Abstract
With this article, we develop the Drinking Water Disparities Framework to explain environmental injustice in the context of drinking water in the United States. The framework builds on the social epidemiology and environmental justice literatures, and is populated with 5 years of field data (2005–2010) from California’s San Joaquin Valley. We trace the mechanisms through which natural, built, and sociopolitical factors work through state, county, community, and household actors to constrain access to safe water and to financial resources for communities. These constraints and regulatory failures produce social disparities in exposure to drinking water contaminants. Water system and household coping capacities lead, at best, to partial protection against exposure. This composite burden explains the origins and persistence of social disparities in exposure to drinking water contaminants.
“Isn’t the issue of contaminated water just an issue of economies of scale, where small systems face the biggest problems?”
“In talking about environmental injustices and contaminated drinking water, are you implying that someone is deliberately polluting people’s water?”
“If there is no statistical correlation between race, class, and water quality, doesn’t that mean there is no injustice?”
—Questions commonly encountered during fieldwork in the San Joaquin Valley
Hundreds of small, rural communities in California and across the United States rely on unsafe drinking water sources that their modest means cannot mitigate. Research and grassroots efforts have drawn attention to high levels of contaminants in California’s San Joaquin Valley (the Valley)1; to inadequate services and infrastructure in US–Mexico border colonias2 and rural communities in the South3,4; and to bacteriological and chemical contamination in unregulated drinking water sources in the Navajo Nation.5 Our own earlier research, conducted between 2005 and 2011, established that race/ethnicity and socioeconomic class were correlated with exposure to nitrate and arsenic contamination and noncompliance with federal standards in community water systems.6,7
But why do social disparities in access to safe water exist and persist in a country where most of the population has access to piped, potable water? A rich understanding of how disparities in access to safe drinking water are produced and maintained is essential for understanding environmental justice concerns and developing effective public health interventions. In this article, we highlight the mechanisms through which natural, built, and sociopolitical factors, along with state, county, and community actors, create a composite and persistent drinking water burden in the Valley. This research reflects the call by environmental justice scholars8,9 for more historically informed work on the causes and consequences of environmental injustice (i.e., disproportionate environmental burdens by race and class).
The drinking water and environmental justice literature has focused on how unequal access to infrastructure drives unequal access to safe drinking water. Wilson et al. have shown that disparities in “basic amenities” drive adverse health outcomes, especially in conjunction with poorly enforced health laws and building codes.4,10 VanDerslice’s infrastructure-oriented framework posits that the extent to which any aspect of water infrastructure—natural, built, or managerial—differs by racial or income disparities drives disparities in water quality, reliability, and cost.11 The literature also notes that small water systems are vulnerable to inadequate regulatory protection,12 and to uneven monitoring and reporting.13,14
Studies on equity and the built environment have discussed how historical and structural conditions shape lack of access to safe drinking water. These conditions include selective enforcement of drinking water regulations,15 noncompliance with federal standards,16,17 inequities in access to funding,18 and (the absence of) a community’s political power in accessing a safe water supply.19 Research has also shown that cost of service extension and low ability to pay drive inadequate service provision2; that municipalities provide or deny access to basic services by determining which areas to annex or exclude from their city boundaries4,10,20; and that segregation allows such determinations to continue.21 Thus the environmental justice and built environment literatures highlight the many causal factors of social disparities, but, to date, do not offer a comprehensive framework for tracing both the origins and persistence of disparities in exposure.
Here, social epidemiology offers a theoretical foundation for our analysis. In particular, an ecosocial epidemiological approach underscores the need to (1) explore the social production, or origins, of health disparities22,23; (2) uncover the multilevel factors that drive the distribution of disease,24,25 or, in our case, exposure; and (3) highlight the “agency and accountability” of multilevel actors in creating these disparities and embodiments of disease.22,24
Our work draws on several social epidemiology–inspired frameworks. These frameworks discuss how race, class, social factors,26,27 and multiple levels of decision-making22 can have an impact on exposure pathways.28 Sexton et al.26 expanded the traditional exposure–disease paradigm29 used in environmental health by positing that differential health risks may be associated with race and socioeconomic class because of exposure (e.g., proximity to source) and susceptibility-related (e.g., gender) attributes. Gee and Payne-Sturges refined Sexton et al.’s work with a multilevel perspective that explores how vulnerability intersects the exposure–disease paradigm.27 deFur et al. complemented this approach by showing that vulnerability can have an impact on exposure pathways between environmental factors and receptors (i.e., individual, community, or population) and response pathways between receptors and outcomes.28 In sum, social epidemiology frameworks emphasize how and why health disparities may arise, and, to some extent, why they persist. They do not, however, focus specifically on drinking water.
We present the Drinking Water Disparities Framework, which builds on the social epidemiology and the infrastructure-centric frameworks discussed previously in 3 main ways. First, our framework describes which infrastructural factors shape disparities, as VanDerslice11 does, but we add the role of social and political factors. VanDerslice’s article hypothesizes that disparities in water-related infrastructure vary by race and class, and supports this claim through the published literature; we use primary field data to trace how and why these disparities exist and also persist, as a consequence of built, natural, and sociopolitical factors. For instance, we show how the historical marginalization of poor communities, coupled with poor source water quality, determines the condition of their physical infrastructure and results in exposure. Second, in line with Wilson,30 we highlight the role of multilevel actors, but we emphasize how specific decisions at different levels, past or present, intentional or accidental, drive disparities in access to drinking water. For example, we show how municipal redlining, limited county oversight, and low household finances together impede mitigation of contaminated water. Third, our multilevel framework extends the classic exposure–disease paradigm29 to show that water system and household coping mechanisms, intended to alleviate exposure, create a feedback loop through which disparities in drinking water quality may be exacerbated. In this way, the framework shows how drinking water disparities comprise both external stressors and susceptibility to them, as well as the capacity, or lack thereof, to cope.28,31
Thus, we emphasize the role of historical and structural factors, and trace the mechanisms through which these lead to exposure disparities. We argue that these structural factors are not deterministic, but that communities and individuals exercise agency within the structures that constrain them. The extent of this agency also has an impact on exposure. A framework that pays attention to history as well as contemporary processes, and to structures as well as agency, reveals both the pathways to unsafe water and the points of leverage at which exposure to contaminants can be reduced.
