Abstract
Background
Abnormal heart rate characteristics (HRC) wax and wane in early stages of culture-positive, late-onset septicemia (LOS) in patients in the neonatal intensive care unit (NICU). Continuously monitoring an HRC index leads to a reduction in mortality among very low birth weight (VLBW) infants. We hypothesized that the reduction in mortality was due to a decrease in septicemia-associated mortality.
Methods
This is a secondary analysis of clinical and HRC data from 2989 VLBW infants enrolled in a randomized controlled trial of HRC monitoring in 9 NICUs from 2004–2010.
Results
LOS was diagnosed 974 times in 700 patients, and the incidence and distribution of organisms were similar in HRC display and non-display groups. Mortality within 30 days of LOS was lower in the HRC display compared to the non-display group (11.8% vs 19.6%, RR 0.61, 95% CI 0.43, 0.87, p<0.01), but mortality reduction was not statistically significant for patients without LOS. There were fewer large, abrupt increases in the HRC index in the days leading up to LOS diagnosis in infants whose HRC index was displayed.
Conclusions
Continuous HRC monitoring is associated with a lower septicemia-associated mortality in VLBW infants, possibly due to diagnosis earlier in the course of illness.
INTRODUCTION
Late-onset septicemia (LOS, presenting beyond 3 days of age) is a leading cause of death among very low birth weight (VLBW, <1500 grams) infants 1–2. Survivors of LOS have longer durations of mechanical ventilation, longer hospital stays, and worse neurodevelopmental outcomes compared with gestational age-matched infants who do not develop sepsis 3–4. Efforts toward reducing the toll of neonatal sepsis include preventive strategies, biomarker measurements for earlier detection, and use of adjunct immunotherapies. Extensive investigation into sepsis biomarkers has yielded promising candidates such as inflammatory cytokines5, acute phase proteins, and leukocyte activation markers 6 but the drawback of these blood tests is that they are available on a limited basis and are usually obtained when a patient is already sick, even if only subtly so. Immune modulating therapies given after a patient develops signs of sepsis have also not proven beneficial 7–8. Treatment with antibiotics or adjunct therapies prior to overt clinical deterioration might lead to better outcomes. The challenge is to identify patients early in transition from being well to being sick; continuous monitoring of heart rate characteristics was developed for this purpose 9–10.
Alterations in heart rate characteristics (HRC) occur as part of the pathophysiologic response to systemic infection. The autonomic nervous system modulates heart rate, with frequent small accelerations and decelerations occurring in response to sympathetic and parasympathetic input to cardiac pacemaker cells. Decreased beat-to-beat variability and transient decelerations occur in acute pathologic conditions such as fetal asphyxia and neonatal sepsis 11–12. In NICU patients, we have shown that changes in HRC wax and wane before onset of clinical signs of sepsis 9, 12–13, raising the possibility of earlier sepsis detection and treatment through display of HRC monitor data to clinicians. Earlier institution of antibiotics and supportive therapies could curb the systemic inflammatory response linked to tissue damage and mortality in sepsis.
Continuous HRC monitoring translates reduced heart rate variability and transient decelerations to estimate the fold-increase in probability of imminent sepsis (HRC index) using mathematical algorithms 14–17. The impact of HRC monitoring on outcomes was tested in a randomized clinical trial of 3003 VLBW infants in 9 neonatal intensive care units (NICUs) 18. The trial had a pragmatic design in that clinicians were given information about how the HRC index was developed and were instructed that an elevation in the HRC index should prompt a bedside evaluation and consideration of appropriate blood tests or treatment, but no specific course of action was mandated in response to the HRC index 18. Importantly, there was a 22% relative reduction in mortality among infants whose HRC index was displayed to clinicians (10.2% to 8.1%, p=0.04). Here, we focused on infants in the clinical trial who had one or more episodes of LOS and tested the hypothesis that mortality within 30 days of LOS is lower in the HRC display compared to the non-display group To explore the possibility that HRC monitoring led to earlier diagnosis of LOS, we analyzed large, abrupt increases, or spikes, in the HRC index and also tested the hypothesis that LOS was diagnosed after fewer spikes when the HRC index was displayed.
