Abstract
Objective
Studies of extubation in preterm infants often define extubation success as a lack of reintubation within a specified time window. However, the duration of observation that defines extubation success in preterm infants has not been validated. The purpose of this study was to systematically review published definitions of extubation success in very preterm infants and to analyze the effect of the definition of extubation success on the reported rates of reintubation.
Design
Studies including very preterm infants published between 1/1/02 and 6/30/12 that reported reintubation as an outcome were reviewed for definitions of extubation success. Stepwise multivariable linear regression was used to explore variables associated with rate of reintubation.
Results
Two independent reviewers performed the search with excellent agreement (κ=0.93). Of the 44 eligible studies, 31 defined a window of observation that ranged from 12-168 hours (7 days). Extubation and reintubation criteria were highly variable. The mean±SD reintubation rate across all studies was 25±9%. In studies of infants with median birth weight (BW) ≤1000g, reintubation rates steadily increased as the window of observation increased, without apparent plateau (p=.001). This trend was not observed in studies of larger infants (p=.85).
Conclusion
Variability in the reported definitions of extubation success makes it difficult to compare extubation strategies across studies. The appropriate window of observation following extubation may depend on the population. In infants with BW≤1000g, even a week of observation may fail to identify some who will require reintubation.
MeSH: Bronchopulmonary dysplasia, Respiratory Distress Syndrome, Artificial Respiration, Airway Extubation, Intratracheal Intubation
INTRODUCTION
Respiratory failure requiring intubation and mechanical ventilation is common in preterm infants. Nearly two thirds of those born at less than 29 weeks gestation will require mechanical ventilation for some duration during the newborn period.[1] Prolonged mechanical ventilation and the subsequent development of bronchopulmonary dysplasia are associated with adverse neurodevelopmental and respiratory outcomes.[2-11] Interventions that minimize exposure to mechanical ventilation and result in successful extubation may therefore provide long-term benefit in preterm infants.
Successful extubation is often defined as not requiring reintubation during a pre-specified window of observation. The duration of extubation that defines success has not been validated in preterm infants, however. While shorter windows may help differentiate failed extubation from reintubation due to other causes, use of non-invasive respiratory support may delay but not prevent reintubation in some infants. Windows of observation that are too short may fail to detect a substantial number of extubation failures and result in inflated estimates of the effectiveness of interventions intended to facilitate extubation.
We summarized published definitions of extubation success in very premature infants and assessed the validity of several definitions by comparing the reported success rate with the duration of the observation window used to define extubation success. We hypothesized that reported reintubation rates would be significantly associated with the duration of observation following extubation.
METHODS
Study Design and Data Extraction
This review was performed using a written protocol. We identified English language studies in PubMed published between 1/1/02 and 6/30/12 containing the terms “extubation” or “intubation” and “preterm” or “premature.” The search was intentionally broad as many types of studies including those of extubation criteria, ventilator management, and medications report reintubation as an outcome. The specific search terms were: (extubation OR intubation) AND (preterm OR premature) AND neonate AND (“2002”[Date - Publication] : “2012/06/30”[Date - Publication]) AND English[Language] NOT “comment”[Publication Type] NOT “editorial”[Publication Type] NOT “review”[Publication Type] NOT “case reports”[Publication Type] NOT “meta analysis”[Publication Type].
Included studies met the following eligibility criteria: (1) subjects included very preterm (<32 weeks gestation) or very low birth weight (<1500g) infants; (2) reintubation was reported as an outcome; (3) intubation was not for anesthesia; (4) study was not a case report, editorial, or review article.
All abstracts were screened independently by two investigators (AG, EJ) for eligibility criteria and need for full-text review. Disagreements were resolved by an independent third party (Sara DeMauro). Data were independently extracted by each investigator onto standardized forms. Any discrepancies were resolved by consensus.
