Abstract
Infertility affects approximately 15% of couples trying to conceive, and a male factor contributes to roughly half of these cases. Oxidative stress (OS) has been identified as one of the many mediators of male infertility by causing sperm dysfunction. OS is a state related to increased cellular damage triggered by oxygen and oxygen-derived free radicals known as reactive oxygen species (ROS). During this process, augmented production of ROS overwhelms the body's antioxidant defenses. While small amounts of ROS are required for normal sperm functioning, disproportionate levels can negatively impact the quality of spermatozoa and impair their overall fertilizing capacity. OS has been identified as an area of great attention because ROS and their metabolites can attack DNA, lipids, and proteins; alter enzymatic systems; produce irreparable alterations; cause cell death; and ultimately, lead to a decline in the semen parameters associated with male infertility. This review highlights the mechanisms of ROS production, the physiological and pathophysiological roles of ROS in relation to the male reproductive system, and recent advances in diagnostic methods; it also explores the benefits of using antioxidants in a clinical setting.
Keywords: Antioxidants; Infertility, male; Oxidative stress; Reactive oxygen species; Spermatozoa
INTRODUCTION
For most couples, procreating is a natural part of life that involves neither special planning nor intervention. Unfortunately, when trying to conceive, 15% to 25% of the couples struggle and, consequently, seek medical advice on how to improve their chances of fertilization and successful pregnancy [1]. According to the World Health Organization [2] guidelines, in approximately half of these cases, the male factor is the cause of infertility when an "alteration in sperm concentration, motility, and/or morphology is present in at least one sample of two sperm analyses, collected 1 to 4 weeks apart" [3]. This problem is further compounded when no identifiable reason can be found. Currently, oxidative stress (OS) is believed to be an important and plausible cause of idiopathic male infertility.
"OS is a condition that reflects an imbalance between the systemic manifestation of reactive oxygen species (ROS) and a biological system's ability to readily detoxify (antioxidant defenses) the reactive interm1ediates or to repair the resulting damage" [4,5]. In a healthy body, pro-oxidants and antioxidants remain in balance. Spermatozoa are equipped with antioxidant defense mechanisms and are likely to quench ROS, thereby protecting gonadal cells and mature spermatozoa from oxidative damage [6]. However, under pathological conditions, the uncontrolled production of ROS exceeds the antioxidant capacity of the seminal plasma, resulting in OS [1,6].
Statistics from the United States indicate that OS is one of the major causes of male infertility; that is, 30% to 40% of infertile men have elevated levels of ROS in their seminal plasma [7]. Spermatozoa were the first cell type reported to show potential susceptibility to OS. In some situations, the damage caused by oxidants may be repaired. Unfortunately, spermatozoa are unable to restore the damage induced by OS because they lack the necessary cytoplasmic-enzyme repair systems. This is one of the features that make spermatozoa unique in their susceptibility to oxidative insult [8]. This is predominantly due to the fact that their cell membranes are rich in polyunsaturated fatty acids (PUFAs), rendering them highly susceptible to oxygen-induced damage and hence, lipid peroxidation (LPO). Subsequently, a rapid loss of intracellular adenosine tri-phosphate (ATP) from LPO causes axonemal damage, decreased sperm viability, and increased mid-piece sperm morphological defects, all of which contribute to decreased sperm motility [9,10].
OS has become an area of great concern for clinicians and scientists because of the fact that this pathway of programmed deterioration has also resulted in poor fertilization, poor embryonic development, pregnancy loss, birth defects (including autism), and childhood cancer [11,12,13,14]. Over the years, the literature on this topic has increased in volume with the addition of several original contributions concerning the role of OS in male reproduction.
In this paper, we will provide a comprehensive overview of the latest evidence regarding the mechanism of ROS production, the physiological roles of ROS, and the patho-physiology of ROS, as well as the impact of OS on male infertility in humans. Furthermore, we will elaborate on different techniques used to measure ROS as well as different treatment strategies implemented by physicians to reduce OS levels in the seminal plasma of infertile men, which hopefully contribute to increased potential for natural fertilization and conception.
REACTIVE OXYGEN SPECIES
ROS, also known as free radicals, have at least one unpaired electron. They are oxidizing agents generated as byproducts from the metabolism of oxygen. Due to the unpaired electron in the outer shell, they form highly reactive molecules [6,15]. ROS represents a collection of a broad range of radicals (e.g., hydroxyl ion [OH-], superoxide ion [O2-], nitric oxide [NO], peroxyl [RO2], lipid peroxyl [LOO], and Thiyl [RS-]) and non-radical molecules (singlet oxygen [-1O2], hydrogen peroxide [H2O2], hypochloric acid [HOCL], lipid peroxide [LOOH], and ozone [O3]) [9].
1. Generation of reactive oxygen species
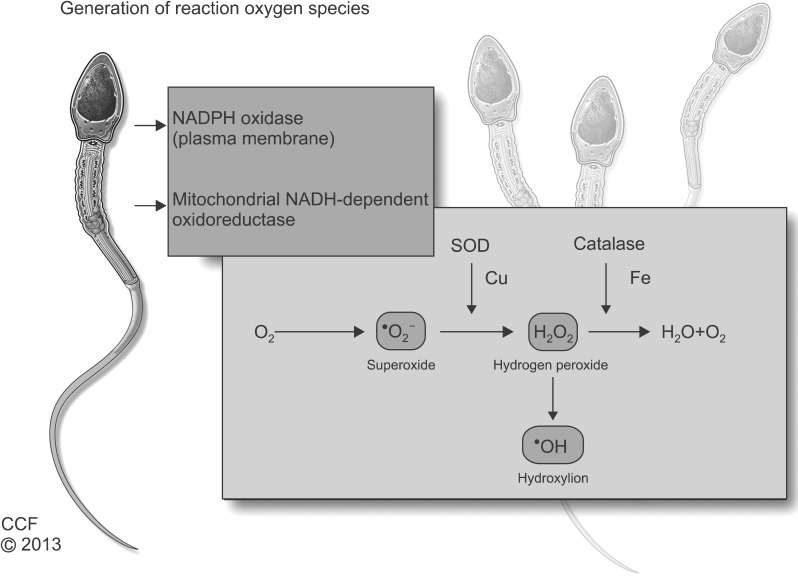
Research has shown that ROS causes electron leakage from actively respiring spermatozoa, mediated by intracellular redox activities. The generation of ROS in spermatozoa may occur via two methods: (1) the nicotinamide adenine dinucleotide phosphate oxidase system at the level of the sperm plasma membrane and/or (2) the nicotinamide adenine dinucleotide-dependent oxido-reductase reaction at the mitochondrial level. The latter mechanism appears to be the main source of ROS. Spermatozoa are rich in mitochondria because a constant supply of energy is required for their motility [6]. Therefore, the presence of dysfunctional spermatozoa in the semen significantly elevates the production of ROS, which in turn affects its mitochondrial function and subsequently, sperm function such as motility.
A majority of ROS generated in human spermatozoa is O2-. This electron-reduced product of O2- reacts with itself via dismutation to generate H2O2. In the presence of transition metals such as iron and copper, H2O2 and O2- undergo the Haber-Weiss reaction to generate the extremely reactive and destructive OH- (Fig. 1). OH- radicals are exceptionally potent initiators of the LPO cascade and can lead to a loss of sperm function from the disruption of membrane fluidity [16,17,18].
Fig. 1.
Generation of reactive oxygen species. NADPH: nicotinamide adenine dinucleotide phosphate, NADH: nicotinamide adenine dinucleotide, SOD: superoxide dismutase, Cu: copper, Fe: Iron.
A recent study describing the production of O2- in spermatozoa revealed that the presence of a calcium-dependent NADPH oxidase called NOX5 (encoded by the NOX5 gene) has been established within human spermatozoa, particularly in the acrosomal and midpiece regions [19]. NOX5 was initially detected in the human testis and is activated when Ca2 binds to its cytosolic N-terminal EF-hand domain. This binding causes conformational changes to the cell, thereby inducing OS. This finding provides further evidence that NOX5 is a major source of ROS generation in human spermatozoa. Whether NOX5 is overexpressed in the spermatozoa of patients exhibiting infertility associated with OS has not yet been determined [16].
SOURCES OF REACTIVE OXYGEN SPECIES IN SEMINAL PLASMA
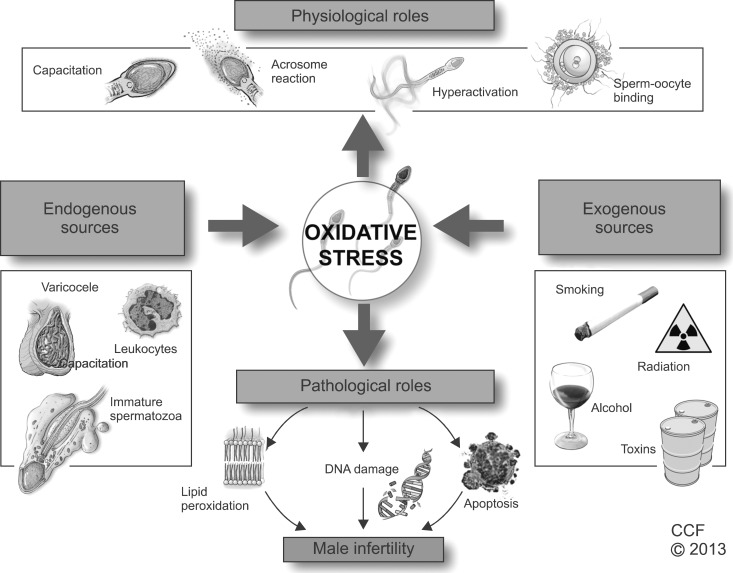
ROS found in seminal plasma originates from various endogenous and exogenous sources. The human ejaculate consists of different types of cells, including mature and immature cells, round cells from different stages of spermatogenesis, leukocytes, and epithelial cells. Of these, leukocytes-mainly neutrophils and macrophages- and immature spermatozoa are considered the main endogenous sources of ROS, while several lifestyle factors such as excessive smoking and alcohol consumption, and environmental factors such as radiation and toxins can contribute to exogenous ROS [10,20,21]. Fig. 2 summarizes the relationship of increasing ROS production in semen with male infertility.