RESULTS
Septicemia incidence and clinical characteristics
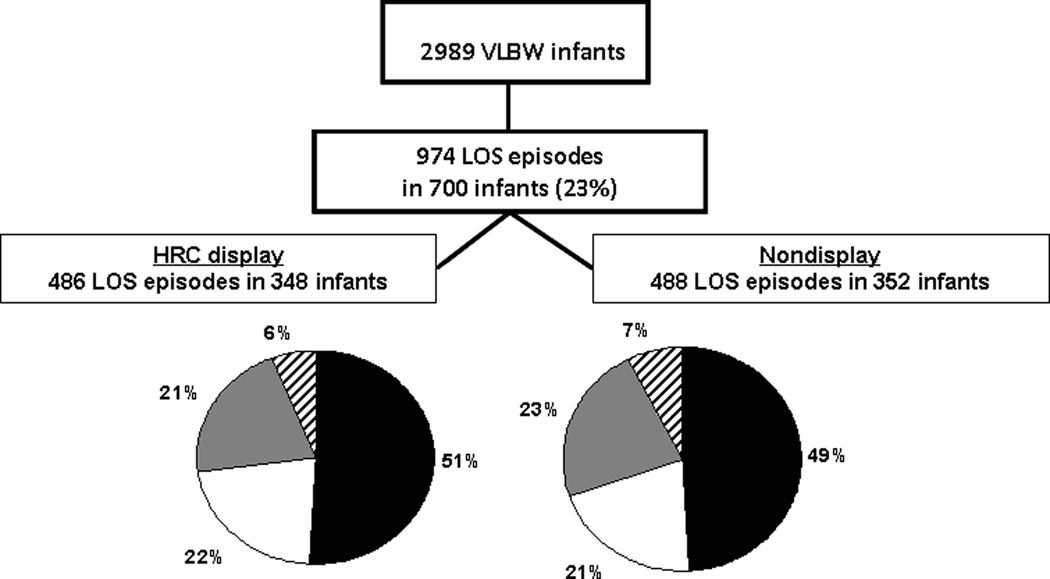
Of 3003 VLBW infants randomized, 2989 met criteria and were included in the original analysis (1500 HRC display, 1489 non-display). Fourteen patients were excluded from analysis due to withdrawal of consent, birthweight ≥ 1500 g, or cardiac arrhythmias 18. 9882 blood cultures were obtained (5225 from 1020 infants in the HRC display group and 4657 from 980 infants in the non-display group), and there were 974 episodes of LOS in 700 patients (Figure 1). The majority of LOS episodes (70%) were caused by Gram-positive bacteria, with coagulase-negative staphylococcus (CONS) accounting for 49%. The 974 episodes of LOS were equally distributed among patients in the HRC display and non-display groups (486 in 348 infants and 488 in 352 infants, respectively). There were no significant differences in the distribution of organism classes causing septicemia in the two groups (Figure 1). Compared to infants without LOS, those who experienced one or more episodes were of lower birth weight and gestational age (Table 1). In the HRC display and non-display groups, there were no significant differences in birth weight, gestational age, or gender for infants with septicemia compared to those without. Infants with one or more episodes of LOS in the HRC display group had more days alive and not on a ventilator (the primary endpoint of the clinical trial) compared to those in the non-display group (76.4 vs 69.7 days, p=0.048). Infants with LOS in the HRC display group also had more antibiotic days compared with those in the non-display group (32.1 vs 29.0 days, p=0.047)
Figure 1.
Late-onset septicemia in a randomized clinical trial of heart rate characteristics (HRC) monitoring in very low birth weight infants. 2989 VLBW infants at 9 neonatal intensive care units had HRC monitoring and were randomized to having their HRC index displayed to clinicians or not displayed. Twenty-three percent of infants had LOS (>3 days of age), and the organism distribution is shown for infants randomized to HRC display (left) or non-display (right). Black=coagulase-negative staphylococcus, white=other Gram-positive, grey=Gram-negative, striped=fungus.
Table 1.
Clinical characteristics and outcomes of VLBW infants with and without septicemia in HRC display and non-display groups
| Septicemia | No Septicemia | |||||
|---|---|---|---|---|---|---|
| HRC Display (n=348) |
Non-Display (n=352) |
p= | HRC Display (n=1152) |
Nondisplay (n=1137) |
p= | |
| Birth weight (g) | 813 (237) | 787 (238) | 0.149 | 1055 (271) | 1047 (276) | 0.52 |
| Gestational age weeks | 26 (2.3) | 26 (2.4) | 0.864 | 29 (2.7) | 28 (2.7) | 0.59 |
| Male (%) | 49 | 49 | 0.628 | 49 | 50 | 0.62 |
| Hospital days | 92 (55) | 86 (48) | 0.130 | 56 (37) | 56 (40) | 0.98 |
| Antibiotic days | 32.1 (21) | 29. 0 (20) | 0.047 | 7.6 (11) | 7.6 (13) | 0.96 |
| Days alive not on MV | 76.4 (43) | 69.7 (46) | 0.048 | 107 (31) | 106 (33) | 0.67 |
| In-hospital mortality % (n) | 15.2 (53) | 21.9 (77) | 0.026 | 6.0 (69) | 6.6 (75) | 0.61 |
| 30 day LOS mortalitya% (n) | 11.8 (41) | 19.6 (68) | 0.005 | |||
Mean (standard deviation) or %, where indicated
MV = mechanical ventilation
30 days from last septicemia episode
Bold p values are statistically significant at p<0.05.
