Abstract
A venue-based HIV prevention study which included Voluntary Counseling and Testing (VCT) was conducted in three diverse areas of Kenya— Malindi, Nanyuki and Rachounyo. Aims of the study were to: 1) assess the acceptability of VCT for the general population, men who have sex with men (MSM), and injecting drug users (IDUs) within the context of a venue-based approach; 2) determine if there were differences between those agreeing and not agreeing to testing; and 3) study factors associated with being HIV positive. Approximately 98% of IDUs and 97% of MSM agreed to VCT, providing evidence that populations with little access to services and whose behaviors are stigmatized and often considered illegal in their countries can be reached with needed HIV prevention services. Acceptability of VCT in the general population ranged from 60% in Malindi to 48% in Nanyuki. There were a few significant differences between those accepting and declining testing. Notably in Rachuonyo and Malindi those reporting multiple partners were more likely to accept testing. There was also evidence that riskier sexual behavior was associated with being HIV positive for both men in Rachounyo and women in Malindi. Overall HIV prevalence was higher among the individuals in this study compared to individuals sampled in the 2008–2009 Kenya Demographic and Health Survey, indicating the method is an appropriate means to reach the highest risk individuals including stigmatized populations.
Keywords: HIV, MSM, IDUs, VCT, Kenya
Introduction
The HIV epidemic in Kenya varies by local context. According to the 2008–2009 Demographic and Health Survey (DHS) current HIV prevalence ranges from 0.9% in Northeastern Province to 13.9% in Nyanza Province.[1] National HIV prevalence in Kenya is 8% for the adult population 15–49.[1] Prevalence data has limitations in the effort to understand current transmission dynamics.[2] Because of the long survival time of individuals infected with HIV, changes in prevalence lag behind changes in risk. With data on incidence, however, temporal changes in the epidemic can be identified and linked to risk behaviors over the same time period.[3] Because data on incidence can be difficult to obtain, mathematical models (such as the UNAIDS modes of transmission model) have been developed to estimate incidence. According to a modes of transmission study in Kenya,[3] heterosexual unions (44.1%) are the largest source for new infections, followed by causal heterosexual sex (20.3%), female sex workers (FSWs) and clients (14.1%), men who have sex with men (MSM) and prison populations (15.2%), injecting drug users –IDUs (3.8%) and health facility related infections (2.5%). There is also much regional variation regarding modes of transmission. For example in Nairobi and the Coast Province, MSM and IDUs account for more of the incidence than at the national level.
Given the multi-faced nature of the HIV epidemic in Kenya, three study sites were selected for a Priority for Local AIDS Control Efforts (PLACE) study. The PLACE method uses available surveillance data and discussions with stakeholders at the national level to identify sub-national areas likely to have the highest HIV incidence. Within each of these priority prevention areas (PPAs), community informants identify venues where people meet new sexual partners and information is collected about the characteristics of the venues and the individuals attending the venues. The method is based on the proximate determinants framework which identifies the rate of new sexual partnerships as one of the drivers of the HIV epidemic. The persistent pattern of HIV surveillance data suggests that local HIV epidemics result in geographic clusters of new infections, rather than a random pattern of transmission [4]. The PLACE method has been shown to be more effective in capturing individuals with more risky sexual behaviors than individuals interviewed in household surveys in Zambia[4] Haiti [5] and South Africa.[4]
Kenyan stakeholders selected three PPAs based on data presented on HIV prevalence, presence of MARPS and the need for more prevention activities. The three PPAs also represent geographic diversity within Kenya - Malindi Town (population 144,426 according to the 1999 Kenya Census), Nanyuki Town (population 31,577 according to the 1999 Kenya Census), and Rachuonyo District (population 307,126 according to the 1999 Kenya Census). Malindi, a Coastal city, was chosen because it includes concentrations of MSM, IDUs, female sex workers (FSWs) and tourists. Nanyuki was chosen because it is a relatively large diverse town which has a substantial transient population. Nanyuki is home to local and foreign armed services, horticultural workers and FSWs. Truck and relief convoys also pass through the town. Rachuonyo is a district in Nyanza Province with high HIV prevalence, particularly among fishing communities. In addition to representing geographic and culturally distinct areas of Kenya, stakeholders felt these areas did not have large-scale prevention programs.
The PLACE study in Malindi included an oversampling of MSM and IDUs. In Kenya (as elsewhere in Africa) programs targeting and collecting data on MSMs and IDUs have been limited.[7] Community-based approaches are needed to reach groups who are highly stigmatized and not protected by the state. [8, 9] Because of stigma and illegality, there is often under-reporting of these behaviors in population-based studies.[10] In addition it is estimated that less than 1% of MSM in Africa have access to basic prevention services.[11]
The data, however, that is available on HIV prevalence among MSM in Kenya and in Africa indicates the need to target this group with prevention and treatment services. Sanders et al.[12] reported a HIV prevalence of 43.0% among MSM who had sex with men exclusively and a prevalence of 12.3% among MSM who had sex with both men and women in a vaccine preparedness cohort study in Mombasa, Kenya. Wade et al.[13] found a prevalence of 21.5% for MSM in urban areas of Senegal, while Baral et al.[14] found an overall prevalence of 17.4% for MSM in Malawi, Namibia and Botswana. In a study using respondent-driven sampling, an HIV prevalence of 17.4% was found for MSM in Lagos, Nigeria,[15] while a study also utilizing respondent-driven sampling found a prevalence of 12.3% for MSM in Zanzibar.[16]
Similarly the limited data on IDUs indicates the need to focus on this group as well. In Africa HIV prevalence among IDUs has been found to exceed that of the general population with prevalence ranging from 9% to 50% [17, 18] A study of IDUs in Nairobi, Kenya found prevalence to be 23% [19]. Another study in Kenya comparing IDUs and non-injecting drug users (NIDUs) found a prevalence of 31.2% for the former and a prevalence of 6.3% for the later [20].
Though over 60 PLACE studies have been conducted around the world, this is one of the first to include an HIV testing component in addition to the questionnaires. A PLACE study in the Congo compared HIV prevalence among men and women at social venues, at sexually transmitted infection (STI) clinics and antenatal (ANC) clinics. HIV prevalence was highest among clients at the STI clinics, followed by the social venues and then the ANC clinics. [19] A PLACE study in Jamaica found that MSM who were of low social economic status, ever homeless and victims of physical violence were significantly more likely to be HIV positive. [20] The aims of this research are to understand the utility of the PLACE method in reaching MSM and IDUs in addition to the general high risk population in Kenya and to understand if voluntary counseling and testing (VCT) for HIV can be provided successfully within the context of a venue-based study. Other aims are to understand if there are differences between individuals who agree to be tested and individuals who decline testing as well as to understand factors associated with being HIV positive.
Methods
The PLACE method has five steps. The first step is the selection of PPAs. The three PPAs (Malindi, Nanyuki and Rachounyo) were selected by stakeholders at a national meeting in Nairobi, Kenya in February 2009. As mentioned earlier, the sites were chosen because they represent varying geographic areas and modes of transmission and were areas felt to be in need of more HIV prevention services.