Fig. 2.
Oxidative stress in male reproduction.
1. Endogenous sources of reactive oxygen species
1) Leukocytes
Peroxidase-positive leukocytes include polymorphonuclear leukocytes (50%~60%) and macrophages (20%~30%) [22]. A large proportion of these peroxidase-positive leukocytes originate from the prostate and seminal vesicles. When these major sources of ROS are activated by various intracellular or extracellular stimuli, such as infection or inflammation, they can discharge up to 100 times more ROS than normal and increase the NADPH production via the hexose monophosphate shunt [23,24]. An increase in proinflammatory cytokines, such as interleukin (IL)-8, and a decrease in the antioxidant superoxide dismutase (SOD) can result in a respiratory burst, production of high levels of ROS, and ultimately, OS. OS will cause sperm damage if seminal leukocyte concentrations are abnormally high as is the case in leukocytospermia [25], which the World Health Organization defines as the presence of more than one million peroxidase-positive cells per milliliter of semen [2].
Over the years, extensive research has been carried out to establish a link between the presence of leukocytes in the ejaculate and a male factor as the cause of infertility. Various studies point to a correlation between decreased sperm function and seminal plasma with abnormally elevated levels of ROS, IL-6, IL-8, and tumor necrosis factor, all of which result in increased sperm cell membrane LPO [23,26].
2) Immature spermatozoa
During spermatogenesis, developing spermatozoa extrude their cytoplasm in order to prepare for fertilization. However, damaged spermatozoa retain excess cytoplasm around the midpiece due to an arrest in spermiogenesis; this condition is known as excess residual cytoplasm (ERC). ERC activates the NADPH system by means of the hexose-monophosphate shunt, which spermatozoa use as a source of electrons for ROS generation and potentially, OS [27]. Hence, ERC ultimately affects sperm motility, morphology, and fertilization potential, which may lead to male infertility [5].
3) Varicocele
Varicocele is defined as an abnormal dilation of veins in the pampiniform plexus around the spermatic cord. Since varicocele is detected in about 40% of male partners of all infertile couples, it is considered the leading cause of male factor infertility [28]. It has been shown that the level of seminal ROS is associated with the grade of varicocele; that is, the higher the grade of varicocele is, the greater is the level of ROS detected [29].
2. Exogenous sources of reactive oxygen species
1) Radiation
Radiation, a natural source of energy, has significant clinical effects on humans. With respect to male reproductive health, several studies have implicated radiation emitted from mobile phones in the increase of the production of ROS in human semen with impaired semen quality [30,31]. In vitro studies have demonstrated that electromagnetic radiation induces ROS production and DNA damage in human spermatozoa, which further decreases the motility and vitality of sperm cells as well as their concentration depending on the duration of exposure to radiation [32]. These radiofrequency electromagnetic waves can negatively affect the electron flow along the internal membranes of the cell as a result of the numerous charged molecules within the cytosol, thus disrupting normal cellular and organelle function [23].
2) Toxins
Toxins released from structural materials or industrial products accumulate in the human body and increase ROS production in the testes, negatively impacting the sperm structure and function [33]. Phthalates, found in a variety of plastic objects used for domestic and industrial purposes, have been studied in great detail [34,35]. They have been found to impair spermatogenesis and induce sperm DNA damage [36]. Furthermore, it was demonstrated that workers who were regularly exposed to toxins in the form of metals such as cadmium, chromium, lead, manganese, and mercury were more likely to have decreased sperm quality, count, volume, and density [37].
3) Smoking
Tobacco is known to be one of the major preventable causes of death worldwide. Cigarettes contain more than 4,000 chemical compounds including alkaloids, nitrosamines, and inorganic molecules. Some of the chemicals were shown to cause an imbalance between ROS and antioxidants in the semen of smokers [23]. This ROS and antioxidant disproportion affects the overall semen quality. Smoking has been shown to result in a 48% increase in seminal leukocyte concentrations and a 107% increase in seminal ROS levels [38]. Moreover, smokers have decreased levels of seminal plasma antioxidants such as vitamin E and vitamin C, placing their sperm at the additional risk of oxidative damage. This has been confirmed by a significant increase in the levels of 8-OHdG, another biomarker of oxidative damage, in the seminal plasma of smokers [21]. A study on the semen profiles of smokers versus non-smokers showed that spermatozoa from smokers were significantly more sensitive to acid-induced DNA denaturation than those of non-smokers and resulted in higher levels of DNA strand breaks [39]. Another study performed on smokers revealed that the increased cadmium and lead concentrations in their blood and semen led to increased ROS production with an accompanying decrease in sperm motility [40]. Further, it was proven that prolonged exposure to tobacco smoke is linked to an increase in sperm DNA damage and apoptosis, leading to increased male infertility.
4) Alcohol consumption
Alcohol is known as a promoter of ROS production and interferes with the body's antioxidant defense mechanism, particularly in the liver. Many factors are involved in causing alcohol-induced OS. When acetaldehyde, one of the by-products of ethanol metabolism, interacts with proteins and lipids, ROS is formed. This results in molecular damage to proteins, lipids, and DNA. Therefore, excessive alcohol consumption is associated with a decreased percentage of normal spermatozoa in asthenozoospermic patients [41]. A study of 46 alcoholic men of reproductive age has reported a significant increase in serum LPO by-products and a decrease in antioxidants, providing further evidence of ethanol-induced OS within the testes [4].
PHYSIOLOGICAL ROLES OF ROS IN SEMINAL PLASMA
Although high concentrations of ROS cause sperm pathologies (ATP depletion) in the form of inadequate axonemal phosphorylation or LPO, resulting in a loss of sperm motility and viability, many studies have demonstrated that low and controlled (physiological levels) concentrations of ROS play an important role in normal physiological processes such as capacitation, hyperactivation, acrosome reaction, and sperm-oocyte fusion in order to ensure appropriate fertilization [8].
1. Capacitation
Capacitation is the penultimate process in the maturation of spermatozoa and is required to render them competent to successfully fertilize the ovum [20]. Controlled ROS production occurs in spermatozoa during the capacitation process, initiating various molecular modifications. The first step involves an increase in cyclic adenosine 3',5'-monophosphate (cAMP). The cAMP pathway is necessary for many living organisms and life processes as it can activate enzymes and regulate gene expression [42]. This pathway involves the activation of protein kinase A (PKA) and the phosphorylation of PKA substrates (arginine, serine, and threonine). This subsequently leads to the phosphorylation of MEK (extracellular signal regulated kinase)-like proteins and threonine-glutamate-tyrosine, and finally tyrosine phosphorylation of fibrous sheath proteins. This increase in cAMP causes hyperactivation of the spermatozoa. Only hyperactivated spermatozoa have increased motility to undergo acrosome reaction and acquire the characteristics required for successful fertilization. From these observations, it was deduced that ROS was involved [16,43,44].
2. Hyperactivation
Hyperactivation is a specific state of sperm motility when spermatozoa become highly motile. The process of hyperactivation is essential for successful fertilization and is considered a subcategory of capacitation. Hyperactive spermatozoa exhibit features of high amplitude, asymmetric flagellar movement, increased side-to-side head displacement, and non-linear motility [45]. The role of ROS in the initiation of hyperactivation has been well documented in vitro as was shown when spermatozoa were incubated with low concentrations of OH- induced hyperactivation [46].
3. Acrosome reaction
Once the hyperactivated spermatozoon passes the cumulus oophorus, it binds to the zona pellucida (ZP) of the oocyte and initiates an exocytotic release of proteolytic enzymes, creating a pore in ZP's extracellular matrix. The spermatozoa then penetrate this physical zona barrier and fuse with the oocyte [44]. The molecular events of the acrosome reaction overlap substantially with those of capacitation, including phosphorylation of similar tyrosine proteins, influx of Ca2+, and increased cAMP and PKA levels. The role of ROS in the in vivo acrosome reaction involves the spermatozoa's actions on the ZP via phosphorylation of three plasma membrane proteins. In vitro activation of the AR was also observed when physiological concentrations of O2-, H2O2, and NO were added to the seminal plasma [9]
4. Sperm-oocyte fusion
For successful fertilization, the spermatozoa must penetrate the ZP and fuse with the oocyte. High amounts of PUFAs, particularly docosahexaenoic acid (DHA), play a major role in regulating membrane fluidity in sperm. In studies of human spermatozoa, ROS has been shown to increase the membrane fluidity and rates of sperm-oocyte fusion, which occurs during the biochemical cascade of capacitation and acrosome reaction. Throughout capacitation, ROS inhibits protein tyrosine phosphatase activity and prevents dephosphorylation and deactivation of phospholipase A2 (PLA2). PLA2 cleaves the secondary fatty acid from the triglycerol backbone of the membrane phospholipid and increases the membrane's fluidity [47,48].
PATHOLOGICAL ROLES OF ROS
When the highly potent ROS overcomes the antioxidant defense systems and disrupts the intricate balance between ROS and antioxidants, pathological defects occur. Depending on the nature, amount, and duration of the ROS insult, these defects cause significant damage to biomolecules such as lipids, proteins, nucleic acids, and sugars [41].