Septicemia-related mortality
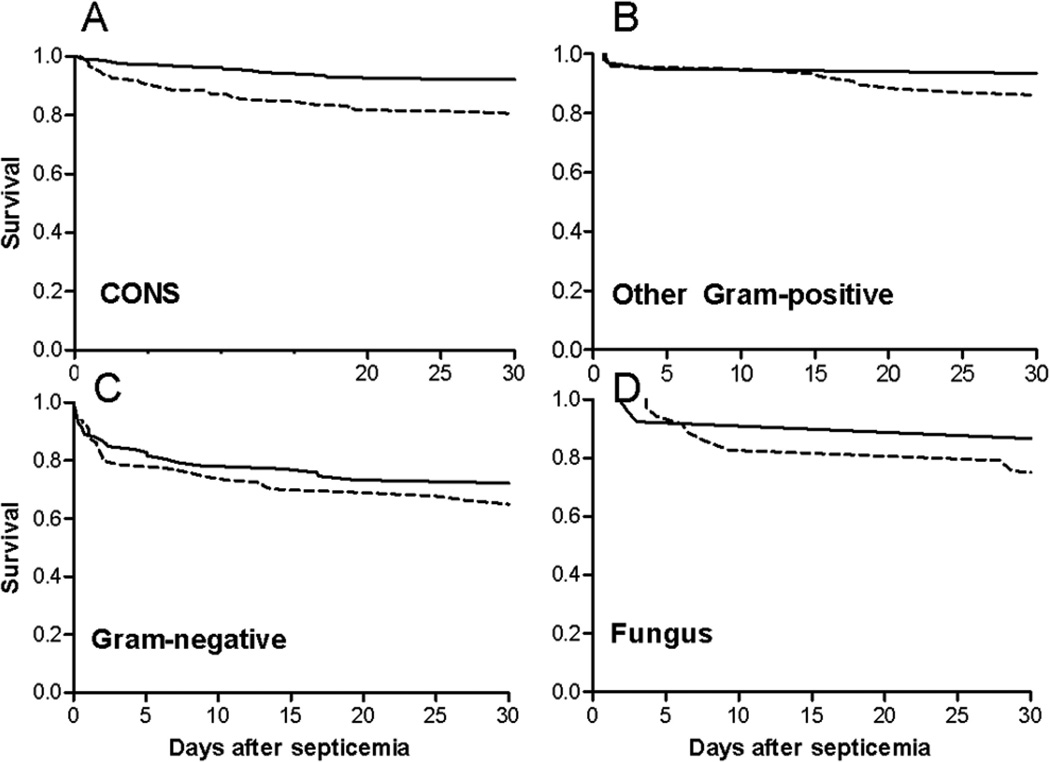
Mortality within 30 days of LOS was significantly lower in HRC display compared to non-display infants (11.8% versus 19.6%, relative risk 0.61, 95% CI 0.43, 0.87, p<0.01), as was overall in-hospital mortality (15.2% vs 21.9%, relative risk 0.70, 95% CI 0.51, 0.96, p<0.03). Mortality within 7 days of LOS was 9.2% in HRC display compared to 13.9% in non-display infants (relative risk 0.66, 95% CI 0.43, 1.01, p=0.059). Within each organism group, there was reduced mortality with HRC display (Figure 2). The mortality reduction reached statistical significance for CONS, the most frequent infecting organism (6.3% versus 18.1% for HRC display versus non-display, p=0.0003). For infants who did not have septicemia, the mortality reduction from 6.6% in the non-display group to 6.0% in the HRC display group was not statistically significant (Table 1). In the randomized trial, there were 30 excess deaths in the non-display compared to the HRC display group, and 27 of these excess deaths occurred within 30 days of LOS.
Figure 2.
Organism-specific mortality based on heart rate characteristics (HRC) monitor display. Survival is shown within 30 days of diagnosis of late-onset septicemia with CONS (A), other Gram-positive bacteria (B), Gram-negative bacteria (C), and fungi (D). Survival was higher in each organism group in infants with HRC displayed (solid line) compared with those with HRC not displayed (dashed line).