Steps 2 through 4 were carried out in April to May 2010. Step 2 involves identifying venues and events that people are believed to frequent to meet new sexual partners. This is done by having interviewers approach potential community informants and requesting them to list the places where people are believed to meet new partners in their local area. In Malindi there were also extra questions on where MSM and IDUs, in particular, meet new partners. Community informants are people believed to be knowledgeable about their community. In Malindi the most common types of informants were health care workers, beer/liquor store owners, mobile hawkers/street vendors, taxi drivers and program coordinators, peer educators and business people. In Nanyuki the most common community informants were mobile hawkers/street vendors, individuals socializing at venues, hairdressers, barbers, hotel workers/managers and taxi drivers. In Rachounyo the most common types of informants were youth, hairdressers/barbers, beer liquor store owners, taxi drivers, fishermen, shopkeepers and fish mongers.
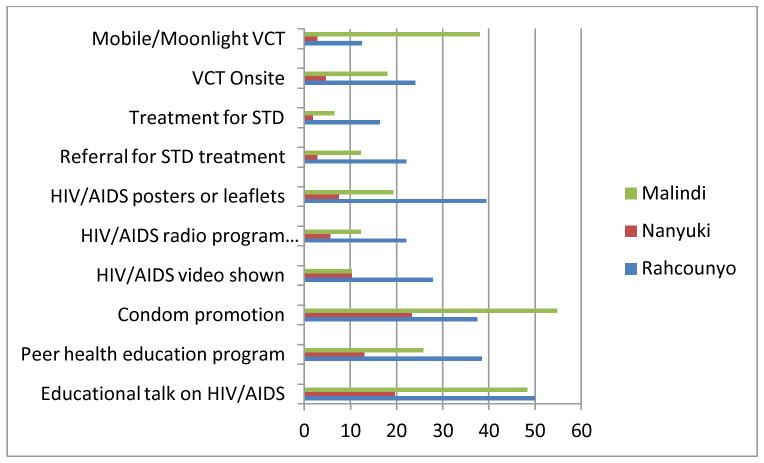
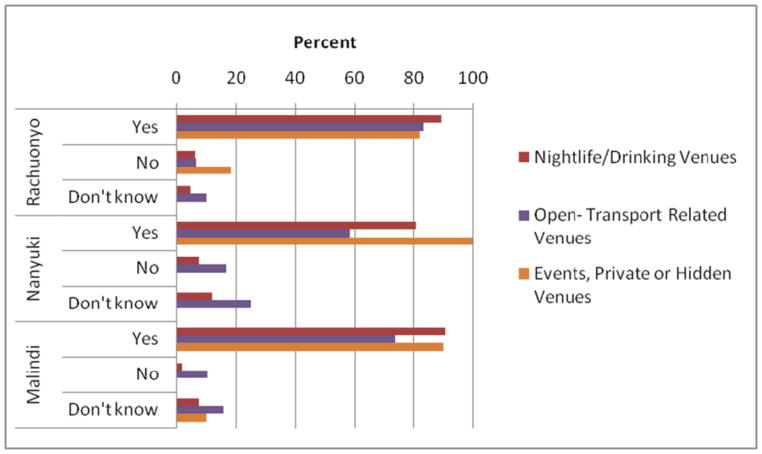
In Step 3 each venue/event was visited and verified. In Malindi 202 community informants listed 157 unique venues. In Nanyuki 205 community informants listed 108 unique venues, and in Rachuonyo 203 community informants listed 108 unique venues. At each of the venues a representative was interviewed to obtain information about the venue and about people who socialize at that venue. For example they were asked about the busiest times for that venue, numbers of people socializing at a busy time, characteristics of the socializers (where did they come from, did they included IDUs and MSM) and activities that occur at the venue (eating, drinking, dancing etc.) The venue representative was typically an owner or manager or someone who worked at the venue (or near the venue in the case of open spaces) and was knowledgeable about the people who typically socialize at that venue. They were also asked about existing HIV prevention activities and the willingness to have such activities. Overall, HIV prevention activities were most common in Rachuonyo, with the exception of condom promotion and mobile VCT, which were both most common in Malindi (Figure 1). About 55% of venue representatives in Malindi indicated that their sites offered condom promotion and 38% had mobile/moonlight VCT. In Rachuonyo the most common prevention activities were educational talks (50%) and peer health education (38%). In Nanyuki the most common prevention activities were condom promotion (24%) and educational talks on HIV/AIDS (20%). Venue representatives indicated a willingness to have HIV prevention activities and some willingness to sell condoms at their sites (Figure 2). Willingness to have HIV prevention activities was over 80% at all sites in Rachounyo. In both Nanyuki and Malindi, willingness to have HIV prevention activities was over 80% at the nightlife/drinking sites and the events/private or hidden sites. However, such openness towards HIV prevention activities was lower in the open-transport related sites.
Figure 1.
Percentage of HIV/AIDS prevention activities at venues, by PPA
Figure 2.
Willingness to have HIV prevention activities, by venue category and PPA
A categorization was used to classify the different types of venues –nightlife/drinking, open/transport-related and events/private or hidden areas.[21] The nightlife/drinking sites include places where people go to eat, drink, dance etc. Often alcohol is consumed at such sites. The open/transport sites are typical community locations such as schools, shops, churches, bus stations etc. The events/private or hidden sites occur in (or are) private locations not open to the general public or are events which require the purchase of a ticket. Common events were funerals, weddings, sporting events and concerts while common private or hidden sites were unused houses, abandoned fields and private dwellings. Figure 3 shows the categorization of venues for each of the three study sites. In each study sites the majority of venues fell into the nightlife/drinking category.
Figure 3.
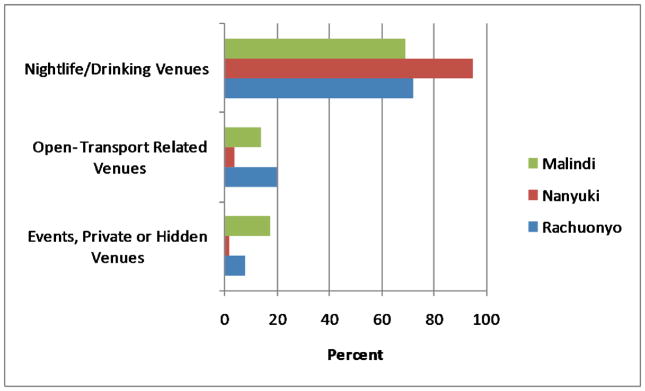
Categories of venues, by PPA
In step 4 the characteristics of people socializing or working at the sites are obtained. Topics in the questionnaire included socioeconomic background, exposure to HIV prevention and testing services and sexual and drug using behavior. Not all venues/events were selected for step 4. Venues/events were randomly selected using a systematic fixed interval sampling strategy with the probability of selection proportional to the size of the venue. Size of the venue was considered the number of people socializing at a busy time as indicated by the venue representative. Venues and events were listed by both geographic code and size. Large venues could be selected more than once if their cluster code number was larger than the selection interval. The systematic fixed interval strategy for sampling produced a self-weighted sample which gives all individuals socializing and working at eligible venues an equal probability of selection for an individual interview. In Malindi the 15 sites identified as being venues where MSM socialize were removed from the list of general venues for Malindi. Interviews were conducted in all venues identified as places where MSM socialize. Probability proportional-to-size was then used to select 27 general venues/events in Malindi (14 nightlife/drinking sites, 9 open/transport sites, and 4 events/private or hidden sites). In Rachuonyo 21 venues/events were selected (13 nightlife/drinking, 6 open/transport, and 2 events/private or hidden sites), and in Nanyuki 30 venues/events (24 nightlife/drinking, 6 open/transport, and no events/private or hidden sites). It should be noted that interviewers in Malindi were experienced in working with the MSM and IDU communities.
