Abstract
With aging, women's bodies undergo changes that can affect body image perception, yet little is known about body image in midlife. The purpose of this study was to examine associations between body image and depressive symptoms in Caucasian and African–American midlife women from the Study of Women's Health Across the Nation (SWAN) Chicago site. Body image was measured using the Stunkard Adult Female Figure Rating Scale, and a clinically significant level of depressive symptoms was defined as Center for Epidemiologic Studies Depression Scale (CES-D) score of ≥16 (N=405; N=63 (15.6 %) with clinically significant levels of depressive symptoms). Differences between perceived actual, perceived ideal, and actual body size and responses to questions concerning weight satisfaction and attractiveness were examined using logistic regression for associations with a CES-D score of ≥16. Women with body image dissatisfaction (odds ratio (OR)=1.91; p=0.04) or who perceived themselves as “unattractive” (OR=7.74; p<0.01) had higher odds of CES-D of ≥16. We found no significant difference by race. Our results were not confounded by BMI. These results suggest that midlife women with poor body image may be more likely to have clinically significant levels of depressive symptoms. Larger prospective studies are needed to better understand this association.
Keywords: Body image, Body-type silhouettes, Depression, Midlife women, Race
Introduction
Body image is defined as “the picture we have in our minds of the size, shape, and form of our bodies” (Slade 1988). As women age, their bodies undergo dramatic changes (Sowers et al. 2007), and these changes can negatively affect their body image perception and satisfaction (Deeks 2004). In the past decades, however, the majority of published body image research on the associations between body image and depression has focused on adolescents, and little is known about the subject in midlife women. Current research has demonstrated associations between perceived weight status and depression in adolescents (Tang et al. 2010) and negative relationships between self-perceived weight and mental health status in adolescents, which were not found when examining actual weight alone (Ali, Fang and Rizzo 2010).
In the USA, up to 25 % of women have suffered from depression during their lifetimes (American Psychiatric Association 2000). Depression and depressive symptoms lead to reduced quality of life and productivity, including significantly lower physical functioning, social functioning, vitality, and overall mental health (Guajardo et al. 2011), as well as greater workplace absences and higher unemployment (Lerner and Henke 2008). Additionally, research has shown that depressive symptoms can lead to body image dissatisfaction (Marsella et al. 1981; Noles et al. 1985). However, the link between body image and depression in midlife is less well understood because little research has examined whether body image dissatisfaction contributes to depression among women from this age group. This is particularly relevant because the prevalence of depression is greatest in young and middle-aged adults and the prevalence of serious psychological distress (which includes symptoms of depression and anxiety) is greatest in middle-aged women (Reeves et al. 2011). Thus, it is important to assess if poor body image is associated with depressive symptoms in midlife women.
Body-type silhouettes have been used to assess body image, specifically differences in body weight perception and actual body weight (e.g., Bulik et al. 2001), as well as differences in actual and ideal body size (Lynch et al. 2007, 2009). The most widely used body-type scale is the Stunkard Adult Figure Rating Scale, which was developed originally for use with Caucasian populations (Stunkard et al. 1983; Sorensen et al. 1983). This scale is used to measure body image perception by examining the difference between perceived current and ideal body size. Individuals' figure selections have been found to be accurate proxy indicators of body mass index (BMI) in midlife women (Tehard et al. 2002) and, therefore, can be used to classify a woman's actual body size. Likewise, numerous studies examining body image perception and satisfaction concluded that body-type silhouettes were an appropriate tool for assessing body image satisfaction (Bulik et al. 2001; Fitzgibbon et al. 2000; Rand and Resnik 2000). These studies suggest that the differences between actual, perceived actual, and perceived ideal body size can be used as proxy measures of a woman's body image.
To our knowledge, no other study has examined the association of body image and depressive symptoms in midlife women or whether the associations differ in Caucasians versus African–American. The primary goal of this study was to examine the association between body image and depressive symptoms in a sample of midlife women in generally good health, using a multidimensional perspective of body image. We hypothesized that women with poor body image perception and satisfaction (measured as body image dissatisfaction, body image discordance, perceived unattractiveness, or weight dissatisfaction) are more likely to report clinically significant levels of depressive symptoms, independent of other factors associated with depression. As there are significant racial differences in depressive symptoms (e.g., Gazmararian et al. 1995) and in body image perception (Lynch et al. 2007; Chithambo and Huey 2013), we also examined whether the associations between body image and depressive symptoms differed in Caucasian and African–American women.
Methods
Participants and study design
The Study of Women's Health Across the Nation (SWAN) is a seven-site, multi-ethnic longitudinal study of women transitioning through menopause. The study design and recruitment have been described in detail previously (Sowers et al. 2000). Briefly, SWAN cohort eligibility criteria included being a woman aged 42–52 years, not pregnant or breastfeeding, having an intact uterus and at least one ovary, had menstruated within the past 3 months, and had not used sex steroid hormones in the past 3 months (Sowers et al. 2000). Participants completed self- and interviewer-administered questionnaires about psychosocial and lifestyle factors, health status, medical history and medication use, and menstrual status and symptoms at entry into the SWAN study and every year thereafter.
Participants for this cross-sectional analysis were 405 women (39.5 % African–American; 60.5 % Caucasian) from the Chicago SWAN site. The Chicago SWAN site featured a population-based design, which drew on a complete community census, and had a 72 % participation rate (Knight et al. 2010). By design, the Chicago site recruited only Caucasian and African–American women. Participants were recruited in such a way that allowed comparability on socioeconomic status within these two race/ethnic groups, thereby minimizing any confounding between race/ethnicity and socioeconomic status (Knight et al. 2010). The Chicago site's research protocol was fully approved by its Institutional Review Board, and the study was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. All women provided written informed consent prior to their inclusion in SWAN and at each study visit.