Heart rate characteristics index and mortality in episodes of LOS
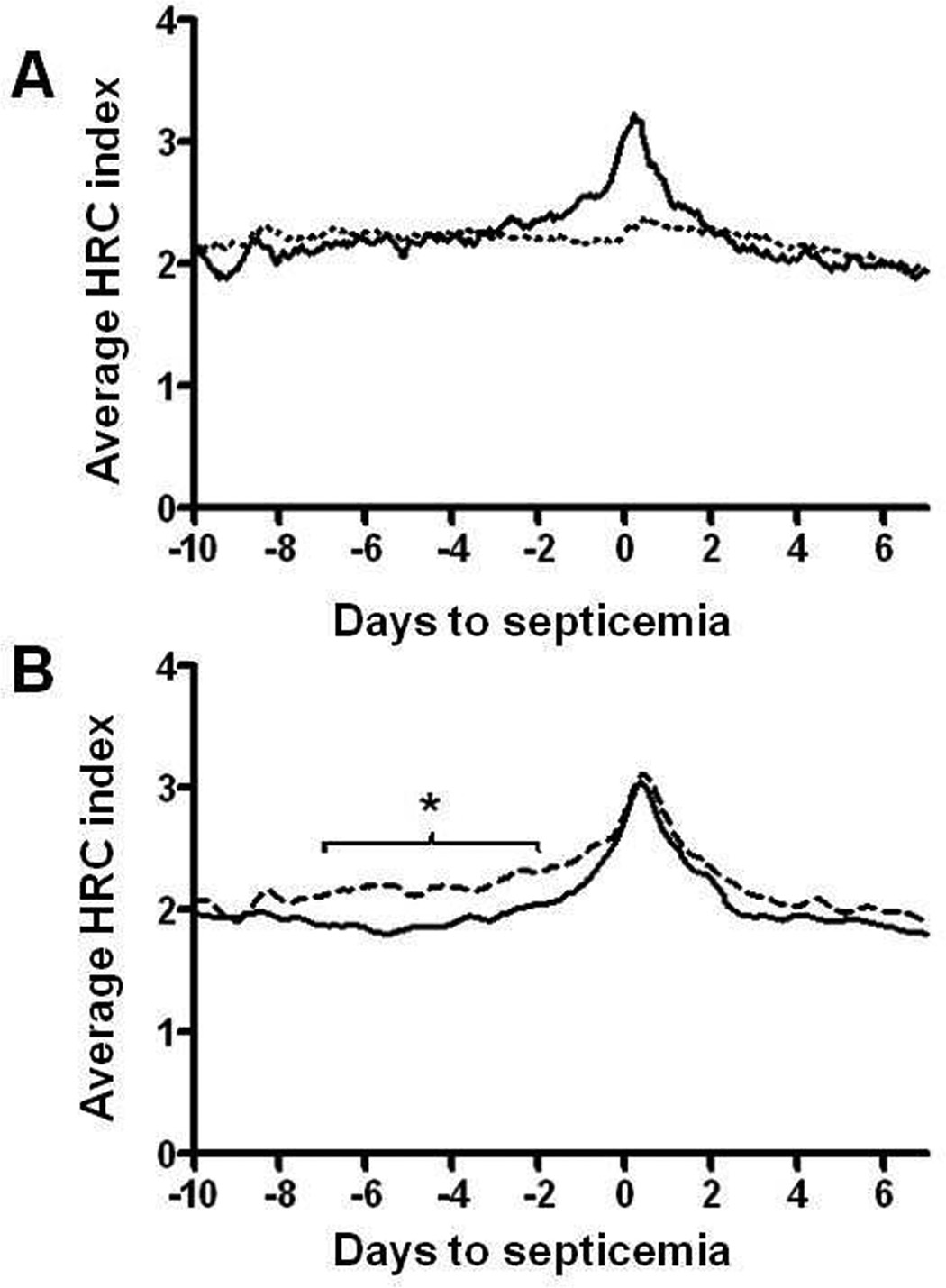
The HRC index increased in the days leading up to clinical diagnosis of LOS, with a significantly higher HRC index at 24 hours compared to 48 hours prior to LOS diagnosis (p<0.01) (Figure 3A). In contrast, the concurrent baseline probability of sepsis, calculated from established risk factors of gestational and postmenstrual age, birth weight, and presence of mechanical ventilation showed only a small increase due to some patients requiring intubation and mechanical ventilation around the time of septicemia. There was an increase in the average HRC index prior to clinical diagnosis of LOS with coagulase-negative staphylococcus, other Gram-positive bacteria, Gram-negative bacteria, and fungi. Peak HRC index was similar for each pathogen group (CONS 3.0 ± 2.2, Other Gram-positive 3.1 ± 2.3, Gram-negative 3.0 ± 2.2, Fungus 3.3 ± 2.2, mean ± SD, p=0.68). 92% of cases of LOS in non-display infants were associated with HRC index >1 and 79% with HRC index >2 within 24h of diagnosis.
Figure 3.