Interviewers were to select 20 individuals (10–13 men and 7–10 women) to interview at each of the selected venues and 4 workers (2 male and 2 female). The numbers of men and women to interview were based on the gender composition of socializers at each venue which was obtained from the venue representative survey. For those sites with more than 20 individuals, interviewers randomly selected individuals. For those sites with fewer than 20 individuals and fewer than 4 workers, all were interviewed. At some of the very small venues, interviewers waited for more socializers to arrive. All individuals aged 18 and older were eligible for interview. Those 16 or 17 could be interviewed if they were at the venue as a socializer (acting as an adult) and not on a family errand.
At sites with more than 20 individuals socializing or more than 4 workers, individuals were randomly selected for interview. Interviewers would start in one corner of the room, count the number of individuals and interview the ith individual. For example if there were 80 socializers, then every 4th individual would be interviewed. An explanation of the study was read aloud as well as an oral consent form. Patrons and workers had an opportunity to be tested for HIV. They were informed of this at the beginning of the questionnaire and again at the end of the questionnaire. Some individuals chose to answer the questionnaire but not to be tested for HIV. Those who agreed to testing were taken to a quiet room in the venue or a nearby venue. In some cases a tent was pitched outside the venue for privacy. VCT was done by experienced and trained counselors. Individuals could receive their results immediately or could call for their results at a later time. All HIV positive individuals were referred to the nearest VCT center for follow-up counseling and guidance on treatment options. This study underwent ethics review at the University of North Carolina at Chapel Hill and also at the Kenyatta National Hospital Ethics Review board. Step 5 of the PLACE Method is to use findings to inform decision-making. This step is being led by the National AIDS Control Council (NACC) of Kenya.
Tested versus non-tested and HIV-positive versus HIV-negative individuals were compared, and analyses were stratified by study site. In Malindi, the male study population was divided into three subgroups: the general population, MSM, and IDUs. Two methods were used to define MSM and IDUs—according to the venues identified by the community informants and by self-reports. Rank sum and chi-square tests were used to test for statistical significance. Several covariates were studied, including the socioeconomic variables age, gender, working status, worker/patron education, residence, marital status and poverty. In keeping with international definitions a person was considered to be living in poverty if they lived on less than $1.25 per day. Several proximate determinants were also studied: partners in the past 4 weeks and 12 months; new partners in the past 4 weeks and 12 months; and transactional sex (given or received money for sex in the past year).
Results
About 92% of individuals at venues identified by community informants self-identified as MSM, and 98% of individuals at venues identified by community informants self-identified as IDUs. In addition 9% and 4% of men socializing at “general” venues in Malindi also self-identified as MSM and IDUs, respectively. In this analysis we use data on self-reporting. No men in Nanyuki or Rachounyo self-identified as MSM, and only a handful identified as IDUs.
Comparison of respondents tested and not tested for HIV
Table 1 shows comparisons between those who agreed to HIV testing and those who did not. Of note is the high testing response rate for the IDU and MSM subpopulations in Malindi (98.1% and 97.3%, respectively). Respondents in Rachounyo who agreed to testing were more likely to be less educated (z = −2.66, P < 0.01), to live in rural areas (55.3% vs. 43.3%, χ2 = 8.38, P < 0.01), and to report multiple new partnerships in the past four weeks (z = 1.96, P < 0.05), while those in Nanyuki who agreed to testing were more likely to be young (z = −3.22, P < 0.01) and less educated (z = −3.70, P < 0.001). The Malindi non-MSM/non-IDU (general) subpopulation which agreed to testing was more likely to be impoverished (20.5% vs. 10.9%, χ2 = 9.63, P < 0.01) and less likely to report multiple partnerships in the past four weeks (z = −2.32, P < 0.05).
Table 1.
Comparison of respondents who were tested for HIV and those who were not tested, by site and risk population
| Rachuonyo (N=599) | Nanyuki (N=600) | Malindi-General (N=623) | Malindi-MSM (N=262) | Malindi-IDU (N=154) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Tested | Not tested |
Test Statistic |
Tested | Not tested |
Test Statistic |
Tested | Not tested |
Test Statistic |
Tested | Not tested |
Test Statistic |
Tested | Not tested |
Test Statistic |
|
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | ||||||
| 343 (57.3) | 256 (42.7) | 287 (47.8) | 313 (52.2) | 374 (60.0) | 249 (40.0) | 255 (97.3) | 7 (2.7) | 151 (98.1) | 3 (1.9) | ||||||
| Age | |||||||||||||||
| 15–24 | 112 (32.7) | 76 (29.7) | 98 (34.1) | 64 (20.4) | 133 (35.6) | 72 (28.9) | 53 (20.8) | 3 (42.9) | 27 (17.9) | 1 (33.3) | |||||
| 25–34 | 138 (40.2) | 115 (44.9) | 135 (47.0) | 177 (56.5) | 154 (41.2) | 119 (47.8) | 128 (50.2) | 4 (57.1) | 86 (57.0) | 2 (66.7) | |||||