Five years of primary data collection in California’s San Joaquin Valley provide the empirical grounding for our framework. This richly nuanced data set reveals not only the role of multilevel actors in shaping disparities, but also the lived experiences of households and communities who struggle for safe water. Ultimately, our framework outlines a “composite burden,” composed of exposure to contaminants and inability of socially vulnerable communities to mitigate contamination. We argue that this composite burden leads to persistent exposures and social disparities in exposure to poor drinking water.
THE DRINKING WATER DISPARITIES FRAMEWORK
The Drinking Water Disparities Framework is presented in Figure 1. It is empirically based on interviews and participant observation with San Joaquin Valley residents, state (i.e., California Department of Public Health) and county drinking water regulators, water board members in unincorporated communities, participants at water conferences and environmental justice meetings, and community-based organizations in the southern San Joaquin Valley that took place from 2005 to 2010.
FIGURE 1—
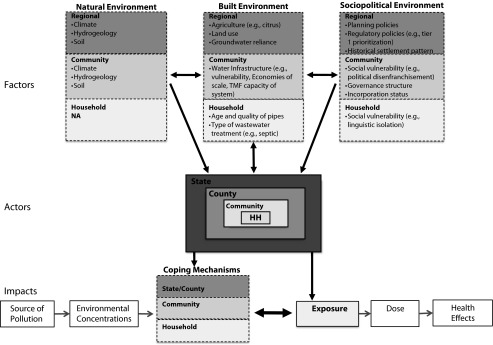
The Drinking Water Disparities Framework.
Note. HH = household; NA = not applicable; TMF = technical, managerial, and financial. Multilevel environmental factors act through multilevel actors to have an impact on exposure and coping capabilities. Race and class characteristics are embedded in many of the factors and actors throughout.
Methods
We developed a semistructured interview guide to interview all 5 California Department of Public Health district engineers in the Valley, its regional engineer, and 3 county-based regulators who regulate systems with fewer than 200 connections. Our questions focused on drinking water problems and impacts; historical factors influencing water quality; institutional, financial, and regulatory factors that have an impact on drinking water quality; perceived connections between environmental justice and drinking water; and the lived experience of drinking water challenges (whether professionally or personally). We used a similar protocol to interview 5 key leaders of the Valley’s key water nonprofits focused on service provision, technical assistance, and advocacy and 3 prominent community water leaders.
In addition, we derived community-based observations and additional qualitative data from a larger collaboration between the University of California, Berkeley, and the Community Water Center, in which the first author conducted ethnographic research of the Center’s organizing and advocacy efforts (community meetings, environmental justice tours, regional water planning meetings, Tulare County Water Board meetings, etc.), had numerous discussions with the Center’s staff and community base, and attended community water meetings in the communities of Seville, Alpaugh, Tooleville, and Plainview—all locations where the Community Water Center works. Interviews were conducted in Spanish and English. We also conducted extensive newspaper analysis in Alpaugh, Lanare, and Tooleville. Data on drinking water quality and Safe Drinking Water Act (SDWA) violations32,33 in community water systems across the Valley complemented the qualitative field data and are cited throughout the article.
Framework Description
Figure 1 depicts the factors within the 3 environments (natural, built, and sociopolitical) that drive drinking water disparities across race and class. Table A (available as a supplement to the online version of this article at http://www.ajph.org) lists additional examples of driving factors either observed in the Valley or derived from the literature. The framework shows that these factors, when mediated through the actions or inactions of state, county, community, and household actors, jointly have an impact on exposure and coping capabilities. Viewed comprehensively, these multiple possible pathways or mechanisms can result in persistent exposures to water contamination that vary by the race and class of different communities.
Three “environments” contain the factors that drive the disparities. The natural environment in Figure 1 includes ecological characteristics such as soil types, hydrology, and climate—these cannot be altered except over a long time frame. The built environment represents human-modified spaces in which “people live, work and recreate”34(p24) such as agricultural land, buildings, and water infrastructure. The sociopolitical environment refers to institutional and group characteristics (e.g., community or household), including historical and present-day planning policies, governance practices, and community demographics. Each environment contains factors that act across 3 scales—conventionally called “levels” in the social epidemiology literature—the regional (including state and county), the community, and the household. Arrows connecting the 3 environments show the factors’ mutual interactions—citrus farming is a part of the built environment that affects the natural environment (e.g., water quality), but agriculture itself is influenced by natural characteristics such as climate and soil type. Dotted lines separating levels indicate that specific drivers of water access can occur at and influence multiple levels within an environment: degraded community-level water infrastructure can (but need not) interact with household infrastructure.
Factors in all 3 environments and across all 3 levels act through, and across, actors within 4 distinct levels relevant to the Valley: the state, the county, the community, and the household. National and within-state regions could potentially be included as additional levels, but, for this study, these are not central. The state and county levels correspond to political and geographic boundaries. State and county regulators function within their respective levels. The community is defined by the physical service area of a community water system that serves water year-round to at least 15 residential units or 25 people.35 A community could be an incorporated city with its own tax base, or it could be unincorporated. Municipal employees, community organizers or community groups, water board members, and nongovernmental organizations are contained within the community level. The household level is where drinking water is usually accessed, though exposure ultimately occurs at the individual level. Ordinary residents are contained within the household level.
Unlike other infrastructure-oriented analyses, our disparities framework emphasizes the role of multilevel coping mechanisms in influencing exposure by adding coping to the classic exposure–disease paradigm (bottom of Figure 1). In general, exposure to drinking water contaminants in excess of SDWA standards necessitates mitigation and requires a water system to implement a solution. However, when a water system is incapable of doing so, or while it waits to solve the contamination problem, households must individually respond. We show that exposure and coping are mutually constitutive, cyclical, and multilevel; the degree of exposure dictates the need for coping, and the degree to which coping mechanisms are successful directly influences exposure. This is indicated by bidirectional arrows in Figure 1. To the extent that coping is not successful by one actor (e.g., the water board), it necessitates coping by another (e.g., the household)—this is indicated by dotted lines within “coping.” Coping leads to additional costs, and these added costs also constrain future coping capacity. Jointly, these feedback cycles and resulting exposure and coping costs define what we have called a “composite drinking water burden.” In the next 2 sections we flesh out this framework with empirical evidence on how potential exposure occurs and how small community water systems cope.