Heart rate characteristics index and risk factor–based probability in cases of late onset septicemia A) Average HRC index (solid line) in the 2-week period around the diagnosis of LOS at day 0, compared to the risk-factor based probability of sepsis (dotted line) based on gestational and postmenstrual age, birth weight, and mechanical ventilation. B) Average HRC index around the diagnosis of LOS in infants randomized to HRC display (solid line) or non-display (dashed line) (* p<0.01).
Infants in the non-display group had a significantly higher average HRC index in the 2 to 7 days leading up to the time of positive blood culture compared to infants in the HRC display group (p<0.01 for each day from −2 to −7 relative to LOS) (Figure 3B). Figure 4 illustrates the occurrence of a single abrupt rise in the HRC index (“spike”) around the time of LOS versus multiple spikes in the days leading up to diagnosis. The proportion of patients with spikes at non-septic times was comparable between the two groups (Table 2). In contrast, more patients in both groups had spikes in the 2 to 7 day time interval prior to diagnosis of LOS, demonstrating that the spikes are relevant to septicemia. Further, more patients in the non-display group had large spikes than in the HRC display group regardless of the infecting organism.
Figure 4.
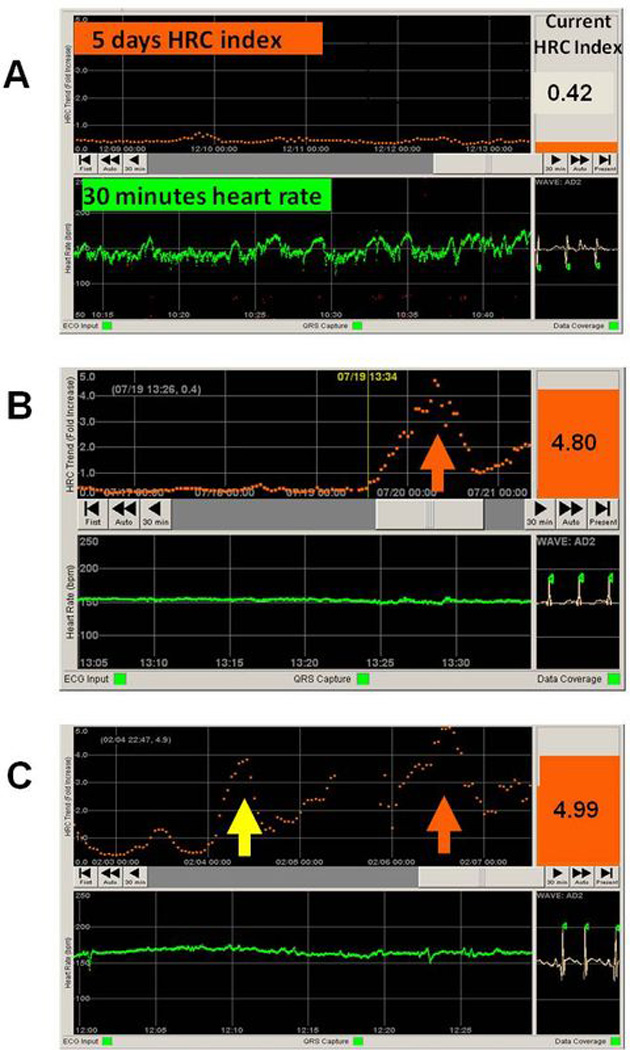
Heart rate characteristics index monitor screen shots illustrating normal HRC and large HRC index spikes. A) HRC monitor individual patient display shows the 5-day HRC index trend (orange), the latest 30 minutes of heart rate in beats per minute (green), and the current HRC index (0.42). In this infant, the HRC index has been low (<1) for at least 5 days, indicating normal heart rate characteristics and low probability of sepsis in the next 24 hours. B) HRC monitor display for an infant with a large HRC index spike at the time of septicemia diagnosis (orange arrow, HeRO score 4.80) and no large spikes in the days before. C) Large HRC index spike at the time of septicemia diagnosis (orange arrow, HeRO score 4.99) and a large HRC index spike two days before sepsis diagnosis (yellow arrow, HeRO score 3.89).
Table 2.
Percent of patients with large HRC index spikes 2–7 days prior to diagnosis of late-onset septicemia, or during random 5-day periods
| HRC display % with spike |
Nondisplay % with spike |
p= | |
|---|---|---|---|
| Never septic | 8.6 | 7.0 | 0.47 |
| Remote from LOSa | 16.1 | 17.6 | 0.66 |
| LOS, all organisms | 22.4 | 34.3 | <0.01 |
| CONS | 22.4 | 36.8 | <0.01 |
| Other Gram-positive | 21.1 | 31.0 | 0.17 |
| Gram-negative | 18.2 | 26.5 | 0.22 |
| Fungus | 33.3 | 46.7 | 0.79 |
More than a week before or after LOS
Bold p values are statistically significant at p<0.05
DISCUSSION
In this secondary analysis of data from a large, randomized clinical trial of HRC monitoring in VLBW infants, we found that mortality reduction was much greater for infants with septicemia when the HRC index was displayed to clinicians than for infants without septicemia. In addition, we found that the average HRC index increased prior to clinical diagnosis of late-onset septicemia, irrespective of infecting organism.