| 34+ | 93 (27.1) | 65 (25.4) | z = −0.22 | 54 (18.8) | 72 (23.0) | z = −3.225** | 87 (23.3) | 58 (23.3) | z = −1.163 | 74 (29.0) | 0 (0) | z = 1.903 | 38 (25.2) | 0 (0) | z = 1.07 |
| Gender | |||||||||||||||
| Male | 219 (63.8) | 148 (57.8) | 175 (61.8) | 214 (68.6) | 247 (66.2) | 156 (62.7) | 252 (100) | 7 (100) | 138 (93.2) | 3 (100) | |||||
| Female | 124 (36.2) | 108 (42.2) | χ2 = 2.25 | 108 (38.2) | 98 (31.4) | χ2 = 2.99 | 126 (33.8) | 93 (37.3) | χ2 = 0.83 | NA | NA | 10 (6.8) | 0 (0) | χ2 = 0.22 | |
| Currently working | |||||||||||||||
| Yes | 301 (88.5) | 224 (88.9) | 243 (85.0) | 275 (88.4) | 318 (85.0) | 211 (86.5) | 216 (85.0) | 6 (85.7) | 133 (89.9) | 3 (100) | |||||
| No | 39 (11.5) | 28 (11.1) | χ2 = 0.02 | 43 (15.0) | 36 (11.6) | χ2 = 1.55 | 56 (15.0) | 33 (13.5) | χ2 = 0.25 | 38 (15.0) | 1 (14.3) | χ2 = 0.00 | 15 (10.1) | 0 (0) | χ2 = 0.34 |
| Highest level of education | |||||||||||||||
| None | 5 (1.5) | 1 (0.4) | 13 (4.6) | 10 (3.2) | 66 (17.6) | 36 (14.6) | 79 (31.3) | 1 (14.3) | 64 (42.7) | 0 (0) | |||||
| Primary | 144 (42.5) | 81 (32.1) | 69 (24.2) | 51 (16.3) | 169 (45.2) | 98 (39.8) | 114 (45.2) | 4 (57.1) | 63 (42.0) | 2 (66.7) | |||||
| Secondary | 139 (41.0) | 124 (49.2) | 140 (49.1) | 142 (45.5) | 97 (25.9) | 80 (32.5) | 44 (17.5) | 1 (14.3) | 21 (14.0) | 0 (0) | |||||
| Post-second. | 51 (15.0) | 46 (18.3) | z = −2.66** | 63 (22.1) | 109 (34.9) | z = −3.70*** | 42 (11.2) | 32 (13.0) | z = −1.899 | 15 (6.0) | 1 (14.3) | z = −0.88 | 2 (1.3) | 1 (33.3) | z = −1.60 |
| Residence | |||||||||||||||
| Urban | 151 (44.7) | 144 (56.7) | 230 (80.4) | 263 (84.6) | 341 (92.4) | 232 (94.7) | 224 (88.9) | 7 (100) | 147 (98.7) | 3 (100) | |||||
| Rural | 187 (55.3) | 110 (43.3) | χ2 = 8.38** | 56 (19.6) | 48 (15.4) | χ2 = 1.78 | 28 (7.6) | 13 (5.3) | χ2 = 1.23 | 28 (11.1) | 0 (0) | χ2 = 0.87 | 2 (1.3) | 0 (0) | χ2 = 0.04 |
| Marital status | |||||||||||||||
| Ever married | 225 (67.2) | 169 (67.6) | 160 (56.1) | 181 (58.8) | 209 (58.2) | 151 (62.4) | 116 (47.0) | 4 (57.1) | 83 (55.7) | 1 (33.3) | |||||
| Never married | 110 (32.8) | 81 (32.4) | χ2 = 0.01 | 125 (43.9) | 127 (41.2) | χ2 = 0.42 | 150 (41.8) | 91 (37.6) | χ2 = 1.05 | 131 (53.0) | 3 (42.9) | χ2 = 0.28 | 66 (44.3) | 2 (66.7) | χ2 = 0.60 |
| Poverty status | |||||||||||||||
| In poverty | 89 (26.4) | 56 (22.6) | 56 (19.9) | 46 (14.9) | 76 (20.5) | 26 (10.9) | 34 (13.5) | 1 (16.7) | 20 (13.3) | 0 (0) | |||||
| Not in poverty | 248 (73.6) | 192 (77.4) | χ2 = 1.12 | 226 (80.1) | 262 (85.1) | χ2 = 2.50 | 295 (79.5) | 213 (89.1) | χ2 = 9.63** | 218 (86.5) | 5 (83.3) | χ2 = 0.05 | 130 (86.7) | 3 (100) | χ2 = 0.46 |
| # partners past 4 weeks | |||||||||||||||
| 0 | 41 (12.0) | 34 (13.4) | 68 (23.8) | 66 (21.2) | 112 (30.0) | 48 (19.4) | 14 (5.5) | 0 (0) | 41 (27.2) | 0 (0) | |||||
| 1 | 210 (61.6) | 168 (66.1) | 148 (51.7) | 163 (52.2) | 186 (49.9) | 144 (58.3) | 35 (13.7) | 3 (42.9) | 61 (40.4) | 2 (66.7) | |||||
| 2+ | 90 (26.4) | 52 (20.5) | z = 1.52 | 70 (24.5) | 83 (26.6) | z = −0.835 | 75 (20.1) | 55 (22.3) | z = −2.320* | 206 (80.8) | 4 (57.1) | z = 1.38 | 49 (32.5) | 1 (33.3) | z = −0.60 |
| # partners past 12 months | |||||||||||||||
| 0 | 17 (5.0) | 18 (7.1) | 30 (10.5) | 33 (10.6) | 32 (8.6) | 16 (6.5) | 0 (0.0) | 0 (0) | 13 (8.6) | 0 (0) | |||||
| 1 | 171 (50.1) | 133 (52.8) | 136 (47.6) | 127 (40.7) | 187 (50.1) | 121 (49.2) | 17 (6.7) | 0 (0) | 48 (31.8) | 1 (33.3) | |||||
| 2+ | 153 (44.9) | 101 (40.1) | z = 1.348 | 120 (42.0) | 152 (48.7) | z = −1.401 | 154 (41.3) | 109 (44.3) | z = −0.938 | 237 (93.3) | 7 (100) | z = −0.71 | 90 (59.6) | 2 (66.7) | z = −0.34 |
| # new partners past 4 weeks | |||||||||||||||
| 0 | 236 (69.2) | 194 (77.0) | 215 (74.9) | 221 (70.8) | 279 (75.2) | 173 (71.2) | 80 (31.6) | 4 (57.1) | 104 (69.3) | 1 (33.3) | |||||
| 1 | 75 (22.0) | 38 (15.1) | 47 (16.4) | 57 (18.3) | 62 (16.7) | 49 (20.2) | 52 (20.6) | 2 (28.6) | 34 (22.7) | 1 (33.3) | |||||
| 2+ | 30 (8.8) | 20 (7.9) | z = 1.96* | 25 (8.7) | 34 (10.9) | z = −1.159 | 30 (8.1) | 21 (8.6) | z = −1.040 | 121 (47.8) | 1 (14.3) | z = 1.77 | 12 (8.0) | 1 (33.3) | z = −1.49 |
| # new partners past 12 months | |||||||||||||||
| 0 | 175 (51.3) | 144 (57.1) | 164 (57.5) | 157 (50.5) | 201 (54.2) | 128 (52.2) | 21 (8.3) | 0 (0) | 55 (36.7) | 1 (33.3) | |||||
| 1 | 79 (23.2) | 45 (17.9) | 59 (20.7) | 77 (24.8) | 96 (25.9) | 61 (24.9) | 42 (16.6) | 2 (28.6) | 38 (25.3) | 0 (0) | |||||
| 2+ | 87 (25.5) | 63 (25.0) | z = 1.056 | 62 (21.8) | 77 (24.8) | z = −1.586 | 74 (19.9) | 56 (22.9) | z = −0.668 | 190 (75.1) | 5 (71.4) | z = 0.077 | 57 (38.0) | 2 (66.7) | z = −0.64 |
P < 0.05,
P < 0.01,
P < 0.001
Comparison of HIV positive and HIV negative respondents
Tables 2 and 3 present results from comparisons between male respondents who tested HIV positive and those who tested negative. MSM and male IDUs in Malindi had a much higher HIV prevalence (19.8% and 22.7%, respectively) than the general male population in Malindi (4.4%). HIV prevalence was also high in Rachuounyo (16.9% for males, 23.4% for females). Of note is that the HIV prevalence for both men and women in all three sites was higher than estimates provided by the Kenya DHS 2008–2009, a population-based survey. According to the DHS, HIV prevalence for men aged 15–49 in Coast Province (Malindi), Nanyuki (Rift Valley Province) and Rachuonyo (Nyzana) was 2.3%, 2.8%, and 11.4%, and for women, 5.8%, 6.3%, and 16.0%, respectively.