1. Lipid peroxidation
Lipids are responsible for the fluidity of membrane layers and the changes that occur during capacitation in the female reproductive tract [49]. The plasma membrane of mammalian spermatozoa is markedly different from mammalian somatic cells in terms of its lipid composition. The plasma membrane contains high levels of lipids in the form of PUFAs. These lipids contain unconjugated double bonds separated by methylene groups. The placement of a double bond adjacent to a methylene group weakens the methyl carbon-hydrogen bond, consequently making hydrogen extremely susceptible to abstraction and oxidative damage. When the levels of ROS within the cell are high, ROS will attack PUFA, causing a cascade of chemical reactions called LPO [46]. Approximately 50% of the fatty acids in human spermatozoa are composed of DHA with 22-carbon chains and six cis double bonds. DHA is thought to play a major role in regulating spermatogenesis and membrane fluidity [13]. As the LPO cascade proceeds in the sperm, almost 60% of the fatty acid is lost from the membrane, hence affecting its function by decreasing its fluidity, increasing non-specific permeability to ions, and inactivating membrane-bound receptors and enzymes. Since LPO is an autocatalytic self-propagating reaction associated with abnormal fertilization, it is critical to understand the mechanism behind this process, which can be conveniently separated into three main steps, namely initiation, propagation, and termination [11].
Initiation involves the abstraction of hydrogen atoms associated with carbon-carbon double bonds, which results in free radical formation. These free radicals react with fatty acid chains and form lipid radicals, which then react with oxygen to form the peroxyl radicals. These peroxyl radicals, which can abstract hydrogen from lipid molecules, particularly in the presence of metals such as copper and iron, cause an autocatalytic chain reaction. The radicals eventually react with hydrogen to form lipid peroxides [4]. This reaction characterizes the propagation stage. These radicals act on additional lipids, forming cytotoxic aldehydes due to hydroperoxide degradation. Peroxyl and alkyl radicals are regenerated in a cyclical fashion in the propagation step until they react with another radical to form a stable end product called malondialdehyde (MDA) during the third step of termination. Thus, MDA is used in biochemical arrays to monitor the degree of peroxidative damage to spermatozoa [18,49]. Another byproduct of LPO is 4-hydroxynonenal, which is formed from low-density lipoproteins. Hydroxynonenals are hydrophilic and can cause severe cell dysfunction at both genomic and proteomic levels [5].
2. DNA damage
Semen parameters such as concentration, motility, and morphology are commonly used to determine the fertilization potential of sperm from an ejaculate. Although this provides a general overview of the quality of sperm, it does not provide information on one of the most important components of the reproductive outcome, DNA. Single- or double-stranded DNA breaks can be a source of differences in reproductive potential between fertile and infertile men [50].
It has been reported that chromatin in the sperm nucleus is vulnerable to oxidative damage, leading to base modifications and DNA fragmentation [50]. The chromatin of human spermatozoa has a highly condensed and organized structure. This is further packaged into nucleosomes and coiled into a solenoid. During the process of spermiogenesis, sperm chromatin undergoes a series of modifications in which histones are replaced with transition proteins and subsequently, protamines. DNA strands are condensed by the protamines and form the basic packaging unit of sperm chromatin called toroid. Toroids are further compacted by intra- and inter-molecular disulfide cross-links. This DNA compaction and organization help protect sperm chromatin from oxidative damage, making them particularly resistant to DNA damage [51]. However, in some cases where poor compaction and incomplete protamination of sperm chromatin exist, DNA is more vulnerable to OS and produces base-free sites, deletions, frame-shift mutations, DNA cross-links, and chromosomal rearrangements. Damaged DNA has been observed in testicular, epididymal, and ejaculated human spermatozoa [52]. Single- and double-stranded DNA breaks can be detected by using either the TUNEL or Comet Assay. Single-strand breaks are a direct result of oxidative damage on sperm DNA, while double-strand breaks may arise from exposure to 4-hydroxyl-2-nonenal- a major product of LPO [53]. It was discovered that 8-hydroxy-2-deoxyguanosine and two ethenonucleosides (1, N6-ethenoadenosine and 1, N6-ethenoguanosine) are the two major DNA adducts found in human sperm DNA, both of which have been considered key biomarkers of DNA damage caused by OS [54,55]. Despite these findings, DNA damage is not a cause for concern during intrauterine insemination and in vitro fertilization (IVF), because the coexisting LPO damage by ROS eliminates the possibility of fertilization. However, if normal natural selection is bypassed during intracytoplasmic sperm injection (ICSI), sperm with significant amounts of DNA damage have the opportunity to fertilize the oocyte [46]. When DNA is minimally damaged, spermatozoa can undergo self-repair and potentially regain the ability to fertilize the oocyte and proceed with development [56]. In fact, the oocyte is also capable of repairing damaged sperm DNA. In cases where the oocyte repair machinery is not sufficient to repair DNA damage, the embryo may fail to develop or implant in the uterus and can be naturally aborted. In other cases, the oocyte may successfully repair sperm DNA-strand breaks before the initiation of the first cleavage division, thereby producing normal offspring. It has been reported that 80% of the structural chromosomal aberrations are of paternal origin in humans [54]. DNA damage is a contributory factor to apoptosis, poor fertilization rate, high frequency of miscarriage, and morbidity in offspring [16].
3. Apoptosis
Another theory regarding sperm DNA damage and impaired fertilization is that of unsuccessful apoptosis. Apoptosis, also known as programmed cell death, is a physiological phenomenon characterized by cellular morphological and biochemical modifications that cause cells to die in a controlled manner [46]. During early development, apoptosis is important in the ontogeny of the germ line as a means of regulating the germ cell to Sertoli cell ratio. In adulthood, apoptosis plays a vital role in selectively destroying the premeiotic spermatogonia during the first round of spermatogenesis by preventing the overproduction of germ cells from seminiferous tubules in response to ROS [11]. During this process, the human ejaculate expresses various apoptotic markers that initiate apoptosis, some of which include Fas, phosphatidylserine (PS), Bcl-Xl, and p53. Fas is a type I membrane protein that belongs to the tumor necrosis factor-nerve growth factor receptor family and is secreted by the Sertoli cells located on the germ cell surface [24]. To further support this theory, the same study reported that the percentage of Fas-positive spermatozoa was as high as 50% in men with abnormal sperm parameters [24]. In addition, this apoptotic pathway activates the inner and outer mitochondrial membranes to cause the release of the signaling molecule cytochrome C, which triggers caspases, such as caspases 3 and 9, and annexin-V binding (Annexins are calcium-dependent phospholipid-binding proteins, which bind to PS). This pathway eventually leads to sperm apoptosis [57]. In an earlier study, it was reported that annexin-V staining was used to study the externalization of PS-a marker for early apoptosis. It was observed that mature spermatozoa from infertile patients with increased ROS levels had significantly higher levels of apoptosis than mature spermatozoa from the control group [58].
IMPAIRED SEMEN PARAMETERS
OS and the excessive production of ROS have been associated with impaired sperm motility, concentration, and morphology. These parameters are the most important predictors of an individual's potential to produce viable sperm [59]. Impaired motility may be the result of a cascade of events that occur during LPO, such as decreased axonemal protein phosphorylation and sperm immobilization. Another hypothesis for the cause of reduced sperm motility proposed is that when H2O2 diffuses across the cell membrane, enzyme activity is inhibited, decreasing NADPH levels and further limiting the antioxidant-defense mechanism of spermatozoa and membrane peroxidation [9,38,41]. A study conducted by du Plessis et al [60] revealed that human spermatozoa incubated and exposed to artificial H2O2 have detrimental effects on sperm motility and give rise to a significant increase in the overall ROS and NO levels. Furthermore, ROS generated by leukocytes or granulocytes have harmful effects on human spermatozoa, causing a marked loss of sperm motility and morphology and hence, reducing hyperactivation and oocyte penetration [61]. An in vitro study conducted by Aitken et al [62] demonstrated that artificial addition of lipid aldehydes, such as 4-hydroxy-2-nonenal (4HNE: α,β-unsaturated hydroxyalkenal, produced by LPO) and acrolein, resulted in the loss of motility and progressive motility in human spermatozoa. This is due to the ability of electrophilic lipid aldehydes to directly adduct onto proteins that regulate sperm movement. Another study evaluated the potential damage that radio frequency electromagnetic radiation (RF-EMR) emitted by mobile phones can cause on sperm parameters. It was found that the spermatozoa exposed to RF-EMR for the longest time periods decreased motility (particularly progressive motility), concentration, and viability [63].
The impact of higher levels of NO has been shown to be damaging to various sperm parameters. Various researchers have reported that the number of sperm bound to the ZP, and sperm motility and viability considerably decreased with the addition of sodium nitroprusside, as compared to the control group [64]. Studies have also demonstrated that there is a higher concentration of NO in the seminal plasma of infertile men than in that of fertile men, thereby resulting in the inhibition of capacitation and sperm oocyte binding [46,65].
Patients with decreased sperm concentrations (oligozoospermia) have minimal chances of fertilization, which can be correlated to increased ROS levels in their seminal plasma. As discussed earlier, pathological levels of ROS are known to cause apoptosis of spermatozoa, resulting in cell death and a reduced sperm count. A number of studies have indicated a higher percentage of apoptotic spermatozoa in oligoasthenozoospermic subjects than in normozoospermic men [16,66,67]. In fact, elevated levels of ROS, known to induce apoptosis, were reported in mature spermatozoa from infertile men as compared to fertile donors. In addition, the presence of ROS in patients with varicocele revealed a negative relationship between ROS and sperm concentration [57].
