Abstract
Background
Argentina’s congress passed a tobacco control law that would enforce 100% smoke-free environments for the entire country, strong and pictorial health warnings on tobacco products and a comprehensive advertising ban. However, the Executive Branch continues to review the law and it has not been fully implemented. Our objective was to project the potential impact of full implementation of this tobacco control legislation on cardiovascular disease.
Methods
The Coronary Heart Disease (CHD) Policy Model was used to project future cardiovascular events. Data sources for the model included vital statistics, morbidity and mortality data, and tobacco use estimates from the National Risk Factor Survey. Estimated effectiveness of interventions was based on a literature review. Results were expressed as life-years, myocardial infarctions and strokes saved in an 8-year-period between 2012 and 2020. In addition we projected the incremental effectiveness on the same outcomes of a tobacco price increase not included in the law.
Results
In the period 2012–2020, 7500 CHD deaths, 16 900 myocardial infarctions and 4300 strokes could be avoided with the full implementation and enforcement of this law. Annual per cent reduction would be 3% for CHD deaths, 3% for myocardial infarctions and 1% for stroke. If a tobacco price increase is implemented the projected avoided CHD deaths, myocardial infarctions and strokes would be 15 500, 34 600 and 11 900, respectively.
Conclusions
Implementation of the tobacco control law would produce significant public health benefits in Argentina. Strong advocacy is needed at national and international levels to get this law implemented throughout Argentina.
INTRODUCTION
Cardiovascular diseases are the leading cause of death in the world.1 Tobacco use is the single most preventable cause of death2 and the promotion of interventions to reduce tobacco use is among the objectives of the WHO Action Plan for the Global Strategy for the Prevention and Control of Noncommunicable Diseases.1 The WHO Framework Convention on Tobacco Control (FCTC)3 and the MPOWER package2 recommend that countries adopt effective tobacco control interventions. Although tobacco use causes 5 million deaths annually, the set of tobacco control interventions that have proven to be effective only protect 5% of the World’s population.2
The situation in Argentina is similar. Although Argentina’s Congress did not ratify the FCTC despite presidential endorsement, several local and provincial governments have enacted smoke-free laws during the last decade. In 2011 the Congress approved a national tobacco control law that included a complete advertising ban, FCTC compliant health warnings and 100% smoke-free environments, applicable to the entire country. However, at this time the national tobacco control law is held up, awaiting authorisation by the Executive Branch before full implementation. If this law is implemented in all provinces, a significant impact on tobacco consumption and related morbidity and mortality could follow in a few years.
Therefore, the aim of this study is to estimate the impact on cardiovascular disease (morbidity and mortality) of the national tobacco control law if it were implemented, and estimate the incremental impact of a price increase on tobacco if implemented in addition to the approved law.
METHODS
To estimate the impact of the interventions we used the Coronary Heart Disease (CHD) Policy Model-Argentina. The CHD Policy Model is a national scale, state-transition (Markov) computer simulation model of the CHD incidence, prevalence, mortality and costs in adults 35–84 years of age.4 The model has been used to describe the trends in CHD and the effectiveness and cost-savings gained from population-wide policies aimed at tobacco control,5 and dietary salt.6 The CHD Policy Model has been successfully adapted to create national cardiovascular disease models for China7 and Argentina.8 The model used for this analysis was adapted to also project stroke events in Argentine adults.
The model has three submodels: demographic–epidemiological, bridge and disease-history. The demographic–epidemiological submodel predicts the incidence of CHD and the rates of death due to causes other than CHD among persons without a history of CHD. CHD and stroke events are predicted based on age, sex and the following six factors: smoking status (active smoker or secondhand smoke exposed), systolic blood pressure (SBP), body mass index (BMI), level of high density lipoprotein (HDL) cholesterol, level of low density lipoprotein (LDL) cholesterol and presence or absence of diabetes mellitus. For persons in whom CHD develops, the bridge submodel characterises the initial CHD event and related events for 30 days. The disease-history submodel then predicts the rate of subsequent CHD events and death rates from CHD and deaths not related to CHD among simulated subjects with CHD, with each category stratified according to age, sex and history of events. A summary of data sources for the CHD Policy Model-Argentina follows, but a detailed description of data sources, calibration and mechanics of the methodology used are included in an online appendix.
Data sources for CHD policy model-Argentina
Population
The estimated population of Argentina aged 35–84 years in the year 2010, by age and sex, and 35-year-olds arriving 2011–2020 was obtained from the Argentina National Statistics and Census Institute.9
Mortality
Cause-specific mortality data by year, age and sex were obtained from the Statistics and Information Department, Ministry of Health10 for the years 1997–2009. The CHD Policy Model-Argentina defined CHD as myocardial infarction (MI) (ICD-10 I21, I22), angina and other CHD (ICD-10 I20, I23-I25), and a fixed proportion of poorly defined cardiovascular disease coded events and deaths (ICD-10 I472, I490, I46, I50, I514, I515, I519 and I709). Stroke deaths were defined using ICD-10 codes I60-I69.