Table 2.
Comparison of male respondents who tested HIV+ and those who tested HIV−, by site and risk population
| Rachuonyo (N=219) | Nanyuki (N=179) | Malindi-General (N=236) | Malindi-MSM (N=253) | Malindi-IDU (N=141) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HIV+ | HIV− | Test Statistic |
HIV+ | HIV− | Test Statistic |
HIV+ | HIV− | Test Statistic |
HIV+ | HIV− | Test Statistic |
HIV+ | HIV− | Test Statistic |
|
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | ||||||
| 37 (16.9) | 182 (83.1) | 10 (5.6) | 169 (94.4) | 11 (4.4) | 236 (95.6) | 50 (19.8) | 203 (80.2) | 32 (22.7) | 109 (77.3) | ||||||
| Age | |||||||||||||||
| 15–24 | 6 (16.2) | 64 (35.2) | 1 (10.0) | 49 (29) | 3 (27.3) | 82 (34.7) | 8 (16.0) | 44 (21.7) | 4 (12.5) | 19 (17.4) | |||||
| 25–34 | 17 (45.9) | 70 (38.5) | 6 (60.0) | 83 (49.1) | 4 (36.4) | 94 (39.8) | 26 (52.0) | 102 (50.2) | 16 (50.0) | 64 (58.7) | |||||
| 34+ | 14 (37.8) | 48 (26.4) | z = 2.182* | 3 (30.0) | 37 (21.9) | z = 1.19 | 4 (36.4) | 60 (25.4) | z = 0.76 | 16 (32.0) | 57 (28.1) | z = 0.86 | 12 (37.5) | 26 (23.9) | z = 1.45 |
| Currently working | |||||||||||||||
| Yes | 36 (97.3) | 157 (87.7) | 10 (100) | 153 (91.1) | 11 (100) | 207 (87.7) | 44 (89.8) | 170 (83.7) | 29 (90.6) | 98 (91.6) | |||||
| No | 1 (2.7) | 22 (12.3) | χ2 = 2.96 | 0 (0) | 15 (8.9) | χ2 = 0.98 | 0 (0) | 29 (12.3) | χ2 = 1.53 | 5 (10.2) | 33 (16.3) | χ2 = 1.13 | 3 (9.4) | 9 (8.4) | χ2 = 0.03 |
| Highest level of education | |||||||||||||||
| None | 1 (2.7) | 3 (1.7) | 0 (0) | 8 (4.8) | 1 (9.1) | 46 (19.5) | 18 (36.0) | 60 (30.0) | 13 (40.6) | 44 (40.7) | |||||
| Primary | 14 (37.8) | 69 (38.3) | 1 (10.0) | 33 (19.8) | 4 (36.4) | 101 (42.8) | 17 (34.0) | 96 (48.0) | 13 (40.6) | 47 (43.5) | |||||
| Secondary | 15 (40.5) | 82 (45.6) | 6 (60.0) | 84 (50.3) | 4 (36.4) | 63 (26.7) | z = 1.24 | 10 (20.0) | 34 (17.0) | 6 (18.8) | 15 (13.9) | ||||
| Post-secondary | 7 (18.9) | 26 (14.4) | z = 0.19 | 3 (30.0) | 42 (25.1) | z = 0.867 | 2 (18.2) | 26 (11.0) | 5 (10.0) | 10 (5.0) | z = 0.19 | 0 (0) | 2 (1.9) | z = 0.14 | |
| Residence | |||||||||||||||
| Urban | 17 (45.9) | 72 (40.0) | 8 (80.0) | 144 (85.2) | 11 (100) | 212 (91.0) | 45 (90.0) | 178 (89.0) | 32 (100) | 106 (98.1) | |||||
| Rural | 20 (54.1) | 108 (60.0) | χ2 = 0.45 | 2 (20.0) | 25 (14.8) | χ2 = 0.20 | 0 (0) | 21 (9.0) | χ2 = 1.08 | 5 (10.0) | 22 (11.0) | χ2 = 0.04 | 0 (0) | 2 (1.9) | χ2 = 0.60 |
| Marital status | |||||||||||||||
| Ever married | 31 (83.8) | 105 (58.7) | 7 (70.0) | 99 (58.9) | 8 (80.0) | 122 (54.0) | 22 (44.9) | 93 (47.4) | 19 (59.4) | 58 (53.7) | |||||
| Never married | 6 (16.2) | 74 (41.3) | χ2 = 8.30** | 3 (30.0) | 69 (41.1) | χ2 = 0.48 | 2 (20.0) | 104 (46.0) | χ2 = 2.62 | 27 (55.1) | 103 (52.6) | χ2 = 0.10 | 13 (40.6) | 50 (46.3) | χ2 = 0.32 |
| Poverty status | |||||||||||||||
| In poverty | 5 (13.5) | 45 (25.4) | 0 (0) | 19 (11.5) | 1 (9.1) | 44 (18.7) | 2 (4.2) | 31 (15.3) | 3 (9.7) | 15 (13.8) | |||||
| Not in poverty | 32 (86.5) | 132 (74.6) | χ2 = 2.42 | 10 (100) | 146 (88.5) | χ2 = 1.29 | 10 (90.9) | 191 (81.3) | χ2 = 0.65 | 46 (95.8) | 171 (84.7) | χ2 = 4.23* | 28 (90.3) | 94 (86.2) | χ2 = 0.36 |
| # partners past 4 wks | |||||||||||||||
| 0 | 2 (5.4) | 30 (16.7) | 3 (30.0) | 33 (19.5) | 3 (27.3) | 76 (32.2) | 3 (6.0) | 11 (5.4) | 11 (34.4) | 29 (26.6) | |||||
| 1 | 21 (56.8) | 109 (60.6) | 4 (40.0) | 88 (52.1) | 6 (54.5) | 109 (46.2) | 11 (22.0) | 23 (11.3) | 11 (34.4) | 46 (42.2) | |||||
| 2+ | 14 (37.8) | 41 (22.8) | z = 2.32* | 3 (30.0) | 48 (28.4) | z = −0.36 | 2 (18.2) | 51 (21.6) | z = 0.09 | 36 (72.0) | 169 (83.3) | z = −1.72 | 10 (31.3) | 34 (31.2) | z = −0.48 |
| # partners past 12 months | |||||||||||||||
| 0 | 0 (0) | 13 (7.2) | 2 (20.0) | 16 (9.5) | 1 (9.1) | 20 (8.5) | 0 (0) | 0 (0) | 7 (21.9) | 6 (5.5) | |||||
| 1 | 12 (32.4) | 92 (51.1) | 4 (40.0) | 69 (40.8) | 7 (63.6) | 116 (49.2) | 6 (12.0) | 10 (5.0) | 8 (25.0) | 37 (33.9) | |||||
| 2+ | 25 (67.6) | 75 (41.7) | z = 3.04** | 4 (40.0) | 84 (49.7) | z = −0.83 | 3 (27.3) | 100 (42.4) | z = −0.89 | 44 (88.0) | 192 (95.0) | z = −1.83 | 17 (53.1) | 66 (60.6) | z = −1.32 |
| # new partners past 4 weeks | |||||||||||||||
| 0 | 23 (62.2) | 127 (70.6) | 7 (70.0) | 124 (73.4) | 8 (72.7) | 173 (73.9) | 15 (30.6) | 64 (31.7) | 19 (61.3) | 80 (73.4) | |||||
| 1 | 9 (24.3) | 41 (22.8) | 2 (20.0) | 33 (19.5) | 3 (27.3) | 42 (17.9) | 11 (22.4) | 41 (20.3) | 10 (32.3) | 21 (19.3) | |||||
| 2+ | 5 (13.5) | 12 (6.7) | z = 1.16 | 1 (10.0) | 12 (7.1) | z = 0.27 | 0 (0) | 19 (8.1) | z = −0.07 | 23 (46.9) | 97 (48.0) | z = −0.02 | 2 (6.5) | 8 (7.3) | z = 1.17 |
| # new partners past 12 months | |||||||||||||||
| 0 | 13 (35.1) | 96 (53.3) | 5 (50.0) | 90 (53.3) | 5 (45.5) | 125 (53.4) | 6 (12.0) | 14 (7.0) | 13 (41.9) | 40 (36.7) | |||||
| 1 | 13 (35.1) | 45 (25.0) | 4 (40.0) | 36 (21.3) | 4 (36.4) | 62 (26.5) | 10 (20.0) | 32 (15.9) | 8 (25.8) | 28 (25.7) | |||||
