-week recall (∼1-month) savings times either 6 or 12.
The hospitalization and emergency department data were provided by the Massachusetts Department of Public Health assessment of average charges in Lowell in 2010 owing to usage because of asthma.
The $100 per doctor visit is an estimated average cost on the basis of discussions with local doctors’ offices.
After deducting the $32 640 intervention cost, we estimated a net savings of $38 522 for the 4-week period, $394 342 for 6 months, and $821 304 for 12 months (Table 3).
DISCUSSION
The postintervention data showed a significant improvement in CHSA scores and reduced health care utilization and medication use. The validated measurement tool (CHSA) showed improvement in all 5 domains of child and family physical and emotional health. Health care utilization data showed fewer hospitalizations, emergency department visits, and doctor office visits.
The combined findings of improved asthma controls with decreased health care utilization and medication use are important. We saw improvement in quality of life as well as reduced health care utilization and medication use. The children’s asthma indicators improved, which we believe is why children used less medication at follow-up.
The housing environment was poor in many cases: nearly 50% of Lowell’s housing stock was built before 1940.13 The intensely urban neighborhood with multiple businesses and nearby transportation byways may increase the amount of time children spend indoors and could be a factor in the home interventions having such a significant effect.
The home interventions also improved outcomes of environmental indicators. In a future article, we will describe the change of environmental indicators in more detail.
Strengths of the study included employing lay home health workers who were culturally aware and proficient in the language of the enrolled families. The home visits provided assessment, education, and remediation in a relaxed setting. The baseline and follow-up health assessments were performed 1 year apart to account for seasonal discrepancies in asthma.
Another strength of the study was the relatively low-cost intervention. Excluding the cost of the project staff, supplies, materials, and contract work for cleaning and pest management totaled $45 242. Per home cost for the 160 individually targeted interventions was $283 and per child cost was $192. Home remediation costs for asthma can be high. In a recent review of the economic value of home asthma interventions, the yearly cost ranged from $231 to $14 858 per participant.14
The study’s health outcome improvements also produced noticeable cost savings for families, health care providers, and society. For the 2 comparative 4-week intervals the drop in hospitalizations, emergency department visits, and doctor visits owing to asthma resulted in a savings of $71 162. This is a decrease in costs in 4-week urgent care of $419 per child (n = 170), which compares favorably with those of other studies.15,16 Note that the Seattle and King County study found an estimated decrease in 2-month urgent care costs of $201 to $334 per child,15 whereas the National Cooperative Inner City Asthma study found an average decrease in medical costs of $245 per child postintervention.16
Although we did not collect follow-up data beyond the 4-week recall period, if we assume the same rates for a full year, the potential cost savings are more significant. For example, if this rate of hospitalizations, emergency department visits, and doctor visits were assumed to have happened monthly for 6 months in a year, then the total decrease in costs would be $426 972, which represents a decrease in urgent care costs of $2512 per child. If we assume a scenario in which this urgent care utilization captured during the 4-week period before baseline assessment represented ongoing monthly urgent care needs, the total decrease in costs over 1 year would be $853 944, or $5023 per child (1 month recall savings × 12).
It should also be noted that we estimated the cost savings on the basis of health outcome data for 170 children for whom we were able to collect follow-up health assessments. There are another 64 children who lived in homes receiving completed interventions for whom we were not able to collect final health outcome data because of nonparticipation in the follow-up survey.
At follow-up, the number of children no longer in the high-risk group having 1 or more indicators of more persistent or severe asthma was significantly lower than was the number at baseline. Two of the indicators of the high risk designation (ever had frequent steroid use or intubation) could not be changed, so the results are truly noteworthy because some children could not change their designation even if they showed improvement. It is important that these children as a whole improved as much or more than did those deemed not at high risk. The increased improvement is notable as a step toward determining whether home interventions are more effective for individuals with more severe asthma, a research gap recently identified.17
A final important note is that our study population is from a high-risk demographic for asthma burden. In the state of Massachusetts, the age-adjusted rates of asthma hospitalizations among Blacks were 3.1 times higher and among Hispanics were 2.7 times higher than were the rates of Whites.18 Emergency department visits in Massachusetts have similar rate differences. Of the population completing our study, 53% was Hispanic, and the most common Hispanic descent in Lowell is Puerto Rican—a very high-risk group for asthma.5
Limitations
Limitations of this study include that we did not use a control group and that asthma can potentially improve over time without interventions. We excluded a control group because our funder’s goal was to maximize intervention benefits and we believed it was unethical to limit the positive effects among study participants. Our data collected by caregiver questionnaire described health care outcomes and utilization in the previous 4 weeks. The data did not cover the entire year of follow-up.