Sepsis-related morbidity and mortality are unacceptably high in part because the diagnosis is often delayed by the subtlety of presenting signs. New biomarker tests for sepsis improve on earlier ones 6 but require clinical suspicion of illness to prompt blood testing. By then, the stage of illness may be so advanced that antibiotic administration fails to curtail the systemic inflammatory response that can lead to death and disability. Adjunct sepsis therapies such as IVIG given to neonates once they show clinical signs of infection have not proven effective in reducing mortality and morbidity 7. Continuous monitoring of heart rate characteristics has the potential advantage of alerting clinicians to pathophysiologic changes in the early phase of sepsis, prior to overt clinical deterioration, leading to earlier treatment and improved outcomes.
In this large trial of VLBW infants, the incidence of sepsis was comparable to that reported in other large surveys 1 and was very similar in HRC display and non-display groups, underscoring that the function of HRC monitoring is not sepsis prevention, but rather early detection. The HRC index increased in the day prior to clinical diagnosis of LOS with Gram-positive or Gram-negative bacteria or fungi. The average HRC index was significantly higher in the week leading up to LOS diagnosis in infants whose HRC index was not displayed to clinicians and was accompanied by more acute HRC index spikes. We have previously described waxing and waning of abnormal heart rate characteristics for several days prior to the clinical presentation of sepsis in NICU patients 9, 12–13. There is no way to determine exactly when an infant develops a bloodstream infection, so we can only speculate that these pre-diagnosis HRC spikes represent an early phase of illness and that recognition, evaluation and treatment at this time averted clinical deterioration and contributed to lower morbidity and mortality. Among the 700 infants who developed sepsis in the randomized trial, those whose HRC index was displayed to clinicians had not only fewer acute increases in HRC index and lower mortality, but also significantly more days alive and not on a ventilator, which was the primary endpoint of the original study. Lower mortality among HRC display infants occurred across all organism classes, with the largest reduction occurring with CONS septicemia, which accounted for nearly half of all LOS cases. The tradeoff for lower mortality is that infants whose HRC index was displayed had 12% more blood cultures obtained and 11% more days on antibiotics. The fact that there were, on average, only 3 extra antibiotic days in the infants in the HRC display compared to non-display group among infants who developed LOS leads us to speculate that monitoring the HRC index may give clinicians insight into appropriate timing of both initiating and discontinuing antibiotics.
The HRC monitoring study is the largest randomized clinical trial in very low birth weight infants reported to date. A limitation of the current analysis of LOS in this trial is that the exact timing of onset of sepsis relative to the changes in the HRC index cannot be known. The design of the clinical trial did not include a mandated intervention for infants with an acute increase in HRC index, and we can only speculate as to whether the increases in the HRC index in the days leading up to the positive blood culture represent a subclinical sepsis prodrome and an opportunity for earlier intervention.
In conclusion, HRC monitoring in very low birth weight infants reduces mortality and this reduction in mortality is associated with a lower mortality following late-onset sepsis. It is possible that HRC monitoring prompts recognition of sepsis in its earlier stages when treatment is more likely to reduce morbidity and mortality.
METHODS
Patient population
VLBW infants at 9 NICUs were enrolled in a randomized clinical trial of HRC monitoring from April 2004 through May 2010. The study was sponsored by the National Institute of Child Health and Human Development and Medical Predictive Science Corporation (Charlottesville, VA). Institutional review boards approved the protocol at each study site, and informed consent was obtained from parents for infants’ participation. In this trial, all infants had their HRC index monitored and were randomized 1:1 (stratified by birthweight ≥ or <1000 grams) to having their HRC index continuously displayed or not displayed to nurses, nurse practitioners, and physicians.
Clinical data collection, and sepsis and mortality definitions
In the RCT, we recorded demographics, dates and results of blood cultures, days on antibiotics or antifungal agents (other than prophylactic fluconazole or ampicillin), days on mechanical ventilation, and date of death or NICU discharge. The current analysis results from a careful reclassification of septicemia episodes in the trial with LOS defined as 1) a positive blood culture obtained at >3 days of age, excluding corynebacterium and diphtheroids, 2) no prior positive blood culture for the same organism in the previous 7 days, and 3) antibiotics administered for at least 5 days when the organism grown was coagulase-negative staphylococcus. “Other positive” blood cultures were reclassified if a specific organism could be identified through database review. The 18 cases of multiple organisms in a blood culture were classified by what was considered the most virulent organism. We excluded 15 episodes from the organism-specific analyses because the organism could not be identified through database review. We also excluded 92 episodes in which there was a positive blood culture for CONS but the infant received fewer than 5 days of antibiotics. As a result of this analysis, 37 patients were reclassified as having no sepsis.