| 2+ | 11 (29.7) | 39 (21.7) | z = 1.88 | 1 (10.0) | 43 (25.4) | z = −0.280 | 2 (18.2) | 47 (20.1) | z = 0.34 | 34 (68.0) | 155 (77.1) | z = −1.40 | 10 (32.3) | 41 (37.6) | z = −0.60 |
| Worker/patron status | |||||||||||||||
| Worker | 25 (67.6) | 90 (49.5) | 0 (0) | 46 (27.9) | 4 (36.4) | 59 (25.1) | 3 (6.0) | 8 (4.0) | 2 (6.3) | 2 (1.8) | |||||
| Patron | 12 (32.4) | 92 (50.5) | χ2 = 4.05* | 9 (100) | 119 (72.1) | χ2 = 3.41 | 7 (63.6) | 176 (74.9) | χ2 = 0.70 | 47 (94.0) | 194 (96.0) | χ2 = 0.40 | 30 (93.8) | 107 (98.2) | χ2 = 1.75 |
| Given or received money for sex in past 12 months | |||||||||||||||
| No | 29 (80.6) | 160 (88.9) | 7 (70.0) | 132 (80.0) | 9 (81.8) | 187 (80.6) | 16 (33.3) | 69 (34.2) | 24 (80.0) | 83 (76.9) | |||||
| Yes | 7 (19.4) | 20 (11.1) | χ2 = 1.90 | 3 (30.0) | 33 (20.0) | χ2 = 0.58 | 2 (18.2) | 45 (19.4) | χ2 = 0.01 | 32 (66.7) | 133 (65.8) | χ2 = 0.01 | 6 (20.0) | 25 (23.1) | χ2 = 0.13 |
P < 0.05,
P < 0.01,
P < 0.001
Table 3.
Comparison of female respondents who tested HIV+ and those who tested HIV−, by site
| Rachuonyo (N=124) | Nanyuki (N=111) | Malindi (N=127) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| HIV+ | HIV− | Test Statistic | HIV+ | HIV− | Test Statistic | HIV+ | HIV− | Test Statistic | |
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | ||||
| 29 (23.4) | 95 (76.6) | 10 (9.0) | 101 (91.0) | 10 (7.9) | 117 (92.1) | ||||
| Age | |||||||||
| 15–24 | 9 (31.0) | 32 (33.7) | 0 (0) | 50 (49.5) | 3 (30.0) | 44 (37.6) | |||
| 25–34 | 15 (51.7) | 36 (37.9) | 4 (40.0) | 43 (42.6) | 4 (40.0) | 52 (44.4) | |||
| 34+ | 5 (17.2) | 27 (28.4) | z = −0.48 | 6 (60.0) | 8 (7.9) | z = 4.10*** | 3 (30.0) | 21 (17.9) | z = 0.778 |
| Currently working | |||||||||
| Yes | 25 (86.2) | 83 (87.4) | 7 (70.0) | 76 (75.2) | 8 (80.0) | 92 (78.6) | |||
| No | 4 (13.8) | 12 (12.6) | χ2 = 0.03 | 3 (30.0) | 25 (24.8) | χ2 = 0.13 | 2 (20.0) | 25 (21.4) | χ2 = 0.01 |
| Highest level of education | |||||||||
| None | 0 (0) | 1 (1.1) | 1 (10.0) | 3 (3.0) | 1 (10.0) | 19 (16.2) | |||
| Primary | 14 (48.3) | 46 (49.5) | 4 (40.0) | 32 (31.7) | 5 (50.0) | 58 (49.6) | |||
| Secondary | 9 (31.0) | 34 (36.6) | 4 (40.0) | 48 (47.5) | 2 (20.0) | 28 (23.9) | |||
| Post-secondary | 6 (20.7) | 12 (12.9) | z = 0.56 | 1 (10.0) | 18 (17.8) | z = −1.106 | 2 (20.0) | 12 (10.3) | z = 0.66 |
| Residence | |||||||||
| Urban | 13 (44.8) | 49 (53.3) | 6 (60.0) | 74 (74.0) | 10 (100) | 108 (93.9) | |||
| Rural | 16 (55.2) | 43 (46.7) | χ2 = 0.63 | 4 (40.0) | 26 (26.0) | χ2 = 0.90 | 0 (0) | 7 (6.1) | χ2 = 0.64 |
| Marital status | |||||||||
| Ever married | 22 (75.9) | 68 (75.6) | 9 (90.0) | 46 (46.0) | 8 (80.0) | 71 (63.4) | |||
| Never married | 7 (24.1) | 22 (24.4) | χ2 = 0.00 | 1 (10.0) | 54 (54.0) | χ2 = 7.04** | 2 (20.0) | 41 (36.6) | χ2 = 1.11 |
| Poverty status | |||||||||
| In poverty | 12 (42.9) | 28 (29.5) | 6 (60.0) | 30 (30.0) | 3 (30.0) | 29 (25.2) | |||
| Not in poverty | 16 (57.1) | 67 (70.5) | χ2 = 1.77 | 4 (40.0) | 70 (70.0) | χ2 = 3.72 | 7 (70.0) | 86 (74.8) | χ2 = 0.11 |
| # partners past 4 weeks | |||||||||
| 0 | 3 (10.3) | 5 (5.3) | 1 (10.0) | 31 (31.0) | 2 (22.2) | 32 (27.4) | |||
| 1 | 16 (55.2) | 64 (67.4) | 8 (80.0) | 50 (50.0) | 3 (33.3) | 68 (58.1) | |||
| 2+ | 10 (34.5) | 26 (27.4) | z = 0.30 | 1 (10.0) | 19 (19.0) | z = 0.619 | 4 (44.4) | 17 (14.5) | z = 1.459 |
| # partners past 12 months | |||||||||
| 0 | 1 (3.4) | 2 (2.1) | 0 (0) | 12 (12.0) | 0 (0) | 11 (9.4) | |||
| 1 | 15 (51.7) | 53 (55.8) | z = 0.18 | 9 (90.0) | 54 (54.0) | 2 (22.2) | 63 (53.8) | ||
| 2+ | 13 (44.8) | 40 (42.1) | 1 (10.0) | 34 (34.0) | z = −0.778 | 7 (77.8) | 43 (36.8) | z = 2.40* | |
| # new partners past 4 weeks | |||||||||
| 0 | 18 (62.1) | 67 (70.5) | 9 (90.0) | 76 (75.2) | 6 (66.7) | 93 (79.5) | |||
| 1 | 6 (20.7) | 19 (20.0) | 0 (0) | 14 (13.9) | 1 (11.1) | 15 (12.8) | |||
| 2+ | 5 (17.2) | 9 (9.5) | z = 0.99 | 1 (10.0) | 11 (10.9) | z = −0.939 | 2 (22.2) | 9 (7.7) | z = 1.03 |
| # new partners past 12 months | |||||||||
| 0 | 15 (51.7) | 51 (53.7) | 9 (90.0) | 60 (60.6) | 3 (33.3) | 68 (58.1) | |||
| 1 | 5 (17.2) | 15 (15.8) | 0 (0) | 20 (20.2) | 1 (11.1) | 29 (24.8) | |||
| 2+ | 9 (31.0) | 29 (30.5) | z = 0.14 | 1 (10.0) | 19 (19.2) | z = −1.66 | 5 (55.6) | 20 (17.1) | z = 2.04* |
| Worker/patron status | |||||||||
| Worker | 15 (51.7) | 60 (63.8) | 0 (0) | 35 (35.7) | 2 (20.0) | 36 (31.0) | |||
| Patron | 14 (48.3) | 34 (36.2) | χ2 = 1.36 | 10 (100) | 63 (64.3) | χ2 = 5.28* | 8 (80.0) | 80 (69.0) | χ2 = 0.53 |
| Given or received money for sex in past 12 months | |||||||||
| No | 24 (82.8) | 84 (89.4) | 9 (90.0) | 82 (82.0) | 4 (40.0) | 96 (83.5) | |||
| Yes | 5 (17.2) | 10 (10.6) | χ2 = 0.90 | 1 (10.0) | 18 (18.0) | χ2 = 0.41 | 6 (60.0) | 19 (16.5) | χ2 = 10.87** |
P < 0.05,
P < 0.01,
P < 0.001