Cardiovascular disease incidence, case-fatality, and prevalence
Total stroke incidence, case-fatality, non-cardiovascular death and prevalence were obtained from local data for the CHD Policy Model-Argentina whenever possible. Incidence of acute MI was obtained from a population-based MI registry in a Buenos Aires district11 and incidence of total stroke from national vital statistics and a hospital admission database maintained by the Ministry of Health of Argentina.10 Incident cases of stable angina without MI were assumed to be non-fatal, and cases of incident out-of-hospital ischaemic cardiac arrest (with or without MI) were assumed to be universally fatal. Inhospital case-fatality was obtained from an Argentine national hospital survey12 and the Ministry of Health admissions database.10 Overall MI case-fatality (including both out-of-hospital ischaemic cardiac arrest and inhospital CHD deaths) was estimated using the Policy Model after first entering incident CHD, hospitalised MI case-fatality, and overall death rates for CHD and non-CHD. Stroke inhospital case-fatality was obtained from an Argentine national registry13 and administrative data. MI and stroke prevalence were obtained from a population-based risk factor telephone survey in Buenos Aires, done by the Ministry of Health.14
Non-cardiovascular mortality
Non-cardiovascular mortality was obtained from national vital statistics10 for the same period. Attributable mortality due to tobacco was included in the model using attributable fractions for different causes, combining tobacco use prevalence and relative risks, whenever possible using local risk estimates, but mostly relative risks were provided by the Cancer Prevention Study II.15
Tobacco use and other cardiovascular risk factors
Age and sex-specific prevalence for smoking and exposure to secondhand smoke (SHS), as well as BMI were obtained from the 2009 Second National Risk Factor Survey (Encuesta Nacional de Factores de Riesgo)16 using a tobacco questionnaire adapted from World Health Organisation and Pan American Health Organisation instruments and validated for Argentina.17 Means of SBP, LDL cholesterol and HDL cholesterol were obtained from Argentina’s sample of participants in the Cardiovascular Risk Factor Multiple Evaluation in Latin America Study, a stratified random sample of men and women aged 25–64 years in the city of Buenos Aires during 2004–2005.18
Cardiovascular disease event prediction
For the main simulations, multivariate risk equations were estimated from US Framingham Heart Study data19 with CHD (including stable or unstable angina, non-fatal MI, fatal MI or arrest) or stroke events (ischaemic stroke, including transient ischaemic attack, plus haemorrhagic stroke)20 as the outcome. Risk coefficients for age, sex, SBP, smoking status, LDL, HDL, diabetes and BMI were estimated in the CHD prediction model and age, sex, SBP, smoking status and diabetes in the total stroke model.20 Statistically significant (p<0.05) age-by-risk-factor interactions were incorporated into age-specific risk factor coefficients. Risk factor beta coefficients were estimated from examinations 9 to 13, 24 and 25 from the original Framingham Heart Study cohort and 1–6 from the Framingham offspring cohort, including participants for whom adequate data were available for a time-dependent logistic regression analysis. In order to model competing mortality risk, a separate non-CHD death equation was also estimated from Framingham data including age, sex, SBP, diabetes and smoking status.
Attributable risk analysis
Annual risk for CHD is calculated for each model cell by a multivariate logistic regression equation. Therefore the annual risk for events is determined by the age, sex and risk factor relative levels assigned to that cell, and the combined multiplicative effect of the risk factor coefficients. The overall proportion of CHD events explained by the selected major risk factors was obtained by simultaneously setting all of the risk factors to the minimum risk exposure level for the entirety of the 10-year simulation and comparing with a base case in which risk factor levels stayed constant at year 2010 levels. The resulting attributable proportions reflect a hypothetical scenario in which all risk factor exposures are removed at the same time, rather than removing the effect of single risk factors once at a time. Table 1 summarises data sources and a more detailed model structure, inputs and methodology could be found in the online appendix.
Table 1.
Model inputs for the CHD Policy Model Argentina
| Variable | Source |
|---|---|
| Population of Argentina and incoming 35-year-old persons, 2010–2050 | 2010 Census; http://www.indec.gov.ar |
| Incidence | |
| CHD | Incidence of hospitalised AMI: Caccavo et al, 2007 |
| Total stroke | Incidence of stroke: national vital statistics and hospital admission registry, Ministry of Health, Argentina |
| Prevalence of CHD in 2010 | Pilot test for the non-communicable diseases telephone surveillance system, Ministry of Health |
| Total and cause-specific mortality | |
| Total | National vital statistics, http://www.indec.gov.ar, all deaths in adults age 35–84 years |
| CHD | 1997–2009 vital statistics; using CHD ICD-10 codes I20–25 and 2000 Global Burden of Disease ‘garbage code’ definitions for a proportion of CHD deaths (see text) |
| Stroke | 1997–2009 vital statistics; using stroke ICD-10 codes I60–69 |
| CHD risk factor means and joint distributions, 2010 | Cardiovascular Risk Factor Multiple Evaluation in Latin America (CARMELA) Study and Segunda Encuesta Nacional de Factores de Riesgo (Second Argentine National Risk Factor Survey) |
| Risk factor hazards for CHD and stroke | Framingham Heart Study (USA) |
| One-day and 28-day CHD case-fatality | |
| CHD | Blanco P et al Encuesta de SAC, 2007 |
| In-hospital | |
| Stroke | |
| In-hospital | Argentinian National Stroke Registry (ReNACer) |
| 28-day case fatality | Proyecto investigacion de Stroke en Chile: Iquique Stroke Study (PISCIS) |
CHD, coronary heart disease
Effectiveness of the tobacco control interventions
We performed a literature review to obtain estimates of the effect of each individual component of the law at reducing tobacco use. We searched Medline, Embase, The Cochrane database of Systematic Reviews and The Community Guide website (http://www.thecommunityguide.org) for size effect estimates on cigarette consumption and not cessation rates. This is because the CHD Policy Model simulates interventions on smoking through a relative reduction in mean number of cigarettes smoked per day in each sex, age and risk factor strata. We also contacted tobacco control experts for additional bibliographic recommendations. To assess the impact of the national law, the three components of smoke-free environments, pictorial health warnings and advertisement ban were considered multiplicative and their effects were considered independent (table 2). An intervention to increase cigarette prices was added to the model to assess the impact of an additional component to the law, also with a multiplicative effect approach. The effects of the interventions were considered annually, assuming the same effectiveness each year.
Table 2.
Estimated changes in cigarette consumption and exposure to Second Hand Smoke (SHS) with the implementation of the tobacco control law approved by Argentina’s Congress and the additional effect of a cigarette price increase
| Intervention | Description | Estimated effect size* |
Reference |
|---|---|---|---|
| National tobacco control law | Advertising, promotion and sponsorship ban | Decrease in cigarette consumption of 0.6% | 21 |
| Health warnings | Decrease in cigarette consumption of 9% | 22 | |
| 100% smoke-free environments | Decrease in exposure to SHS of 60% | 23 | |
| National law plus a price increase | 100% of price increase | Decrease in cigarette consumption of 31% | Martinez E, Mejia R, Perez-Stable E. Elasticity of cigarette demand in Argentina: an empirical analysis using vector error-correction model. Unpublished work. Personal communication |
The size effects are expressed as relative reductions.