The framework treats average exposure level and violations of maximum contaminant levels (MCLs) as measures of “potential risk” of negative health outcomes. Therefore, we focus on exposure as opposed to health outcomes. The reasons for this are 3-fold. First, health effects associated with common drinking water contaminants (e.g., nitrate and arsenic) in the Valley are well documented.36–42 Second, obtaining health outcome data associated with water quality served is often infeasible because there are multiple confounders and insufficient data available on them. Third, inequalities in environmental exposures are one important driver of racial/ethnic and socioeconomic health disparities,43 and are, therefore, important to consider in and of themselves.
THE FRAMEWORK IN ACTION
To understand how the framework works, one can start by tracing how multilevel factors acting through and across actors can drive exposure to drinking water contaminants.
Multilevel Factors and Actors Have an Impact on Exposure
To begin, the natural and built environments, such as hydrogeology and land use practices, shape source water quality, which in turn partially defines baseline contaminant levels. For example, the climate and soil of Tulare County’s eastern foothills create favorable growing conditions for citrus trees that use high amounts of nitrate fertilizer. Because the water table in this region is shallow (Figure A, available as a supplement to the online version of this article at http://www.ajph.org), nitrates can leach more rapidly into it and have a shorter travel time into well water.44 As a result, communities such as Tooleville, located on the eastern side of Tulare County, have some of the highest nitrate levels in the Valley.45 On the western side of the Valley, in communities such as Alpaugh, the Corcoran clay layer plays a converse role. This impermeable layer requires that community water systems relying on groundwater drill deeper wells,46 but at these deeper levels wells are likely to draw naturally occurring arsenic-laden water.47,48
Built and sociopolitical factors interact with natural factors to determine exposure levels at the community and household level. For example, the allocation of water rights and development of water resources in the Valley have played a direct role in determining drinking water quality. Government financing of large-scale water projects historically enabled the storage and conveyance of vast quantities of snowmelt from the Sierra Nevada Mountains and the California Delta to farmlands. Farmers received nearly unlimited surface water rights for agriculture,49 but 95% of the Valley’s residents were left to rely on groundwater for drinking.32 This might not have mattered, were it not for the baseline natural conditions of groundwater and agriculture’s contamination of it caused by chemical runoff from pesticides and fertilizers45,50; in 2007, 75% of all of California’s nitrate violations occurred in the Valley,32 the main source of which was agricultural fertilizer.51
Policies at multiple levels interact to explicitly deprive communities of adequate drinking water resources. For example, the 1973 Tulare County General Plan reads
Public commitments to communities with little or no authentic future should be carefully examined before final action is initiated. These non-viable communities would, as a consequence of withholding major public facilities such as sewer and water systems, enter a process of long term, natural decline as residents depart for improved opportunities in nearby communities.52(p2)
Among the 15 communities listed were Allensworth, Alpaugh, Lemon Cove, Plainview, Seville, and Tooleville. Many of these communities were once labor camps, or are currently unincorporated, without their own tax base and municipal representation to draw on for infrastructure improvements. This de jure discrimination results in the de facto discrimination of redlining, where designations of “nonviability” justify withholding of resources and thus allow for the perpetuation of poor infrastructure. Residents understand the ironies of these policies. A leader from one of the allegedly nonviable communities noted
One of the questions a lot of people ask me is, if the water’s so bad … why don’t you move? And I’m thinking, why would you want me to move? That’s my house. That’s my town. I was born and raised there… . Do you think by moving it’s going to get solved?
As with county-level plans, selective annexation at the city level has allowed water problems to persist. The City of Exeter is less than half a mile away from Tooleville and has used its municipal decision-making authority to (in effect) prolong exposure in Tooleville in 2 ways. First, since the 2000s, Exeter has cited prevailing wages as a barrier to extending pipelines to Tooleville. Two Senate Bills (SB X2 9 and SB 110) explicitly exempted the city from having to pay prevailing wage,53 but the city still dismissed requests for consolidation. Second, Exeter has selected other surrounding areas to which to expand. Figure B (available as a supplement to the online version of this article at http://www.ajph.org) shows Exeter’s planned expansion for 2020. Included in the areas where growth is planned are undeveloped agricultural parcels and ranchette houses toward the east. The growth areas extend in some cases to at least the same distance as Tooleville, but they do not extend toward Tooleville. Residents experience this as a case of “municipal underbounding”20: “If we were rich, we’d raise their tax base. But we’re poor, so they’re not interested in us.” Only after 2009, when California Department of Public Health regulators stepped in, has some movement toward Tooleville’s goal of connecting to Exeter’s water supply been made.
On balance, however, county drinking water regulators have been unable to ameliorate the Valley’s ongoing contamination problems. The SDWA promotes a system-by-system focus and provides few incentives for regulators to support regional solutions. As one county regulator noted, “[Tooleville residents] pay taxes in our county, they pay taxes in our stores, their children go to our school… . It irritates me that [Exeter] won’t help those people.” He went on, however: “[But] I don’t have an opinion; I’m a regulator.” In essence, this regulator can see the need for intercommunity solutions, but the solution is outside his regulatory mandate. Residents in unincorporated places see this problem clearly: “Do you know how long we’ve been knocking on the County’s door? … We’ve been doing this since my dad was a farmworker.”