A self-report questionnaire, which included questions concerning body image and body-type silhouettes (Sorensen et al. 1983), was administered at the first annual follow-up assessment and only at the Chicago site. This self-administered questionnaire was completed by 420 (89.6 %) of the 469 women who received it. A higher percentage of women who completed the questionnaire were premenopausal, as compared with noncompleters, but no other significant differences were found between these two groups in the sample characteristics of age, BMI, hormone therapy use, marital status, education, financial strain, smoking, number of very upsetting life events, or percentage with Center for Epidemiologic Studies Depression Scale (CES-D) scores of ≥16. Of the 420 women who completed the questionnaire, participants with missing height or weight measurements, missing CES-D scores, or missing any data pertaining to body image (actual silhouette, ideal silhouette, perceived attractiveness score, and weight satisfaction score) were excluded (n=15, 3.6 %). The resulting 405 women (160 African–American; 245 Caucasian) formed the sample for our cross-sectional analysis. Compared with the 15 women excluded from the sample, these women did not differ in any of the characteristics reported in Table 1.
Table 1.
Characteristics of the sample, overall and by race
| Total | Caucasian | African American | ||
|---|---|---|---|---|
| n | 405 | 245 | 160 | |
| Age (years, mean (SD)) | 46.8 (2.9) | 46.7 (3.0) | 47.0 (2.8) | |
| BMI (kg/m2, mean (SD)) | 29.2 (6.4) | 28.2 (6.4) | 30.7 (6.1)* | |
| Menopausal status (n (%)) | Premenopausal | 140 (34.6 %) | 87 (35.5 %) | 53 (33.1 %) |
| Early perimenopausal | 197 (48.6 %) | 119 (48.6 %) | 78 (48.8 %) | |
| Late perimenopausal | 17 (4.2 %) | 9 (3.7 %) | 8 (5.0 %) | |
| Postmenopausal | 51 (12.6 %) | 30 (12.2 %) | 21 (13.1 %) | |
| Hormone therapy use (n (%)) | 34 (8.4 %) | 24 (9.8 %) | 10 (6.3 %) | |
| Unmarried (n (%))a | 111 (27.4 %) | 47 (19.2 %) | 64 (40.0 %)* | |
| Education≤high school (n (%)) | 43 (11.6 %) | 21 (9.3 %) | 22 (15.1 %) | |
| Financial strain (n (%)) | 132 (36.3 %) | 67 (30.3 %) | 65 (45.5 %)* | |
| Current smoker (n (%)) | 81 (20.7 %) | 46 (19.5 %) | 35 (22.6 %) | |
| Physical activity (n (%)) | Not active | 125 (30.9 %) | 65 (26.5 %) | 60 (37.5 %)* |
| Somewhat active | 211 (52.1 %) | 127 (51.8 %) | 84 (52.5 %) | |
| Vigorously active | 69 (17.0 %) | 53 (21.6 %) | 16 (10.0 %) | |
| Very upsetting life events | 0 events | 200 (51.0 %) | 123 (52.1 %) | 77 (49.4 %) |
| (n(%))b | 1 event | 85 (21.7 %) | 48 (20.4 %) | 37 (23.7 %) |
| 2+ events | 107 (27.3 %) | 65 (27.5 %) | 42 (26.9 %) | |
| Current CES-D≥16 (n (%)) | 63 (15.6 %) | 36 (14.7 %) | 27 (16.9 %) |
*p<0.05
Includes single, separated, widowed, and divorced
N=405 for all characteristics except very upsetting life events (N=392, due to missing data for 13 women)
Study measures
Depressive symptoms
Depressive symptoms were measured with the 20-item interviewer-administered CES-D, which assesses the frequency of being bothered by depressive symptoms in the past week on a scale from 0 (rarely) to 3 (most or all of the time) (Radloff 1977). Responses to the 20 items are summed for a total score ranging from 0 to 60. CES-D scores of 16 or higher indicate a high (and clinically significant) level of depressive symptoms (Weissman et al. 1977). The CES-D has been shown to be a valid and reliable measure of current symptoms in Caucasian and African-American populations (Roberts 1980).
Figure ratings
Figure ratings were obtained at the first annual follow-up using the Stunkard Adult Female Figure Rating Scale (Fig. 1), which consists of nine adult female silhouettes increasing in size from very thin (one) to very heavy (nine). Subjects were asked to “circle the number of the silhouette that looks most like you,” and “circle the number of the silhouette that best shows how you would like to look.” From these responses, we obtained the variables “perceived actual body size” and “perceived ideal body size,” respectively.
Fig. 1.
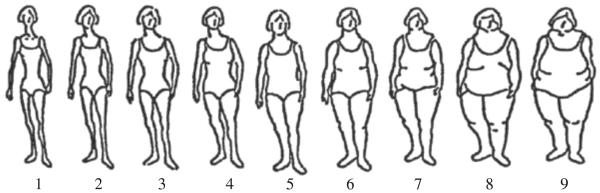
Adult Female Figure Rating Scale (Sorensen et al. 1983). Reprinted by permission from Macmillan Publishers Ltd: International Journal of Obesity (Sorensen et al. 1983), copyright 1983
The nine silhouettes were divided into three BMI strata: underweight (BMI, <20 kg/m2; silhouettes 1–3), normal/overweight (BMI, 20–30 kg/m2; silhouettes 4–6), and obese (BMI, >30 kg/m2; silhouettes 7–9), consistent with other studies of this type (Bulik et al. 2001). Using this categorization, each participant was placed into a stratum based on her calculated BMI (computed as weight in kilograms divided by height in meters squared) using height and weight measured with a stadiometer and a balance beam scale or electronic scale, respectively, at the first annual follow-up visit. From these measurements, we obtained the variable “actual body size.”
Body image dissatisfaction
Body image dissatisfaction was defined as perceived actual body size minus perceived ideal body size (Lynch et al. 2007, 2009). A score closer to 0 in either direction represents low body image dissatisfaction, whereas a score farther away from 0 in either direction represents high body image dissatisfaction. Subjects scoring 0 or ±1 were considered to be satisfied, and subjects scoring ±2 or more were considered to have body image dissatisfaction.
Body image discordance
Body image discordance was defined as perceived actual body size minus actual body size (Bulik et al. 2001). Each subject's perceived actual body size (that is, her silhouette choice for perceived actual body size) was placed into one of the three BMI categories corresponding to those created for actual body size (underweight, normal/overweight, and obese). Body image discordance was then generated by subtracting actual body size from perceived actual body size, forming three categories: perceived larger than actual (a difference of 1), perceived the same (a difference of 0), and perceived smaller than actual (a difference of −1). Subjects whose perceived body size was smaller or larger than actual were considered to have body image discordance.