Comprehensive advertising, promotion and sponsorship ban
Several studies have shown that a complete ban on advertising can reduce tobacco consumption24 and prevent relapse,25 but usually estimated the effect of ban as a component of other effective tobacco control measures, such as smoke-free environments. 26 The national law included a comprehensive ban on advertising, promotion and sponsorship, but excludes point of sale restrictions on advertising. Although not a truly comprehensive ban, it implies a much stronger ban that the current national and local regulations. We assumed a 0.6% reduction in cigarette consumption per year if this level of advertising ban was implemented.21
FCTC compliant tobacco products health warnings
Although there is not a clear association between health warnings in tobacco products and cigarette smoking prevalence, strong and pictorial health warnings, adequately sized and located are better recalled and noticed, and are more effective at inducing smoking cessation and preventing smoking initiation in youth.27 The Argentinean law required FCTC compliant health warnings on tobacco products, including pictorial health warnings, strong text messages and images covering at least 50% of all displayed areas, with frequent rotation. We estimated a 9% annual reduction in cigarette consumption if this intervention component was implemented.22
Nationwide 100% smoke-free environment without exceptions
There is consistent evidence that 100% smoking bans reduce exposure to SHS in workplaces, restaurants, bars and public places. The relative reduction in exposure is nearly 60% in most places after several years of implementation of the laws.23 The available data indicates that smoking prevalence may not be reduced by smoke-free environments,23 although in some studies consumption was reduced among workers.28 Therefore, we considered for the CHD Policy Model simulation that this component of the law would result in a 60% relative reduction in SHS exposure, without impact on smoking prevalence or cigarette consumption.
Price increase
Although in Argentina the specific cigarette excise tax contributes to 60–70% of the cigarette price (ad valorem tax), the price of a pack of cigarettes is one of the lowest in Latin America, and sustains it as an affordable product.29 It is known that an increase in the price of cigarettes may lead to a reduction in consumption and has been suggested as one of the most important measures for tobacco control.2 However, the effectiveness of this intervention has to be adjusted for local elasticity (relationship between price and demand). We estimated a 100% final price increase for the model simulation. We modelled an increase in final price since the current low price of a package in Argentina reduces the impact of the ad valorem tax increase, resulting in a non-significant final price increase. Analysing local econometric data, incorporating cigarette consumption elasticity, we considered for the model that a 100% price increase would reduce cigarette consumption by 31% (E Martinez, R Mejia, E Perez-Stable. Elasticity of cigarette demand in Argentina: an empirical analysis using vector error-correction model. Unpublished work. Personal communication).
Sensitivity analysis
Since the effects of the new law cannot be precisely known in advance, we conducted sensitivity analyses considering ‘low effect’ and ‘high effect’ scenarios. For the low effect scenario, we modelled a scenario with less than full compliance of the law and a smaller price increase. A study conducted by the Ministry of Health evaluated smoke-free law’s compliance in cities with local 100% smoke-free laws and reported 21% non-compliance. 30 Based on that data, we assumed a reduction in 21% of 100% smoke-free environment size effect for modelling the low effect scenario. Other econometric studies about cigarette consumption elasticity in Argentina evaluated the impact of increasing the specific cigarette excise tax and suggested that an increase of 50% of this ad valorem tax (that may represent approximately a 30% final price increase) would reduce cigarette consumption by 12%.31 For the ‘low effects’ scenario of the ‘law plus price increase’ we modelled that an increase of 50% in the ad valorem tax would reduce cigarette consumption by 12%. The advertising ban and warning labels size effects remained unchanged due to the scarce evidence that linked these variables and consumption.
We also modelled a ‘high effect’ scenario considering the effects that 100% smoke-free environments could have on active cigarette smoking. Although evidence is not conclusive about this effect,23 we modelled that implementing 100% smoke-free environments would have an additional impact producing a 4.6% relative reduction in the number of cigarettes smoked.32 The other size effect inputs (on advertising bans and warning labels and also on the effect of price increase) remained unchanged from the original model.
Finally, in order to take into account the uncertainty in the model’s parameters, we ran Monte Carlo simulations with 1000 iterations, drawing from distributions for each of the risk function beta coefficients. The results of these simulations were used to determine CIs for the projected benefits of each modelled scenario.