Male respondents in Rachuonyo who tested positive for HIV were more likely to be older (z = 2.18, P < 0.05), ever married (83.8% vs. 58.7%, χ2 = 8.30, P < 0.01), report multiple partners in the past four weeks (z = 2.32, P < 0.05) and past 12 months (z = 3.04, P < 0.01), and be workers as opposed to patrons at the venues (67.6% vs. 49.5%, χ2 = 4.05, P < 0.05; Table 2). MSM respondents in Malindi who tested positive were less likely to be impoverished (4.2% vs. 15.3%, χ2 = 4.23, P < 0.05). Female respondents in Nanyuki who tested positive were more likely to be older (z = 4.10, P < 0.01), ever married (90.0% vs. 46.0%, χ2 = 7.04, P < 0.01), and to be patrons at the venues (100% vs. 64.3%, χ2 = 5.28, P < 0.05), while those in Malindi who tested positive were more likely to report multiple partners in the past 12 months (z = 2.40, P < 0.05), multiple new partners in the past 12 months (z = 2.04, P < 0.05), and to have exchanged sex for money in the past year (60.0% vs. 16.5%, χ2 = 10.87, P < 0.01; Table 3).
Conclusions
Findings from this study are both methodological and substantive. First we will discuss the methodological findings. Smith et al.[22] indicated the need for acceptable, valid and generalizable research methods to engage with stigmatized groups. Reporting of stigmatized behaviors is believed to be under-reported in household surveys.[10] The PLACE method is a community-based approach which has been used in over 60 studies. The methodology can be adapted to local context. In this study the community informants in Malindi were able to successfully identify venues were MSM and IDUs socialize as indicated by the high correlation between the informant reports and the self-identification. The MSM and IDU respondents did engage in the opportunity for prevention services as evidence by the high response rates for HIV testing. Interviewers in Malindi were familiar with the MSM and IDUs community and thus likely had some established rapport. Given the low access to prevention and treatment services among MSM and IDUs,[11] the PLACE method offers a means to successfully reach this population.
Can HIV testing work with a venue-based approach? Response rates were also high among the general population in Malindi (60.0%), and slightly lower in Rachuonyo (57.3%) and Nanyuki (47.8%). Thus HIV testing worked fairly well in urban Malindi and slightly less well in a rural district, Rachuonyo, and a small town, Nanyuki. Thus the strategy of including testing in a venue-based approach must be considered carefully. It could be that while the MSM and IDUs who have little access to services appreciated the opportunity to have VCT, individuals with more ready access to testing may not feel compelled to get tested, particularly when going out to socialize.
Approximately 78% of respondents in the current study had ever been tested for HIV, and prior testing did not predict willingness to be tested. The overall testing rate of 63% in our study was lower than the rate reported in the 2008–2009 Kenya DHS (83%), which found some differences in testing rates by province: Coast province had the highest rate of testing (89%), followed by Nyanza and Western provinces (86% each), while Central (77%) and North Eastern (71%) provinces had the lowest rates. In every province, women were more likely to be tested than men. Similar to the DHS, we found higher testing rates in the Coastal area (Malindi-General), followed by Nyanza (Rachuonyo) and Rift Valley (Nanyuki), and higher testing rates among women. The lower testing rates in the current study likely reflect methodological differences such as the unconventional provision of VCT at venues where people socialize, as mentioned above.
The PLACE method successfully captured individuals more likely to be HIV positive than individuals interviewed in the DHS. In previous comparisons to household studies, the PLACE method captured individuals who reported higher sexual risk behaviors.[4–6] The PLACE Kenya study is the first time it has been possible to compare HIV prevalence obtained from the PLACE approach versus a household survey.
In terms of substantive findings, there were several differences between those who tested positive and those who tested negative. Among males in Rachuonyo there was clearly a link between sexual risk behavior (partners in the past 4 weeks and 12 months) and HIV positive status, but this was seen neither in Nanyuki nor Malindi. The only significant finding for MSM in Malindi was poverty status, with those not impoverished more likely to be HIV positive. Among females in Nanyuki, those who were ever married and who were venue patrons were more likely to be HIV positive, and among females in Malindi there was also an association between sexual risk behaviors (partners and new partners in the past 12 months and transactional sex) and HIV positive status. Overall sexual risk behaviors were significant factors for the general population in Rachounyo and Malindi. In addition MSM and IDUs in Malindi had much higher HIV prevalence than the general population.