Perceived attractiveness
Perceived attractiveness was defined as the response to the prompt, “Do you think your figure is: (1) attractive, (2) somewhat attractive, (3) somewhat unattractive, or (4) unattractive.”
Weight satisfaction
Weight satisfaction was defined as the response to the prompt, “How do you feel about your current weight?” Possible responses to this question were coded on a four-point scale: (1) satisfied, (2) somewhat satisfied, (3) somewhat dissatisfied, and (4) dissatisfied.
Covariates
Covariates were selected based on literature reporting their associations with depression and included age, current use of hormone therapy (yes or no), and current smoking status (yes or no). Number of very upsetting life events (categorized as 0, 1, or 2 or more events) was determined by women's responses to a checklist of 18 possible life events that might have occurred. Women indicated whether the event occurred and, if so, how upsetting it was (not at all, somewhat upsetting, very upsetting) (Bromberger et al. 2013). Current marital status was defined as either “married” (including currently married and living as married) or “unmarried” (including single, widowed, divorced, and separated). Highest level of education was dichotomized as “education≤high school” and “any education post high school”. Level of physical activity was assessed using an adapted version of the Kaiser Physical Activity Survey (KPAS) (Sternfeld et al. 1999; Ainsworth et al. 2000) and categorized as either “not active,” “somewhat active,” or “vigorously active.” Financial strain was assessed with a three-level item indicating difficulty in paying for necessities (i.e., food, housing, and medical care) and was dichotomized as “somewhat or very hard” versus “not hard at all.” Menopausal status was categorized based on menstrual bleeding criteria as “premenopausal” (no change in menstrual bleeding regularity), “early perimenopausal” (menses in the preceding 3 months with an increase in bleeding irregularity), “late perimenopausal” (menses in the previous 12 months, but not the previous 3 months), or “postmenopausal” (≥12 months of amenorrhea) (World Health Organization Scientific Group 1996).
Data analysis
Participant characteristics were summarized using mean (SD) for continuous variables and N (%) for categorical variables for the overall cohort and by race. The distribution of all continuous variables was checked for skewness. Group differences were tested using t tests for continuous variables and chi-squared tests for categorical variables. The proportion of subjects in each race that selected each figure size was calculated for both perceived actual body size and perceived ideal body size. Validity and correlation of body image variables were assessed using Spearman correlation coefficients for categorical variables.
The relations between each body image variable and clinically significant levels of depressive symptoms (CES-D, ≥16) were then tested individually using three distinct logistic regression models (unadjusted, partially adjusted, and fully adjusted) and are presented as odds ratios (OR) for CES-D scores of ≥16. Age, marital status, menopausal status, and race were included in all partially adjusted models because of their established associations with depression in midlife women (Llaneza et al. 2012; Freeman et al. 2004; Soares 2007). Additional covariates were selected for fully adjusted analyses from associations with both CES-D score of ≥16 and body image variable at p≤0.2 (Hosmer and Lemshow 2000). For this reason, all four fully adjusted models may not contain the same covariates. To examine whether the associations of body image satisfaction, body image discordance, perceived attractiveness, and weight satisfaction with a clinically significant level of depressive symptoms differed by race, each of the four fully adjusted logistic regression models were reanalyzed to include an interaction term of race with the body image variable.
Although consistent with other figure rating studies (e.g., Bulik et al. 2001), the BMI cut-points used in these analyses differed from the standard cut-points (National Heart, Lung, and Blood Institute 1998). Therefore, we conducted a sensitivity analysis to assess the validity of our chosen cut-points. After removing women with BMI near the cut-point between underweight and normal weight and between overweight and obese (that is, women with BMI between 19 and 21 or between 29 and 31), the body image discordance regression models were reanalyzed using the smaller sample.
Lastly, to examine whether the BMI component of body image may be driving the association between body image and clinically significant levels of depressive symptoms, we compared the mean BMI in the depressed and nondepressed groups, using a two sample t test for the difference. If no significant difference between the two groups is found, it is not likely that the association between body image and depressive symptoms is due to BMI.
SAS 9.1 (SAS Institute, Cary, NC) was used to perform all statistical analyses and assumption checks. For all models, two-sided p values <0.05 were considered statistically significant.
Results
Sample characteristics
Table 1 shows the characteristics of the cohort overall and by race. African–American participants had a higher mean BMI, and higher percentages reported being currently unmarried, not physically active, and experiencing financial strain compared with Caucasians, whereas a larger percentage of Caucasians reported being vigorously active. No other differences were detected between the two groups. Overall, 15.6 % (n=63) of the sample had a current CES-D score of ≥16, with no significant difference by race.
Body image interrelationships and distributions
Body image satisfaction was significantly positively correlated with perceived attractiveness (r=0.51; p<0.0001) and weight satisfaction (r=0.54; p<0.0001). Perceived attractiveness and weight satisfaction were also positively correlated (r=0.62; p<0.0001). Body image discordance was not significantly correlated with any of the other three body image variables (r=−0.08–0.08; p≥0.11).
Table 2 shows the distributions of actual, perceived actual, and perceived ideal body size. There was a statistically significant difference in actual body size by race when examined by BMI category. The actual body size of half of the African–American women, compared with only a third of the Caucasian women, was in the “obese” category (p<0.01). There was no statistically significant racial difference for either the perceived actual silhouette or the perceived ideal silhouette. The majority of women selected perceived actual silhouette 4 or 5 from Fig. 1. Less variability was observed for responses to their perceived ideal silhouette than to their perceived actual silhouette. Over half of both Caucasian and African–American women selected silhouette 3 as their ideal. No woman selected an ideal silhouette from the “obese” category, and only 11 % perceived themselves as such (i.e., silhouettes 7–9). Among women categorized as “obese” (BMI, >30; n=164), 69.1 % of Caucasian women and 81.3 % of African–American women perceived themselves as normal or overweight; however, no statistically significant difference between the races was found (p=0.07).
Table 2.