RESULTS
Model calibration
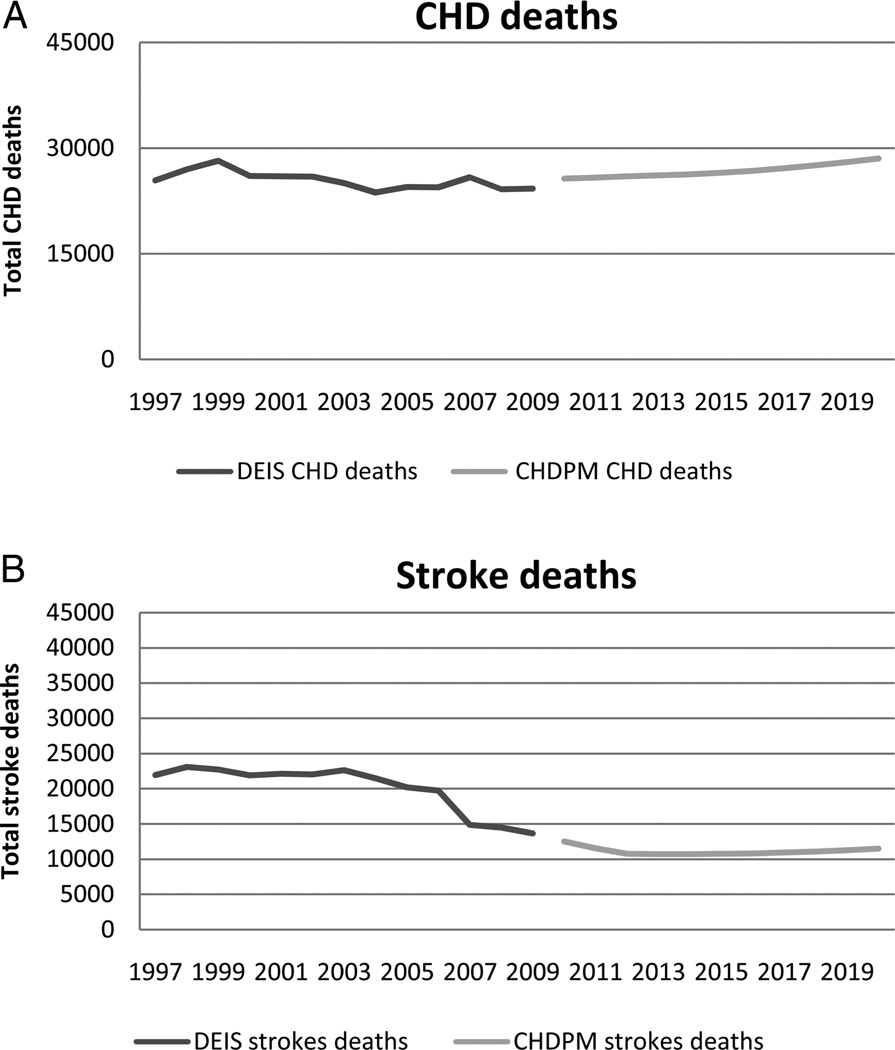
The CHD Policy Model-Argentina predicted number of deaths was compared with actual CHD deaths observed from Argentina vital statistics for the years 1997–2009. We calculated from our national statistics database total CHD deaths in ages 35–84 years, that included definite CHD deaths (codes I20–I25) plus a percentage of poorly defined deaths (named ‘garbage’ codes) that could be attributed to CHD deaths (I461, I469, I472, I490, I460, I500, I501, I509, I514, I515, I516, I519, I709).33 We found a difference of less than 5% between the last total CHD deaths available from national statistics (24 246 for year 2009), compared with the first estimation of total CHD deaths from the CHD Policy Model (24 640 for year 2010) (figure 1A). Regarding stroke deaths, the difference observed was less than 10% (figure 1B). Moreover, the trend in projected CHD deaths (2010–2020) is similar to the trend in previous years. Poorly defined coded CHD deaths recorded by Argentina vital statistics remained a constant proportion of total deaths, suggesting that coding practices remained unchanged over that interval. Similar bias does not affect stroke mortality statistics, so stroke death rates were not adjusted.
Figure 1.
Coronary heart disease (CHD) deaths (A) and stroke deaths (B) from vital statistics (Dirección de Estadística e Información en Salud, Ministerio de Salud de la Nación, DEIS) and projected by CHD Policy Model-Argentina (CHDPM).
Projected impact
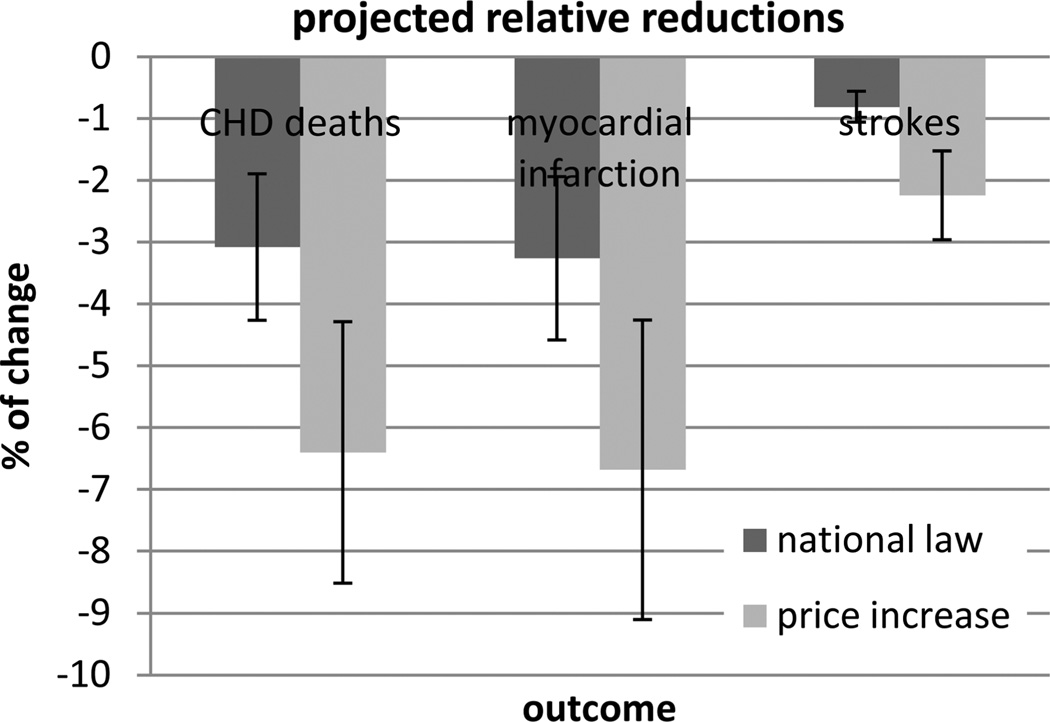
The implementation of the current national law would avoid 7500 CHD deaths, 16 900 MIs and 4300 strokes through 2020 (table 3). These avoided events would represent a reduction of 3%, 3% and 1% in CHD deaths, MIs and strokes, respectively, as compared to continuing current baseline. If the price increase was added to the intervention components of the national law, the number of avoided events would potentially increase to: 15 500CHD deaths, 34 600 MIs and 11 900 strokes saved (what would represent a decrease in 8%, 7% and 6% in CHD deaths, MIs and strokes, respectively) (figure 2). It is important to note that the benefits of reducing tobacco use and exposure are observed in a short time period and by 2016 4200 CHD deaths, 9000 MIs and 2500 strokes would be avoided if the law was implemented and 8900 CHD deaths, 19 500 MIs and 6700 strokes if the price increase was added to the law.