State and county regulatory failures add to the exposure burden produced by historically poor infrastructure and limited municipal support. In interviews, regulators agreed that, limited by funding and staff time, they were forced to prioritize which drinking water regulations to enforce. Some of this prioritization derives from the SDWA itself. Maximum contaminant level violations of tier-1 contaminants (those that can cause acute or immediate health impacts, such as total coliform or nitrate) are explicitly prioritized over a system’s failure to comply with SDWA’s monitoring requirements. But prioritizing MCL violations over monitoring violations leads to unforeseen exposure risks. In 2007, Fresno County returned primacy for water systems with fewer than 200 connections to state-level regulators because county officials could not adequately implement the SDWA. In interviews, state officials noted that they subsequently found that many of the community water systems had failed to monitor for several years, but had not been given monitoring violations by county regulators. Few MCL violations had been recorded though recent water quality results indicated MCL exceedances. Without water quality data, county regulators had been unable to issue MCL violations, and with no notices of MCL violations, residents had lacked information on whether they faced exposure to harmful levels of contaminants.
Impact of Multilevel Factors and Actors on Coping and Mitigation
If coping and mitigation strategies—at the community or household level—could adequately address drinking water contamination, then vulnerability to exposure, even persistent exposure, could be minimized (Figure 1). However, our fieldwork indicated that inadequate infrastructure; poor technical, managerial, and financial (TMF) capacity at the community level; failures of the regulatory system to provide timely information on near-term coping options; and inadequate funding mechanisms at the state level all undermine the success of coping mechanisms.
The joint role of poor infrastructure and poor TMF capacity in undermining community-level mitigation is best understood through the examples of Alpaugh and Lanare. Alpaugh, located in southwest Tulare County, had exceeded the old arsenic standard of 50 micrograms per liter since the early 2000s,32 and had experienced water outages when its backup wells broke down. In 2005, the water board obtained $4.2 million to rehabilitate its pumping, distribution, and storage system, but it did not include plans to upgrade to the Revised Arsenic Rule of 2006 (10 μg/L). As one newspaper article noted, “officials were just focusing on getting water flowing. Once that was accomplished … they would worry about the arsenic issue.”54(pB5) In the unincorporated community of Lanare, Fresno County, the MCL for arsenic had been exceeded by 2005. In July 2006, after securing money from a Community Block Grant, residents celebrated the installation of a new treatment plant.55 Six months later the plant was closed because the system was not collecting enough revenue to cover expenses. A Grand Jury investigation found that “Because of mismanagement, unacceptable arsenic levels, and the absence of any other water source, the district is in crisis.”56(p4)
The cases of Alpaugh and Lanare could partly be explained by poor TMF capacity, which is particularly problematic in small water systems. One regulator explained that in small communities local residents and volunteers run the water boards: “They live there, they’re residents. They don’t really understand our regulatory requirements.” But regulators also noted how low TMF stems from a community’s low resource base. They described how small, low-asset communities are unable to hire full-time operators that know the ins and outs of drinking water requirements and planning. In the words of the regulator, “Just having good, qualified candidates is difficult. It’s a very small community.”
State funding mechanisms for new water sources or treatment could offer system-level solutions, but, as currently designed, often do not promote timely solutions. Congress revised the 1996 SDWA Amendments to include capacity development programs for small systems,57 but, in California, TMF capacity is still required for water systems to be eligible for state revolving funds.58,59 Similarly, the American Recovery and Reinvestment Act of 2009 set aside approximately $160 million for drinking water infrastructure; it earmarked stimulus money for “high priority” projects that were “shovel ready.”60 In both cases, the funding criteria (TMF capacity and shovel-readiness) define eligibility on the core weaknesses of resource-poor communities. Communities that lack resources lack TMF; without TMF, funding is harder to attain; and without funding, TMF cannot be developed. Water systems that are shovel-ready are likely to be those with the TMF to develop credible plans in the first place. The funding conditions through which exposure could be mitigated are thus conditions through which exposures and social disparities are prolonged.
When system-level coping fails, households assume the burden of mitigation. But a combination of disenfranchised residents, inadequate water system responses, and regulatory failures is yet another pathway toward vulnerability. Interviewees reported that local water boards sometimes discriminate against residents on the basis of language, race/ethnicity, socioeconomic status, or homeownership. In 2010, residents from the community of East Orosi testified to the United Nations Special Rapporteur on the Human Right to Water and Sanitation that, because they speak in English with Spanish accents, they were continually turned away by water board administrators when seeking clarification on their water quality reports.61
Regulatory failures further undermine household-level coping mechanisms. The SDWA focuses on a contaminant-by-contaminant mode of regulation, but has no stipulations on how public notices should explain how residents can address multiple contaminants (e.g., nitrate and total coliform). In 2007, 5% of the Valley’s 677 active community water systems received an MCL violation for both nitrate and total coliform.32 A violation of the total coliform MCL triggers a boil-water order. Yet boiling water can increase concentrations of nitrate. The SDWA does not require that Consumer Confidence Reports explain what to do in such a case. Neither does the SDWA explicitly address how to cope with long-term exposures. A resident from the community of Cutler explained that for years she had received Consumer Confidence Reports indicating that dibromochloropropane levels in the water exceeded the MCL. These reports noted that residents should not worry because health impacts were not based on immediate exposure, but rather on lifetime exposure (Figure C, available as a supplement to the online version of this article at http://www.ajph.org). She had lived in her community for nearly 30 years—so, she asked, should she worry or not?
In these situations, water systems simply leave residents to cope with contaminated drinking water as best they can. As one regulator admitted,
some of [the water systems] aren’t going to have the money to do anything more than tell their customers, “We are trying to figure out how to solve this problem … but if you want to use bottled water or use other means, go ahead.”
In these instances, SDWA regulations ultimately fail the (low-income) household.
Even, the right to know does not translate to the ability to act. Even when households take action to reduce exposure, individual coping mechanisms may not be effective. Households may purchase bottled water, but individuals may not consistently drink it. Households may install water filters, but often incorrectly assume that the filter treats for the contaminant of interest.62 Significant costs are incurred for these partially protective measures. In many low-income Valley communities, households pay 4% to 10% of their monthly income for water,62 including the utility bill and vended water, well above the US Environmental Protection Agency’s affordability criterion of 2.5% of median household income.63 Certainly when a (successful) system-level mitigation strategy (i.e., treatment) is developed, these costs are passed along to the household. But at least under those circumstances there is a higher probability of the end result being water quality of adequate standards.
