Abstract
BACKGROUND
Only 56% of outpatient substance abuse treatment programs in the U.S. provide HIV/AIDS education, likely due to the time required to complete existing educational interventions. This report describes results of a third study in a series to develop a brief educational intervention to increase HIV/AIDS knowledge among cocaine-dependent outpatients.
METHODS
Participants (N=90) were randomized to experimental or control conditions and completed two HIV/AIDS knowledge pre-tests with response formats modified to “true-false-don’t know.” Pre-test results were later compared to historical controls that completed pre-tests in their original “true-false” format. Next, participants in the experimental condition completed an HIV/AIDS educational intervention while participants in the control condition completed a sham intervention. Participants in both conditions then completed knowledge tests a second time. Participants in both conditions were subsequently crossed over, and then completed knowledge tests a third time. Post-intervention analyses were conducted using test data from all participants who completed the educational intervention (N=56). A subset of these participants (N=40) completed follow-up tests approximately 9 weeks after completing the educational intervention.
RESULTS
Scores on both pre-tests were lower than those observed in historical controls (p < .001). Scores on knowledge tests increased from baseline after participants completed the educational intervention (p < .001), but not after the sham intervention (p >.05). Scores at follow-up remained higher than baseline scores (p < .001).
CONCLUSIONS
Modifying response formats to include a “don’t know” option likely increases identification of baseline knowledge deficits. This brief intervention is effective at increasing HIV/AIDS knowledge among cocaine-dependent outpatients.
Keywords: HIV/AIDS education, HIV/AIDS drug users, HIV/AIDS knowledge
1. INTRODUCTION
Approximately 1.9 million people the U.S. use cocaine each year (Substance Abuse and Mental Health Services Administration (SAMSHA), 2009). Cocaine users are disproportionately affected by Human Immunodeficiency Virus/Acquired Immunodeficiency Syndrome (HIV/AIDS), primarily because of risky injection drug use and sexual behavior. Around 10% of users inject cocaine, risking HIV infection by sharing injection equipment (syringes, “cookers”, “cottons”, etc.; Chaisson et al., 1989; Hudgins et al., 1995; Morrisette et al., 2007). About 80% of cocaine users are sexually active and risk infection by having multiple sexual partners, failing to use condoms consistently, and/or exchanging sex for drugs or money (Booth et al., 2000; Des Jarlais et al., 1988; Des Jarlais and Semaan, 2008; Astemborski et al., 1994; Celentano, et al., 2008; Strathdee and Stockman, 2010). These behaviors result in HIV prevalence rates that are many times higher among cocaine users than in the general population (4–22% vs. 0.4%; Booth et al., 1993, 2000; Centers for Disease Control and Prevention, 2010; Mathers et al., 2008; McCoy et al., 2004; Strathdee and Sherman, 2003). Prevention of HIV transmission among cocaine users remains a public health priority (National Institute on Drug Abuse, 2011).
Knowledge of HIV transmission and prevention has been identified as a determinant of risk behavior (Catania et al., 1990; Fisher and Fisher, 1992). Cocaine users have deficits in HIV knowledge (Heil et al., 2005; Johnston et al., 2011; Metsch et al., 2004), placing education among the first lines of defense against the spread of HIV. Educational interventions aimed at reducing HIV transmission often combine multiple techniques (e.g., educational lectures or counseling, written materials, audiovisual presentations, etc.) to inform individuals of behaviors that carry transmission risk (e.g., sharing injection equipment, unprotected sexual intercourse, etc.) and effective risk-reduction strategies (e.g., sterilizing injection equipment, using condoms, etc.). A meta-analysis of 18 studies evaluating the efficacy of educational interventions in substance abuse treatment programs concluded that such interventions are effective, but time-consuming, requiring an average of 6 hours to complete (Prendergast et al., 2001). Constraints on time and resources have likely limited adoption of these existing interventions, with only 56% of U.S. treatment providers offering “HIV/AIDS education, counseling, or support” (Academy for Educational Development, 2002; SAMSHA, 2010). Taken together, these data suggest that the availability of a brief, empirically validated intervention may encourage more programs to provide HIV/AIDS education.