Distribution of actual and perceived body size overall and by race
| Body size | Overall (n=405) | Caucasian (n=245) | African–American (n=160) | |
|---|---|---|---|---|
| Actuala | Underweight | 8 (2.0 %) | 7 (2.9 %) | 1 (0.6 %) |
| Normal/overweight | 233 (57.5 %) | 154 (62.9 %) | 79 (49.4 %) | |
| Obese | 164 (40.5 %) | 84 (34.3 %) | 80 (50.0 %) | |
| Perceived actualb | Underweight | 69 (17.0 %) | 43 (17.6 %) | 26 (16.3 %) |
| Normal/overweight | 291 (71.9 %) | 173 (70.6 %) | 118 (73.8 %) | |
| Obese | 45 (11.1 %) | 29 (11.8 %) | 16 (10.0 %) | |
| Perceived idealc | Underweight | 284 (70.1 %) | 177 (72.2 %) | 107 (66.9 %) |
| Normal/overweight | 121 (29.9 %) | 68 (27.8 %) | 53 (33.1 %) | |
| Obese | 0 (0 %) | 0 (0 %) | 0 (0 %) |
χ2 =11.4; df=2; p<0.01
χ2 =0.52; df=2; p=0.77
χ2 =1.09; df=1; p=0.30
Table 3 shows the distribution of body image dissatisfaction and discordance, perceived attractiveness, and weight satisfaction for the cohort as a whole and by race. Overall, 52.8 % of the participants were satisfied with their body image; that is, they selected a perceived ideal silhouette within one figure of their perceived actual silhouette. Body image dissatisfaction did not differ by race. Only five participants perceived their actual silhouette as larger than their actual body size based on BMI; these participants were removed from the body image discordance analysis due to their small numbers, and therefore body image discordance is only a measure of “perceived body image smaller than actual.” African–American women were more likely than Caucasian women to have a perceived body image smaller than actual (p<0.001). Overall, 61.2 % of the women believed their figure to be “somewhat attractive” (51.6 %) or “attractive” (9.6 %). No significant difference in perceived attractiveness was found between races. The majority of women (73.3 %) were “somewhat unsatisfied” or “unsatisfied” with their weight, and there was no significant difference in body weight satisfaction between races.
Table 3.
Body image variables, overall and by race
| Overall (N (%))a | Caucasian (N (%)) | African–American (N (%)) | p value | |
|---|---|---|---|---|
| Body image dissatisfaction | ||||
| Satisfied | 214 (52.8 %) | 130 (53.1 %) | 84 (52.5 %) | 0.91 |
| Dissatisfied | 191 (47.2 %) | 115 (46.9 %) | 76 (47.5 %) | |
| Body image discordance | ||||
| Perceived same | 215 (53.8 %) | 146 (60.6 %) | 69 (43.4 %)* | <0.001 |
| Perceived smaller than actual | 185 (46.2 %) | 95 (39.4 %) | 90 (56.6 %)* | |
| Perceived attractiveness | ||||
| Attractive | 39 (9.6 %) | 21 (8.6 %) | 18 (11.3 %) | 0.14 |
| Somewhat attractive | 209 (51.6 %) | 118 (48.2 %) | 91 (56.9 %) | |
| Somewhat unattractive | 103 (25.4 %) | 70 (28.6 %) | 33 (20.6 %) | |
| Unattractive | 54 (13.3 %) | 36 (14.7 %) | 18 (11.3 %) | |
| Weight satisfaction | ||||
| Satisfied | 35 (8.6 %) | 20 (8.2 %) | 15 (9.4 %) | 0.67 |
| Somewhat satisfied | 73 (18.0 %) | 46 (18.8 %) | 27 (16.9 %) | |
| Somewhat unsatisfied | 180 (44.4 %) | 104 (42.5 %) | 76 (47.5 %) | |
| Unsatisfied | 117 (28.9 %) | 75 (30.6 %) | 42 (26.3 %) |
p<0.05
N=405 for all analyses except body image discordance (N=400; see text for details)
Multivariate analyses
Table 4 shows the results of the logistic regression OR relating each of the four body image measures to clinically significant levels of depressive symptoms.
Table 4.
Odds ratios (and 95 % confidence intervals) for clinically significant depressive symptoms (CES-D, ≥16) by body image variables
| Overall (N) | Subjects with CES-D of ≥16 (N (%)) | Unadjusted | Partially adjusteda | Fully adjusted | |
|---|---|---|---|---|---|
| Body image dissatisfactionb | |||||
| Satisfied | 214 | 26 (12.2 %) | Reference | Reference | Reference |
| Dissatisfied | 191 | 37 (19.4 %) | 1.73 (1.01, 3.00)* | 1.89 (1.09, 3.31)* | 1.91 (1.05, 3.48)* |
| Body image discordancec | |||||
| No discordance | 215 | 41 (19.1 %) | Reference | Reference | Reference |
| Discordance | 185 | 22 (11.9 %) | 0.57 (0.33, 1.00) | 0.59 (0.33, 1.06) | 0.59 (0.33, 1.06) |
| Perceived attractivenessd | |||||
| Attractive | 39 | 4 (10.3 %) | Reference | Reference | Reference |
| Somewhat attractive | 209 | 29 (13.9 %) | 1.41 (0.47, 4.26) | 1.41 (0.46, 4.32) | 2.31 (0.60, 8.89) |
| Somewhat unattractive | 103 | 13 (12.6 %) | 1.26 (0.39, 4.14) | 1.35 (0.41, 4.51) | 1.90 (0.45, 8.03) |
| Unattractive | 54 | 17 (31.5 %) | 4.02 (1.23, 13.13)* | 4.36 (1.31, 14.47)* | 7.74 (1.84, 32.57)** |
| Weight satisfactione | |||||
| Satisfied | 35 | 1 (2.9 %) | Reference | Reference | Reference |
| Somewhat satisfied | 73 | 9 (12.3 %) | 4.78 (0.58, 39.31) | 5.13 (0.62, 42.68) | 4.18 (0.49, 35.30) |
| Somewhat dissatisfied | 180 | 30 (16.7 %) | 6.79 (0.90, 51.57) | 7.18 (0.94, 54.90) | 5.70 (0.73, 44.26) |
| Dissatisfied | 117 | 23 (19.7 %) | 8.32 (1.08, 63.94)* | 8.67 (1.12, 67.21)* | 5.91 (0.75, 46.84) |
p<0.05;
p<0.01
All partially adjusted models are adjusted for age, marital status, menopausal status, and race
Fully adjusted model includes age, marital status, menopausal status, and race, plus financial strain and physical activity
Fully adjusted model includes age, marital status, menopausal status, and race (no additional covariates entered)
Fully adjusted model includes age, marital status, menopausal status, and race, plus financial strain and physical activity
Fully adjusted model (N=392) includes age, marital status, menopausal status, and race, plus number of upsetting life events and physical activity
Body image dissatisfaction
In the fully adjusted logistic regression model (adjusted for age, marital status, menopausal status, race, financial strain, and physical activity), women with body image dissatisfaction, compared with those who were satisfied with their body image, were nearly twice as likely to report clinically significant levels of depressive symptoms (OR=1.91 (95 % confidence interval (CI), 1.05, 3.48); p=0.04).