REACTIVE OXYGEN SPECIES IN AN ASSISTED REPRODUCTIVE SETTING
Advances in infertility treatment have led to the development of new and improved procedures. However, success rates have remained low because IVF settings are still unable to mimic the physiological conditions of an in vivo microenvironment. Three factors contributing to the accumulation of ROS in vitro are (1) the lack of endogenous defense mechanisms, (2) the exposure of spermatozoa to various manipulations, and (3) an environment that is susceptible to OS.
A potential source of ROS in the assisted reproductive setting (ART) media occurs during the preparation of semen, which can cause the activation of ROS production by immature spermatozoa. This occurs during centrifugation in the absence of antioxidant-rich seminal plasma or from contamination by leukocytes, oxygen partial pressure, light, culture media, cryopreservation, and thawing [68].
1. Culture media
Different culture media designed to mimic the physiological environment are used in ART treatments. The composition of the commercially available culture media, such as Ham's F-10, contains metallic ions (e.g., Fe2+ and Cu2+) that can independently facilitate ROS generation within spermatozoa and damage DNA by participating in the Fenton and Haber-Weiss reactions. Moreover, media additives like serum albumin contain high levels of amine oxidase, which leads to an increase in the H2O2 production [22,68].
2. Laboratory environment
Increased ROS production by spermatozoa can be initiated by and originate from various possible sources present in the ART laboratory during procedures. For instance, approximately 95% of the gas intake by incubators is directly from the environmental air, causing the partial pressure for oxygen (PO2) in the culture media to be much higher than what it normally is in vivo at the tissue level. It has been shown that at 37℃, the O2 concentration in a medium equilibrated with atmospheric oxygen inside an incubator is 20 times higher than the physiological intracellular O2 concentration. This higher-than-normal PO2 level activates various intracellular oxidase systems, which contribute to increased ROS generation [69]. Visible light may also lead to a higher-than-normal ROS production. Visible light induces photodynamic stress, causing potential oxidative damage to unsaturated lipids and cholesterol in the sperm membrane as well as DNA damage. Some researchers speculate that the generation of pathological ROS levels within spermatozoa depends on the duration of light exposure. Light exposure of more than 5 min has been shown to cause a significant increase in the H2O2 levels [70].
3. Assisted reproductive setting techniques
During ART, the gametes are manipulated and prepared in order to perform various types of fertilization procedures. This is one of the reasons why the cellular sources of ROS in conventional IVF are different from those of ICSI. Spermatozoa are routinely centrifuged during preparation. The centrifugation process has been shown to increase ROS production and cause OS in male gametes. In a study conducted by Agarwal et al [24], it was reported that the production of ROS by human spermatozoa increased significantly when spermatozoa were exposed to repeated cycles of centrifugation. Interestingly, the researchers observed that the duration of centrifugation was more important than the force of centrifugation, hence causing more DNA fragmentation with adverse consequences on ART.
Furthermore, it is known that the cryopreservation of spermatozoa can induce cellular damage and cause cells to lose their antioxidant defense systems [68]. After freeze-thawing cycles, the SOD activity was reduced by 50% in human spermatozoa, thus further enhancing the susceptibility of membranes to LPO by ROS [9,68].
MEASUREMENT OF OXIDATIVE STRESS
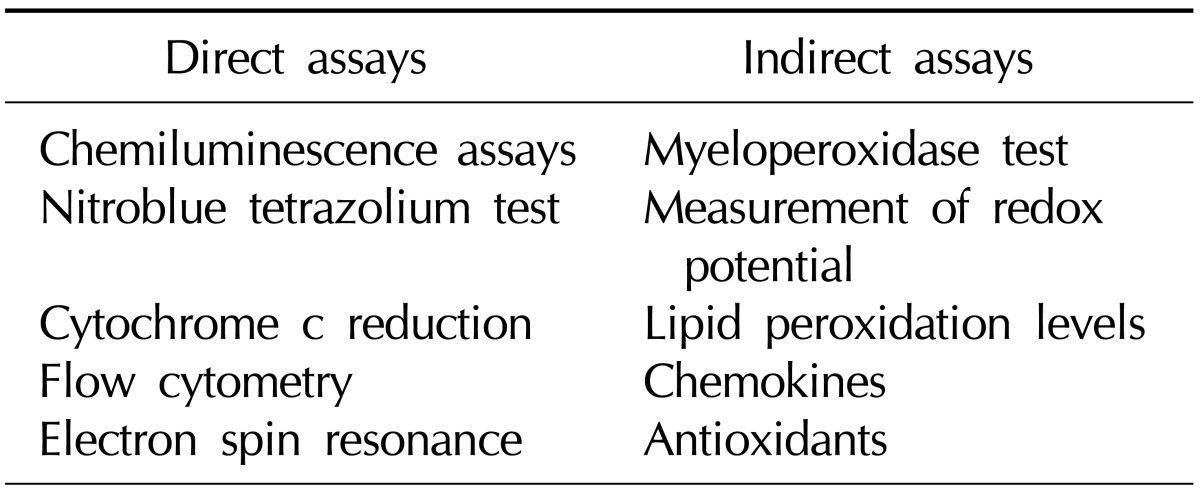
Over the last decade, research has provided growing support to indicate that excess ROS production leads to abnormal semen parameters and increased sperm damage. Standard semen analysis continues to be the backbone of clinical evaluation of male infertility. Studies have shown that ROS-mediated damage to sperm is a considerable contributing pathology in 30% to 80% of unselected infertile patients [11,46,68]. Therefore, it would be reasonable to expect the screening of all infertile men for the presence of increased ROS levels. However, the detection of the levels and sources of excess ROS production in semen is currently not included in the routine evaluation of subfertile men [67,71]. Some of the reasons include mere inconvenience, cost-effective and efficient assays, and, perhaps most importantly, the lack of a universally accepted analysis method. All three contribute to the widespread limitations when measuring ROS as part of a male infertility assessment, despite its importance. At present, over 30 different assays are used to measure ROS and the presence of OS in the semen of men (Table 1).
Table 1.
Various direct and indirect assays to measure reactive oxygen species human semen
1. Indication of sperm oxidative stress from routine semen analysis
Routine semen analyses have allowed clinicians to make a fairly accurate diagnosis of OS. A reduction in any of the semen parameters (count, motility, and morphology) is more frequently seen in men with OS. Asthenozoospermia is most likely the best surrogate marker for OS in a routine semen analysis. The hyperviscosity of seminal plasma is also associated with increased levels of seminal plasma MDA and reduced seminal plasma antioxidant status [72], making impaired viscosity a reasonable surrogate marker of OS [11]. In addition, infection of the semen with the bacterial microorganism Ureaplasma urealyticum is associated with increased seminal plasma viscosity and an increase in ROS production [73]. It is possible that these infections may damage the prostate and seminal vesicles, altering the substrates involved in maintaining normal semen viscosity. The indication and the presence of a large number of round cells imply possible OS caused by leukocytospermia. However, these round cells may be immature spermatozoa rather than leukocytes. For this reason, an accurate identification of these cells requires ancillary tests such as the peroxidase test, CD45 (transmembrane glycoprotein expressed at high levels on the cell surface) antibody staining or measurement of seminal elastase [74]. Abnormal sperm morphology related to ERC and cytoplasmic droplets are principal features of anomalous spermatozoa generating high levels of ROS. Lastly, poor sperm membrane integrity, which may be assessed by the hypo-osmotic swelling test (HOST), has been linked to the presence of OS [75].
2. Laboratory assessment of oxidative stress
As mentioned earlier, OS results from an imbalance between ROS production and the intracellular/extracellular antioxidants present in seminal plasma. Direct assays of OS measures the net oxidative result of this imbalance by detecting and measuring the amount of oxidation in the sperm cell membrane. MDA, which is one of the final products of membrane LPO, can be measured via the thiobarbituric acid assay, which is one of the oldest and most widely used direct assays for assessing sperm membrane oxidation. Various authors have reported that increased levels of MDA are associated with decreased sperm motility and sperm-oocyte fusion [41,67].
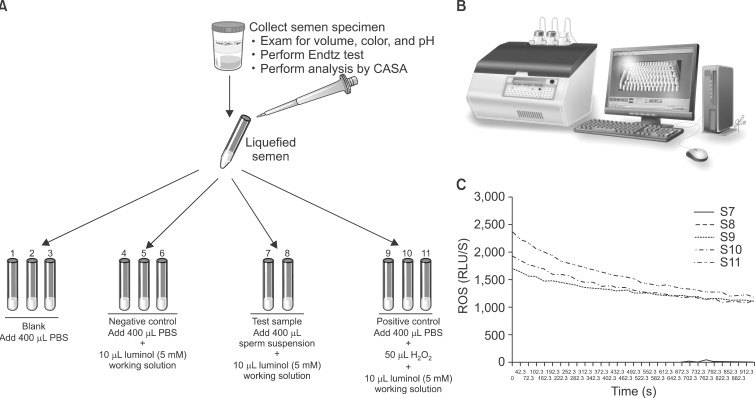
Chemiluminescence assays are most commonly used for measuring seminal ROS. A luminometer is used in conjunction with a chemiluminescent probe such as luminol (5-amino-2,3,-dihydro-1,4-phthalazinedione; Sigma-Aldrich, St. Louis, MO, USA). Aliquots of liquefied semen are centrifuged at 300× g for 7 minutes. Seminal plasma is aliquoted and frozen at -20℃ for a later measurement of the total antioxidant levels. The pellet is washed with phosphate-buffered saline (PBS, pH 7.4) and re-suspended in the same washing medium at a concentration of 2×106 sperm/mL. 400-µL aliquots of the resulting cell suspensions containing sperm and leukocytes are used to assess the basal ROS levels. A negative control is prepared by adding 10 mL of 5-mM luminol to 400 mL of PBS. Luminol (5-amino-2,3,-dihydro-1,4-phthalazinedione; Sigma), which is prepared as 5-mM stock in dimethyl sulfoxide, is added to the mixture and serves as a probe. All the test tubes are loaded into the luminometer for 15 minutes to assess the ROS levels [8]. Luminol is extremely sensitive and reacts with a variety of ROS at neutral pH [76]. It has the ability to measure both intracellular and extracellular ROS. The free radicals in the semen sample combine with luminol to generate a light signal that is converted to an electric signal (photon) by the luminometer (Fig. 3). The number of free radicals produced is measured as relative light units/s/106 sperm. Normal ROS levels in washed sperm suspensions range from 0.10 to 1.03×106 cpm per 20×106 sperm [77].