We have previously reported on two studies examining the efficacy of a brief educational intervention for increasing HIV/AIDS knowledge among cocaine-dependent outpatients. The first study (Sigmon et al., 2000) provided evidence that this brief intervention significantly increases HIV/AIDS knowledge. The second study (Heil et al., 2005) replicated these findings using a more rigorous experimental design and also demonstrated that increases in knowledge largely persist for several months. However, the materials used in these studies may have limited the impact of the educational intervention in at least two ways. First, both HIV/AIDS knowledge tests used were administered in a “true-false” response format, encouraging participants to guess on items if they do not know the correct answer (Kelly et al., 1989; Carey et al., 1997). Randomized trials comparing test response formats suggest that the addition of a “don’t-know” option to “true-false” tests significantly decreases guessing and more accurately identifies knowledge deficits without negatively effecting test reliability (Harris and Changas, 1994; Pennington et al., 2001). Second, both the HIV/AIDS educational video and pamphlet used previously were produced over a decade before the studies were conducted and did not represent the most current HIV/AIDS knowledge available. Modifying this intervention to incorporate more current educational materials may further increase its efficacy. The present report describes the results of a study that employed the same rigorous experimental design used previously (Heil et al., 2005) with the addition of these two modifications.
2. METHODS
2.1. Design
This two-arm, randomized, controlled, crossover study was designed to examine the efficacy of a brief educational intervention aimed at increasing HIV knowledge while providing all study participants with HIV education. Participants were recruited from ongoing randomized clinical trials of community reinforcement therapy (CRA) plus vouchers for treating cocaine dependence (Budney and Higgins, 1998; Higgins et al., 2003). All assessments/intervention components took place during four regularly scheduled treatment visits, and no additional monetary compensation was provided for participation. At their first available visit, participants provided informed consent, were randomized to either experimental or control conditions, and completed two HIV/AIDS knowledge pre-tests (described below). At their second available visit, participants in the experimental condition completed the educational intervention (described below), while participants in the control condition completed the sham intervention (described below). Participants in both conditions then completed knowledge tests a second time (post-test 1). At their third available visit, participants in both conditions were crossed over; control condition participants completed the educational intervention and experimental condition participants completed the sham intervention. Participants in both conditions then completed knowledge tests a third time (post-test 2). Participants in both conditions completed knowledge tests a fourth time as a follow-up assessment at least 6 weeks after completing the educational intervention. The University of Vermont’s institutional review board approved all study procedures before study commencement.
2.2 Measures
2.2.1 Instruments
HIV/AIDS knowledge was measured with versions of the AIDS Risk Behavior Knowledge Test (ARBKT; Kelly et al., 1989) and Marsch test (Marsch; Marsch and Bickel, 2001) modified from their original “true-false” response format to a “true-false-don’t know” format. The ARBKT is a standardized 40-item test that measures knowledge of high-risk sexual and drug taking practices, risk reduction steps, and misconceptions regarding HIV/AIDS, and was subjected to reliability and validity testing during its initial development (Kelly et al., 1989). The Marsch is a 50-item test that assesses knowledge in the same three areas as the AKBRT, but includes additional items specific to drug-use related risks. Prior work utilizing the Marsch has shown it to be more comprehensive than, but strongly correlated with, the ARBKT (Marsch et al., 1999; Marsch and Bickel, 2001).
2.3 Interventions
2.3.1 Educational intervention
The educational intervention was delivered to each participant individually in a single session by a master’s level therapist, and consisted of three components: (1) viewing a 23-minute HIV/AIDS educational video (HIV/AIDS: The Untold Truth and Myths; NIMCO Inc., 2002); (2) reviewing a 15-page HIV/AIDS education pamphlet (“HIV and AIDS -What you need to know”; Channing L. Bete Company, 2008) with the therapist; and (3) reviewing pre-tests with the therapist, who provided corrective feedback on questions answered incorrectly or “don’t know”. The educational intervention took ~50 minutes to deliver.