Case Study of the Struggle for Safe Water in Tooleville
The unincorporated community of Tooleville is an exemplar of the Drinking Water Disparities Framework in action (Figure 2). Located at the eastern edge of Tulare County’s Valley floor, at the foot of the rolling Sierra hills dotted with orange groves and residential enclaves, Tooleville has been a farmworker community since the Dust Bowl days. Today, the roughly 70 households living there are predominantly Latino, with a median annual household income of $16 000 (about a third of that of California). Residents pride themselves on the beauty of their natural surroundings and their high rates of homeownership. Ms Jimenez (pseudonym) remembers the day her father purchased a home in Tooleville: “I was so proud that we owned a house.” She still lives there and is determined to stay in her community, despite the challenges Tooleville faces.
FIGURE 2—
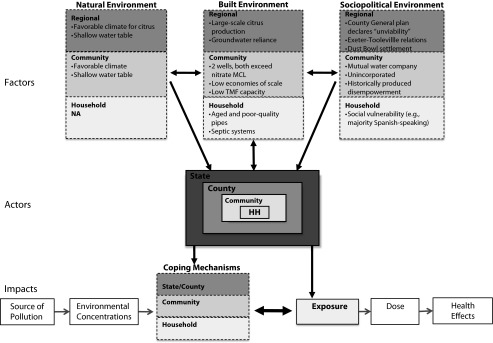
The Drinking Water Disparities Framework applied to the specific case of Tooleville, California.
Note. HH = household; MCL = maximum contaminant level; NA = not applicable; TMF = technical, managerial, and financial. Multilevel environmental factors act through multilevel actors to have an impact on exposure and coping capabilities. Race and class characteristics are embedded in many of the factors and actors throughout.
Like most small communities in the Valley, Tooleville residents rely on groundwater for drinking. From 2005 to 2010, Tooleville’s 2 wells received MCL violations (i.e., exceeding 45 mg NO3/L) for nitrate in 3 different years and had average yearly nitrate levels ranging from 34 to 51 milligrams of nitrate per liter and averaging 40 milligrams of nitrate per liter.33,64–69 At these elevated levels, infants are at risk for methemoglobinemia (blue baby syndrome) and women are at risk for adverse reproductive effects. During this time frame, Tooleville also received 7 MCL violations for exceeding total coliform standards.32,67–69 Residents were advised to boil the water to deal with bacteriological contamination, but boiling further concentrates the nitrates.
Just at the end of Tooleville runs the Friant-Kern Canal, channeling Sierra snowmelt to agriculture. Tooleville does not have legal access to this water source; by and large, farmers hold the water rights. Even if Tooleville held legal rights, the cost of treating surface water would be too high for this small community. Residents are also frustrated that historical planning processes have limited their financial and infrastructure resources. As noted previously, until the 2012 revision of the 1973 Tulare County General Plan, the county’s plan had listed Tooleville as a “nonviable” community from which public resources, including water infrastructure, should be withheld.
Solutions have been hard to come by. Attempts to drill new wells have yielded poor results—the water all around the community is high in nitrates. This has left Tooleville with a persistent compliance and exposure burden, prolonging risks from exposure as well as household coping costs. Even coping mechanisms such as purchasing bottled water are only partially protective. Most residents have drunk the contaminated well water at some point, and still use it for cooking.
Regional solutions have also been hard to achieve. As noted previously, for several years, residents and county officials hoped that Tooleville could consolidate with Exeter, which is less than half a mile away, has more wells, and has lower nitrate levels (ranging from 23 to 28 mg NO3/L and averaging 25 mg NO3/L; Figure B, available as a supplement to the online version of this article at http://www.ajph.org).33 Consolidation would bring a pipeline to Tooleville with some of Exeter’s water. But the city has expanded its spheres of influence in other directions. In the meantime, residents continue to rely on their contaminated wells and pay twice for water—once for their utility bill, and once for bottled or vended water.
With the framework in mind, we can return to the 3 questions at the beginning of this article. First, Tooleville shows that, although small size does make a system physically vulnerable (e.g., relying only on 1 or 2 wells), a range of political actors and sociohistorical factors also determines exposure and coping capacity. Second, cases like Tooleville underscore the complexity of isolating “the cause” of drinking water pollution. Third, the composite burden—of exposure and coping costs—can create place-specific environmental injustices regardless of whether region-wide statistics show a “significant” association between poor water quality and community demographics. Thus, intentional environmental harm is not necessary, and low economies of scale are not sufficient, to explain why many small community systems in the Valley continue to serve contaminated drinking water.
CONCLUSIONS
The Drinking Water Disparities Framework traces the development of a composite burden that comprises the exposure and coping costs that many water systems and households face. It uncovers the broad processes that have an impact on access to safe water, and it can also be tailored to specific contexts such as Tooleville. The framework argues, and the Tooleville case confirms, that there is no direct causal path between race and class and disproportionate burdens; rather, race and class are imbricated in almost all the factors and actors that have historically combined, and still combine, to produce this composite burden.
Building on social epidemiology approaches, and using empirical data from the Valley, the framework makes central the interactions between environmental factors (sociopolitical, natural, and built) and their multiple levels of operation. It shows how decisions of multiple actors made at every level, intentionally or by default, prolong exposure and impede households’ coping capabilities. The framework reveals how, alongside a baseline of contaminated source water, a series of planning policies have constrained access to physical and financial resources. These decisions, in conjunction with regulatory failures, a lack of community resources to mitigate contamination, and political disenfranchisement of local residents, help explain the origins of environmental injustice in the context of drinking water. These same forces also influence coping capacities, which may lead only to partial protection that, in turn, exacerbates the impacts of drinking water contamination.
A multipronged research and intervention agenda is needed to reduce and mitigate the drinking water disparities highlighted in this article because race and class are embedded within multiple individual “causes.” Methodologically and theoretically, this framework provides the impetus for environmental justice and social epidemiology–oriented research to focus on a broader set of outcomes, such as coping costs or multiple contaminants, in addition to exposure disparities. It reminds public health practitioners and policymakers to look beyond proximate causes and include historical and structural factors in the analysis of exposure disparities. As new contexts and evidence are analyzed, additional factors and pathways may emerge and be added to refine the framework.