Fig. 3.
Measurement of reactive oxygen species (ROS) in sperm suspensions by chemiluminescence assay. (A) Preparation of the samples for ROS measurement. A total of 11 tubes are labeled from S1-S11: Blank, negative control, patient sample, and positive control. Luminol is added to all tubes except blank. Hydrogen peroxide is added only to the positive control. (B) Autolumat 953 plus luminometer used in the measurement of ROS by chemiluminescence assay. Multiple tubes can be loaded simultaneously for measuring ROS. The luminometer is connected to a computer and a monitor, and all the steps can be observed on the screen. (C) A typical graph showing the ROS levels in the 11 tubes (S1-S11). As can be seen, only positive controls have significantly higher levels of ROS. Those producing low levels (Tubes S1-S8) of ROS are seen very close to the X axis. ROS levels measured by the luminometer are expressed as relative light units/s (or RLU/s).
Luminol can also be used to indirectly measure the total antioxidant capacity (TAC) within the seminal plasma. TAC is then quantified against a vitamin E analog Trolox (a water-soluble tocopherol analog). The results are expressed as an ROS-TAC score, and this gives an indication of the combined antioxidant activities of all constituents, including vitamins, proteins, and lipids. This assay appears to be the best established method for analyzing the balance between ROS and the antioxidant protection of sperm [78]. However, the cost of performing this technique remains a hurdle to its use in clinical laboratories [66].
An assay that has gained popularity due to its cost-effectiveness and user-friendliness is nitroblue tetrazolium (NBT). This assay provides information on the source(s) of ROS. This technique involves only a light microscope and accurately predicts whether ROS has been produced by spermatozoa or leukocytes. When NBT interacts with the O2-. present within spermatozoa or leukocytes, it is converted into a blue pigment called diformazam. With the aid of a light microscope, the amount of diformazam can be observed, measured, and correlated to the intracellular ROS concentration [66,67].
Both direct and indirect assays have been used to quantify the levels of ROS. However, all assays of OS in the sperm are relatively expensive and time consuming as compared to a routine semen analysis. Therefore, many clinicians continue to avoid testing their patients for OS and by default offer therapeutic plans with the hope of relieving OS and improving the overall semen quality. It can be seen that an OS test may precisely distinguish between fertile and infertile men as well as clinically diagnose male factor infertility. Moreover, such tests can help identify subgroups of infertile patients suffering from OS that may be treated with antioxidant supplementation [71].
PREVENTION AND MANAGEMENT OF OXIDATIVE STRESS
As mentioned earlier, there are innate mechanisms in place to prevent OS from occurring in healthy males. However, in instances where these natural defenses fail to maintain the fine balance between ROS and antioxidants, measures can be taken to alleviate OS, such as lifestyle changes and antioxidant supplementation (both enzymatic and non-enzymatic).
1. Prevention of oxidative stress
In healthy males, sperm DNA is protected from OS by two main mechanisms. Firstly, the DNA is tightly coiled and packaged into chromatin such that the genetic material is minimally exposed to attack by ROS [69]. Secondly, natural antioxidants in the seminal plasma and spermatozoa assist in minimizing the ROS production to normal levels. Some natural antioxidants include enzymes like catalase and SOD as well as non-enzymatic compounds like vitamins C and E and carotenoids. These antioxidants react with and neutralize ROS, assisting in preventing OS onset and preserving the spermatozoa function [79]. Spermatozoa also contain the antioxidants lactoferrin and coenzyme Q10 [7]. A third lesser-mentioned protection mechanism is that of the prostasomes from the prostate. The presence of prostasomes in the seminal plasma results in a decreased ability of neutrophils to produce superoxide radicals [7].
To remain healthy, a sufficient amount of antioxidants must be consumed in one's diet to prevent OS from occurring [7]. However, in some patients who suffer from infertility, there may be either an overproduction of ROS or an underproduction of antioxidants, which disrupts the intricate balance and results in OS.
2. Management of oxidative stress
In the management of OS, the first step to take is to ascertain the underlying cause of the imbalance and treat it [80]. For instance, chlamydia infections can be treated with antibiotics and anti-inflammatory medication, while varicocele can be corrected by surgery [11]. Thereafter, antioxidant treatment may be given to supplement the natural antioxidants and increase the ability of the seminal plasma to combat OS [80]. The following section explores the different methods, including lifestyle changes and antioxidant supplements, which can be employed to help reduce OS.
1) Lifestyle changes
Modernization, affluence, and the accompanying stresses of the society have resulted in an increase in negative behaviors, including, but not limited to, smoking, substance abuse, obesity, and an unbalanced diet. All these have been shown to contribute to OS, and therefore, minimizing such detrimental behavior is likely to aid in alleviating OS [11].
It is also recognized that exposure to heat, pollution, toxins, and heavy metals play a role in the development of OS. In addition, any activity that may cause the scrotum's temperature to increase, such as hot baths, saunas, extended periods of driving, and long and sedentary office hours should be avoided. Lastly, adequate protective equipment and aeration should be ensured at work places to limit exposure to any chemical or vapor that may cause OS [11].
Undertaking these lifestyle changes can contribute to the reduction of the ROS production and help correct the imbalance causing OS.
2) Antioxidants
Another precautionary measure that can be taken is antioxidant supplementation. Antioxidants work by halting the oxidative chain reaction-eliminating, taking up, or reducing the formation of ROS [9]. They can be divided into two types on the basis of their actions: (1) preventive antioxidants are metal chelators or binding proteins, such as lactoferrin and transferrin, which prevent the formation of ROS; and (2) scavenging antioxidants, like vitamins C and E, remove the ROS that is already present [69]. There have been various studies conducted to elucidate the effectiveness of each individual antioxidant. However, results have been inconclusive as most experiments have a small sample size, differ in dosage and duration of therapy, and lack controls [81].
Moreover, antioxidants work cooperatively, and thus, it is extremely challenging to measure the effect of any single one alone [79]. This is supported in theory because a suitable combination of antioxidants with their different profiles will neutralize any ROS in its vicinity, hence resulting in an additive effect on the decrease in the total OS level of the body [10].
For the purpose of this review, antioxidants are categorized as enzymatic and non-enzymatic. Some enzymatic oxidants, or natural oxidants, include glutathione reductase (GSH), SOD, and catalase, while some non-enzymatic oxidants include vitamins C, E, and B; carotenoids; carnitines; cysteines, pentoxifylline, metals, taurine, hypotaurine, and albumin [9]. The non-enzymatic oxidants are acquired from fruits or vegetables containing the supplements [69]. Table 2 summarizes the mechanisms of action and the effects of the more important antioxidants used clinically.
Table 2.
Mechanisms of action and effects of various antioxidants
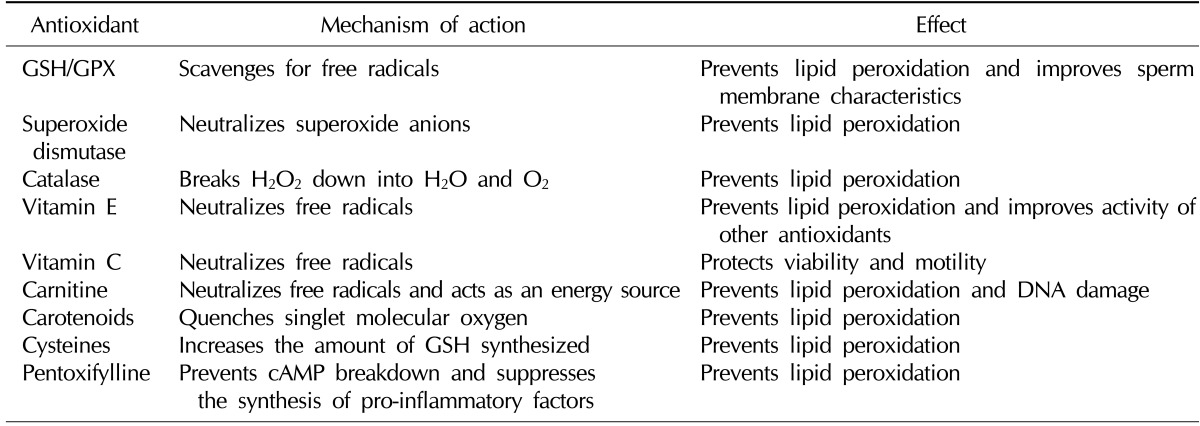
GSH: glutathione reductase, GPX: glutathione peroxidase, cAMP: cyclic adenosine 3',5'-monophosphate.
(1) Enzymatic antioxidants
① Glutathione reductase and glutathione peroxidase
GSH/glutathione peroxidase are the main reducing agents in the body and act as scavenging antioxidants in the epididymis and testes [82]. Their modification of the spermatozoa membrane confers protection on the lipid constituents, thus preserving sperm viability and motility [7]. Previous in vitro studies have shown that GSH preserves the tail-beat frequency, reduces LPO, and improves the sperm membrane characteristics [83].