2.3.2 Sham intervention
The sham intervention was delivered in the same manner as the educational intervention, and consisted of two components: (1) viewing a 10-minute video excerpt on the pharmacology of cocaine (The Haight-Ashbury Cocaine Film: Physiology, Compulsion, Recovery; Cohen and Steinbroner, 1985); and (2) reviewing a 4-page pamphlet on the psychopharmacology of stimulants (“Mind Over Matter: The Brain’s Response to Stimulants”; National Institute on Drug Abuse, 1997). The sham intervention took ~20 minutes to deliver.
2.4 Participants
2.4.1 Study population
Ninety cocaine-dependent outpatients consented, were randomized (47 to the experimental condition and 43 to the control condition), and completed pre-tests. Of these, 34 (17 experimental, 17 control) withdrew from the cocaine treatment trial before completing the educational intervention. The remaining 56 participants completed the educational intervention an average of 29(±28) days after completing pre-tests. Sixteen additional participants (9 experimental, 7 control) withdrew from cocaine treatment before completing the follow-up assessment. The remaining 40 participants completed follow-up an average of 61(±16) days after completing the educational intervention.
2.4.2 Participant characteristics
Baseline characteristics (demographics, cocaine use, other drug dependence, and HIV risk behaviors) were collected at treatment intake and compared between experimental and control conditions using chi-square tests (categorical variables) or t tests (continuous variables). There was no evidence of differential dropout rates between experimental and control conditions and no differences between dropouts and completers on pre-test scores or demographic variables (Table 1).
Table 1.
Demographics, cocaine use, other drug dependence, and HIV risk behaviors among participants who completed the educational intervention in the experimental and control conditions.
| Characteristic | Experimental (n=30) | Control (n=26) |
|---|---|---|
| Demographics | ||
| Age (years) (Mean ± SD) | 36 (9.2) | 36 (9.3) |
| Race (% white) | 90 | 81 |
| Gender (% male) | 70 | 73 |
| Marital Status (% married) | 13 | 15 |
| Education (≥ 12 years) | 87 | 86 |
| Employed full-time (≥ 35 hours/week) (%) | 60 | 35 |
| Cocaine Use | ||
| Preferred route (%) | ||
| Intranasal | 27 | 23 |
| Inhalation | 53 | 54 |
| Intravenous | 20 | 27 |
| Years regular use (Mean ± SD) | 12 (9.2) | 9 (6.8) |
| Previous treatment (%) | 77 | 54 |
| Other drug dependence | ||
| Alcohol | 43 | 39 |
| Cannabis | 33 | 42 |
| Opioids | 33 | 46 |
| HIV risk behaviors | ||
| Intravenous cocaine use in past 12 months (%) | 27 | 46 |
| Ever injected drugs with a borrowed syringe (%) | 17 | 31 |
| Ever injected drugs without cleaning borrowed syringe (%) | 17 | 23 |
| Uses cocaine with sexual partner (%) | 43 | 35 |
2.5. Data Analysis
2.5.1 Characterizing HIV/AIDS knowledge
Mean scores on ARBKT and Marsch pre-tests were calculated to assess baseline knowledge. To evaluate the effect of modifying response formats on the identification of deficits in HIV/AIDS knowledge, independent samples t-tests were used to compare pre-test scores of all participants in the present study (N=90) to pre-test scores from historical controls who completed tests in their original “true-false” format (N=107; Heil et al., 2005). Statistical significance was determined at the level of p < .05. Descriptive analyses of the frequency of “don’t know” responses on each test overall and on individual test items that received “don’t know” responses from over 30% of participants were also performed.
2.5.2 Improving HIV/AIDS Knowledge
In order to evaluate the efficacy of the educational intervention at increasing HIV/AIDS knowledge, repeated-measures analysis of variance (ANOVA) was used to examine temporal changes in both ARBKT and Marsch scores among the subset of participants who completed the educational intervention (N=56). Independent samples t-tests were then used to compare post-intervention scores between study conditions. McNemar’s test for correlated proportions was used to examine change over time in percentage correct for individual items on each test in order to determine the items on which knowledge significantly improved as a result of the educational intervention. Statistical significance was determined at the level of p < .05 for ANOVA and a more stringent p < .01 for McNemar’s test, since it involved comparisons between 90 pre-test – post-intervention sets of questions.