Table 3.
Projected and saved events from 2012–2020 in different scenarios
| CHD deaths | Myocardial infarction | Strokes | |
|---|---|---|---|
| Events | |||
| Baseline | |||
| Men | 155100 (152000–159000) | 334400 (324000–344000) | 248100 (247000–249000) |
| Women | 87300 (86000–89000) | 182700 (179000–186000) | 281700 (280000–284000) |
| Total | 242400 (238000–247000) | 517100 (503000–531000) | 529800 (527000–532000) |
| Events avoided | |||
| Tobacco law | |||
| Men | 5300 (3300–7200) | 12100 (7400–17000) | 2500 (1400–3600) |
| Women | 2200 (1300–3100) | 4800 (2600–6900) | 1800 (1000–2500) |
| Total | 7500 (4600–10300) | 16900 (10000–23700) | 4300 (3000–5600) |
| Law plus price increase | |||
| Men | 11400 (7800–15000) | 26000 (17100–34800) | 7700 (4300–11200) |
| Women | 4100 (2600–5700) | 8600 (4900–12300) | 4200 (2300–6000) |
| Total | 15500 (10400–20700) | 34600 (22000–47100) | 11900 (8100–15700) |
CHD, coronary heart disease.
Figure 2.
Projected relative reductions in coronary heart disease (CHD) deaths, myocardial infarctions and stroke if the national law was implemented and if price increase was included in the law compared with the basal scenario.
Although it was not the aim of the study, the implementation of this law would also have benefits in non-CHD mortality due to the reduction of lung cancer for example. It is projected that 8600 non-CHD deaths could be avoided with the law and 24 800 if a price increase was included.
Sex and age differences in estimated benefit
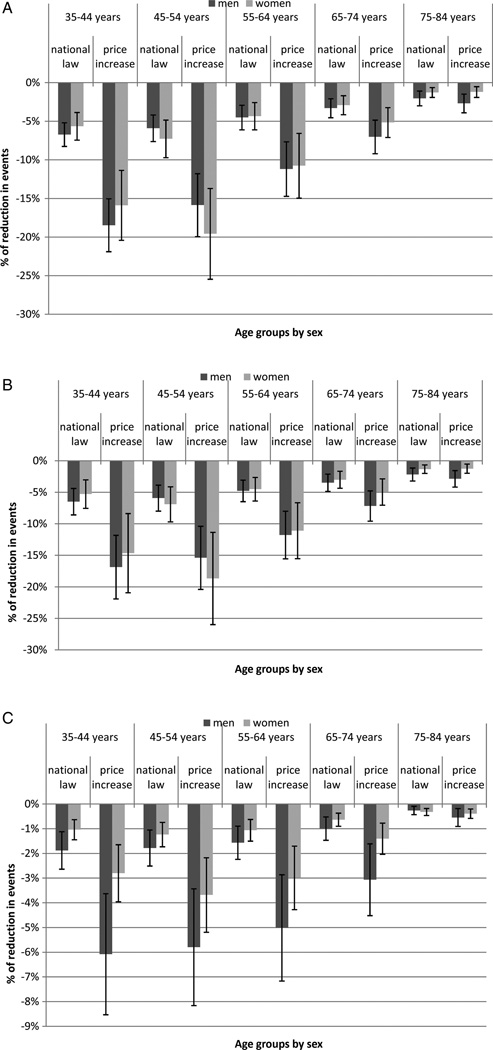
The CHD deaths prevented with the implementation of the national law would occur mostly in men since men are the gender that suffers more CHD deaths (149 900, 64% of all deaths). This benefit would also be more evident in men if the law included the price increase (143 400, 63% of all deaths). In both cases, the tobacco control interventions would have more impact among the younger age groups (35–54 years) for CHD deaths included in the policy model (figure 3A). The MIs avoided would also occur mainly among men and those between 35–64 years if the national law was implemented, and similarly, if a cigarette price increase was added to the law since men are more likely to develop MIs (322 200, 64% and 377 800, 64% of all MIs respectively; figure 3B). On the other hand, the impact of these interventions on stroke prevention would be greater among women who would have a majority of avoided strokes (307 700, 53% of all strokes) if the law was implemented. If the cigarette price was increased, there were similar findings in stroke prevention that benefit more women than men (280 000 strokes, women with 54%). Similar to the previous analysis of avoided CHD events and MIs, the youngest groups from 35 to 64 years would benefit the most from implementation of the law (figure 3C).
Figure 3.
Absolute reductions in coronary heart disease deaths (A), myocardial infarctions (B) and strokes (C) if the national law was implemented and if price increase was included in the law, compared with the existing baseline scenario, by sex and age groups.
Sensitivity analysis
The sensitivity analysis shows that the benefits would be even high in the ‘low effect’ scenario since the implementation of the Argentinean Tobacco Law could avoid 6800 CHD deaths, 15 400 MIs and 4000 strokes. In addition, if the price increase was added to this ‘low effect’ scenario the CHD deaths, MIs and strokes saved could be 7900, 17 700 and 4900 respectively (table 4).
Table 4.