② Superoxide dismutase and catalase
SOD protects sperm from superoxide anions by catalyzing the conversion of superoxide into oxygen and H2O2, thereby preventing LPO and improving motility [80]. On the other hand, catalase aids in the decomposition of H2O2 into water and oxygen [82]. Thus, both SOD and catalase assist in removing ROS that has the potential to damage sperm.
(2) Non-enzymatic antioxidants
① Vitamin E
Vitamin E (α-tocopherol) is a chain-breaking antioxidant found in the sperm's cell membrane and acts by neutralizing H2O2 and quenching free radicals [9], hence halting chain reactions that produce lipid peroxides and protecting the membrane from the damage induced by ROS [69]. Furthermore, it improves the activity of other scavenging oxidants [82]. In these ways, vitamin E helps to preserve both sperm motility and morphology [80].
② Vitamin C
Vitamin C (ascorbate) is another chain-breaking antioxidant that plays a significant role (up to 65%) in combatting OS in the seminal plasma [79]. It reacts with OH-, O2-, and H2O2 in the extracellular fluid, thus protecting sperm viability and motility [69]. However, vitamin C is only a weak ROS scavenger in the cell membrane and, hence, has almost no effect within the cell [7].
③ Carnitine
Carnitine is a water-soluble antioxidant commonly attained from dietary sources. It may participate in sperm motility as a fuel source by assisting free fatty acid utilization and preventing lipid oxidation [82]. Therefore, carnitine protects the sperm DNA and membranes from oxidative damage, and maintains the sperm viability and motility [79].
④ Carotenoids
Although carotenoids have short half-lives, they are very effective and efficient singlet molecular oxygen quenchers [84]. Two major carotenoids worth mentioning are β-carotene, which prevents lipids in the cell membrane from being peroxidized [9], and lycopene, which is the most potent and readily available carotenoid that prevents peroxidation in the seminal plasma [69].
⑤ Cysteines
Cysteines are precursors of intracellular GSH and therefore, increase the amount of GSH synthesized. GSH subsequently scavenges oxidants and prevents oxidative damage to the cell membrane and DNA [9]. N-acetyl-L-cysteine works via two mechanisms: (1) by boosting the amount of reducing agent produced and (2) ridding the spermatozoa of free radicals [82], thereby proserving sperm motility [10].
⑥ Pentoxifylline
Pentoxifylline acts as a competitive phosphodiesterase inhibitor and prevents the breakdown of intracellular cyclic adenosine monophosphate (cAMP). It also suppresses the synthesis of tumor necrosis factor-α (TNF-α) and leukotrienes and as a result, decreases the inflammation levels [82]. When the amount of superoxide produced by spermatozoa is decreased, less LPO occurs and sperm motility is preserved [81]. A study has also shown that a 1,200-mg dose of oral pentoxifylline daily results in increased motility and beat cross frequency [79].
(3) Other antioxidants
There are a few other minor antioxidants that contribute to relieving OS, such as albumin, taurine/hypotaurine, inositol, and some metals. Albumin, a plasma protein, also has antioxidative properties. It interacts with peroxyl radicals and prevents the chain reactions that generate more free radicals, hence reducing the ROS production and proserving sperm motility and viability [79]. Taurine is another non-enzymatic antioxidant that scavenges ROS, while inositol is known to enhance GSH activity and preserve normal sperm morphology [9]. Furthermore, certain metals have antioxidant properties. For example, selenium is an important component in the regular development and maturation of the testes and contributes to the protection of sperm DNA and cell membranes, particularly when used as an adjunct to vitamin E [85]. Additionally, zinc acts as a chelator and binds ROS [84], while manganese enhances sperm motility and viability [9].
3) Surgery
Varicocele refers to the abnormal dilation and elongation of the pampiniform plexus of veins around the spermatic cord [86]. Corrective surgery, involving the occlusion of these dilated veins, may be performed on subfertile males or men suffering from testicular aches and pains [87]. This has been shown to decrease the ROS levels in semen, thereby protecting the sperm membrane and DNA from oxidative damage [11]. Surgical repair also improves other biomarkers of infertility, including sperm parameters and pregnancy rates [87].
CONCLUSION
OS has been considered a major contributory factor to male infertility. Studies have demonstrated that low and controlled concentrations of ROS play an important role in normal sperm physiological processes such as capacitation, hyperactivation, acrosome reactions, and signaling processes to ensure appropriate fertilization. Moreover, there is growing evidence that an increase in OS significantly impairs sperm function. These impairments have resulted in male infertility via mechanisms involving the induction of peroxidative damage to the sperm plasma membrane, DNA damage, and apoptosis. ROS must be maintained at appropriate levels to ensure appropriate physiological function, while preventing pathological damage to the spermatozoa. When the natural balance between ROS and antioxidants is disturbed, the first restorative measure to be taken should be changes in lifestyle, such as cessation of smoking, limiting substance use, and maintaining a healthy and balanced diet. Antioxidant supplementation may then be taken together to improve the patient's health outcomes.
An accurate assessment of the seminal ROS levels should become an integral part of the andrology work-up of men in order to assist clinicians in elucidating the fertility status and thereby providing an optimal treatment regime for these patients.
ACKNOWLEDGEMENTS
This research was supported by funds from The Center for Reproductive Medicine, Glickman Urological & Kidney Institute, Cleveland Clinic (Cleveland, OH, USA).
References
- 1.Trussell JC. Optimal diagnosis and medical treatment of male infertility. Semin Reprod Med. 2013;31:235–236. doi: 10.1055/s-0033-1345269. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organisation. WHO Laboratory Manual for the Examination and Processing of Human Semen. 5th ed. Geneva: World Health Organization; 2010. [Google Scholar]
- 3.Agarwal A, Sekhon LH. Oxidative stress and antioxidants for idiopathic oligoasthenoteratospermia: is it justified? Indian J Urol. 2011;27:74–85. doi: 10.4103/0970-1591.78437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Saalu LC. The incriminating role of reactive oxygen species in idiopathic male infertility: an evidence based evaluation. Pak J Biol Sci. 2010;13:413–422. doi: 10.3923/pjbs.2010.413.422. [DOI] [PubMed] [Google Scholar]
- 5.Hampl R, Drábková P, Kanďár R, Stěpán J. Impact of oxidative stress on male infertility. Ceska Gynekol. 2012;77:241–245. [PubMed] [Google Scholar]
- 6.Henkel RR. Leukocytes and oxidative stress: dilemma for sperm function and male fertility. Asian J Androl. 2011;13:43–52. doi: 10.1038/aja.2010.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lanzafame FM, La Vignera S, Vicari E, Calogero AE. Oxidative stress and medical antioxidant treatment in male infertility. Reprod Biomed Online. 2009;19:638–659. doi: 10.1016/j.rbmo.2009.09.014. [DOI] [PubMed] [Google Scholar]
- 8.Saleh RA, Agarwal A. Oxidative stress and male infertility: from research bench to clinical practice. J Androl. 2002;23:737–752. [PubMed] [Google Scholar]
- 9.Bansal AK, Bilaspuri GS. Impacts of oxidative stress and antioxidants on semen functions. Vet Med Int. 2010;2010:686137. doi: 10.4061/2011/686137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gharagozloo P, Aitken RJ. The role of sperm oxidative stress in male infertility and the significance of oral antioxidant therapy. Hum Reprod. 2011;26:1628–1640. doi: 10.1093/humrep/der132. [DOI] [PubMed] [Google Scholar]
- 11.Tremellen K. Oxidative stress and male infertility--a clinical perspective. Hum Reprod Update. 2008;14:243–258. doi: 10.1093/humupd/dmn004. [DOI] [PubMed] [Google Scholar]
- 12.De Iuliis GN, Wingate JK, Koppers AJ, McLaughlin EA, Aitken RJ. Definitive evidence for the nonmitochondrial production of superoxide anion by human spermatozoa. J Clin Endocrinol Metab. 2006;91:1968–1975. doi: 10.1210/jc.2005-2711. [DOI] [PubMed] [Google Scholar]
- 13.Aitken RJ, Baker MA, De Iuliis GN, Nixon B. New insights into sperm physiology and pathology. Handb Exp Pharmacol. 2010;(198):99–115. doi: 10.1007/978-3-642-02062-9_7. [DOI] [PubMed] [Google Scholar]