Body image discordance
The body image discordance association with depressive symptoms was not statistically significant in any model.
Perceived attractiveness
Perceived attractiveness was significantly associated with clinically significant levels of depressive symptoms in women responding “unattractive.” In the fully adjusted model (adjusted for age, marital status, menopausal status, race, financial strain, and physical activity), women reporting an “unattractive” figure had a higher odds of reporting clinically significant levels of depressive symptoms than did women reporting an “attractive” figure (OR=7.74 (95 % CI, 1.84, 32.57); p<0.01).
Weight satisfaction
Both the unadjusted and partially adjusted models for weight satisfaction indicated that weight satisfaction was significantly associated with having clinically significant levels of depressive symptoms. Adding “number of upsetting life events” to the fully adjusted model (adjusted for age, marital status, menopausal status, race, number of upsetting life events, and physical activity) attenuated the magnitude of the OR for women who were “dissatisfied” with their weight compared with those who were “satisfied,” and the association between weight satisfaction and CES-D score of ≥16 no longer was statistically significant in the fully adjusted model (OR=5.91 (95 % CI, 0.75, 46.84); p=0.09).
Race interactions
Multivariate analyses adding the race interaction term to the fully adjusted model indicated that race did not significantly moderate the associations between the body image variables (body image dissatisfaction or discordance, perceived attractiveness, or weight dissatisfaction) and clinically significant levels of depressive symptoms (p=0.58, 0.95, 0.30, and 0.24, respectively; data not shown).
Additional analyses
To assess the validity of our BMI and silhouette cut-points, we removed the 64 women with BMI between 19 and 21 (n=23) or between 29 and 31 (n=41) and reanalyzed the association between body image discordance and clinically significant levels of depressive symptoms as a sensitivity analysis. The results obtained after removing the 64 women with borderline BMI were no different than those obtained using the entire sample. This indicates that women on the border between these two silhouette categories did not significantly affect the associations between body image discordance and clinically significant levels of depressive symptoms. Similarly, the two-sample t test for difference in mean BMI by depression group (i.e., CES-D, ≥16; yes/no) indicated that BMI did not differ significantly between the two groups (p=0.24), which suggests that our results are not confounded by BMI. We, therefore, did not include BMI as a covariate in the analysis to avoid over-adjusting for BMI; as BMI is a component of a woman's body image, it is already included in the models as part of each predictor variable.
Discussion
To our knowledge, this is the first study exploring the relationship between body image and depression in both Caucasian and African–American midlife women. As hypothesized, women with body image dissatisfaction were more likely to report a clinically significant level of depressive symptoms, as did women who reported feeling unattractive. Although the confidence interval around the OR for perceived attractiveness is wide, this lack of precision is likely due to the small number of women reporting feeling “unattractive,” and our results still suggest an association between feeling unattractive and reporting clinically significant levels of depressive symptoms. Our findings are consistent with studies involving adolescents and young adults (Tang et al. 2010; Ali et al. 2010; Stice et al. 2000).
Although the magnitude of the OR point estimate (OR=5.91) was high for the association of weight dissatisfaction on clinically significant levels of depressive symptoms, our results lack precision, and therefore we found no significant support for our hypotheses that women with weight dissatisfaction would also report clinically significant levels of depressive symptoms. The addition of negative life events as a covariate into the fully adjusted model attenuated the OR for women who were “dissatisfied” with their weight compared with those who were “satisfied.” As stated in the “Data analysis,” we selected covariates for the fully adjusted model based on significant associations with depression and body image variable at p≤0.2. A significant association between a body image variable and negative life events was only found for weight satisfaction (p=0.17). One possible explanation could be that our significant findings exist between the two most extreme categories of variables. Therefore, the fact that negative life events attenuated the weight satisfaction model may be due to the difference between extreme groups.
There was no support for the hypothesis that women with body image discordance would also report clinically significant levels of depressive symptoms. On the contrary, women with body image discordance (i.e., those with a perceived actual silhouette smaller than actual) were less likely to report high CES-D scores; this finding, however, was not statistically significant (see Table 4). The concept of “depressive realism,” which states that depressed persons lose the positive bias that allows them to see themselves in an unjustifiably positive light (Moore and Fresco 2012), suggests that depressed women would also experience less body image discordance (that is, they would not perceive their body size to be smaller than actual). This concept could explain why women with body image discordance also reported lower levels of depressive symptoms. A possible explanation for the lack of significance is that the overall majority of women in our study did not experience body image discordance (i.e., their perceptions were concordant with their actual body sizes). As each of the nine silhouettes are not assigned a specific BMI, we were only able to detect body image discordance when a subject perceived her body size to be in a different BMI category than her actual body size. The categorization of silhouettes into three BMI categories (as opposed to using all nine silhouettes) may not have allowed for the precision in measurement necessary to detect an actual difference in level of depressive symptoms.