Among the subset of participants who completed the follow-up assessment (N=40), a second set of repeated-measures ANOVA were conducted to assess the maintenance of any gains in knowledge resulting from the educational intervention. Mean scores on ARBKT and Marsch follow-up tests were compared to pre-test and post-intervention scores collapsed across experimental and control conditions to determine to what extent gains in knowledge persisted after completing the educational intervention. Statistical significance was determined at the level of p < .05.
3. RESULTS
3.1. Characterizing Baseline HIV/AIDS Knowledge Levels
3.1.1 Pre-test
Scores on both ARBKT and Marsch pre-tests were significantly lower in the current study than in the historical control cohort [75% vs. 85% correct on the ARBKT (t(195) =6.74, p < .001) and 72% vs. 84% correct on the Marsch (t(195) = 67.34, p < .001)]. Participants in the current study readily endorsed the “don’t know” option on both pre-tests, with 14% of responses on the ARBKT and 16% of responses on the Marsch being “don’t know.” Thirteen items (7 from the ARBKT and 6 from the Marsch; Table 2.) received “don’t know” responses from at least 30% of participants. Four of these items assess knowledge of high-risk sexual practices, 2 assess knowledge of risk reduction steps and 7 assess misconceptions regarding HIV/AIDS.
Table 2.
Items that ≥ 30% of participants answered “don’t know” on the pre-tests
| Item | Correct Answer | % Answered “don’t know” |
|---|---|---|
| High-risk sexual practices | ||
| M24. The HIV virus is present in vaginal secretions. | TRUE | 36 |
| A16. Pre-ejaculatory fluids carry the AIDS virus. | TRUE | 33 |
| M42. Using oil-based lubricants, such as hand lotion, cold cream, food products or baby oil, with a condom will weaken the condom and increase the likelihood that it may break during sex. | TRUE | 33 |
| M32. HIV can be transmitted through menstrual blood. | TRUE | 32 |
| Risk-reduction steps | ||
| M31. Latex condoms are better than natural skin or lambskin condoms in preventing the spread of HIV. | TRUE | 36 |
| M43. Boiling “drug works” for 15 minutes before each use will reduce the likelihood of becoming infected with the AIDS virus. | TRUE | 34 |
| Misconceptions regarding HIV/AIDS | ||
| A30. A positive result on the AIDS antibody test can occur even for people who do not carry the virus. | TRUE | 42 |
| A33. Most present cases of AIDS are due to blood transfusions that took place before 1984. | FALSE | 37 |
| A29. A negative result on the AIDS virus antibody test can occur even for people who carry the virus. | TRUE | 36 |
| M16. An infected mother can give HIV to her infant via breastfeeding (milk). | TRUE | 33 |
| A40. The AIDS virus can be transmitted by mosquitoes or cockroaches | FALSE | 33 |
| A37. No cases of AIDS have ever been linked to social (dry) kissing. | TRUE | 31 |
| A13. The AIDS virus does not penetrate unbroken skin. | TRUE | 30 |
Note. “A” denotes items from the ARBKT. From “An Objective Test of AIDS Risk Behavior Knowledge: Scale Development, Validation, and Norms” by J. A. Kelly, J. S. St. Lawrence, H. V. Hood, and T. L. Brasfield, 1989, Journal of Behavior Therapy and Experimental Psychiatry, 20, 227–234. “M” denotes items from the Marsch test (Marsch and Bickel, 2001; Marsch, Bickel, & Jacobs, 1999).
3.2. Improving HIV/AIDS Knowledge
3.2.1. Post-test 1
Differential changes between conditions in mean percentage correct were observed on both the ARBKT and Marsch tests from pre-test to post-test 1 (F(1,55) = 25.87, p < .001 and F(1,55) = 27.23, p < .001) (Figure 1). Mean percentage correct on both tests increased significantly in the experimental condition [78% vs. 94% correct on the ARBKT (F(1,29) = 42.03, p < .001) and 76% vs. 94% correct on the Marsch (F(1,29) = 48.78, p < .001)], but not the control condition [73% vs. 75% correct on the ARBKT (F(1,25) = 3.20, p = .08) and 69% vs. 71% correct on the Marsch (F(1,25) = 1.86, p = .18)].
Figure 1.