All data were analyzed as reported in the published articles except median birth weight (BW) and reintubation rate, which were often reported only for subgroups. In our analysis, the median subject birth weight was estimated by calculating a weighted average of the subgroups if no summary measure was reported. The overall reintubation rate was calculated directly from the raw data in every case and did not require estimation. If reintubation rates for multiple observation windows were reported, only those from the observation period defined in the methods as the primary outcome were used in the analysis.
Statistical Analysis
Descriptive analysis was planned for most variables. Reported reintubation rates followed a normal distribution, allowing for the use of stepwise multivariable linear regression to explore study characteristics associated with higher rates of reintubation. The duration of post-extubation observation and median study birth weight were a priori selected for evaluation. Studies could not be compared by median subject gestational age because some studies reported the average subject gestational age in whole completed weeks and others reported partial weeks. All regression models were weighted on study sample size. Significance was measured at the α=0.05 level. Analyses were performed with STATA/IC 12.1.
RESULTS
Our PubMed search yielded 394 abstracts. Eighty-six full text articles were reviewed, of which 44 studies were included in this review (Figure 1). A complete list of included studies can be found in Appendix A (web only). Initial inter-rater agreement for study selection was high (κ=0.93). Characteristics of the included studies are shown in Table 1. Most were small and single center, however 77% were prospective, with 50% clinical trials (experimental design) and 27% observational studies.
Figure 1.
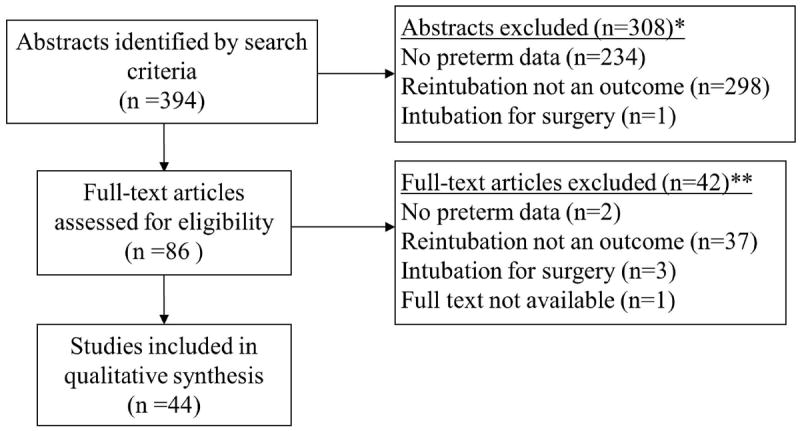
Flow diagram of included and excluded studies.
*84 studies did not meet 1 inclusion, 223 studies did not meet 2 inclusions, and 1 study did not meet 3 inclusions.
**41 studies did not meet 1 inclusion and 1 study did not meet 2 inclusions.
Table 1.
Study Characteristics
| Median [IQR] | |
|---|---|
| Number of participants enrolled | 59 [40-138] |
| Number (%) | |
| Median birthweight <1000g* | 21 (47.7) |
| Single center | 37 (84.1) |
| Region | |
| International | 1 (2.3) |
| United States | 10 (22.7) |
| Canada | 3 (6.8) |
| Central/South America | 2 (4.6) |
| Europe | 12 (27.3) |
| United Kingdom | 8 (18.2) |
| Australia/New Zealand | 4 (9.1) |
| Asia | 3 (6.8) |
| Africa | 1 (2.3) |
| Study design | |
| Clinical trial | 22 (50) |
| Prospective observational | 12 (27.3) |
| Retrospective | 10 (22.7) |
Estimated by calculating a weighted average of subgroups
Only 31 studies (71%) reported the duration of observation used to define extubation success. The windows ranged from 12-168 hours with 48, 72, and 168 hours (7 days) used most frequently (Table 2). The methodological rigor of the studies varied as well; 56% and 63% of the clinical trials (n=22) reported strict extubation and reintubation criteria, respectively. The specific criteria for extubation and reintubation are summarized in Table 3. Positive inspiratory pressure (PIP), fraction of inspired oxygen (FiO2), and mechanical ventilation rate were the most common extubation criteria, albeit with a wide range in values across the studies. The maximum PIP allowed for extubation ranged from 12-20 cm H20 and for FiO2 ranged from 0.25-0.40. Apnea, FiO2, and the development of respiratory acidosis were the most commonly cited reintubation criteria. The cutoff values for these criteria also ranged widely. The type of post-extubation support was described in 29 (66%) studies. Of these, 22 (76%) used positive pressure airway support after extubation (greater than 2L/min nasal cannula).