We did not validate the questionnaires against medical records for accuracy concerning health care utilization. To look at an approximate comparison over the closest possible time frame, we reviewed state and local data for fiscal years 2010 and 2011 for age-specific (aged ≤ 14 years) asthma emergency department visits.19 Although not a direct comparison, the state and Lowell rates data do show a decrease from 2010 to 2011 but not in the same magnitude as those in our study. Our study participants showed hospitalization change from 8 total to zero and emergency department mean visits from 0.19 to 0.04 (79% reduction). The statistics for Lowell obtained from the state department of public health showed total emergency department visits dropping from 196 to 175 in fiscal year 2011 (11% reduction).19
Another limitation is that it remains unclear which part of the intervention was most helpful in improving child and family physical and emotional health. This is consistent with other multicomponent intervention studies, but one possibility is that the lay workers provided crucial education and support that contributed to the improvement in health outcomes.17 Nevertheless, there could be some component of a Hawthorne or placebo effect with compassionate evaluation and remediation in these homes.
There was an approximately 30% loss to follow-up rate, which is not unusual among low-income, diverse populations. From the data analyzed we have no indication that these children were different from those who completed the study. Finally, the CHSA has been validated in children aged 3 to 12 years, and our study included children aged 0 to 14 years at enrollment.
Conclusions
Childhood asthma continues to be a significant health problem for US children, especially in urban environments. Environmental asthma triggers include both indoor and outdoor sources. Allergens, dust, pets, mold, and tobacco smoke are known indoor asthma triggers. We have demonstrated that a relatively low-cost comprehensive home environmental intervention can significantly improve the health and emotional well-being of diverse, low-income children with asthma and their caregivers living in an urban environment. The potential for health care savings in decreased medication use and health care utilization is significant. Medical providers and insurers need to consider the utilization of such interventions, but further studies are needed on the optimal intervention design.20
Acknowledgments
Funding was provided by the US Department of Housing and Urban Development, Office of Healthy Homes and Lead Hazard Control (grant MALHH0171-8).
The authors acknowledge and thank Stephanie Chalupka (co-principal investigator) at Worcester State University for her contribution to the original study idea and data collection design as well as for the initial training of field staff. We also acknowledge our field staff (Carla Caraballo and Bophamony Vong, Lowell Community Health Center, and Joanne Vaillette and Fred Youngs, University of Massachusetts, Lowell) and community partners (Coalition for a Better Acre, Community Teamwork, Lowell Community Health Center, Lowell Housing Authority, and Merrimack Valley Housing Partnership) for their contributions to the project.
Human Participant Protection
The University of Massachusetts, Lowell institutional review board approved the study before data collection began and provided annual review of the study’s progress.
References
- 1.Etzel RA. How environmental exposures influence the development and exacerbation of asthma. Pediatrics. 2003;112(1 pt 2):233–239. [PubMed] [Google Scholar]
- 2.Wu F, Takaro TK. Childhood asthma and environmental interventions. Environ Health Perspect. 2007;115(6):971–975. doi: 10.1289/ehp.8989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bryant-Stephens T, Kurian C, Guo R, Zhao H. Impact of a household environmental intervention delivered by lay health workers on asthma symptom control in urban, disadvantaged children with asthma. Am J Public Health. 2009;99(suppl 3):S657–S665. doi: 10.2105/AJPH.2009.165423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Takaro TK, Krieger JW, Song L. Effects of environmental interventions to reduce exposure to asthma triggers in homes of low-income children in Seattle. J Expo Anal Environ Epidemiol. 2004;14(suppl 1):S133–S143. doi: 10.1038/sj.jea.7500367. [DOI] [PubMed] [Google Scholar]
- 5.Akinbami LJ, Moorman JE, Liu X. Asthma prevalence, health care use and mortality: United States, 2005–2009. Natl Health Stat Reports. 2011;(32):1–14. [PubMed] [Google Scholar]
- 6.Massachusetts Department of Public Health, Bureau of Environmental Health. Pediatric asthma surveillance in Massachusetts 2008–2009. 2012 Available at: http://www.mass.gov/eohhs/consumer/community-health/environmental-health/public-health-track/asthma-env/pediatric-asthma-surveillance-in-massachusetts.html. Accessed January 5, 2013. [Google Scholar]
- 7.US Census Bureau. Factfinder2. Available at: http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?src=bkmk. Accessed January 4, 2013.