There are limitations to this study. Acceptance of VCT was relatively low among the general populations at each of the three sites, so future efforts to include HIV testing for the general population should be considered carefully. It is quite likely that there was some under-reporting of stigmatized behaviors, particularly for MSM and IDUs. However the relaxed nature of the interviews and the fact that they occur in a social environment with interviewers known to the MSM and IDUs, may have mitigated such bias. General limitations of the PLACE method are the possibility that some individuals avoid the interviewers and the possibility that community informants do not mention all key meeting places.
The PLACE is an effective tool for understanding local HIV epidemics. The methodology yields information about the highest risk individuals and the venues/events where they socialize. A key strategy is thus to place interventions at these venues/events to reach high risk individuals. The PLACE study in Kenya indicates that a venue-based strategy did work to reach MSM and IDUs with interventions. In the context of a human rights approach to combating HIV, this study offers hope in efforts to reach the most stigmatized individuals in addition to the general population at high risk.
Acknowledgments
Funding for this project was provided by the APHIA II Evaluation. The authors wish to thank all interviewers and study participants as well as Erica Haney for her assistance with the literature review.
References
- 1.Kenya National Bureau of Statistics and ICF Macro. Kenya Demographic and Health Survey 2008–09. Calverton, Maryland: 2010. [Google Scholar]
- 2.Garcia-Calleja JM, Gouws E, Ghys PD. National population based HIV prevalence surveys in sub-Saharan Africa: Results and implications for HIV and AIDS estimates. Sex Transm Infect. 2006 Jun;82:III64–III70. doi: 10.1136/sti.2006.019901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National AIDS Control Council. Kenya HIV Prevention Response and Modes of Transmission Analysis: Final Report. 2009. [Google Scholar]
- 4.Weir SS, Tate JE, Zhusupov B, Boerma JT. Where the action is: Monitoring local trends in sexual behaviour. Sex Transm Infect. 2004 Dec;80:63–8. doi: 10.1136/sti.2004.012336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tate J, Singh K, Ndubani P, Kamwanga J, Buckner B. Measurement of HIV prevention indicators: A comparison of the PLACE method and a household survey in Zambia. AIDS Behav. 2010;14(1):209–17. doi: 10.1007/s10461-008-9505-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Speizer IS, Beauvais H, Gomez AM, Outlaw TF, Roussel B. Using multiple sampling approaches to measure sexual risk-taking among young people in Haiti: Programmatic implications. Stud Fam Plan. 2009 Dec;40(4):277–88. doi: 10.1111/j.1728-4465.2009.00211.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.USAID/Kenya. HIV/AIDS Health Profile. 2010. Sep, [Google Scholar]
- 8.Human Rights Watch. Kenya: Halt Anti-Gay Campaign. Human Rights Watch. [press release] 2010 [cited February 1, 2011]; Available from: http://www.hrw.org/en/news/2010/02/17/kenya-halt-anti-gay-campaign.
- 9.Beyrer C, Wirtz AL, Baral S, Peryskina A, Sifakis F. Epidemiologic links between drug use and HIV epidemics: An international perspective. Jaids. 2009 Dec;55:S10–S6. doi: 10.1097/QAI.0b013e3181f9c0c9. [DOI] [PubMed] [Google Scholar]
- 10.Adam PCG, de Wit JBE, Toskin I, Mathers BM, Nashkhoev M, Zablotska I, et al. Estimating levels of HIV testing, HIV prevention coverage, HIV knowledge, and condom use among men who have sex with men (MSM) in low-income and middle-income countries. Jaids. 2009 Dec;52:S143–S51. doi: 10.1097/QAI.0b013e3181baf111. [DOI] [PubMed] [Google Scholar]
- 11.Global HIV Prevention Working Group. Bringing HIV Prevention to Scale: An Urgent Global Priority. Bill & Melinda Gates Foundation, Henry J. Kaiser Family Foundation; 2007. [Google Scholar]
- 12.Sanders EJ, Graham SM, Okuku HS, van der Elst EM, Muhaari A, Davies A, et al. HIV-1 infection in high risk men who have sex with men in Mombasa, Kenya. AIDS. 2007 Nov;21(18):2513–20. doi: 10.1097/QAD.0b013e3282f2704a. [DOI] [PubMed] [Google Scholar]
- 13.Wade AS, Kane CT, Diallo PAN, Diop AK, Gueye K, Mboup S, et al. HIV infection and sexually transmitted infections among men who have sex with men in Senegal. AIDS. 2005 Dec;19(18):2133–40. doi: 10.1097/01.aids.0000194128.97640.07. [DOI] [PubMed] [Google Scholar]
- 14.Baral S, Trapence G, Motimedi F, Umar E, Iipinge S, Dausab F, et al. HIV prevalence, risks for HIV infection, and human rights among men who have sex with men (MSM) in Malawi, Namibia, and Botswana. PLoS One. 2009 Mar;4(3) doi: 10.1371/journal.pone.0004997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Merrigan M, Azeez A, Afolabi B, Chabikuli ON, Onyekwena O, Eluwa G, et al. HIV prevalence and risk behaviours among men having sex with men in Nigeria. Sex Transm Infect. 2010 doi: 10.1136/sti.2008.034991. [DOI] [PubMed] [Google Scholar]
- 16.Dahoma M, Johnston L, Holman A, Miller L, Mussa M, Othman A, et al. HIV and related risk behavior among men who have sex with men in Zanzibar, Tanzania: Results of a behavioral surveillance survey. AIDS Behav. 2011;15(1):186–92. doi: 10.1007/s10461-009-9646-7. [DOI] [PubMed] [Google Scholar]
- 17.United Nations Office on Drug and Crime. Consensus Statement of the Reference Group to the United Nations on HIV and Injectign Drug Use. Vienna: 2010. [Google Scholar]
- 18.Needle RH, Kroegger K, Belani H, Hegle J. Substance abuse and HIV in sub-Saharan Africa: Introduction to the special issue. Afr, J Drug Alcol Stud. 2006;5:83–95. [Google Scholar]
- 19.Odek-Ogunde M, Okoth FA, Lore W, Owiti FR. Seroprevalence of HIV, HBC and HCV in Injecting Drug Users in Nairobi, Kenya. World Health Organization Drug Injecting Study Phase II Findings, 15th International AIDS Conference; Bangkok. 2004. [Google Scholar]
- 20.Deveau C, Levine B, Beckerleg S. Heroin use in Kenya and findings from a community based outreach programme to reduce the spread of HIV/AIDS. Afr J Drug Stud. 2006;5:95–107. [Google Scholar]
- 21.Singh K, Sambisa W, Munyati S, Chandiwana B, Chingono A, Monash R, et al. Targeting HIV interventions for adolescent girls and young women in southern Africa: Use of the PLACE methodology in Hwange District, Zimbabwe. AIDS Behav. 2010 Feb;14(1):200–8. doi: 10.1007/s10461-009-9572-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Smith AD, Tapsoba P, Peshu N, Sanders EJ, Jaffe HW. Men who have sex with men and HIV/AIDS in sub-Saharan Africa. Lancet. 2009 Aug;374(9687):416–22. doi: 10.1016/S0140-6736(09)61118-1. [DOI] [PubMed] [Google Scholar]