- 14.Butler A, He X, Gordon RE, Wu HS, Gatt S, Schuchman EH. Reproductive pathology and sperm physiology in acid sphingomyelinase-deficient mice. Am J Pathol. 2002;161:1061–1075. doi: 10.1016/S0002-9440(10)64267-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miranda-Vilela AL, Alves PC, Akimoto AK, Pereira LC, Nazaré Klautau-Guimarães M, Grisolia CK. The effect of hydrogen peroxide-induced oxidative stress on leukocytes depends on age and physical training in healthy human subjects carrying the same genotypes of antioxidant enzymes' gene polymorphisms. Am J Hum Biol. 2010;22:807–812. doi: 10.1002/ajhb.21086. [DOI] [PubMed] [Google Scholar]
- 16.Chen SJ, Allam JP, Duan YG, Haidl G. Influence of reactive oxygen species on human sperm functions and fertilizing capacity including therapeutical approaches. Arch Gynecol Obstet. 2013;288:191–199. doi: 10.1007/s00404-013-2801-4. [DOI] [PubMed] [Google Scholar]
- 17.Hazout A, Menezo Y, Madelenat P, Yazbeck C, Selva J, Cohen-Bacrie P. Causes and clinical implications of sperm DNA damages. Gynecol Obstet Fertil. 2008;36:1109–1117. doi: 10.1016/j.gyobfe.2008.07.017. [DOI] [PubMed] [Google Scholar]
- 18.Sikka SC. Relative impact of oxidative stress on male reproductive function. Curr Med Chem. 2001;8:851–862. doi: 10.2174/0929867013373039. [DOI] [PubMed] [Google Scholar]
- 19.Sabeur K, Ball BA. Characterization of NADPH oxidase 5 in equine testis and spermatozoa. Reproduction. 2007;134:263–270. doi: 10.1530/REP-06-0120. [DOI] [PubMed] [Google Scholar]
- 20.Choudhary R, Chawala VK, Soni ND, Kumar J, Vyas RK. Oxidative stress and role of antioxidants in male infertility. Pak J Physiol. 2010;6:54–59. [Google Scholar]
- 21.Esteves SC. Effect of cigarette smoking on levels of seminal oxidative stress in infertile men: a prospective study. Int Braz J Urol. 2002;28:484–485. [PubMed] [Google Scholar]
- 22.Saleh RA, Agarwal A, Nada EA, El-Tonsy MH, Sharma RK, Meyer A, et al. Negative effects of increased sperm DNA damage in relation to seminal oxidative stress in men with idiopathic and male factor infertility. Fertil Steril. 2003;79(Suppl 3):1597–1605. doi: 10.1016/s0015-0282(03)00337-6. [DOI] [PubMed] [Google Scholar]
- 23.Lavranos G, Balla M, Tzortzopoulou A, Syriou V, Angelopoulou R. Investigating ROS sources in male infertility: a common end for numerous pathways. Reprod Toxicol. 2012;34:298–307. doi: 10.1016/j.reprotox.2012.06.007. [DOI] [PubMed] [Google Scholar]
- 24.Agarwal A, Saleh RA, Bedaiwy MA. Role of reactive oxygen species in the pathophysiology of human reproduction. Fertil Steril. 2003;79:829–843. doi: 10.1016/s0015-0282(02)04948-8. [DOI] [PubMed] [Google Scholar]
- 25.Lu JC, Huang YF, Lü NQ. WHO Laboratory Manual for the Examination and Processing of Human Semen: its applicability to andrology laboratories in China. Zhonghua Nan Ke Xue. 2010;16:867–871. [PubMed] [Google Scholar]
- 26.Nandipati KC, Pasqualotto FF, Thomas AJ, Jr, Agarwal A. Relationship of interleukin-6 with semen characteristics and oxidative stress in vasectomy reversal patients. Andrologia. 2005;37:131–134. doi: 10.1111/j.1439-0272.2005.00668.x. [DOI] [PubMed] [Google Scholar]
- 27.Rengan AK, Agarwal A, van der Linde M, du Plessis SS. An investigation of excess residual cytoplasm in human spermatozoa and its distinction from the cytoplasmic droplet. Reprod Biol Endocrinol. 2012;10:92. doi: 10.1186/1477-7827-10-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Will MA, Swain J, Fode M, Sonksen J, Christman GM, Ohl D. The great debate: varicocele treatment and impact on fertility. Fertil Steril. 2011;95:841–852. doi: 10.1016/j.fertnstert.2011.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shiraishi K, Matsuyama H, Takihara H. Pathophysiology of varicocele in male infertility in the era of assisted reproductive technology. Int J Urol. 2012;19:538–550. doi: 10.1111/j.1442-2042.2012.02982.x. [DOI] [PubMed] [Google Scholar]
- 30.Agarwal A, Deepinder F, Sharma RK, Ranga G, Li J. Effect of cell phone usage on semen analysis in men attending infertility clinic: an observational study. Fertil Steril. 2008;89:124–128. doi: 10.1016/j.fertnstert.2007.01.166. [DOI] [PubMed] [Google Scholar]
- 31.Aitken RJ, Bennetts LE, Sawyer D, Wiklendt AM, King BV. Impact of radio frequency electromagnetic radiation on DNA integrity in the male germline. Int J Androl. 2005;28:171–179. doi: 10.1111/j.1365-2605.2005.00531.x. [DOI] [PubMed] [Google Scholar]
- 32.De Iuliis GN, Newey RJ, King BV, Aitken RJ. Mobile phone radiation induces reactive oxygen species production and DNA damage in human spermatozoa in vitro. PLoS One. 2009;4:e6446. doi: 10.1371/journal.pone.0006446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Esfandiari N, Saleh RA, Blaut AP, Sharma RK, Nelson DR, Thomas AJ, Jr, et al. Effects of temperature on sperm motion characteristics and reactive oxygen species. Int J Fertil Womens Med. 2002;47:227–233. [PubMed] [Google Scholar]
- 34.Pant N, Shukla M, Kumar Patel D, Shukla Y, Mathur N, Kumar Gupta Y, et al. Correlation of phthalate exposures with semen quality. Toxicol Appl Pharmacol. 2008;231:112–116. doi: 10.1016/j.taap.2008.04.001. [DOI] [PubMed] [Google Scholar]
- 35.Latini G, Del Vecchio A, Massaro M, Verrotti A, De Felice C. Phthalate exposure and male infertility. Toxicology. 2006;226:90–98. doi: 10.1016/j.tox.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 36.Kasahara E, Sato EF, Miyoshi M, Konaka R, Hiramoto K, Sasaki J, et al. Role of oxidative stress in germ cell apoptosis induced by di(2-ethylhexyl)phthalate. Biochem J. 2002;365:849–856. doi: 10.1042/BJ20020254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jurasović J, Cvitković P, Pizent A, Colak B, Telisman S. Semen quality and reproductive endocrine function with regard to blood cadmium in Croatian male subjects. Biometals. 2004;17:735–743. doi: 10.1007/s10534-004-1689-7. [DOI] [PubMed] [Google Scholar]
- 38.Saleh RA, Agarwal A, Sharma RK, Nelson DR, Thomas AJ., Jr Effect of cigarette smoking on levels of seminal oxidative stress in infertile men: a prospective study. Fertil Steril. 2002;78:491–499. doi: 10.1016/s0015-0282(02)03294-6. [DOI] [PubMed] [Google Scholar]
- 39.Jarow JP. Semen quality of male smokers and nonsmokers in infertile couples. J Urol. 2003;170:675–676. [PubMed] [Google Scholar]
- 40.Kiziler AR, Aydemir B, Onaran I, Alici B, Ozkara H, Gulyasar T, et al. High levels of cadmium and lead in seminal fluid and blood of smoking men are associated with high oxidative stress and damage in infertile subjects. Biol Trace Elem Res. 2007;120:82–91. doi: 10.1007/s12011-007-8020-8. [DOI] [PubMed] [Google Scholar]
- 41.Agarwal A, Prabakaran SA. Mechanism, measurement, and prevention of oxidative stress in male reproductive physiology. Indian J Exp Biol. 2005;43:963–974. [PubMed] [Google Scholar]
- 42.Tsai WW, Niessen S, Goebel N, Yates JR, 3rd, Guccione E, Montminy M. PRMT5 modulates the metabolic response to fasting signals. Proc Natl Acad Sci U S A. 2013;110:8870–8875. doi: 10.1073/pnas.1304602110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kothari S, Thompson A, Agarwal A, du Plessis SS. Free radicals: their beneficial and detrimental effects on sperm function. Indian J Exp Biol. 2010;48:425–435. [PubMed] [Google Scholar]
- 44.de Lamirande E, O'Flaherty C. Sperm activation: role of reactive oxygen species and kinases. Biochim Biophys Acta. 2008;1784:106–115. doi: 10.1016/j.bbapap.2007.08.024. [DOI] [PubMed] [Google Scholar]
- 45.Suarez SS. Control of hyperactivation in sperm. Hum Reprod Update. 2008;14:647–657. doi: 10.1093/humupd/dmn029. [DOI] [PubMed] [Google Scholar]
- 46.Makker K, Agarwal A, Sharma R. Oxidative stress & male infertility. Indian J Med Res. 2009;129:357–367. [PubMed] [Google Scholar]
- 47.Calamera J, Buffone M, Ollero M, Alvarez J, Doncel GF. Superoxide dismutase content and fatty acid composition in subsets of human spermatozoa from normozoospermic, asthenozoospermic, and polyzoospermic semen samples. Mol Reprod Dev. 2003;66:422–430. doi: 10.1002/mrd.10368. [DOI] [PubMed] [Google Scholar]
- 48.Khosrowbeygi A, Zarghami N. Fatty acid composition of human spermatozoa and seminal plasma levels of oxidative stress biomarkers in subfertile males. Prostaglandins Leukot Essent Fatty Acids. 2007;77:117–121. doi: 10.1016/j.plefa.2007.08.003. [DOI] [PubMed] [Google Scholar]