- 8.Massachusetts Department of Public Health. Asthma report for Lowell mortality and hospital data. Available at: http://www.mass.gov/eohhs/docs/dph/masschip/asthma/asthmacity-townlowell.rtf. Accessed November 7, 2012.
- 9.Asmussen L, Olson LM, Grant EN, Fagan J, Weiss KB. Reliability and validity of the children’s health survey for asthma. Pediatrics. 1999;104(6):e71. doi: 10.1542/peds.104.6.e71. [DOI] [PubMed] [Google Scholar]
- 10.Sharek PJ, Mayer ML, Loewy L et al. Agreement among measures of asthma status: a prospective study of low-income children with moderate to severe asthma. Pediatrics. 2002;110(4):797–804. doi: 10.1542/peds.110.4.797. [DOI] [PubMed] [Google Scholar]
- 11.American Academy of Pediatrics. Children’s Health Survey for Asthma (CHSA) User’s Guide. Elk Grove Village, IL; 2000. [Google Scholar]
- 12.National Asthma Education and Prevention Program, Third Expert Panel on the Diagnosis and Management of Asthma. Expert panel report 3: guidelines for the diagnosis and management of asthma. 2007 Available at: http://www.ncbi.nih.gov/books. Accessed August 26, 2012. [Google Scholar]
- 13.City of Lowell, MA. Office of the City Manager, Department of Planning, and development master plan update: existing conditions report. 2011 Available at: http://www.lowellma.gov/depts/dpd/master_plan/complete_masterplan/master-plan-update/reports. Accessed January 4, 2013. [Google Scholar]
- 14.Nurmagambetov TA, Barnett SL, Jacob V et al. Economic value of home-based, multi-trigger, multicomponent interventions with an environmental focus for reducing asthma morbidity. Am J Prev Med. 2011;41(2S1):S33–S47. doi: 10.1016/j.amepre.2011.05.011. [DOI] [PubMed] [Google Scholar]
- 15.Krieger JW, Takaro TK, Song L, Weaver M. The Seattle–King County Healthy Homes Project: a randomized, controlled trial of a community health worker intervention to decrease exposure to indoor asthma triggers. Am J Public Health. 2005;95(4):652–659. doi: 10.2105/AJPH.2004.042994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sullivan SD, Weiss KB, Lynn H et al. National Cooperative Inner-City Asthma Study (NCICAS) Investigators. The cost-effectiveness of an inner-city asthma intervention for children. J Allergy Clin Immunol. 2002;110(4):576–581. doi: 10.1067/mai.2002.128009. [DOI] [PubMed] [Google Scholar]
- 17.Crocker DD, Kinyota S, Dumitru GG et al. Effectiveness of home-based, multi-trigger, multicomponent interventions with an environmental focus for reducing asthma morbidity: a community guide systematic review. Am J Prev Med. 2011;41(2S1):S5–S32. doi: 10.1016/j.amepre.2011.05.012. [DOI] [PubMed] [Google Scholar]
- 18.Massachusetts Department of Public Health. Burden of Asthma in Massachusetts. Boston, MA: Asthma Prevention and Control Program; 2009. [Google Scholar]
- 19.Massachusetts Department of Public Health Asthma Prevention and Control Program. Data Source MA: FY 2009–2011. 2012 Massachusetts Emergency Department Discharge Database. [Google Scholar]
- 20.Atherly AJ. The economic value of home asthma interventions. Am J Prev Med. 2011;41(2S1):S59–S61. doi: 10.1016/j.amepre.2011.05.008. [DOI] [PubMed] [Google Scholar]