From a policy perspective, the framework identifies multiple potential intervention points.23 Numerous policies have attempted to address drinking water contamination and small water systems challenges, including American Economic Recovery Act monies and State Drinking Water Revolving Funds. But unless future incarnations of these policies take seriously the disparity-producing mechanisms highlighted in this article, these policies are unlikely to improve drinking water conditions in the most disadvantaged communities. Although new efforts to support small communities are under way (e.g., Emergency Funding and Small Water System Program Plan), we show that a concerted focus on improving TMF capacity in disadvantaged communities is critical. We argue that funding mechanisms should not always use TMF capacity as a requirement, but should find ways to support it, or enhance other sustainable solutions. For instance, rather than prioritizing “shovel-ready” projects, we suggest that funds should be made available for “planning-ready” systems. These funds would help small or disadvantaged systems to develop their engineering and financial plans for contaminant mitigation and infrastructure needs.
Likewise, the promotion of water system consolidation—be it physical connection of a small system to a larger one or sharing of management capacities—must acknowledge the underlying political and social barriers noted in this article. Water policy experts often say that smaller systems fear losing local autonomy and therefore stall or block consolidation efforts. But our work argues that a deeper and long-standing set of social, economic, and political processes also creates barriers. Local politics can compromise consolidation efforts; thus, consolidation may be more successful if it is not left to isolated cities and communities but is facilitated by a regional drinking water development program (for an example from New Mexico see Sturgeon70). We recognize that this may require abdication of some municipal authority, something many cities are loath to surrender.
Finally, future amendments to the SDWA are needed on 3 fronts. First, the ability of water systems to comply with monitoring and reporting violations should be given particular priority. Second, drinking water regulations should clearly address the co-occurrence of contaminants, and how to adequately inform residents about long-term protective measures. And third, regional or cross-system solutions will be necessary—system-by-system monitoring and contaminant-by-contaminant remediation cannot alleviate the composite burden of drinking water vulnerability in low-income communities.
In sum, the Drinking Water Disparities Framework uncovers the multilayered, historical, and ongoing structures and processes that explain the origins and persistence of contaminated drinking water and its relation to social disparities. It shows that solutions—whether at the household, community, or county level—must address the vulnerability of residents, the role of political influence, the need to strengthen coping capacities, and a need for regional interventions, as opposed to the more prevalent community-by-community, contaminant-by-contaminant fixes.
Acknowledgments
This research was supported by the National Science Foundation Graduate Research Fellowship, the California Endowment (through a collaborative grant between Community Water Center and University of California, Berkeley), the California Environmental Protection Agency (07-020), and the Switzer Environmental Fellowship.
We thank Rachel Morello-Frosch, PhD, and Gene Rochlin, PhD, for valuable insights on an earlier draft of this article; Laurel Firestone, Susana deAnda Maria Herrera (of Community Water Center), Rich Haberman and Dave Spath (formerly of California Department of Public Health), the Energy and Resources Group’s Water Group, Morello-Frosch lab group, and Bhavna Shamasunder for support and feedback on analysis; David Guendelman for conceptual insights; and California Department of Public Health and Tulare County Environmental Health Services for water quality data. We are grateful to the anonymous reviewers of this article.
Human Participant Protection
This study was approved by the University of California’s institutional review board.
References
- 1.Dubrovsky NM, Burow KR, Clark GM . Menlo Park, CA: US Geological Survey; 2010. The quality of our nation’s waters—nutrients in the nation’s streams and groundwater, 1992–2004. [Google Scholar]
- 2.Olmstead SM. Thirsty colonias: rate regulation and the provision of water service. Land Econ. 2004;80(1):136–150. [Google Scholar]
- 3.Heaney C, Wilson SM, Wilson O, Cooper J, Bumpass N, Snipes M. Use of community-owned and -managed research to assess the vulnerability of water and sewer services in marginalized and underserved environmental justice communities. J Environ Health. 2011;74(1):8–17. [PubMed] [Google Scholar]
- 4.Wilson SM, Heaney CD, Cooper J, Wilson O. Built environment issues in unserved and underserved African-American neighborhoods in North Carolina. Environ Justice. 2008;1(2):63–72. [Google Scholar]
- 5. Murphy M, Lewis L, Sabogal RI, Bell C. Survey of unregulated drinking water sources on Navajo nation. Oral presentation at: American Public Health Association 137th Annual Meeting and Exposition; November 10, 2009; Philadelphia, PA.