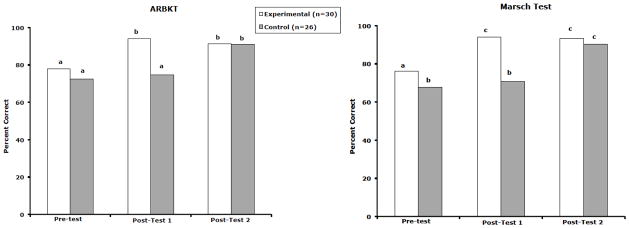
Mean percentage correct in the experimental and control conditions on the ARBKT (Kelly et al., 1989; left panel) and Marsch (Marsch et al., 2001; right panel) tests of HIV/AIDS knowledge at three assessment time points (Pre-test, Post-test 1, and Post-test 2). Bars with a common letter are not significantly different from each other (Fisher’s least significant difference, p < .05).
3.2.2. Post-test 2
Mean percentage correct on both ARBKT and March tests increased in the control condition after crossover [73% vs. 91% correct on the ARBKT (F(1,25) = 34.62, p < .001) and 69% vs. 90% correct on the Marsch (F(1,25) = 65.04, p < .001)]. Post-test 2 scores in the control condition were not significantly different from the post-test 1 scores observed in the experimental condition [91% vs. 94% correct on the ARBKT (t(55) = 1.43, p = .16) and 90% vs. 94% correct on the Marsch, (t(55) = 1.96, p = .06)], indicating that the crossover eliminated earlier differences between conditions.
3.2.3. Individual items
The educational intervention significantly improved percentage correct on 36 individual items [15 from the ARBKT and 21 from the Marsch (Supplementary Table 11). Thirteen items assessed knowledge of risky sex and drug practices, 5 addressed knowledge of risk reduction steps, and 18 addressed misconceptions regarding HIV/AIDS.
3.2.4. Follow-up
Mean scores on the ARBKT follow-up were significantly lower than post-intervention scores, while mean scores on the Marsch were unchanged [(93% vs. 89% correct on the ARBKT, F(1,39) = 9.92, p < .01) and (92% vs. 90% correct on the Marsch, F(1,39) = 3.55, p = .07)]. Perhaps most importantly, mean scores on both follow-up tests remained significantly higher than baseline scores [(89% vs. 74% correct on the ARBKT, (F(1,39) = 36.03, p < .001) and 90% vs. 72% correct on the Marsch, (F(1,39) = 43.35, p < .001), respectively].
4. DISCUSSION
The present report describes the results of a prospective, experimental study designed to further develop and examine the efficacy of a brief educational intervention to increase HIV/AIDS knowledge among cocaine-dependent outpatients. This study represents the first use, to our knowledge, of ARBKT and Marsch tests with modified response formats. Other studies demonstrated that modifying response formats from “true-false” to “true-false-don’t know” increases identification of knowledge deficits (Harris and Changas, 1994; Pennington et al., 2001). Consistent with these findings, the addition of a “don’t know” response option resulted in significantly lower pre-test scores than those observed in our historical control cohort, suggesting that the present study more accurately characterizes baseline HIV/AIDS knowledge among cocaine-dependent outpatients by identifying additional knowledge deficits. More than 30% of participants in the present study reported not knowing the answer to items related to high-risk sexual practices (4 items) and risk-reduction steps (2 items). For example, 33% of participants indicated they did not know that pre-ejaculatory fluids can carry the HIV virus, and 36% did not know that latex condoms are better than natural skin or lambskin condoms at preventing the spread of HIV. Failure to include a “don’t know” option on HIV/AIDS knowledge assessment instruments risks overlooking such important gaps in knowledge. In this particular situation where deficits in knowledge can lead to contracting a life-threatening condition, we feel the potential clinical advantages of using a “true-false- don’t know” response format far outweigh any potential limitations associated with modifying the tests.
The present results further support the efficacy of this brief educational intervention for increasing HIV/AIDS knowledge among cocaine-dependent outpatients. Significant increases in overall knowledge were observed on both tests after participants completed the educational intervention. Most importantly, these gains in knowledge largely persisted for at least 6 weeks following the educational intervention, indicating that the intervention has some lasting effect on HIV/AIDS knowledge.