- 49.Sanocka D, Kurpisz M. Reactive oxygen species and sperm cells. Reprod Biol Endocrinol. 2004;2:12. doi: 10.1186/1477-7827-2-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zribi N, Chakroun NF, Elleuch H, Abdallah FB, Ben Hamida AS, Gargouri J, et al. Sperm DNA fragmentation and oxidation are independent of malondialdheyde. Reprod Biol Endocrinol. 2011;9:47. doi: 10.1186/1477-7827-9-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Schulte RT, Ohl DA, Sigman M, Smith GD. Sperm DNA damage in male infertility: etiologies, assays, and outcomes. J Assist Reprod Genet. 2010;27:3–12. doi: 10.1007/s10815-009-9359-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kemal Duru N, Morshedi M, Oehninger S. Effects of hydrogen peroxide on DNA and plasma membrane integrity of human spermatozoa. Fertil Steril. 2000;74:1200–1207. doi: 10.1016/s0015-0282(00)01591-0. [DOI] [PubMed] [Google Scholar]
- 53.Badouard C, Ménézo Y, Panteix G, Ravanat JL, Douki T, Cadet J, et al. Determination of new types of DNA lesions in human sperm. Zygote. 2008;16:9–13. doi: 10.1017/S0967199407004340. [DOI] [PubMed] [Google Scholar]
- 54.González-Marín C, Gosálvez J, Roy R. Types, causes, detection and repair of DNA fragmentation in animal and human sperm cells. Int J Mol Sci. 2012;13:14026–14052. doi: 10.3390/ijms131114026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Valavanidis A, Vlachogianni T, Fiotakis C. 8-hydroxy-2'-deoxyguanosine (8-OHdG): a critical biomarker of oxidative stress and carcinogenesis. J Environ Sci Health C Environ Carcinog Ecotoxicol Rev. 2009;27:120–139. doi: 10.1080/10590500902885684. [DOI] [PubMed] [Google Scholar]
- 56.Aitken RJ, Koppers AJ. Apoptosis and DNA damage in human spermatozoa. Asian J Androl. 2011;13:36–42. doi: 10.1038/aja.2010.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Aitken RJ, Baker MA. Causes and consequences of apoptosis in spermatozoa; contributions to infertility and impacts on development. Int J Dev Biol. 2013;57:265–272. doi: 10.1387/ijdb.130146ja. [DOI] [PubMed] [Google Scholar]
- 58.Agarwal A, Said TM. Role of sperm chromatin abnormalities and DNA damage in male infertility. Hum Reprod Update. 2003;9:331–345. doi: 10.1093/humupd/dmg027. [DOI] [PubMed] [Google Scholar]
- 59.Kao SH, Chao HT, Chen HW, Hwang TI, Liao TL, Wei YH. Increase of oxidative stress in human sperm with lower motility. Fertil Steril. 2008;89:1183–1190. doi: 10.1016/j.fertnstert.2007.05.029. [DOI] [PubMed] [Google Scholar]
- 60.du Plessis SS, McAllister DA, Luu A, Savia J, Agarwal A, Lampiao F. Effects of H(2)O(2) exposure on human sperm motility parameters, reactive oxygen species levels and nitric oxide levels. Andrologia. 2010;42:206–210. doi: 10.1111/j.1439-0272.2009.00980.x. [DOI] [PubMed] [Google Scholar]
- 61.Koppers AJ, Mitchell LA, Wang P, Lin M, Aitken RJ. Phosphoinositide 3-kinase signalling pathway involvement in a truncated apoptotic cascade associated with motility loss and oxidative DNA damage in human spermatozoa. Biochem J. 2011;436:687–698. doi: 10.1042/BJ20110114. [DOI] [PubMed] [Google Scholar]
- 62.Aitken RJ, Whiting S, De Iuliis GN, McClymont S, Mitchell LA, Baker MA. Electrophilic aldehydes generated by sperm metabolism activate mitochondrial reactive oxygen species generation and apoptosis by targeting succinate dehydrogenase. J Biol Chem. 2012;287:33048–33060. doi: 10.1074/jbc.M112.366690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.La Vignera S, Condorelli RA, Vicari E, D'Agata R, Calogero AE. Effects of the exposure to mobile phones on male reproduction: a review of the literature. J Androl. 2012;33:350–356. doi: 10.2164/jandrol.111.014373. [DOI] [PubMed] [Google Scholar]
- 64.Miraglia E, De Angelis F, Gazzano E, Hassanpour H, Bertagna A, Aldieri E, et al. Nitric oxide stimulates human sperm motility via activation of the cyclic GMP/protein kinase G signaling pathway. Reproduction. 2011;141:47–54. doi: 10.1530/REP-10-0151. [DOI] [PubMed] [Google Scholar]
- 65.Doshi SB, Khullar K, Sharma RK, Agarwal A. Role of reactive nitrogen species in male infertility. Reprod Biol Endocrinol. 2012;10:109. doi: 10.1186/1477-7827-10-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Agarwal A, Makker K, Sharma R. Clinical relevance of oxidative stress in male factor infertility: an update. Am J Reprod Immunol. 2008;59:2–11. doi: 10.1111/j.1600-0897.2007.00559.x. [DOI] [PubMed] [Google Scholar]
- 67.Kefer JC, Agarwal A, Sabanegh E. Role of antioxidants in the treatment of male infertility. Int J Urol. 2009;16:449–457. doi: 10.1111/j.1442-2042.2009.02280.x. [DOI] [PubMed] [Google Scholar]
- 68.Agarwal A, Said TM, Bedaiwy MA, Banerjee J, Alvarez JG. Oxidative stress in an assisted reproductive techniques setting. Fertil Steril. 2006;86:503–512. doi: 10.1016/j.fertnstert.2006.02.088. [DOI] [PubMed] [Google Scholar]
- 69.Lampiao F. Free radicals generation in an in vitro fertilization setting and how to minimize them. World J Obstet Gynecol. 2012;1:29–34. [Google Scholar]
- 70.du Plessis SS, Makker K, Desai NR, Agarwal A. Impact of oxidative stress on IVF. Obstet Gynecol. 2008;34:539–554. [Google Scholar]
- 71.Deepinder F, Cocuzza M, Agarwal A. Should seminal oxidative stress measurement be offered routinely to men presenting for infertility evaluation? Endocr Pract. 2008;14:484–491. doi: 10.4158/EP.14.4.484. [DOI] [PubMed] [Google Scholar]
- 72.Aydemir B, Onaran I, Kiziler AR, Alici B, Akyolcu MC. The influence of oxidative damage on viscosity of seminal fluid in infertile men. J Androl. 2008;29:41–46. doi: 10.2164/jandrol.107.003046. [DOI] [PubMed] [Google Scholar]
- 73.Wang Y, Liang CL, Wu JQ, Xu C, Qin SX, Gao ES. Do Ureaplasma urealyticum infections in the genital tract affect semen quality? Asian J Androl. 2006;8:562–568. doi: 10.1111/j.1745-7262.2006.00190.x. [DOI] [PubMed] [Google Scholar]
- 74.Zorn B, Sesek-Briski A, Osredkar J, Meden-Vrtovec H. Semen polymorphonuclear neutrophil leukocyte elastase as a diagnostic and prognostic marker of genital tract inflammation--a review. Clin Chem Lab Med. 2003;41:2–12. doi: 10.1515/CCLM.2003.002. [DOI] [PubMed] [Google Scholar]
- 75.Menkveld R. Clinical significance of the low normal sperm morphology value as proposed in the fifth edition of the WHO Laboratory Manual for the Examination and Processing of Human Semen. Asian J Androl. 2010;12:47–58. doi: 10.1038/aja.2009.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Aitken RJ, Baker MA, O'Bryan M. Shedding light on chemiluminescence: the application of chemiluminescence in diagnostic andrology. J Androl. 2004;25:455–465. doi: 10.1002/j.1939-4640.2004.tb02815.x. [DOI] [PubMed] [Google Scholar]
- 77.Benjamin D, Sharma RK, Moazzam A, Agarwal A. Methods for the detection of ROS in human sperm samples. In: Agarwal A, Aitken RJ, Alvarez JG, editors. Studies on Men's Health and Fertility. New York: Humana Press; 2012. pp. 257–274. [Google Scholar]
- 78.Jamsai D, O'Bryan MK. Genome-wide ENU mutagenesis for the discovery of novel male fertility regulators. Syst Biol Reprod Med. 2010;56:246–259. doi: 10.3109/19396361003706424. [DOI] [PubMed] [Google Scholar]
- 79.Sharma RK, Agarwal A. Role of reactive oxygen species in male infertility. Urology. 1996;48:835–850. doi: 10.1016/s0090-4295(96)00313-5. [DOI] [PubMed] [Google Scholar]
- 80.Agarwal A, Nallella KP, Allamaneni SS, Said TM. Role of antioxidants in treatment of male infertility: an overview of the literature. Reprod Biomed Online. 2004;8:616–627. doi: 10.1016/s1472-6483(10)61641-0. [DOI] [PubMed] [Google Scholar]
- 81.Zini A, Al-Hathal N. Antioxidant therapy in male infertility: fact or fiction? Asian J Androl. 2011;13:374–381. doi: 10.1038/aja.2010.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Mora-Esteves C, Shin D. Nutrient supplementation: improving male fertility fourfold. Semin Reprod Med. 2013;31:293–300. doi: 10.1055/s-0033-1345277. [DOI] [PubMed] [Google Scholar]
- 83.Griveau JF, Le Lannou D. Effects of antioxidants on human sperm preparation techniques. Int J Androl. 1994;17:225–231. doi: 10.1111/j.1365-2605.1994.tb01247.x. [DOI] [PubMed] [Google Scholar]
- 84.Sies H. Strategies of antioxidant defense. Eur J Biochem. 1993;215:213–219. doi: 10.1111/j.1432-1033.1993.tb18025.x. [DOI] [PubMed] [Google Scholar]
- 85.Lombardo F, Sansone A, Romanelli F, Paoli D, Gandini L, Lenzi A. The role of antioxidant therapy in the treatment of male infertility: an overview. Asian J Androl. 2011;13:690–697. doi: 10.1038/aja.2010.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Agarwal A, Hamada A, Esteves SC. Insight into oxidative stress in varicocele-associated male infertility: part 1. Nat Rev Urol. 2012;9:678–690. doi: 10.1038/nrurol.2012.197. [DOI] [PubMed] [Google Scholar]
- 87.Hamada A, Esteves SC, Agarwal A. Insight into oxidative stress in varicocele-associated male infertility: part 2. Nat Rev Urol. 2013;10:26–37. doi: 10.1038/nrurol.2012.198. [DOI] [PubMed] [Google Scholar]