Table 2.
Duration of Observation Window (if specified)
| Observation window (n=31) | N (%) |
|---|---|
| 12 hours | 1 (3.2) |
| 24 hours | 2 (6.4) |
| 48 hours | 9 (29) |
| 72 hours | 11 (35.5) |
| 168 hours | 8 (25.8) |
Table 3.
Extubation and Reintubation Criteria (if specified)
| Extubation criteria (n=21) | No. (%) | Median cutoff (range) |
|---|---|---|
| FiO2 | 16 (76.2) | 35 (25-40) |
| PIP | 15 (71.4) | 16 (12-20)* |
| Ventilator rate | 15 (71.4) | 20 (12-35) |
| PEEP | 4 (19) | 4 (3-5) * |
| Mean airway pressure | 4 (19) | 8.5 (5-10) * |
| Amplitude | 2 (9.5) | 20* |
| Frequency | 1 (4.8) | 9 Hz |
| pH | 3 (14.3) | 7.25 |
| PaO2 | 1 (4.8) | 50† |
| PaCO2 | 5 (23.8) | 60 (45-65)† |
| Hemoglobin | 1 (4.8) | 13 g/dL |
| Minute ventilation test | 2 (9.5) | Pass |
| Spontaneous breathing trial | 1 (4.8) | Pass |
| Reintubation criteria (n=25) | ||
| Apnea | 23 (92) | |
| FiO2 | 20 (80) | 60 (40-100) |
| pH | 22 (88) | 7.25 (7.2-7.25) |
| PaO2 | 9 (36) | 50† |
| PaCO2 | 19 (76) | 65 (55-65)† |
| Respiratory distress‡ | 3 (12) |
FiO2: fraction of inspired oxygen; PIP: positive inspiratory pressure; PEEP: positive end-expiratory pressure; PaO2: partial pressure of oxygen; PaCO2: partial pressure of CO2
cm H20;
mmHg;
Included stridor, tachypnea, Downe’s score, Silverman’s score, “severe distress”
The mean±SD reintubation rate across all studies was 25±9%. In the multivariable linear regression analysis median subject birth weight ≤1000g was found to be an effect modifier (p=0.03) of the association between duration of post-extubation observation and rate of reintubation; therefore we stratified our analysis on this variable. We found that in studies of infants with median birth weight ≤1000g, the reintubation rate increased significantly with longer duration of observation (p=.001). This relationship was not observed in studies of larger infants >1000g, (p=0.85) (Figure 2).
Figure 2.
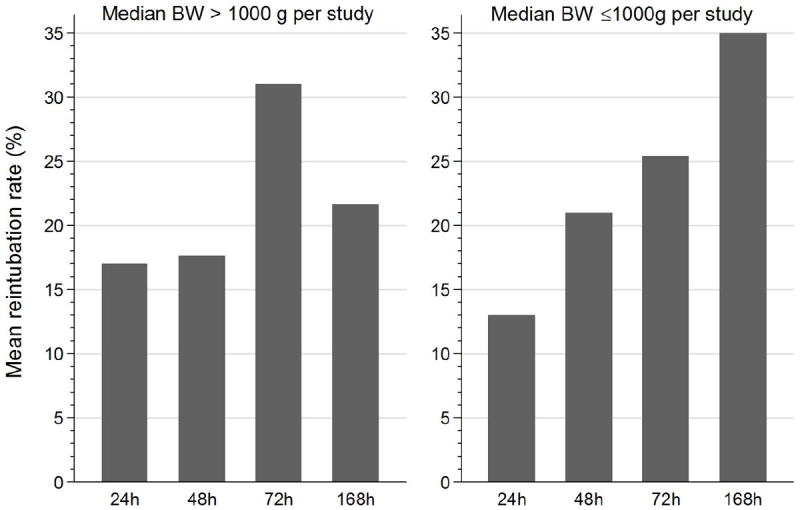
Reintubation rate by time window.