Mortality was assessed as all in-hospital mortality and as death within 30 days and within 7 days of the last episode of LOS.
Analysis of risk factor-based LOS probability
The HRC index was originally conceived, developed, and validated for assessment of probability of imminent LOS in VLBW infants 12, 19–21. To establish the baseline probability of LOS based on standard risk factors 1, we developed a model incorporating gestational and postmenstrual age, birth weight, and presence of mechanical ventilation in the patients in the control, non-display group.
HRC index monitoring and spike analysis
The FDA 510(k)-cleared HeRO (Heart Rate Observation) monitoring system was provided by Medical Predictive Science Corporation (Charlottesville, VA). The monitor uses existing electrocardiogram or heart rate data from standard bedside monitors to calculate the HRC index, which is the fold-increase in probability that the patient will have a clinical deterioration consistent with sepsis in the next 24 hours. The HRC index is derived from an externally validated logistic regression expression that relates decreased HR variability and transient HR decelerations to the probability that the baby will imminently be diagnosed with sepsis. The monitor displays the current HRC index, which is updated every hour and represents heart rate characteristics over the previous 12 hours. The monitor also displays the 5-day HRC index trend.
We analyzed the average hourly HRC index around the time of LOS in infants in the HRC display and non-display groups. In order to examine a possible mechanism of lower mortality with HRC index monitoring, we also counted large, abrupt increases in the HRC index (“spikes”) in the 2–7 day period before clinical diagnosis of LOS (the time period during which there was a significant difference in average HRC index in HRC display versus non-display infants). We defined a spike as an increase in HRC index of at least 3 compared with the prior 5-day running average, excluding the 12 hours before the peak. Rates of large spikes were compared in infants who never developed LOS, and in infants in the HRC display and non-display groups who developed LOS, both during a randomly chosen non-septic 5-day period and in the 2 to 7 day period prior to LOS diagnosis.
Statistical analysis
HRC index is reported as mean ± SD. We used multivariable logistic regression modeling adjusted for repeated measures using the Huber-White method and determined confidence intervals by bootstrap 22. Differences in demographics, sepsis rates, and organism types were tested for significance using non-parametric tests. Differences in survival after sepsis diagnosis were tested for significance using a proportional hazards model. Statistical testing was performed with Matlab software (MathWorks, Natick, MA), with a two-tailed level of significance of 0.05.
Acknowledgments
STATEMENT OF FINANCIAL SUPPORT: Supported by National Institutes of Health (Bethesda, MD: grant R01-HD48562 to J.R.M.).
Footnotes
DISCLOSURES: J.R.M. and D.E.L. have consulting agreements and equity shares in Medical Predictive Science Corporation, Charlottesville, VA. The other authors declare no conflicts of interest.
REFERENCES
- 1.Stoll BJ, Hansen N, Fanaroff AA, et al. Late-onset sepsis in very low birth weight neonates: the experience of the NICHD Neonatal Research Network. Pediatrics. 2002;110:285–291. doi: 10.1542/peds.110.2.285. [DOI] [PubMed] [Google Scholar]
- 2.Makhoul IR, Sujov P, Smolkin T, Lusky A, Reichman B. Pathogen-specific early mortality in very low birth weight infants with late-onset sepsis: a national survey. Clin Infect Dis. 2005;40:218–224. doi: 10.1086/426444. [DOI] [PubMed] [Google Scholar]
- 3.Schlapbach LJ, Aebischer M, Adams M, et al. Impact of sepsis on neurodevelopmental outcome in a Swiss National Cohort of extremely premature infants. Pediatrics. 2011;128:e348–e357. doi: 10.1542/peds.2010-3338. [DOI] [PubMed] [Google Scholar]
- 4.Stoll BJ, Hansen NI, Adams-Chapman I, et al. Neurodevelopmental and growth impairment among extremely low-birth-weight infants with neonatal infection. JAMA. 2004;292:2357–2365. doi: 10.1001/jama.292.19.2357. [DOI] [PubMed] [Google Scholar]