Although the overall majority of women did not experience body image discordance, we did find that, consistent with previous studies, African–American women were more likely than Caucasians to perceive their body size as smaller than actual. In the USA, the proportion of African–American women who are overweight or obese is much higher compared with Caucasian women (CDC 2009), a difference which we also saw in our sample. Through social comparison to other women of the same race, African–American women may perceive themselves as having a smaller body size than women of races/ethnicities in which the prevalence of obesity is lower (Bennett and Wolin 2006). This difference could also be related to the fact that African–American women, on average, have a higher proportion of fat-free body mass for a given BMI than do Caucasian women (Wagner and Heyward 2000; Evans et al. 2006). Thus, an African–American woman with a given BMI will generally have a lower percentage of body fat than a Caucasian woman with the same BMI. Although ethnic/racial differences in body composition are on the order of 1–3 BMI points for a given percentage body fat (Deurenberg et al. 1998), it may partially account for higher body image discordance in African–American women. The two race groups did not differ significantly in body image dissatisfaction, perceived attractiveness, or weight satisfaction.
While the SWAN cohort comprises a relatively large number of both Caucasian and African–American midlife women, one limitation of our study was having only a small sample of women in each body image group of interest. Although large enough to detect differences when examining body image satisfaction and perceived attractiveness, our sample was not large enough to detect differences between our other two predictors, body image discordance and weight satisfaction, while still controlling for covariates. Grouping the women into two categories instead of four would allow for more balanced groups and therefore could alleviate the issue of small sample sizes; however, this grouping reduces the distinction between the most extreme groups, and therefore reduces the ability to detect associations with clinically significant levels of depressive symptoms (see Table 4). Additionally, our sample size did not allow us to detect differential race effects in body image perceptions. Lastly, because we had only five women who perceived their body size to be larger than actual, we eliminated them from the analysis involving body image discordance, as they would not contribute meaningful results and would produce unstable estimates. However, women perceiving their body size to be larger than actual could provide additional insight into the relationship that body image discordance may have on depressive symptoms.
Another possible limitation of our study concerns the validity of the Stunkard Adult Female Figure Rating Scale (Stunkard et al. 1983; Sorensen et al. 1983) as an accurate measure of a woman's actual or perceived body size. The silhouettes represent generalized versions of a woman's figure, and do not address individual areas of her body that could be large or small. Tehard et al. (2002) examined how well silhouette choice corresponded with actual body size (i.e., BMI) and found that this scale could most accurately predict BMI when used with normal weight women. Our sample consisted of more women with an actual body size in the obese category (40.5 %) and fewer in the normal/overweight category (57.5 %) than reported in the general population of American women (CDC 2012; NHANES 2003). The mean BMI in our sample was 29.2, which is well over the traditional cut-point for normal weight, and on the border between over-weight and obese. However, in our sample, BMI was highly correlated with perceived actual silhouette choice (r=0.78; r= 0.83, Caucasians only; r=0.72 African–Americans only; p<0.001 for all), which suggests that a woman's actual silhouette is an accurate measure of actual body size. Another concern is that, because the Stunkard scale was originally developed for use in Caucasian populations, it may not be valid when used with African–Americans. However, it has been found that, when compared with other scales generated for use in African–American populations, the Stunkard scale performed similarly (Patt et al. 2002).
Additionally, our choice of BMI cut-points did not allow us to separate normal weight and overweight women or to measure body image discordance between those two groups. To our knowledge, cut-points distinguishing between normal and overweight BMI categories have not been validated for midlife women. Future studies should consider determining valid cut-points between these BMI categories, as examining associations between discordance and depression separately in normal weight and overweight women could provide additional insight.
Gardner (1996) expressed concern over the limited number of responses a woman could choose as her perceived actual body size, which could force her to choose between silhouettes of different categories. We addressed this concern with a sensitivity analysis, which indicated that women forced to choose between silhouettes bordering different BMI categories did not significantly affect the model results.
Lastly, this was a cross-sectional analysis, and therefore we cannot conclude that low body image causes high levels of depressive symptoms. In fact, the association could be in the opposite direction or be bidirectional. Longitudinal research is needed to examine the temporal relationship between body image and depression.
A major strength of our study was the ability to consider a multidimentional perspective of body image. Body image is a multifaceted construct that can be difficult to assess (Thompson 2004), and multiple measurement techniques should be applied to better explore these multiple dimensions (Garner et al. 1987). We considered body image through both use of the Stunkard Adult Female Figure Rating Scale and women's answers to specific body image questions, allowing us to examine multiple aspects of body image and their associations with depressive symptoms. The SWAN study is a large epidemiologic study that crosses multiple disciplines, and time did not permit the addition of a full length body image assessment. Single-item measures cannot be validated for internal consistency (Thompson 2004), and future studies using a validated full assessment of body image, such as the Body Image Ideals Questionnaire (Cash and Szymanski 1995), could provide further verification of the association between body image and depression. However, the positive correlations among body image variables suggest that our question selection does provide a valid proxy for body image satisfaction. Body image satisfaction, perceived attractiveness, and weight satisfaction were moderately correlated; this level of correlation is to be expected, as each variable measures a similar yet distinct aspect of a woman's overall body image. We found no correlation between body image discordance and any of our other body image variables; this is likely because body image discordance measures the discrepancy between perception and reality, whereas the other variables each measure the satisfaction of that perception.
Another strength of this study is its ability to examine how aging women's perception of their bodies is related to their mental health. Additionally, this study used the CES-D scores to assess depression, which is a well validated assessment of depressive symptoms for women of all ages, including midlife women (Radloff 1977; Knight et al. 1997). The 16 % prevalence of clinically significant levels of depressive symptoms in our study indicates that this outcome is not rare, and therefore it is important to examine its correlates. Little is known about the relationship between body image satisfaction and depression in this age group, yet our data suggest that it has potential clinical relevance and should be considered when treating midlife women with depressive symptoms.
In summary, we observed that body image dissatisfaction and perceived unattractiveness were associated with clinically significant levels of depressive symptoms in midlife women. These results suggest that poor body image may be related to depressive symptoms. This relationship has potentially important clinical relevance, especially because little is known about this relationship in midlife women. Further investigation, however, is necessary to determine whether race modifies this association and to explore the directionality. Longitudinal analyses could examine both the directionality and the long-term effects of body image on depressive symptoms, as well as the effect of perceived change in body size during the menopausal transition on body image satisfaction and depressive symptoms.