Since both the ARBKT and Marsch tests contained items related to high-risk practices, risk reduction steps, and misconceptions about HIV/AIDS, it is important to look beyond overall test scores to ensure that knowledge increases are in an area of potential clinical significance. For example, teaching patients that oral sex and sharing drug works can transmit HIV is more likely to reduce their risk of contracting HIV than correcting their misconceptions about HIV being transmitted through shared kitchen utensils or by mosquitoes or bugs. Analyses of scores on individual items pre-and-post-intervention revealed improvements in HIV/AIDS knowledge on a number of items related to high-risk behaviors and risk-reduction steps, suggesting the educational intervention is increasing HIV/AIDS knowledge in areas that could impact HIV transmission risk.
These findings must be considered in light of some limitations. First, one-third of the randomized sample did not complete the educational intervention and were excluded from the analyses evaluating its efficacy. The fact that all drop-outs withdrew from the parent cocaine treatment trial rather than the present study and that there were no differences between drop-outs and completers with regard to baseline demographic characteristics, pre-test scores, or study condition decrease potential concerns about the generalizability of these results. In addition, drop out would be of less concern in actual clinical practice, where the educational intervention could be delivered in a single session rather than the multiple sessions required by the rigorous design of the present study. Second, the same HIV/AIDS knowledge tests reviewed during the educational intervention were used as the post-intervention assessments, making it unclear whether observed knowledge gains generalize to real-world scenarios of HIV risk. Future studies may benefit from the use of additional instruments that force participants to apply their knowledge. Third, we did not measure self-reported HIV risk behaviors to determine whether the experimental intervention actually changed behavior. It seems unlikely that a brief educational intervention alone is sufficient to modify risky behaviors, but HIV/AIDS knowledge has been identified as one determinant of risk behavior (Catania et al., 1990; Fisher and Fisher, 1992) and HIV education should be part of standard outpatient substance abuse treatment.
This report summarizes the third in a series of studies on the development of a brief educational intervention to improve HIV/AIDS knowledge among cocaine-dependent outpatients. The modification of HIV knowledge tests to include “don’t know” as a response option allowed us to identify and provide corrective education to address deficits in HIV knowledge that may have been missed by knowledge tests administered in a traditional “true-false” format. The educational intervention produced significant and persistent increases in HIV/AIDS knowledge among individuals at risk for HIV infection. This intervention is inexpensive, requires few materials, and takes less than one hour to complete. These characteristics make it a practicable option for outpatient substance abuse treatment programs that want to provide HIV/AIDS education, but have limited resources.
Supplementary Material
Acknowledgments
Role of Funding Source
Supported by grants R01DA009378 and T32DA07242 from the National Institute on Drug Abuse (NIDA). The NIDA had no further role in study design; in the collection, analysis, or interpretation of data; in the writing of this report; or in the decision to submit this paper for publication.
The authors would like to thank Gary Badger for consultation on statistical methods and Robert Donham, Kristen Ironside, and Christopher Pepin for their assistance in data collection. Kelly E. Dunn is now at Johns Hopkins University School of Medicine, Baltimore, MD. Yukiko Washio is now at The Treatment Research Institute, Philadelphia, PA.
Footnotes
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:...
Supplementary material can be found by accessing the online version of this paper at http://dx.doi.org and by entering doi:...
Contributors
Authors Evan Herrmann, Sarah Heil, and Kelly Dunn designed the study and developed the protocol. Evan Herrmann, Yukiko Washio, and Sarah Heil managed data collection. Evan Herrmann undertook the statistical analysis. Evan Herrmann, Sarah Heil, Stacey Sigmon, and Stephen Higgins wrote the first draft of the manuscript. All authors contributed to and have approved the final manuscript.