Of the 31 studies that defined extubation success, only 6 (19.3%) provided rates of reintubation after the specified observation window. Five of these reported reintubation rates at 7 days in addition to a shorter window (48-72 hours) and one also reported reintubation at 14 days. The remaining study reported the number of infants reintubated after the observation window but did not report the timing of reintubation.
DISCUSSION
To our knowledge, this is the first systematic review of the outcome of extubation success in premature infants. We reviewed 44 studies published within the last 10 years using reintubation as an outcome. We found a large degree of heterogeneity in the duration of the observation window used to define extubation success, ranging from 12 hours to seven days. In addition, we found that in studies predominately enrolling infants with birth weight less than 1000g, rates of extubation success were negatively associated with the duration of observation. By relying on shorter windows of observation, studies enrolling a large proportion of small infants may therefore underestimate the true rate of reintubation. In fact, the reintubation rate did not appear to plateau even at a week of observation, indicating that longer periods may be necessary to adequately capture this outcome in extremely low birth weight (ELBW) infants.
Methodologic rigor varied across studies of extubation success. Many of the reviewed clinical trials lacked specific extubation and reintubation criteria, and when present there was considerable variability in the cutoffs used to meet each criterion. This was particularly true of extubation criteria, implying that infants enrolled in clinical trials of extubation are extubated from a wide range of respiratory support. This makes it difficult to compare results across studies or pool data for meta-analysis.
This review presents a novel approach for comparing studies of extubation in premature infants. Previous reviews have compared studies solely by intervention and not by outcome. In multiple Cochrane reviews on this topic, results of studies using different definitions of extubation success were pooled together for meta-analysis.[12-21] The heterogeneity in the duration of observation after extubation was not raised as a limitation in pooling the data. Our findings suggest that the duration of the observation window may be important when interpreting the results of these studies and challenges the assumption that these data can be pooled.
The main limitation of this review is the possibility of missing data due to reliance on published reports. Published trials often lack key methodological information.[22] For example, 7 (17.9%) of the 39 studies that reported reintubation rates in the results section did not specify the duration of observation following extubation. There is a possibility that the window was defined but not described in the published report. Unfortunately, the small number of eligible studies and variability of reported extubation and reintubation criteria prevented evaluation of other factors potentially associated with reintubation rate. Individual patient level data may have allowed for a more robust analysis of the effect of birth weight and other factors on reintubation rate within each time window.
This study provides cause for concern regarding the validity and generalizability of respiratory studies using extubation success as a key outcome. The heterogeneity in the definition of this outcome makes comparing the effectiveness of different respiratory strategies difficult. Since an observation window of a week may not adequately capture all small infants requiring reintubation, the current literature may provide an overly optimistic estimate of the likelihood of success of extubation in the smallest babies. Decreasing heterogeneity in the methodology of clinical trials is crucial for the evaluation of therapies in neonatal medicine. This will allow for more robust pooling of data and faster identification of promising strategies for study in large, multi-center trials. Studies of extubation success should consider including a cumulative distribution curve of extubation failure rate over time to help readers better understand the effect of an intervention on the likelihood of reintubation. Such data are urgently needed to better describe the rate and timing of extubation failure and to facilitate the development of a valid definition of extubation success.