- 6.Balazs C, Morello-Frosch R, Hubbard A, Ray I. Social disparities in nitrate contaminated drinking water in the San Joaquin Valley. Environ Health Perspect. 2011;119(9):1272–1278. doi: 10.1289/ehp.1002878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Balazs CL, Morello-Frosch R, Hubbard A, Ray I. Environmental justice implications of arsenic contamination in California’s San Joaquin Valley: a cross-sectional, cluster design examining exposure and compliance in community drinking water systems. Environ Health. 2012;11:84. doi: 10.1186/1476-069X-11-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pulido L. A critical review of the methodology of environmental racism research. Antipode. 1996;28(2):142–159. [Google Scholar]
- 9.Pulido L, Sidawi S, Vos R. An archaeology of environmental racism in Los Angeles. Urban Geogr. 1996;17(5):419–439. [Google Scholar]
- 10.Wilson SM, Heaney CD, Wilson O. Governance structures and the lack of basic amenities: can community engagement be effectively used to address environmental injustice in underserved Black communities? Environ Justice. 2010;3(4):125–133. [Google Scholar]
- 11.VanDerslice J. Drinking water infrastructure and environmental disparities: evidence and methodological considerations. Am J Public Health. 2011;101(suppl 1):S109–S114. doi: 10.2105/AJPH.2011.300189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Committee on Small Water Systems. Safe Water From Every Tap. Improving Water Service to Small Communities. Washington, DC: National Research Council; 1997. [Google Scholar]
- 13.Washington, DC: US General Accounting Office; 1990. Drinking water: compliance problems undermine EPA program as new challenges emerge. GAO/RCED-90-127. [Google Scholar]
- 14.Washington, DC: US General Accounting Office; 2011. Unreliable state data limit EPA’s ability to target enforcement priorities and communicate water systems’ preferences. GAO-11-381. [Google Scholar]
- 15.Cory DC, Rahman T. Environmental justice and enforcement of the safe drinking water act: the Arizona arsenic experience. Ecol Econ. 2009;68:1825–1837. [Google Scholar]
- 16.Guerrero-Preston R, Norat J, Rodriguez M, Santiago L, Suarez E. Determinants of compliance with drinking water standards in rural Puerto Rico between 1996 and 2000: a multilevel approach. P R Health Sci J. 2008;27(3):229–235. [PubMed] [Google Scholar]
- 17.Rahman T, Kohli M, Megdal S, Aradhyula S, Moxley J. Determinants of environmental noncompliance by public water systems. Contemp Econ Policy. 2010;28(2):264–274. [Google Scholar]
- 18.Imperial MT. Environmental justice and water pollution control: The Clean Water Act Construction Grants Program. Public Works Manage Policy. 1999;4(2):110–118. [Google Scholar]
- 19.Francis R, Firestone L. Implementing the human right to water in California’s Central Valley: building a democratic voice through community engagement in water policy decision making. Willamette Law Rev. 2011;47:495–537. [Google Scholar]
- 20.Marsh B, Parnell AM, Moss Joyner A. Institutionalization of racial inequality in local political geographies. Urban Geogr. 2010;31(5):691–709. [Google Scholar]
- 21.Troesken W. The limits of Jim Crow: race and the provision of water and sewerage services in American cities, 1880–1925. J Econ Hist. 2002;62(3):734–772. [Google Scholar]
- 22.Krieger N. Theories for social epidemiology in the 21st century: an ecosocial perspective. Int J Epidemiol. 2001;30(4):668–677. doi: 10.1093/ije/30.4.668. [DOI] [PubMed] [Google Scholar]
- 23.Susser M, Susser E. Choosing a future for epidemiology: from black box to Chinese boxes and eco-epidemiology. Am J Public Health. 1996;86(5):674–677. doi: 10.2105/ajph.86.5.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Krieger N. Methods for the scientific study of discrimination and health: an ecosocial approach. Am J Public Health. 2012;102(5):936–944. doi: 10.2105/AJPH.2011.300544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Soobader M, Cubbin C, Gee GC, Rosenbaum A, Laurenson J. Levels of analysis for the study of environmental health disparities. Environ Res. 2006;102(2):172–180. doi: 10.1016/j.envres.2006.05.001. [DOI] [PubMed] [Google Scholar]
- 26.Sexton K, Olden K, Johnson BL. “Environmental justice”: the central role of research is establishing a credible scientific foundation for informed decision making. Toxicol Ind Health. 1993;9(5):685–695. doi: 10.1177/074823379300900504. [DOI] [PubMed] [Google Scholar]
- 27.Gee GC, Payne-Sturges DC. Environmental health disparities: a framework integrating psychosocial and environmental concepts. Environ Health Perspect. 2004;112(17):1645–1653. doi: 10.1289/ehp.7074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.deFur PL, Evans GW, Cohen Hubal EA, Kyle AD, Morello-Frosch R, Williams DR. Vulnerability as a function of individual and groups resources in cumulative risk asssessment. Environ Health Perspect. 2007;115(5):817–824. doi: 10.1289/ehp.9332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lioy PJ. Assessing total human exposure to contaminants. Environ Sci Technol. 1990;24(7):938–945. [Google Scholar]
- 30.Wilson S. An ecological framework to study and address environmental justice and community health issues. Environ Justice. 2009;2(1):15–23. [Google Scholar]
- 31.Washington, DC: National Environmental Justice Advisory Committee; 2004. Ensuring risk reduction in communities with multiple stressors: environmental justice and cumulative risks/impacts. [Google Scholar]
- 32.Sacramento, CA: California Department of Public Health; 2008. Permits Inspections Compliance Monitoring and Enforcement (PICME) [Google Scholar]
- 33.Water Quality Monitoring. Sacramento, CA: California Department of Public Health, Division of Drinking Water and Environmental Management; 2008. [Google Scholar]
- 34.Roof K, Oleru N. Public health: Seattle and King County’s push for the built environment. J Environ Health. 2008;71(1):24–27. [PubMed] [Google Scholar]
- 35.Washington, DC: US Environmental Protection Agency; 2010. Public drinking water systems: facts and figures. [Google Scholar]
- 36.Bates MN, Smith AH, Cantor KP. Case–control study of bladder cancer and arsenic in drinking water. Am J Epidemiol. 1995;141(6):523–530. doi: 10.1093/oxfordjournals.aje.a117467. [DOI] [PubMed] [Google Scholar]
- 37.Smith AH, Hopenhayn-Rich C, Bates MN et al. Cancer risks from arsenic in drinking water. Environ Health Perspect. 1992;97:259–267. doi: 10.1289/ehp.9297259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Steinmaus C, Yuan Y, Bates MN, Smith AH. Case–control study of bladder cancer and drinking water arsenic in the western United States. Am J Epidemiol. 2003;158(12):1193–1201. doi: 10.1093/aje/kwg281. [DOI] [PubMed] [Google Scholar]