Conflict of Interest
No conflict declared.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Academy for Educational Development. Linking HIV prevention services and substance abuse treatment programs. U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2002. http://www.cdc.gov/idu. [Google Scholar]
- Astemborski J, Vlahov D, Warren D, Solomon L, Nelson KE. The trading of sex for drugs or money and HIV seropositivity among female intravenous drug users. Am J Public Health. 1994;84:382–387. doi: 10.2105/ajph.84.3.382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Booth RE, Kwiatkowski CF, Chitwood DD. Sex related HIV risk behaviors: differential risks among injection drug users, crack smokers, and injection drug users who smoke crack. Drug Alcohol Depend. 2000;58:219–226. doi: 10.1016/s0376-8716(99)00094-0. [DOI] [PubMed] [Google Scholar]
- Booth RE, Watters JK, Chitwood DD. HIV risk-related sex behaviors among injection drug users, crack smokers, and injection drug users who smoke crack. Am J Public Health. 1993;83:1144–1148. doi: 10.2105/ajph.83.8.1144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Budney A, Higgins ST. Treating cocaine addiction: a community reinforcement plus vouchers approach (NIH Publication No 98-4309) National Institute on Drug Abuse; Rockville, MD: 1998. [Google Scholar]
- Carey MP, Morrison-Beedy D, Johnson BT. The HIV-Knowledge Questionnaire: development and evaluation of a reliable, valid, and practical self-administered questionnaire. AIDS Behav. 1997;1:61–74. [Google Scholar]
- Catania JA, Kegeles SM, Coates TJ. Towards an understanding of risk behavior: an AIDS risk reduction model (ARRM) Health Educ Behav. 1990;17:53–72. doi: 10.1177/109019819001700107. [DOI] [PubMed] [Google Scholar]
- Celentano DD, Latimore AD, Mehta SH. Variations in sexual risks in drug users: emerging themes in a behavioral context. Curr HIV/AIDS Rep. 2008;5:212–218. doi: 10.1007/s11904-008-0030-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chaisson RE, Bacchetti P, Osmond D, Brodie B, Sande MA, Moss AR. Cocaine use and HIV infection in intravenous drug users in San Francisco. JAMA. 1989;261:561–565. [PubMed] [Google Scholar]
- Channing L Bete Company. HIV and AIDS -- What you need to know [Brochure] South Deerfield, MA: 2008. [Google Scholar]
- Cohen WE, Steinbroner P. The Haight-Ashbury cocaine film: Physiology, compulsion, recovery [Motion picture] Cinemed; United States: 1985. [Google Scholar]
- Des Jarlais DC, Friedman SR, Stoneburner RL. HIV infection and intravenous drug use: critical issues in transmission dynamics, infection outcomes, and prevention. Rev Infect Dis. 1988;10:151–158. doi: 10.1093/clinids/10.1.151. [DOI] [PubMed] [Google Scholar]
- Des Jarlais DC, Semaan S. HIV prevention for injecting drug users: the first 25 years and counting. Psychosom Med. 2008;70:606–611. doi: 10.1097/PSY.0b013e3181772157. [DOI] [PubMed] [Google Scholar]
- Fisher JD, Fisher WA. Changing AIDS-risk behavior. Psychol Bull. 1992;111:455–471. doi: 10.1037/0033-2909.111.3.455. [DOI] [PubMed] [Google Scholar]
- Harris DK, Changas PS. Revision of Palmore’s second facts on aging quiz from a true-false to a multiple-choice format. Educ Gerontol. 1994;20:741–754. [Google Scholar]
- Heil SH, Sigmon SC, Mongeon JA, Higgins ST. Characterizing and improving HIV/AIDS knowledge among cocaine-dependent outpatients. Exp Clin Psychopharmacol. 2005;13:238–245. doi: 10.1037/1064-1297.13.3.238. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Sigmon SC, Wong CJ, Heil SH, Badger GJ, Donham BD. Community reinforcement therapy for cocaine-dependent outpatients. Arch Gen Psychiatry. 2003;60:1043–1052. doi: 10.1001/archpsyc.60.9.1043. [DOI] [PubMed] [Google Scholar]
- Hudgins R, McCusker J, Stoddard A. Cocaine use and risky injection and sexual behaviors. Drug Alcohol Depend. 1995;37:7–14. doi: 10.1016/0376-8716(94)01060-x. [DOI] [PubMed] [Google Scholar]