WHAT IS KNOWN ABOUT THIS TOPIC
In clinical trials, successful extubation is typically defined as not requiring reintubation during a specified period of observation.
No definition for extubation success has been validated in premature infants.
WHAT THIS STUDY ADDS
Definitions of success in studies of extubation in very premature infants vary widely.
The duration of observation may affect the rate of reintubation in extremely low birth weight infants.
Acknowledgments
We gratefully acknowledge the assistance of Rui Feng, PhD, for her statistical advice, and the help of Sara DeMauro, MD, for acting as a third reviewer.
References
- 1.Stoll BJ, Hansen NI, Bell EF, et al. Neonatal outcomes of extremely preterm infants from the NICHD Neonatal Research Network. Pediatrics. 2010;126(3):443–56. doi: 10.1542/peds.2009-2959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Avery ME, Tooley WH, Keller JB, et al. Is chronic lung disease in low birth weight infants preventable? A survey of eight centers. Pediatrics. 1987;79(1):26–30. [PubMed] [Google Scholar]
- 3.Jobe AH, Hillman N, Polglase G, Kramer BW, Kallapur S, Pillow J. Injury and inflammation from resuscitation of the preterm infant. Neonatology. 2008;94(3):190–6. doi: 10.1159/000143721. [DOI] [PubMed] [Google Scholar]
- 4.Van Marter LJ, Allred EN, Pagano M, et al. Do clinical markers of barotrauma and oxygen toxicity explain interhospital variation in rates of chronic lung disease? The Neonatology Committee for the Developmental Network. Pediatrics. 2000;105(6):1194–201. doi: 10.1542/peds.105.6.1194. [DOI] [PubMed] [Google Scholar]
- 5.Smith VC, Zupancic JA, McCormick MC, et al. Rehospitalization in the first year of life among infants with bronchopulmonary dysplasia. J Pediatr. 2004;144(6):799–803. doi: 10.1016/j.jpeds.2004.03.026. [DOI] [PubMed] [Google Scholar]
- 6.Jeng SF, Hsu CH, Tsao PN, et al. Bronchopulmonary dysplasia predicts adverse developmental and clinical outcomes in very-low-birthweight infants. Dev Med Child Neurol. 2008;50(1):51–7. doi: 10.1111/j.1469-8749.2007.02011.x. [DOI] [PubMed] [Google Scholar]
- 7.Majaesic CM, Jones R, Dinu IA, Montgomery MD, Sauve RS, Robertson CM. Clinical correlations and pulmonary function at 8 years of age after severe neonatal respiratory failure. Pediatr Pulmonol. 2007;42(9):829–37. doi: 10.1002/ppul.20663. [DOI] [PubMed] [Google Scholar]
- 8.Palta M, Sadek-Badawi M, Sheehy M, et al. Respiratory symptoms at age 8 years in a cohort of very low birth weight children. Am J Epidemiol. 2001;154(6):521–9. doi: 10.1093/aje/154.6.521. [DOI] [PubMed] [Google Scholar]
- 9.Kobaly K, Schluchter M, Minich N, et al. Outcomes of Extremely Low Birth Weight (<1 kg) and Extremely Low Gestational Age (<28 Weeks) Infants With Bronchopulmonary Dysplasia: Effects of Practice Changes in 2000 to 2003. Pediatrics. 2008;121(1):73–81. doi: 10.1542/peds.2007-1444. [DOI] [PubMed] [Google Scholar]
- 10.Vohr BR, Wright LL, Poole WK, McDonald SA for the NICHD Neonatal Research Network Follow-up Study. Neurodevelopmental Outcomes of Extremely Low Birth Weight Infants <32 Weeks’ Gestation Between 1993 and 1998. Pediatrics. 2005;116(3):635–43. doi: 10.1542/peds.2004-2247. [DOI] [PubMed] [Google Scholar]