Projected and saved events in the low and high effects scenarios from 2012–2020
| CHD deaths |
Myocardial infarction |
Strokes |
||||
|---|---|---|---|---|---|---|
| Scenario | Low effects | High effects | Low effects | High effects | Low effects | High effects |
| Events | ||||||
| Baseline | ||||||
| Men | 155.100 (152000–159000) | 155.100 (152000–159000) | 334.400 (324000–344000) | 334.400 (324000–344000) | 248.100 (247000–249000) | 248.100 (247000–249000) |
| Women | 87.300 (86000–89000) | 87.300 (86000–89000) | 182.700 (179000–186000) | 182.700 (179000–186000) | 281.700 (280000–284000) | 281.700 (280000–284000) |
| Total | 242.400 (238000–247000) | 242.400 (238000–247000) | 517.100 (503000–531000) | 517.100 (503000–531000) | 529.800 (527000–532000) | 529.800 (527000–532000) |
| Events avoided | ||||||
| Tobacco law | ||||||
| Men | 4.800 (3100–6600) | 6.500 (4200–8700) | 11.100 (6800–15400) | 14.800 (9400–20100) | 2.400 (1300–3500) | 3.300 (13800–4700) |
| Women | 2.000 (1100–2800) | 2.600 (1600–3700) | 4.300 (2300–6200) | 5.700 (3300–8100) | 1.600 (900–2300) | 2.200 (1200–3100) |
| Total | 6.800 (4200–9400) | 9.100 (5800–12400) | 15.400 (92000–21600) | 20.500 (127000–28300) | 4.000 (2700–5400) | 5.500 (3700–7200) |
| Law plus price increase | ||||||
| Men | 5.700 (3700–7700) | 11.800 (8200–15500) | 12.900 (8100–17700) | 26.800 (17800–35900) | 3.000 (1600–4400) | 8.100 (4600–11600) |
| Women | 2.200 (1300–3200) | 4.200 (2600–5800) | 4.800 (2600–6900) | 8.800 (5000–12600) | 1.900 (1100–2700) | 4.400 (2400–6400) |
| Total | 7.900 (5000–10800) | 16.000 (10800–21300) | 17.700 (10700–24700) | 35.600 (22800–48500) | 4.900 (3200–6600) | 12.500 8500–16500) |
CHD, coronary heart disease.
Moreover, in the setting of a ‘high effect’ scenario the additional impact would be considerable, avoiding 9100 CHD deaths, 20 500 MIs and 5500 strokes with the law and 16 000 CHD deaths, 35 600 MIs and 12 500 stroke if the price increase was included (table 4).
DISCUSSION
The impact of the implementation of the national tobacco control law on the health of the public in Argentina would be dramatic in terms of avoided CHD deaths, MIs and strokes. These results should provide persuasive evidence to convince the Executive Branch to authorise full implementation of the law before more unnecessary deaths occur in the population. In addition, if this law could be improved with a mandate to increase the price of cigarettes, the number of avoided heart attacks and strokes and saved lives would be even higher. Men have both higher CHD risk34 and higher smoking prevalence compared with women, and, as a consequence men would benefit more from increased tobacco control in terms of avoided CHD deaths and MIs. The middle-aged population represents the targeted segment for many tobacco control programs1 and it is precisely in this group for whom interventions would be the most cost effective, even though the target population of these tobacco control measures includes everyone.
These results reflect the expected effectiveness of the measures included in the national law, such as implementation of smoke-free environments, advertising, promotion and sponsorship ban and pictorial warnings in cigarette packages, and assuming a full implementation and enforcement. Even in the ‘low effect’ scenario that considered a weak enforcement the impact would be really high. There is strong evidence that a tobacco control initiative like this will reduce deaths from CHD over a few years.28 We also modelled the incremental effect of a significant price increase even though it is not currently included in the national tobacco control law.35 Additionally, if the price increase was limited, as modelled in the ‘low effect’ scenario, the impact of such measure is still considerable. Given that a price increase is known to be the most effective measure to reduce tobacco consumption, cigarette price increase needs to be discussed as part of Argentina’s public health agenda.
Some modelling experiences regarding tobacco control have been developed in the region. Ferrante et al modelled the effect of tobacco control policies in smoking prevalence and associated future premature mortality using the SimSmoke36 but projecting the effect of a generic package of tobacco control laws.37 The availability of new epidemiological and demographic data, improved non-communicable diseases surveillance methods and the recent sanction of a national tobacco control law enhances the value and timeliness of the current modelling. Moreover, to our knowledge this is the first time that the potential benefit of a concrete law is modelled for a Latin American country and in addition the first time the CHD Policy Model is used for this purpose.
National tobacco control laws have been successfully implemented in several countries of Latin America. In 2006 Uruguay became the first Latin American country to adopt a comprehensive 100% smoke-free tobacco control law that achieved a dramatic reduction in smoking prevalence29 and in cardiovascular morbidity. 38 These analyses based on the CHD Policy model are likely to be applicable to other Latin American countries and can be used to advocate robust tobacco control legislation in the region.
Although legislation is considered one of the most powerful resources for improving health of populations,39 some threats may undermine its impact. Wong et al40 identified lobby group opposition as a threat to legislative intervention but suggested the need to be assessed the feasibility of tobacco industry lobbying in each case. There is evidence of tobacco interferences through lobbying not only in Latin America41 but also in Argentina, for example, impeding the ratification of the FCTC.42 Authorities should be alerted about these tactics and must be convinced of the huge impact on public health the implementation of this law will have to be able to succeed.
We identified several limitations in this study. Uncertainty regarding the external validity of some intervention effect size data collected from other jurisdictions could represent a threat to the accuracy of the findings. It is difficult to estimate the isolated effect of each intervention, since the available evidence often comes from pre–post studies that implement several interventions at the same time. In addition, although we incorporated all the available local and regional data to the model, some of them could not be representative of the national level. Lastly, although the CHD Policy Model was developed in a population that could suffer cardiovascular events with a different set of associations and weights between risk factors and outcomes, compared with a Latin American population,43 the model has been calibrated to Argentina and evidence suggest that the effect of risk factors on cardiovascular disease outcomes are essentially universal.44
In order to improve the accuracy of these findings, disease morbidity registries need to be developed and sustained at a national level so that population based data increases generalisability. The availability of comprehensive information of the Global Adult Tobacco Survey, now being implemented in Argentina, could also help to contextualise the impact that the implementation of this law may have.