- 5.Raynor LL, Saucerman JJ, Akinola MO, Lake DE, Moorman JR, Fairchild KD. Cytokine screening identifies NICU patients with Gram-negative bacteremia. Pediatr Res. 2012;71:261–266. doi: 10.1038/pr.2011.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ng PC, Ang IL, Chiu RW, et al. Host-response biomarkers for diagnosis of lateonset septicemia and necrotizing enterocolitis in preterm infants. J Clin Invest. 2010;120:2989–3000. doi: 10.1172/JCI40196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brocklehurst P, Farrell B, King A, et al. Treatment of neonatal sepsis with intravenous immune globulin. N Engl J Med. 2011;365:1201–1211. doi: 10.1056/NEJMoa1100441. [DOI] [PubMed] [Google Scholar]
- 8.Carr R, Modi N, Dore C. G-CSF and GM-CSF for treating or preventing neonatal infections. Cochrane Database Syst Rev. 2003:CD003066. doi: 10.1002/14651858.CD003066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fairchild KD, O'Shea TM. Heart rate characteristics: physiomarkers for detection of late-onset neonatal sepsis. Clin Perinatol. 2010;37:581–598. doi: 10.1016/j.clp.2010.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fairchild K, Aschner JL. HeRO monitoring to reduce mortality in NICU patients. Research and Reports in Neonatology. 2012;2:65–76. [Google Scholar]
- 11.Griffin MP, Lake DE, Bissonette EA, Harrell FE, Jr, O'Shea TM, Moorman JR. Heart rate characteristics: novel physiomarkers to predict neonatal infection and death. Pediatrics. 2005;116:1070–1074. doi: 10.1542/peds.2004-2461. [DOI] [PubMed] [Google Scholar]
- 12.Griffin MP, O'Shea TM, Bissonette EA, Harrell FE, Jr, Lake DE, Moorman JR. Abnormal heart rate characteristics preceding neonatal sepsis and sepsis-like illness. Pediatr Res. 2003;53:920–926. doi: 10.1203/01.PDR.0000064904.05313.D2. [DOI] [PubMed] [Google Scholar]
- 13.Moorman JR, Lake DE, Griffin MP. Heart rate characteristics monitoring for neonatal sepsis. IEEE Trans Biomed Eng. 2006;53:126–132. doi: 10.1109/TBME.2005.859810. [DOI] [PubMed] [Google Scholar]
- 14.Griffin MP, Scollan DF, Moorman JR. The dynamic range of neonatal heart rate variability. Journal of Cardiovascular Electrophysiology. 1994;5:112–124. doi: 10.1111/j.1540-8167.1994.tb01151.x. [DOI] [PubMed] [Google Scholar]
- 15.Cao H, Lake DE, Griffin MP, Moorman JR. Increased nonstationarity of neonatal heart rate before the clinical diagnosis of sepsis. Ann Biomed Eng. 2004;32:233–244. doi: 10.1023/b:abme.0000012743.81754.0b. [DOI] [PubMed] [Google Scholar]
- 16.Kovatchev BP, Farhy LS, Cao H, Griffin MP, Lake DE, Moorman JR. Sample asymmetry analysis of heart rate characteristics with application to neonatal sepsis and systemic inflammatory response syndrome. Pediatr Res. 2003;54:892–898. doi: 10.1203/01.PDR.0000088074.97781.4F. [DOI] [PubMed] [Google Scholar]
- 17.Lake DE, Richman JS, Griffin MP, Moorman JR. Sample entropy analysis of neonatal heart rate variability. Am J Physiol Regul Integr Comp Physiol. 2002;283:R789–R797. doi: 10.1152/ajpregu.00069.2002. [DOI] [PubMed] [Google Scholar]
- 18.Moorman JR, Carlo WA, Kattwinkel J, et al. Mortality reduction by heart rate characteristic monitoring in very low birth weight neonates: a randomized trial. J Pediatr. 2011;159:900–906. doi: 10.1016/j.jpeds.2011.06.044. e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Griffin MP, Moorman JR. Toward the early diagnosis of neonatal sepsis and sepsis-like illness using novel heart rate analysis. Pediatrics. 2001;107:97–104. doi: 10.1542/peds.107.1.97. [DOI] [PubMed] [Google Scholar]
- 20.Griffin MP, Lake DE, Moorman JR. Heart rate characteristics and laboratory tests in neonatal sepsis. Pediatrics. 2005;115:937–941. doi: 10.1542/peds.2004-1393. [DOI] [PubMed] [Google Scholar]
- 21.Griffin MP, Lake DE, O'Shea TM, Moorman JR. Heart rate characteristics and clinical signs in neonatal sepsis. Pediatr Res. 2007;61:222–227. doi: 10.1203/01.pdr.0000252438.65759.af. [DOI] [PubMed] [Google Scholar]
- 22.Harrell FE. Regression modeling strategies: with applications to linear models, logistic regression and survival analysis. Berlin: Springer; 2001. [Google Scholar]