Acknowledgement
The SWAN has grant support from the National Institutes of Health (NIH), DHHS, through the National Institute on Aging (NIA), the National Institute of Nursing Research (NINR), and the NIH Office of Research on Women's Health (ORWH; grants U01NR004061, U01AG012505, U01AG012535, U01AG012531, U01AG012539, U01AG012546, U01AG012553, U01AG012554, and U01AG012495). The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the NIA, NINR, ORWH, or the NIH.
Footnotes
Publisher's Disclaimer: Your article is protected by copyright and all rights are held exclusively by Springer-Verlag Wien. This e-offprint is for personaluse only and shall not be self-archived in electronic repositories. If you wish to self-archive your article, please use the accepted manuscript version for posting on your own website. You may further deposit the accepted manuscript version in any repository, provided it is only made publicly available 12 months after official publication or later and provided acknowledgement is given to the original source of publication and a link is inserted to the published article on Springer's website. The link must be accompanied by the following text: “The final publication is available at link.springer.com”.
Conflict of interest statement The authors have no financial relationship with the NIH, which funded the study (see Acknowledgements) and declare that they have no conflict of interest.
References
- Ainsworth BE, Sternfeld B, Richardson MT, et al. Evaluation of the Kaiser Physical Activity Survey in women. Med Sci Sports Exerc. 2000;32:1327–1338. doi: 10.1097/00005768-200007000-00022. [DOI] [PubMed] [Google Scholar]
- Ali MM, Fang H, Rizzo JA. Body weight, self-perception and mental health outcomes among adolescents. J Ment Health Policy Econ. 2010;13:53–63. [PubMed] [Google Scholar]
- American Psychiatric Association . American Psychiatric Association: Diagnostic and Statistical Manual of Mental Disorders Fourth Edition, Text Revision. American Psychiatric Association; Washington, DC: 2000. [Google Scholar]
- Bennett GG, Wolin KY. Satisfied or unaware? Racial differences in perceived weight status [electronic article] Int J Behav Nutr Phys Act. 2006;3:40. doi: 10.1186/1479-5868-3-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bromberger JT, Kravitz HM, Chang Y, et al. Does risk for anxiety increase during the menopausal transition? Study of Women's Health Across the Nation. Menopause. 2013;20:488–495. doi: 10.1097/GME.0b013e3182730599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bulik CM, Wade TD, Heath AC, et al. Relating body mass index to figural stimuli: population-based normative data for Caucasians. Int J Obes Relat Metab Disord. 2001;25:1517–1524. doi: 10.1038/sj.ijo.0801742. [DOI] [PubMed] [Google Scholar]
- Cash TF, Szymanski ML. The development and validation of the body-image ideals questionnaire. J Pers Assess. 1995;46:466–477. doi: 10.1207/s15327752jpa6403_6. [DOI] [PubMed] [Google Scholar]
- CDC Differences in prevalence of obesity among black, white, and Hispanic adults—United States, 2006–2008. MMWR. 2009;58:740–744. [PubMed] [Google Scholar]
- CDC [Accessed 22 January 2014];NCHS Fact Sheet-NCHS Data on obesity. 2012 http://www.cdc.gov/nchs/data/factsheets/factsheet_obesity.htm.
- Chithambo TP, Huey SJ. Black/white differences in perceived weight and attractiveness among overweight women. J Obes. 2013;2013:1–4. doi: 10.1155/2013/320326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deeks AA. Is this menopause? Women in midlife—psychosocial issues. Aust Fam Physician. 2004;33:889–893. [PubMed] [Google Scholar]
- Deurenberg P, Yap M, van Staveren WA. Body mass index and percent body fat: a meta analysis among different ethnic groups. Int J Obes Relat Metab Disord. 1998;22:1164–1171. doi: 10.1038/sj.ijo.0800741. [DOI] [PubMed] [Google Scholar]
- Evans EM, Rowe DA, Racette SB, et al. Is the current BMI obesity classification appropriate for black and white postmenopausal women? Int J Obes (Lond) 2006;30:837–843. doi: 10.1038/sj.ijo.0803208. [DOI] [PubMed] [Google Scholar]
- Fitzgibbon ML, Blackman LR, Avellone ME. The relationship between body image discrepancy and body mass index across ethnic groups. Obes Res. 2000;8:582–589. doi: 10.1038/oby.2000.75. [DOI] [PubMed] [Google Scholar]
- Freeman EW, Sammel MD, Liu L, et al. Hormones and menopausal status as predictors of depression in women in transition to menopause. Arch Gen Psychiatry. 2004;61:62–70. doi: 10.1001/archpsyc.61.1.62. [DOI] [PubMed] [Google Scholar]
- Gardner RM. Methodological issues in assessment of the perceptual component of body image disturbance. Br J Psychol. 1996;87:327–337. doi: 10.1111/j.2044-8295.1996.tb02593.x. [DOI] [PubMed] [Google Scholar]
- Garner DM, Garfinkel PE, Bonato DP. Body image measurement in eating disorders. Adv Psychosom Med. 1987;17:119–133. doi: 10.1159/000414010. [DOI] [PubMed] [Google Scholar]
- Gazmararian JA, James SA, Lepkowski JM. Depression in black and white women. The role of marriage and socioeconomic status. Ann Epidemiol. 1995;5:455–463. doi: 10.1016/1047-2797(95)00061-5. [DOI] [PubMed] [Google Scholar]
- Guajardo VD, Souza BP, Henriques SG, et al. Loss of interest, depressed mood and impact on the quality of life: cross-sectional survey. BMC Public Health. 2011;11:826. doi: 10.1186/1471-2458-11-826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hosmer DW, Lemshow S. Applied logistic regression. 2nd edn John Wiley & Sons Inc; New York, NY: 2000. [Google Scholar]
- Knight JM, Avery EF, Janssen I, et al. Cortisol and depressive symptoms in a population-based cohort of midlife women. Psychosom Med. 2010;72:855–861. doi: 10.1097/PSY.0b013e3181f4ab87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knight RG, Williams S, Mcgee R, et al. Psychometric properties of the Centre for Epidemiologic Studies Depression Scale (CES-D) in a sample of women in middle life. Behav Res Ther. 1997;35:373–380. doi: 10.1016/s0005-7967(96)00107-6. [DOI] [PubMed] [Google Scholar]
- Lerner D, Henke RM. What does research tell us about depression, job performance, and work productivity? J Occup Environ Med. 2008;50:401–410. doi: 10.1097/JOM.0b013e31816bae50. [DOI] [PubMed] [Google Scholar]
- Llaneza P, Garcia-Portilla MP, Llaneza-Suarez D, et al. Depressive disorders and the menopause transition. Maturitas. 2012;71:120–130. doi: 10.1016/j.maturitas.2011.11.017. [DOI] [PubMed] [Google Scholar]
- Lynch E, Liu K, Spring B, et al. Association of ethnicity and socioeconomic status with judgments of body size: the Coronary Artery Risk Development in Young Adults (CARDIA) study. Am J Epidemiol. 2007;165:1055–1062. doi: 10.1093/aje/kwk114. [DOI] [PubMed] [Google Scholar]
- Lynch E, Liu K, Wei GS, et al. The relation between body size perception and change in body mass index over 13 years: the Coronary Artery Risk Development in Young Adults (CARDIA) study. Am J Epidemiol. 2009;169:857–866. doi: 10.1093/aje/kwn412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marsella AJ, Shizuru L, Brennan J, et al. Depression and body image satisfaction. J Cross-Cult Psychol. 1981;12:360–371. [Google Scholar]
- Moore MT, Fresco DM. Depressive realism: a meta-analytic review. Clin Psychol Rev. 2012;32:496–509. doi: 10.1016/j.cpr.2012.05.004. [DOI] [PubMed] [Google Scholar]
- National Heart, Lung, and Blood Institute . Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report. National Institutes of Health; Bethesda, MD: 1998. [PubMed] [Google Scholar]
- NHANES [Accessed 22 January 2014];Healthy weight, overweight, and obesity among U.S. adults. 2003 http://www.cdc.gov/nchs/data/nhanes/databriefs/adultweight.pdf.