We believe that the impact of this law, especially if price increases are included, would be very significant in Argentina. We consider that these results may also be extended to other Latin American countries that may not be considering robust tobacco control laws, with demonstrated health benefits, due to tobacco industry influence. This analysis should urge authorities to authorise and fully implement the national tobacco control law since it is an initiative that would save thousands of lives and would reduce the incidence of major cardiovascular events. Although a cost-effective analysis was not developed it is probable that this constitutes a cost saving intervention for Argentina.37 The simulation of a scenario of cigarette price increase reflects the importance of including such interventions into a more comprehensive tobacco control law. Our results provide evidence-based support for advocates to convince government authorities and for authorities themselves to face tobacco industry lobby that could help to authorise and fully implement the current legislation and to eventually improve the national tobacco control law through a price increase. The development of this type of report may represent an invaluable component in support of Argentina’s tobacco control movement.
Supplementary Material
What this paper adds.
-
▸
Although legislation is considered one of the most powerful resources for improving health of populations, particularly for tobacco control, some threats (tobacco industry lobbying for eg) may undermine its impact.
-
▸
This paper reflects the effectiveness of the Argentinean tobacco control law in terms of cardiovascular disease and provides evidence-based support for government and advocates fighting for full implementation of the current legislation.
Acknowledgments
Funding This work was supported by the Tobacco Research Network Programme, Fogarty International Center, National Cancer Institute, National Institute of Drug Abuse, National Institutes of Health grant number TW05935.
Footnotes
Contributors JK undertook the literature review, designed the study, modelled the data, interpreted the results and drafted of the paper. DF undertook the literature review, designed the study, modelled the data and drafted the paper. RM designed the study and drafted the paper. PC modelled the data and drafted the paper. AM designed the study and drafted the paper. LG designed the study and drafted the paper. EPS designed the study and drafted the paper.
Competing interests None.
Provenance and peer review Not commissioned; externally peer reviewed.
Data sharing statement Supplementary data is available in appendix 1. Additional data may be sent upon request.
REFERENCES
- 1.World Health Organization. 2008–2013 Action Plan for the Global Strategy for the Prevention and Control of Noncommunicable Diseases. Geneva: World Health Organization; 2008. [Google Scholar]
- 2.WHO Report on the Global Tobacco Epidemic. The MPOWER package. 2008. [Google Scholar]
- 3.World Health Organization. Framework Covention on Tobacco Control. Geneva: 2003. [Google Scholar]
- 4.Weinstein M, Coxson P, Williams L, et al. Forecasting coronary heart disease incidence, mortality, and cost: the Coronary Heart Disease Policy Model. Am J Public Health. 1987;77:1417–1426. doi: 10.2105/ajph.77.11.1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tosteson A, Weinstein M, Williams L, et al. Long-term impact of smoking cessation on the incidence of coronary heart disease. Am J Public Health. 1990;80:1481–1486. doi: 10.2105/ajph.80.12.1481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bibbins-Domingo K, Chertow G, Coxson P, et al. Projected effect of dietary salt reductions on future cardiovascular disease. N Engl J Med. 2010;362:590–599. doi: 10.1056/NEJMoa0907355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moran A, Gu D, Zhao D, et al. Future cardiovascular disease in china: markov model and risk factor scenario projections from the coronary heart disease policy model-china. Circ Cardiovasc Qual Outcomes. 2010;3:243–252. doi: 10.1161/CIRCOUTCOMES.109.910711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moran A, Degennaro V, Ferrante D, et al. Coronary heart disease and stroke attributable to major risk factors is similar in Argentina and the United States: the Coronary Heart Disease Policy Model. J Cardiol. 2011;150:332–337. doi: 10.1016/j.ijcard.2011.04.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Instituto Nacional de Estadísticas y Censos. [accessed 15 February];Ministerio de Economía. 2011 www.indec.gov.ar.
- 10.Dirección de Estadísticas e Información en Salud. Ministerio de Salud de la Nación. 2011 [Google Scholar]
- 11.Caccavo A, Alvarez A, Bello F, et al. Incidencia poblacional del infarto con elevación del ST o bloqueo de rama izquierda a lo largo de 11 años en una comunidad de la provincia de Buenos Aires. Rev Argent Cardiol. 2007;75:185–188. [Google Scholar]
- 12.Blanco P, Gagliardi J, Higa C, et al. Infarto agudo de miocardio. Resultados de la Encuesta SAC 2005 en la República Argentina. Rev Argent Cardiol. 2007;75:163–179. [Google Scholar]
- 13.Sposato L, Esnaola M, Zamora R, et al. Quality of Ischemic Stroke Care in Emerging Countries: The Argentinean National Stroke Registry (ReNACer) Stroke. 2008;39:3036–3041. doi: 10.1161/STROKEAHA.108.521062. [DOI] [PubMed] [Google Scholar]
- 14.Ministerio de Salud de la Nación. Factibilidad de Implementación de un sistema de vigilancia telefónico para factores de riesgo de enfermedades crónicas no transmisibles. Boletín de Vigilancia. 2011;5:5–21. [Google Scholar]
- 15.Calle E, Rodriguez E, Jacobs E, et al. The American Cancer Society Cancer Prevention Study II Nutrition Cohort: rationale, study design, and baseline characteristics. Cancer. 2002;94:2490–2501. doi: 10.1002/cncr.101970. [DOI] [PubMed] [Google Scholar]
- 16.Ministerio de Salud de la Nación. Segunda Encuesta Nacional de Factores de Riesgo. Buenos Aires: Ministerio de Salud de la Nación; 2011. [Google Scholar]