- Johnston CL, Marshall BD, Qi J, Zonneveld CJ, Kerr T, Montaner JS, Wood E. HIV knowledge and perceptions of risk in a young, urban, drug-using population. Public Health. 2011;125:791–794. doi: 10.1016/j.puhe.2011.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JA, St Lawrence JS, Hood HV, Brasfield TL. An objective test of AIDS risk behavior knowledge: scale development, validation, and norms. J Behav Ther Exp Psychiatry. 1989;20:227–234. doi: 10.1016/0005-7916(89)90027-x. [DOI] [PubMed] [Google Scholar]
- Marsch LA, Bickel WK. Risk behavior: gender differences during buprenorphine treatment. In: Petry N, editor. Symposium on Gender-Specific Issues in the Addictions. Symposium conducted at the 109th Annual Convention of the American Psychological Association; San Francisco. 2001. [Google Scholar]
- Mathers BM, Degenhardt L, Phillips B, Wiessing L, Hickman M, Strathdee SA, Wodak A, Panda S, Tyndall M, Toufil A, Mattich RP. Global epidemiology of injecting drug use and HIV among people who inject drugs: a systematic review. Lancet. 2008;372:1733–1745. doi: 10.1016/S0140-6736(08)61311-2. [DOI] [PubMed] [Google Scholar]
- McCoy CB, Lai S, Metsch LR, Messiah SE, Zhao W. Injection drug use and crack cocaine smoking: independent and dual risk behaviors for HIV infection. Ann Epidemiol. 2004;14:535–542. doi: 10.1016/j.annepidem.2003.10.001. [DOI] [PubMed] [Google Scholar]
- Metsch LR, McCoy CB, Miles CC, Wohler B. Prevention myths and HIV risk reduction by active drug users. AIDS Educ Prev. 2004;16:150–159. doi: 10.1521/aeap.16.2.150.29392. [DOI] [PubMed] [Google Scholar]
- Morissette C, Cox J, Prithwish D, Tremblay C, Roy C, Allard R, Stephenson R, Graves L. Minimal uptake of sterile drug preparation equipment in a predominantly cocaine injecting population: implications for HIV and hepatitis C prevention. Int J Drug Policy. 2007;18:204–212. doi: 10.1016/j.drugpo.2006.08.004. [DOI] [PubMed] [Google Scholar]
- National Institute on Drug Abuse. Mind Over Matter: The Brain’s Response to Stimulants (NIH Publication No 98-3592) Rockville, MD: 1997. [Google Scholar]
- National Institute on Drug Abuse AIDS Research Program. Current AIDS research priorities. 2011:FY 12. http://www.nida.nih.gov/about/organization/arp/arp-current.htm.
- NIMCO Inc. HIV/AIDS: The Untold Truth and Myths [Motion Picture] Calhoun, KY: 2002. [Google Scholar]
- Pennington HR, Pachana NA, Coyle SL. Use of the facts on aging quiz in New Zealand: validation of questions, performance of a student sample, and effects of a don’t know option. Educ Gerontol. 2001;27:409–416. [Google Scholar]
- Prendergast ML, Urada D, Podus D. Meta-analysis of HIV risk-reduction interventions within drug abuse treatment programs. J Consult Clin Psychol. 2001;69:389–405. doi: 10.1037//0022-006x.69.3.389. [DOI] [PubMed] [Google Scholar]
- Sigmon S, Higgins ST, Badger GJ. August. Characterizing HIV/AIDS Knowledge Among Cocaine-Dependent Outpatients. Paper presented at the 108th Annual Convention of the American Psychological Association; Washington, DC. 2000. [Google Scholar]
- Strathdee SA, Sherman SG. The role of sexual transmission of HIV infection among injection and non-injection drug users. J Urban Health. 2003;80(Suppl 3):iii7–14. doi: 10.1093/jurban/jtg078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strathdee SA, Stockman JK. Epidemiology of HIV among injecting and non-injecting drug users: current trends and implications for interventions. Curr HIV/AIDS Rep. 2010;7:99–106. doi: 10.1007/s11904-010-0043-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. National Survey of Substance Abuse Treatment Services (N-SSATS), 2010 [Survey Documentation and Analysis] 2010 Available from the Substance Abuse and Mental Health Data Archive Website, http://www.icpsr.umich.edu/cocoon/SAMHDA/DAS3/00058.xml.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