- 39.Chiu HF, Tsai SS, Yang CY. Nitrate in drinking water and risk of death from bladder cancer: an ecological case–control study in Taiwan. J Toxicol Environ Health A. 2007;70(12):1000–1004. doi: 10.1080/15287390601171801. [DOI] [PubMed] [Google Scholar]
- 40.De Roos A, Ward M, Lynch C, Cantor K. Nitrate in public water systems and the risk of colon and rectum cancers. Epidemiology. 2003;14:640–649. doi: 10.1097/01.ede.0000091605.01334.d3. [DOI] [PubMed] [Google Scholar]
- 41.Fan AM, Steinberg VE. Health implications of nitrate and nitrite in drinking water: an update of methemoglobinemia occurrence and reproductive and developmental toxicity. Regul Toxicol Pharmacol. 1996;23(1 pt 1):35–43. doi: 10.1006/rtph.1996.0006. [DOI] [PubMed] [Google Scholar]
- 42.Fan AM, Willhite CC, Book SA. Evaluation of the nitrate drinking water standard with reference to infant methemoglobinemia and potential reproductive toxicity. Regul Toxicol Pharmacol. 1987;7(2):135–148. doi: 10.1016/0273-2300(87)90024-9. [DOI] [PubMed] [Google Scholar]
- 43.Morello-Frosch R, Zuk M, Jerrett M, Shamasunder B, Kyle A. Synthesizing the science on cumulative impacts and environmental health inequalities: implications for research and policy-making. Health Aff (Millwood) 2011;30(5):879–887. doi: 10.1377/hlthaff.2011.0153. [DOI] [PubMed] [Google Scholar]
- 44.Nash LL. Inescapable Ecologies: A History of Environment, Disease, and Knowledge. Berkeley, CA: University of California Press; 2006. [Google Scholar]
- 45.Dubrovsky NM, Kratzer CR, Brown LR, Gronberg JM, Burow KR. Water quality in the San Joaquin–Tulare Basins, California, 1992–95. Denver, CO: US Geological Survey; 1998. [Google Scholar]
- 46.Galloway D, Riley FS. Land Subsidence in the United States. Menlo Park, CA: US Geological Survey; 2006. San Joaquin Valley, California: largest human alteration of the Earth’s surface. Circular 1182. [Google Scholar]
- 47.Gao S, Tanji KK, Banueos GS. Processes and conditions affecting elevated arsenic concentrations in groundwaters of Tulare Basin, California, USA. In: Bhattacharya P, Mukherjee AB, Bundschuh J, Zevenhoven R, Loeppert RH, editors. Trace Metals and Other Contaminants in the Environment. Amsterdam, The Netherlands: Elsevier BV; 2007. pp. 383–410. [Google Scholar]
- 48.Welch AH, Westjohn DB, Helsel DR, Wanty RB. Arsenic in ground water of the United States: occurrence and geochemistry. Ground Water. 2000;38(4):589–604. [Google Scholar]
- 49.Reisner M. Cadillac Desert: The American West and Its Disappearing Water. New York, NY: Viking; 1986. [Google Scholar]
- 50.Viers JH, Liptzin D, Rosenstock TS . Davis, CA: Center for Watershed Sciences, University of California, Davis; 2012. Technical report 2: addressing nitrate in California’s drinking water with a focus on Tulare Lake Basin and Salinas Valley groundwater. Report for the State Water Resources Control Board to the Legislature. [Google Scholar]
- 51.Harter TJ, Lund JR, Darby GE . Davis, CA: University of California, Davis; 2012. Addressing nitrate in California’s drinking water with a focus on Tulare Lake Basin and Salinas Valley groundwater: report for the State Water Resources Control Board Report to the Legislature. [Google Scholar]
- 52.Visalia, CA: Tulare County Planning Department; 1973. County of Tulare general plan: water and liquid waste management, policies, programs; pp. 1–6. [Google Scholar]
- 53. Cal Senate Bill X2 9 §20209.7 (2009)
- 54.Boyles D. The Fresno Bee. June 3, 2005. Alpaugh water system work starts. Local News:B5. [Google Scholar]
- 55.Nolen E.Lanare treatment plant dedicated Twin City Times.April 18, 2007News:1 [Google Scholar]
- 56.Fresno, CA: Fresno Superior Court; 2008. Fresno County Grand Jury. Fresno County Grand Jury 2007–2008 final report; pp. 1–11. [Google Scholar]
- 57.Shanaghan P, Bielanski J. Achieving the capacity to comply. In: Pontius F, editor. Drinking Water Regulation and Health. New York, NY: John Wiley and Sons; 2003. pp. 449–462. [Google Scholar]
- 58.Sacramento, CA: California Department of Public Health; 2009. American Recovery and Reinvestment Act (ARRA) CDPH FINAL criteria Safe Drinking Water State Revolving Fund projects. [Google Scholar]
- 59.Sacramento, CA: California Department of Public Health; 2009. ARRA funding for public drinking water systems: funding criteria. [Google Scholar]
- 60.Sacramento, CA: California Environmental Protection Agency; 2010. Financial assistance programs—grants and loans clean water state revolving fund program. [Google Scholar]
- 61.United Nations General Assembly, UN Human Rights Council. Report of the Special Rapporteur on the human right to safe drinking water and sanitation. 2011 Available at: http://www2.ohchr.org/english/bodies/hrcouncil/docs/18session/A-HRC-18-33-Add4_en.pdf. Accessed December 3, 2013. [Google Scholar]
- 62.Moore E, Matalon E, Balazs C . The Human Costs of Nitrate-Contaminated Drinking Water in the San Joaquin Valley. Oakland, CA: Pacific Institute; 2011. [Google Scholar]
- 63.Washington, DC: US Environmental Protection Agency; 2003. Recommendations of the National Drinking Water Advisory Council to US EPA on its national small systems affordability criteria. [Google Scholar]
- 64.Annual Compliance Report. Sacramento, CA: California Department of Public Health, Division of Drinking Water and Environmental Management; 2005. [Google Scholar]
- 65.Annual Compliance Report. Sacramento, CA: California Department of Public Health, Division of Drinking Water and Environmental Management; 2006. [Google Scholar]
- 66.Annual Compliance Report. Sacramento, CA: California Department of Public Health, Division of Drinking Water and Environmental Management; 2007. [Google Scholar]
- 67.Annual Compliance Report. Sacramento, CA: California Department of Public Health, Division of Drinking Water and Environmental Management; 2008. [Google Scholar]
- 68.Annual Compliance Report. Sacramento, CA: California Department of Public Health, Division of Drinking Water and Environmental Management; 2009. [Google Scholar]
- 69.Annual Compliance Report. Sacramento, CA: California Department of Public Health, Division of Drinking Water and Environmental Management; 2010. [Google Scholar]
- 70.Sturgeon B. Lighting the Path to Secure, Safe and Affordable Water for All. Merced, CA: University of California, Merced; 2010. Distributive systems and multiple community water board collaboration: models that work and how to fund them. [Google Scholar]