- 17.Ferrante D, Virgolini M. Encuesta Nacional de Factores de Riesgo 2005: resultados principales Prevalencia de factores de riesgo de enfermedades cardiovasculares en la Argentina. Rev Argent Cardiol. 2007;75:20–29. [Google Scholar]
- 18.Schargrodsky H, Hernandez-Hernandez R, Champagne B, et al. CARMELA: assessment of cardiovascular risk in seven Latin American cities. Am J Med. 2008;1:58–65. doi: 10.1016/j.amjmed.2007.08.038. [DOI] [PubMed] [Google Scholar]
- 19.Framingham Heart Study CD-ROM: Department of Health and Human Services. 2005. [Google Scholar]
- 20.Wolf P, D’Agostino R, Belanger A, et al. Probability of stroke: a risk profile from the Framingham Study. Stroke. 1991;22:312–318. doi: 10.1161/01.str.22.3.312. [DOI] [PubMed] [Google Scholar]
- 21.Zaza SBP, Harris KW, editors. The Guide to Community Preventive Services: What Works to Promote Health? Atlanta, GA: Oxford University Press; 2005. [Google Scholar]
- 22.Gospodinov N, Irvine I. Global Health Warnings on Tobacco Packaging: Evidence from the Canadian Experiment. Journal of Economic Analysis & Policy. 2004;4 Article 30. Berkeley Electronic Press, 2004. [Google Scholar]
- 23.Callinan J, Clarke A, Doherty K, et al. Legislative smoking bans for reducing secondhand smoke exposure,smoking prevalence and tobacco consumption. Cochrane Database Syst Rev. 2010;4:CD005992. doi: 10.1002/14651858.CD005992.pub2. [DOI] [PubMed] [Google Scholar]
- 24.Fathelrahman A, Omar M, Awang R, et al. Smokers’ responses toward cigarette pack warning labels in predicting quit intention, stage of change, and self-efficacy. Nicotine Tob Res. 2009;11:248–253. doi: 10.1093/ntr/ntn029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Partos T, Borland R, Yong H, et al. Cigarette packet warning labels can prevent relapse: findings from the International Tobacco Control 4-Country policy evaluation cohort study. Tob Control. doi: 10.1136/tobaccocontrol-2011-050254. (In Press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Quentin W, Neubauer S, Leidl R, et al. Advertising bans as a means of tobacco control policy: a systematic literature review of time-series analyses. Int J Public Health. 2007;52:295–307. doi: 10.1007/s00038-007-5131-0. [DOI] [PubMed] [Google Scholar]
- 27.Conference of Parties. COP-3. Fact Sheet: plain packaging. 2008 2008. [Google Scholar]
- 28.Fichtenberg C, Glantz S. Effect of smoke-free workplaces on smoking behaviour: systematic review. BMJ. 2002;325:188. doi: 10.1136/bmj.325.7357.188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Amercian Cancer Society. The Tobacco Atlas. 4th edition. Atlanta: American Cancer Society; 2012. [Google Scholar]
- 30.Ministerio de Salud de la Nación. Monitoreo del cumplimiento de la legislación sobre ambientes libres de humo en 15 ciudades de Argentina. Boletín de Vigilancia. 2011;4:25–34. [Google Scholar]
- 31.Gonzalez Rosada M, Sanchez G, Angueira M, et al. [accessed 15 Oct 2012];Análisis economico del consumo de tabaco en Argentina Buenos Aires 2002. http://www.msal.gov.ar/tabaco/images/stories/institucional/pdf/analisis-economico-tabaco-argentina-2002.pdf.
- 32.Braverman M, Aaro L, Hetland J. Changes in smoking among restaurant and bar employees following Norway’s comprehensive smoking ban. Health Promotion Int. 2008;23:5–15. doi: 10.1093/heapro/dam041. [DOI] [PubMed] [Google Scholar]
- 33.Naghavi M, Makela S, Foreman K, et al. Algorithms for enhancing public health utility of national causes-of-death data. Population Health Metrics. 2010;8 doi: 10.1186/1478-7954-8-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.World Health Organization. Global Burden of Disease Report. Geneva: 2004. [Google Scholar]
- 35.Ranson M, Jha P, Chaloupka F, et al. Global and regional estimates of the effectiveness and cost-effectiveness of price increases and other tobacco control policies. Nicotine Tobacco Res. 2002;4:311–319. doi: 10.1080/14622200210141000. [DOI] [PubMed] [Google Scholar]
- 36.Levy D, Nikolayev L, Mumford E. Recent trends in smoking and the role of public policies: results from the SimSmoke Tobacco Control Policy Simulation Model. Addiction. 2005;10:1526–1537. doi: 10.1111/j.1360-0443.2005.01205.x. [DOI] [PubMed] [Google Scholar]
- 37.Ferrante D, Levy D, Peruga A, et al. The role of public policies in reducing smoking prevalence and deaths: the Argentina Tobacco Policy Simulation Model. Rev Panam Salud Pública. 2007;21:37–49. doi: 10.1590/s1020-49892007000100005. [DOI] [PubMed] [Google Scholar]
- 38.Sebrié E, Sandoya E, Hyland A, et al. Hospital admissions for acute myocardial infarction before and after implementation of a comprehensive smoke-free policy in Uruguay. Tob Control. doi: 10.1136/tobaccocontrol-2011-050134. Published Online First: 15 Feb 2012. doi: 10.1136/tobaccocontrol-2011-050134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gostin L. Public Health Law. Berkeley: University of California Press; 2008. [Google Scholar]
- 40.Wong G, Pawson R, Owen L. Policy guidance on threats to legislative interventions in public health: a realist synthesis. BMC Public Health. 2011;11:222. doi: 10.1186/1471-2458-11-222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Barnoya J, Glantz S. Tobacco industry success in preventing regulation of secondhand smoke in Latin America: the Latin Project. Tob Control. 2002;11:305–314. doi: 10.1136/tc.11.4.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Mejia R, Schoj V, Barnoya J, et al. Tobacco industry strategies to obstruct the FCTC in Argentina. CVD Prevention and Control. 2008;3:173–179. doi: 10.1016/j.cvdpc.2008.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yusuf S, Hawken S, Ounpuu S, et al. INTERHEART Study Investigators. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 44.D’Agostino R, Gundy S, Sullivan L, et al. CHD Risk Prediction Group. Validation of the Framingham coronary heart disease prediction scores: results of a multiple ethnic groups investigation. JAMA. 2001;286:180–187. doi: 10.1001/jama.286.2.180. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.