- Noles SW, Cash TF, Winstead BA. Body image, physical attractiveness, and depression. J Consult Clin Psych. 1985;53:88–94. doi: 10.1037//0022-006x.53.1.88. [DOI] [PubMed] [Google Scholar]
- Patt MR, Lane AE, Finney CP, et al. Body image assessment: comparison of figure rating scales among urban Black women. Ethn Dis. 2002;12:54–62. [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- Rand CS, Resnik JL. The “good enough” body size as judged by people of varying age and weight. Obes Res. 2000;8:309–316. doi: 10.1038/oby.2000.37. [DOI] [PubMed] [Google Scholar]
- Reeves WC, Strine TW, Pratt LA, et al. Mental illness surveillance among adults in the United States. MMWR Surveill Summ. 2011;60:1–29. [PubMed] [Google Scholar]
- Roberts RE. Reliability of the CES-D scale in different ethnic contexts. Psychiatr Res. 1980;2:125–134. doi: 10.1016/0165-1781(80)90069-4. [DOI] [PubMed] [Google Scholar]
- Slade PD. Body image in anorexia nervosa. Br J Psychiatry Suppl. 1988;153:20–22. [PubMed] [Google Scholar]
- Soares CN. Menopausal transition and depression: who is at risk and how to treat it? Expert Rev Neurother. 2007;7:1285–1293. doi: 10.1586/14737175.7.10.1285. [DOI] [PubMed] [Google Scholar]
- Sorensen TI, Stunkard AJ, Teasdale TW, et al. The accuracy of reports of weight: children's recall of their parents' weights 15 years earlier. Int J Obes. 1983;7:115–122. [PubMed] [Google Scholar]
- Sowers MF, Crawford SL, Sternfeld B, et al. SWAN: a multi-center, multi-ethnic, community-based cohort study of women and the menopause. In: Lobo R, Kelsey J, Marcus R, editors. Menopause: biology and pathobiology. Academic Press; San Diego, CA: 2000. pp. 175–188. [Google Scholar]
- Sowers MF, Zheng H, Tomey K, et al. Changes in body composition in women over six years at midlife: ovarian and chronological aging. J Clin Endocrinol Metab. 2007;92:895–901. doi: 10.1210/jc.2006-1393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stemfeld B, Ainsworth BE, Quesenberry CP. Physical activity patterns in a diverse population of women. Prev Med. 1999;28:313–323. doi: 10.1006/pmed.1998.0470. [DOI] [PubMed] [Google Scholar]
- Stice E, Hayward C, Cameron RP, et al. Body-image and eating disturbances predict onset of depression among female adolescents: a longitudinal study. J Abnorm Psychol. 2000;109:438–444. [PubMed] [Google Scholar]
- Stunkard AJ, Sorensen T, Schulsinger F. Use of the Danish adoption register for the study of obesity and thinness. Res Publ Assoc Res Nerv Ment Dis. 1983;60:115–120. [PubMed] [Google Scholar]
- Tang J, Yu Y, Du Y, et al. Association between actual weight status, perceived weight and depressive, anxious symptoms in Chinese adolescents: a cross-sectional study. BMC Public Health. 2010;10:594. doi: 10.1186/1471-2458-10-594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tehard B, van Liere MJ, Com Nouque C, et al. Anthropometric measurements and body silhouette of women: validity and perception. J Am Diet Assoc. 2002;102:1779–1784. doi: 10.1016/s0002-8223(02)90381-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson KJ. The (mis)measurement of body image: ten strategies to improve the assessment for applied and research purposes. Body Image. 2004;1:7–14. doi: 10.1016/S1740-1445(03)00004-4. [DOI] [PubMed] [Google Scholar]
- Wagner DR, Heyward VH. Measures of body composition in blacks and whites: a comparative review. Am J Clin Nutr. 2000;71:1392–1402. doi: 10.1093/ajcn/71.6.1392. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Sholomskas D, Pottinger M, et al. Assessing depressive symptoms in five psychiatric populations: a validation study. Am J Epidemiol. 1977;106:203–214. doi: 10.1093/oxfordjournals.aje.a112455. [DOI] [PubMed] [Google Scholar]
- World Health Organization Scientific Group Research on the menopause in the 1990s. Report of a WHO Scientific Group. WHO Tech Serv Rep Ser. 1996;866:1–107. [PubMed] [Google Scholar]