- 11.Schmidt B, Asztalos EV, Roberts RS, et al. Impact of bronchopulmonary dysplasia, brain injury, and severe retinopathy on the outcome of extremely low-birth-weight infants at 18 months: results from the trial of indomethacin prophylaxis in preterms. JAMA. 2003;289(9):1124–9. doi: 10.1001/jama.289.9.1124. [DOI] [PubMed] [Google Scholar]
- 12.Davis PG, Henderson-Smart DJ. Nasal continuous positive airways pressure immediately after extubation for preventing morbidity in preterm infants. Cochrane Database Syst Rev. 2003;(2) doi: 10.1002/14651858.cd000143. CD000143. [DOI] [PubMed] [Google Scholar]
- 13.Davis PG, Henderson-Smart DJ. Nasal continuous positive airways pressure immediately after extubation for preventing morbidity in preterm infants. Cochrane Database Syst Rev. 2000;(2) doi: 10.1002/14651858.cd000143. CD000143. [DOI] [PubMed] [Google Scholar]
- 14.Davis PG, Henderson-Smart DJ. Extubation from low-rate intermittent positive airways pressure versus extubation after a trial of endotracheal continuous positive airways pressure in intubated preterm infants. Cochrane Database Syst Rev. 2001;(4) doi: 10.1002/14651858.cd001078. CD001078. [DOI] [PubMed] [Google Scholar]
- 15.Davis PG, Henderson-Smart DJ. Extubation from low-rate intermittent positive airways pressure versus extubation after a trial of endotracheal continuous positive airways pressure in intubated preterm infants. Cochrane Database Syst Rev. 2000;(2) doi: 10.1002/14651858.cd001078. CD001078. [DOI] [PubMed] [Google Scholar]
- 16.Davis PG, Lemyre B, de Paoli AG. Nasal intermittent positive pressure ventilation (NIPPV) versus nasal continuous positive airway pressure (NCPAP) for preterm neonates after extubation. Cochrane Database Syst Rev. 2001;(3) doi: 10.1002/14651858.cd003212. CD003212. [DOI] [PubMed] [Google Scholar]
- 17.De Paoli AG, Davis PG, Faber B, Morley CJ. Devices and pressure sources for administration of nasal continuous positive airway pressure (NCPAP) in preterm neonates. Cochrane Database Syst Rev. 2002;(4) doi: 10.1002/14651858.cd002977. CD002977. [DOI] [PubMed] [Google Scholar]
- 18.Henderson-Smart DJ, Davis PG. Prophylactic methylxanthines for extubation in preterm infants. Cochrane Database Syst Rev. 2003;(1) doi: 10.1002/14651858.cd000139. CD000139. [DOI] [PubMed] [Google Scholar]
- 19.Henderson-Smart DJ, Davis PG. Prophylactic methylxanthines for endotracheal extubation in preterm infants. Cochrane Database Syst Rev. 2010;(12) doi: 10.1002/14651858.CD000139.pub2. CD000139. [DOI] [PubMed] [Google Scholar]
- 20.Lemyre B, Davis PG, De Paoli AG. Nasal intermittent positive pressure ventilation (NIPPV) versus nasal continuous positive airway pressure (NCPAP) for apnea of prematurity. Cochrane Database Syst Rev. 2000;(3) doi: 10.1002/14651858.cd002272. CD002272. [DOI] [PubMed] [Google Scholar]
- 21.Wilkinson D, Andersen C, O’Donnell CP, De Paoli AG. High flow nasal cannula for respiratory support in preterm infants. Cochrane Database Syst Rev. 2011;(5) doi: 10.1002/14651858.CD006405.pub2. CD006405. [DOI] [PubMed] [Google Scholar]
- 22.Demauro SB, Giaccone A, Kirpalani H, Schmidt B. Quality of Reporting of Neonatal and Infant Trials in High-Impact Journals. Pediatrics. 2011;128:e639–44. doi: 10.1542/peds.2011-0377. [DOI] [PMC free article] [PubMed] [Google Scholar]


